Abstract
Background: The benefit of haptic feedback in laparoscopic virtual reality simulators (VRS) is ambiguous. A previous study found 32% faster acquisition of skills with the combination of 3 D and haptic feedback compared to 2 D only. This study aimed to validate perception and effect on performance of haptic feedback by experienced surgeons in the previously tested VRS. Material and methods: A randomized single blinded cross-over study with laparoscopists (>100 laparoscopic procedures) was conducted in a VRS with 3 D imaging. One group started with haptic feedback, and the other group without. After performing the suturing task with haptics either enabled or disabled, the groups crossed over to the opposite setting. Face validity was assessed through questionnaires. Metrics were obtained from the VRS. Results: The haptics for ‘handling the needle’, ‘needle through tissue’ and ‘tying the knot’ was scored as completely realistic by 3/22, 1/22 and 2/22 respectively. Comparing the metrics for maximum stretch damage between the groups revealed a significantly lower score when a group performed with haptics enabled p = .027 (haptic first group) and p < .001(haptic last group). Conclusion: Haptic feedback in VRS has limited fidelity according to the tested laparoscopic surgeons. In spite of this, significantly less stretch damage was caused with haptics enabled.
Introduction
High fidelity virtual reality simulators (VRS) have shown to be as effective as box trainers in teaching laparoscopic suturing [Citation1–4]. Constructors of VRS have tried to mimic the authentic sense of touch in laparoscopic surgery for years [Citation5,Citation6]. Haptic feedback is not a generic property and different simulators use different types of actuation with different qualities to mimic touch, i.e. shape memory metals, magnetic, piezoelectric materials, electrorheological fluids, DC electric motors (the most common), pneumatic, as well as hydraulic actuation [Citation6]. To compensate for lack of haptic feedback in the simulator, researchers have also tried to mimic this through programming increased resistance in the trocars to mimic the resistance when inserting instruments through the trocars [Citation7].
There is a lack of validation studies on VRS offering this sense of touch, called haptics or force feedback. The few studies performed on VRS with haptics have shown conflicting results concerning usefulness and transferability to the operating room [Citation8–11].
LapSim® (surgicalscience, Gothenburg, Sweden) is a worldwide well-known VRS validated in several studies [Citation12–15]. A previous study found that the time to reach a set proficiency level in a VRS basic skills course, using the LapSim® Haptic System (surgicalscience) with 3 D vision and haptic feedback, was significantly faster than not having 3 D or haptic feedback [Citation16]. Another study using the same LapSim® simulator without haptic feedback, but with 3 D vision, found that skills acquisition was enhanced by the 3 D feature [Citation17]. No validation on the latest LapSim® Haptic System considering haptic feedback has previously been reported.
The primary aim of this study was to establish face validity regarding user experience and perception of haptic feedback in the LapSim® Haptic System by experienced laparoscopic surgeons. The secondary aim was to assess if haptic feedback affected the performance in the VRS for experienced surgeons.
Material and methods
Participants
Surgeons with a minimum experience of 100 laparoscopic procedures were included in this study. All surgeons employed at the Department of Surgery or Paediatric Surgery, Skåne University Hospital, Sweden, were invited to participate and the first 26 responders were included. Background information was obtained (). Self-perception of not being able to perceive 3 D was an exclusion criterion. Microsoft® Excel 2013 was used for randomization into two groups.
Table 1. Demography and experience of participating surgeons.
Study design and setup
A randomized single blinded cross over study was conducted in a VRS with 3 D imaging (LapSim® VR Haptic System, Surgical Science Sweden AB, Gothenburg, Sweden). The instrument joysticks delivered haptic feedback to the user, which was interpreted as tactile sensations, or force feedback, when touching objects in the virtual operating space. The haptic feedback was provided to the joysticks by electrical motors, connected through an interface to the software.
The experiment started with standardized oral instructions and warm-up consisting of a basic “grasping and holding” task with haptics enabled followed by a suturing instruction video on the VRS. The surgeons then performed five suturing attempts with haptics either enabled at start (referred to as ‘haptic-first’ group) or disabled at start (referred to as ‘haptic-last’ group), followed by five new suturing attempts in the opposite haptic setting. The participants rated their perception of three haptic aspects; the needle, tissue and thread, on a 3-point Likert scale, and five graphical aspects; the visceral anatomy, instruments, needle, thread and complete task, on a 5-point Likert scale after each set of five attempts (Appendix A). Graphics were identical throughout the study. The setup and difficulty level for the suturing task were the same as in previous studies examining novices’ learning curves with 3 D and haptics [Citation16]. The participants were informed that the maximum time for each suturing attempt was set at 180 s.
Ethical approval was considered unnecessary since all data were non-sensitive and collected anonymously. Consent for participation was retrieved from each participant before entering the study and it was made clear that participation could be cancelled by the participant without questions and at any moment.
Data analysis and statistical methods
Data from the questionnaire regarding the experts’ opinions were presented with descriptive statistics. A sum score of variables concerning perception of haptic feedback and graphics was constructed and compared using Wilcoxon signed rank test.
Metrics was extracted from the LapSim® software for the parameters time (s), maximum target error (mm), knot error (%), instrument path length (m), instrument angular path length (degrees), instrument outside view (# and s), tissue damage (#) and maximum stretch damage (mm and %) for each attempt in both settings. The three variables that could potentially be influenced by haptics; maximum stretch damage (%), maximum damage (mm) and number of damages to the tissue were analyzed using a linear mixed model, allowing for repeated measures. A p value of <.05 was considered significant. All statistical computations were performed by a statistician using the computer program R (version 3.4.2) [Citation18].
Results
All 26 surgeons enrolled completed the study. Four participants, one in the ‘haptic first’- group and three in the ‘haptic last’-group, had no experience in laparoscopic suturing and were excluded from rating the haptic feedback.
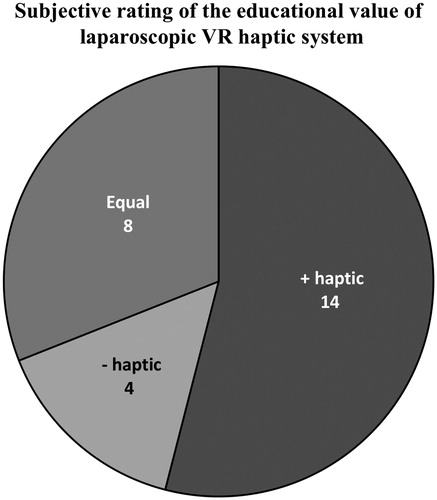
Face validity haptic feedback
The sense of ‘handling the needle’ was scored as completely realistic by 3/22 and moderately realistic by 14/22 in the haptic setting. No surgeon rated “handling of the needle” as completely realistic without haptic feedback. One participant found the ‘needle through tissue’ completely realistic in the haptic setting, but a majority considered this aspect totally unrealistic both with (13/22) and without (16/22) haptic feedback (). For ‘tying the knot’ 17/22 and 13/22 considered it moderately realistic with and without haptic, respectively (). One person (the same) considered ‘tying the knot’ completely realistic in both settings. A sum score of the rating of the haptic feedback (the needle, tissue and thread), showed a significant difference and a higher total score from both groups in the haptic setting (p = .008) and no difference in rating between the two groups (p = .10).
Figure 1. Subjective rating of the sense of touch (haptic feedback) in a VR laparoscopic suturing task. Results from questionnaire rating user experience of ‘handling the needle’, ‘needle through tissue’ and ‘tying the knot’ with or without haptic feedback enabled in the VR simulator on a 3-point Likert scale. Haptic feedback was scored by 22 of 26 surgeons; the four who had never performed laparoscopic suturing were excluded. Values are shown in percent. A sum of the rating showed a significantly higher total score in the haptic setting, p = .0008.
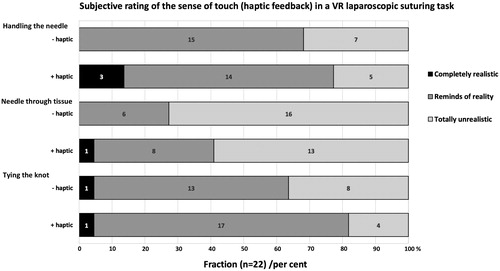
Face validity graphics
The graphics was identical when haptics was enabled or disabled, and was rated twice by the 26 participants. No significant difference in scores between the two settings or groups (p > .3 and p = .07 respectively) was seen. The graphics for ‘instruments’ and ‘needle’ received the highest score as it was considered completely realistic by 12/52 and 13/52, respectively. The graphics of the ‘visceral anatomy’ and the ‘thread’ received the lowest scores for ‘completely realistic’, with 2/52 and 6/52, respectively (). One participant considered the overall graphics for the ‘suturing task’ completely realistic in the haptic setting. All graphical aspects received most ratings as ‘moderately realistic’, ranging from 40 to 65% ().
Figure 2. Subjective rating of the graphic aspects in a VR laparoscopic suturing task. Results from questionnaire rating the graphical interface on a 5-point Likert scale with and without haptic feedback. The needle and instruments were considered the most realistic. A majority found all aspects moderately realistic for all aspects queried. Values are shown in percent. There was no difference in the scores depending on whether haptics was enabled or not.
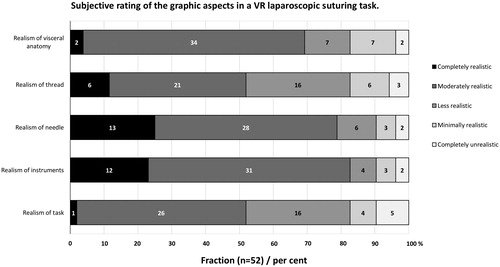
Educational value
A majority of the surgeons (14/26) considered the haptic setting best for education of novices for laparoscopic suturing. One third found the two settings equally good for education (). There was a significant difference in the answers between the two groups; 9/13 participants in the ‘haptic last’ group preferred the haptic setting, and 7/13 in the ‘haptic first’ group considered the two tested settings to have equal educational value (p = .029).
Performance
Four of 26 surgeons reached the required passing level during the first five attempts, and 8/26 in the following five. The passing participants were equally distributed between the groups and settings. Maximum stretch damage changed significantly when haptic feedback was enabled. With this feature both groups outperformed the other group (). The ‘haptic first’-group had a significantly lower score compared to ‘haptic last’-group in the first five attempts, p = .027. The ‘haptic last’-group performed better in the last five attempts (haptic setting) compared to the ‘haptic first’-group without, p < .001.
Table 2. Maximum stretch damage.
Within-group comparisons after cross-over showed that the ‘haptic first’-group had the same level of skills in the non-haptic setting, p = .308, while the ‘haptic last’-group improved when they had haptic feedback, p = .048 (). The other two performance parameters that possibly could be influenced by haptic feedback; maximum damage (mm) and number of tissue damages (#), did not show any significant difference within or between the groups. No sex difference was noted.
Discussion
The aim of this study was to investigate how laparoscopists perceived the new haptic interface of a common laparoscopic VRS and how it affected their performance in the simulator. The results showed that the surgeons exhibited less stretch damage to the simulated tissue when haptics was enabled. However, their rating of the experienced haptic sense showed limitations in perception of fidelity.
The surgeons rated the VRS sense of touch significantly more realistic with haptic feedback enabled than without. However, only a handful considered any of the haptic feedback aspects to be completely realistic. A majority found ‘tying the knot’ and ‘handling the needle’ to ‘resemble reality’ and rated it 2 on a 3-point Likert scale. A majority thought the ‘needle through tissue’ was completely unrealistic (). These results indicate that true sense of touch is yet to be achieved.
The surgeons rated ‘needle through tissue’ to be the most unrealistic part of the task concerning sense of haptic feedback; thus a discrepancy towards the graphical rating of the tissue which scored well with a total of 36/52 considering the visceral anatomy ‘moderately’ or ‘completely’ realistic. In what way the participants felt the ‘needle through tissue’ to be unrealistic is not known since no in-depth questions were asked. The well-known ‘representation’ of tissue texture for surgeons with years of experience may be hard to evaluate [Citation19].
Even if the experience of haptic feedback was considered not completely realistic, a majority preferred the haptic setting and would recommend it to novices for training. The ‘haptic last’-group who improved their performance with the addition of haptics displayed a more positive attitude towards haptic feedback than the ‘haptic first’-group, with nine of 13 recommending the haptic setting for novices. It is likely that this shows performance influence since a small majority in the ‘haptic first’-group found the settings equally good, in agreement with that their performance did not improve during the last five attempts. This is in contrast to Våpenstad et al. who found that the surgeons preferred the non-haptic system [Citation20]. However, in the Våpenstad study, other instrument handles and older software for the haptic feedback with LapSim® VRS were used, indicating that the quality of the haptic feedback in the latest LapSim® Haptic System is now enhanced compared to previous systems.
In spite of the perceived limited sense of touch, a significantly better performance score for the parameter most sensitive to force, maximum stretch damage was seen with haptic feedback enabled, for both groups (). This is of importance since this parameter describes, on a linear scale, how much the surgeon tears the tissue when performing the stitching. Thus, 100% represent >21 mm deviation from the optimal stitch position and possible tearing of tissue, 50% represent >15 mm deviation and 0% represent <10 mm stretch by the stitch. With haptic feedback enabled, better scores were seen. The ‘haptic last’-group improved their individual scores when haptic feedback was enabled, while the ‘haptic first’-group maintained theirs. There was no difference in performance level between the two groups when performing with haptic feedback. This could indicate that haptics ‘guide’ the surgeon to more precise needle movements and thereby reduce the tearing of tissue and have a positive effect on performance right from the start.
Moreover, only four out of 26 surgeons ‘passed’ the suturing task in the first five attempts and another four managed the task in their last five attempts regardless of whether haptics were added or not. If this finding was due to the unfamiliar simulator environment or a lack of intracorporeal suturing skills is unknown. Even for experienced surgeons, as in the present investigation in which 22 of 26 previously had performed laparoscopic suturing, suturing may not be part of the participants’ daily surgical routine. Studies investigating the surgeons’ sense of touch during laparoscopy have revealed that this is quite subtle, but it could still help the surgeon to apply the appropriate tension [Citation19,Citation21,Citation22]. Too much haptic feedback could on the other hand lead to a negative training effect [Citation6,Citation10,Citation23].
In a previous study, novices acquired a predetermined proficiency level of skills 32% faster with 3 D vision and haptic feedback enabled than without neither 3 D nor haptic feedback [Citation15]. The results from the present study suggest that haptic feedback in itself plays a role to aid surgeons to apply proper force to the tissue when practicing intracorporeal suturing. Salkini et al. and Thompson et al. on the other hand found no beneficial effect at all of haptic feedback, while Ström et al. found that haptic feedback in VRS had a transfer effect [Citation11,Citation24,Citation25]. However, there were important differences between these studies. In the study by Ström et al. all participants were novices and they benefitted from haptic feedback in the early learning phase while, in contrast, experts in the current study already should have passed the initial learning phase. The studies of Salkini et al. and Thompson et al. were conducted on a different VRS with a different haptic technology, LapMentorTM II (3 D Systems, Littleton, CO, USA), whereas Ström et al. also had a different haptic setup compared to the current study [Citation11,Citation24,Citation25]. A recent study by Våpenstad et al. found a negative training effect for transfer to the operating theatre when combining LapSim® with Xitact® haptic handles (Mentice, Gothenburg, Sweden) [Citation10]. Comparisons between different simulator setups are difficult to make, since there is an on-going development in the field. The commercially available simulators are at present not comparable to those used in studies performed just a few years ago [Citation8,Citation26,Citation27]. Further, one LapSim® study is not easily comparable to another since haptic setups may differ [Citation10,Citation16,Citation20].
In other studies, investigating user experience of VRS, surgical residents preferred porcine models or high fidelity synthetic models to VRS [Citation28–31]. However, these studies used VRS without haptic feedback. Expert opinion is important when new VRS are released since novices are unfamiliar with the true sense of touch and texture doing laparoscopic surgery.
Strengths and limitations
The suturing task is an advanced laparoscopic task that offers a good opportunity to study the haptic feedback settings in the VRS. The suturing task and particular level of difficulty has been used in previous studies showing transfer to the operating room, though without haptic feedback [Citation12]. The crossover study design provided unbiased estimates for the difference between the two groups. A limitation of this study was the relatively small group of participants, with only 13 in each group and four were excluded from rating the experienced sense of touch from haptic feedback due to lack of suturing experience, leaving only 22 participants left for this part. There were no statistical differences between the groups, but five of the six surgeons who had performed over 1000 laparoscopic procedures were randomized in the ‘haptic first’-group. A sub analysis of the surgeons with more than 1000 procedures was performed and no statistical difference on the evaluated parameters was found. However, lack of evidence for a difference is not evidence that differences might have been found if the numbers had been larger. Potential confounding factors are that only six individuals had this large experience. Furthermore, the group with experience of between 100 – 1000 procedures might be heterogenous, with some having done 101 and others 999 laparoscopic operations. A 3-point Likert scale was chosen to ‘force’ the surgeons to clearly state if they perceived the haptic feedback to be completely realistic or not. More important, open-ended questions revealing descriptions on what aspects they found realistic or unrealistic would have given more in-depth information concerning their opinions.
The use of a time cap of three minutes per trial and a number of five trails per setup inherently prohibits us to know the true time needed to complete and pass the suturing task. To what extent this failure for many of the participants affected their opinion on the simulator is unclear, but no significant difference was found in ratings between the haptic and non-haptic setting based on passing the task or not.
This study evaluated expert opinion of the latest LapSim® Haptic System, with 3 D vision and haptic feedback. Future studies are suggested to compare this version of VRS to other VRS with haptic feedback (i.e LapMentorTM), video box trainers, augmented VRS (i.e ProMISTM) or hybrid systems (i.e Simball® Box, TrEndo, VBLaST©) to further investigate the added value of haptic feedback [Citation25,Citation32–35]. Research should also aim to evaluate the transfer effect from acquired skills in haptic simulators to the operating room to ensure that no negative effects of haptic feedback occur.
Conclusion
The surgeons performed significantly better causing less stretch damage with haptic feedback enabled. However, the haptic feedback feature in this 3 D VR simulator has limited fidelity according to the tested surgeons’ opinion. Despite the limited perception of haptic feedback, and when blinded, a small majority preferred the setting with haptic feedback for educational purposes in novices. This implies that not only novices could benefit from haptic feedback and that it gives no disadvantage in the VR simulator investigated.
Declaration of interest
Drs. Anderberg, Bergenfelz, Ekelund, Hagelsteen and Johansson have no conflicts of interest or financial ties to disclose. This statement covers all parts of the study and includes no attachment, in any aspect, to the manufacturers of LapSim®. Surgical Science Sweden AB provided technical support for the VRS, but had no influence on financing, design, data analysis and interpretation of the results and on the content of the manuscript.
MITAT-2018-0087.R1_Appendix_final_version.docx
Download MS Word (21.6 KB)Acknowledgements
The authors would like to thank administrative and surgeons on staff at the Skåne University Hospital for making the study possible. The authors would also like to thank Fredrik Nilsson for statistical calculations and Surgical Science for technical support with the VRS.
Additional information
Funding
References
- Dehabadi M, Fernando B, Berlingieri P. The use of simulation in the acquisition of laparoscopic suturing skills. Int J Surg. 2014;12:258–268.
- Orzech N, Palter VN, Reznick RK, et al. A comparison of 2 ex vivo training curricula for advanced laparoscopic skills: a randomized controlled trial. Ann Surg. 2012;255:833–839.
- Zhou M, Tse S, Derevianko A, et al. Effect of haptic feedback in laparoscopic surgery skill acquisition. Surg Endosc. 2012;26:1128–1134.
- McDougall EM, Kolla SB, Santos RT, et al. Preliminary study of virtual reality and model simulation for learning laparoscopic suturing skills. J Urol. 2009;182:1018–1025.
- Westebring-van der Putten EP, Goossens RH, Jakimowicz JJ, et al. Haptics in minimally invasive surgery-a review. Minim Invasive Ther Allied Technol. 2008;17:3–16.
- Coles TR, Meglan D, John NW. The role of haptics in medical training simulators: a survey of the state of the art. IEEE Trans Haptics. 2011;4:51–66.
- Buzink SN, Goossens RH, De Ridder H, et al. Training of basic laparoscopy skills on SimSurgery SEP. Minim Invasive Ther Allied Technol. 2010;19:35–41.
- Vapenstad C, Hofstad EF, Bo LE, et al. Limitations of haptic feedback devices on construct validity of the LapSim® virtual reality simulator. Surg Endosc. 2013;27:1386–1396.
- Chmarra MK, Dankelman J, van den Dobbelsteen JJ, et al. Force feedback and basic laparoscopic skills. Surg Endosc. 2008;22:2140–2148.
- Vapenstad C, Hofstad EF, Bo LE, et al. Lack of transfer of skills after virtual reality simulator training with haptic feedback. Minim Invasive Ther Allied Technol. 2017;26:346–354.
- Strom P, Hedman L, Sarna L, et al. Early exposure to haptic feedback enhances performance in surgical simulator training: a prospective randomized crossover study in surgical residents. Surg Endosc. 2006;20:1383–1388.
- Ahlberg G, Enochsson L, Gallagher AG, et al. Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg. 2007;193:797–804.
- Duffy AJ, Hogle NJ, McCarthy H, et al. Construct validity for the LAPSIM laparoscopic surgical simulator. Surg Endosc. 2005;19:401–405.
- van Dongen KW, Tournoij E, van der Zee DC, et al. Construct validity of the LapSim: can the LapSim virtual reality simulator distinguish between novices and experts?. Surg Endosc. 2007;21:1413–1417.
- Fairhurst K, Strickland A, Maddern G. The LapSim virtual reality simulator: promising but not yet proven. Surg Endosc. 2011;25:343–355.
- Hagelsteen K, Langegard A, Lantz A, et al. Faster acquisition of laparoscopic skills in virtual reality with haptic feedback and 3D vision. Minim Invasive Ther Allied Technol. 2017;26:269–277.
- Sorensen SMD, Konge L, Bjerrum F. 3D vision accelerates laparoscopic proficiency and skills are transferable to 2D conditions: a randomized trial. Am J Surg. 2017;214:63–68.
- R Core Team. (2017). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2017.
- Lamata P, Gomez EJ, Sanchez-Margallo FM, et al. Tissue consistency perception in laparoscopy to define the level of fidelity in virtual reality simulation. Surg Endosc. 2006;20:1368–1375.
- Vapenstad C, Hofstad EF, Lango T, et al. Perceiving haptic feedback in virtual reality simulators. Surg Endosc. 2013;27:2391–2397.
- Bholat OS, Haluck RS, Murray WB, et al. Tactile feedback is present during minimally invasive surgery. J Am Coll Surg. 1999;189:349–355.
- Picod G, Jambon AC, Vinatier D, et al. What can the operator actually feel when performing a laparoscopy? Surg Endosc. 2005;19:95–100.
- van der Meijden OA, Schijven MP. The value of haptic feedback in conventional and robot-assisted minimal invasive surgery and virtual reality training: a current review. Surg Endosc. 2009;23:1180–1190.
- Thompson JR, Leonard AC, Doarn CR, et al. Limited value of haptics in virtual reality laparoscopic cholecystectomy training. Surg Endosc. 2011;25:1107–1114.
- Salkini MW, Doarn CR, Kiehl N, et al. The role of haptic feedback in laparoscopic training using the LapMentor II. J Endourol. 2010;24:99–102.
- Pinzon D, Byrns S, Zheng B. Prevailing trends in haptic feedback simulation for minimally invasive surgery. Surg Innov. 2016;23:415–421.
- Schijven M, Jakimowicz J. Virtual reality surgical laparoscopic simulators. Surg Endosc. 2003;17:1943–1950.
- Shetty S, Zevin B, Grantcharov TP, et al. Perceptions, training experiences, and preferences of surgical residents toward laparoscopic simulation training: a resident survey. J Surg Educ. 2014;71:727–733.
- Botden SM, Buzink SN, Schijven MP, et al. Augmented versus virtual reality laparoscopic simulation: what is the difference? A comparison of the ProMIS augmented reality laparoscopic simulator versus LapSim virtual reality laparoscopic simulator. World J Surg. 2007;31:764–772.
- Madan AK, Frantzides CT, Tebbit C, et al. Participants' opinions of laparoscopic training devices after a basic laparoscopic training course. Am J Surg. 2005;189:758–761.
- Palter VN, Orzech N, Aggarwal R, et al. Resident perceptions of advanced laparoscopic skills training. Surg Endosc. 2010;24:2830–2834.
- Zhang L, Grosdemouge C, Arikatla VS, et al. The added value of virtual reality technology and force feedback for surgical training simulators. Work. 2012;41: 2288–2292.
- Hagelsteen K, Sevonius D, Bergenfelz A, et al. Simball box for laparoscopic training with advanced 4D motion analysis of skills. Surg Innov. 2016;23:309–316.
- Botden SM, Buzink SN, Schijven MP, et al. ProMIS augmented reality training of laparoscopic procedures face validity. Simul Healthc. 2008;3:97–102.
- Chmarra MK, Grimbergen CA, Dankelman J. Systems for tracking minimally invasive surgical instruments. Minim Invasive Ther Allied Technol. 2007;16:328–340.