Abstract
Objective: It has been hypothesised that clinically important age-related differences between adults with anxiety disorders exist; this study aims to elucidate these differences.
Methods: We analysed data from 1950 outpatients diagnosed with DSM-IV-TR anxiety disorders treated at a Dutch hospital or affiliated mental healthcare centres. Three age-groups (young- (18–25; n = 435), mid- (26–40; n = 788) and older adult (41–65; n = 727)) were compared with regard to social demographic characteristics, diagnostic characteristics, anxiety symptom profile, general psychiatric symptom profile and generic health status, in addition, linear analyses were carried out with age as a continuous variable.
Results: Average age was 36.48 years (SD 11.71), 62.8% were female. Significant associations with age emerged for gender, employment, education level, living situation, observed depression, agoraphobia (AP), social phobia, aches and pains, inner tension, sleep, interpersonal sensitivity, observed hostility, physical functioning, role limitations due to physical problems, vitality and bodily pain in categorical and continuous analyses. Self reported hostility was only significant in group-wise comparisons; role limitations due to emotional problems were only significant in linear analyses (all at p < .001).
Conclusions: This study identified clinically relevant differences between younger and older adult outpatients with anxiety disorders. Clinicians should take these findings into account, as they may support treatment.
Objective
Adult psychiatry is generally regarded as a uniform concept, with homogenous treatment protocols and guidelines. However, between an 18-year old and a 60-year old diagnosed with an anxiety disorder, numerous differences may exist. Age related differences in the adult population might, for example, be related to changes in physical health associated with aging. In addition, social demographic cohort differences impacting emotionality, such as lower education levels and related competitive disadvantages in the labour market among older subjects, could exist (Schieman et al. Citation2001). Finally, possibly relevant differences between life phases exist: During ages 18–25, achieving social, psychological and financial independence are central. Ages 26 through 40, are marked by growing responsibilities associated with career development and family planning. During ages 41 through 65, interests shift to social responsibility, caregiving duties, helping the next generation and adjusting to approaching retirement and post-work identity (Wong et al. Citation2015). Altogether, these physical changes, cohort differences and life phases may impact the phenomenology of anxiety disorders, which in turn may require different diagnostic and therapeutic approaches from health care professionals (Schneider et al. Citation2004; Husain et al. Citation2005).
To date, however, the phenomenology of anxiety across the adult life span has not been studied extensively. Therefore, this study explored age-related differences in anxiety disorders. We focused on outpatients diagnosed with (DSM-IV-TR) (American Psychiatric Association Citation2000) panic disorder (with or without agoraphobia) (PD), agoraphobia (without panic) (AP), social phobia (SP) and generalised anxiety disorder (GAD). We compared data on a broad set of social demographic, clinical and functional characteristics. With regard to social demographic characteristics, on average, we expected older patients to have lower education levels, to more often live with a partner and to be employed less often. Based on previous findings in depression (Husain et al. Citation2005; Wilkowska-Chmielewska et al. Citation2013), and on comparisons between adult subjects with anxiety disorders with child- and adolescent and geriatric subjects, respectively (Wolitzky-Taylor et al. Citation2010; Lenze & Wetherell Citation2011), several hypotheses with regard to clinical characteristics could be formulated: we hypothesised more panic in younger patients (Wolitzky-Taylor et al. Citation2010) and more drug abuse in younger subjects (Husain et al. Citation2005). With regard to symptom presentation we expected more irritability in younger patients (Husain et al. Citation2005; Lenze & Wetherell Citation2011; Wilkowska-Chmielewska et al. Citation2013), more anhedonia in younger patients (Wilkowska-Chmielewska et al. Citation2013), and more health-related worry in older patients (Husain et al. Citation2005; Wolitzky-Taylor et al. Citation2010; Lenze & Wetherell Citation2011). In addition, we expected older patients to have more physical complaints, more sleep problems, less vitality and more pain (Husain et al. Citation2005; Lenze & Wetherell Citation2011). In order to fully explore associations with age, we examined age-related differences allowing for non-linear associations, as well as linear associations. This study is the first to examine age related differences among adults with anxiety disorders. Findings may help clinicians better adapt treatment to the needs of individual patients.
Methods
Routine outcome monitoring
As part of routine practice at the facilities involved in this study, all patients completed an extensive battery of self-report and observer-rated measures at intake. This procedure is known as routine outcome monitoring (ROM), and is described in more detail by De Beurs et al. (Citation2011). Both generic and disorder-specific questionnaires were administered by trained psychiatric nurses and through supervised computerised self-report which prevented missing data within questionnaires. Although participation in ROM is voluntary, inclusion is high with an estimated 80% of all patients being assessed at intake (van Noorden et al. Citation2011; Zitman Citation2012). Although the primary goal of ROM is to inform both clinicians and patients, data were anonymised and their use in scientific research was approved by the Ethical Review Board at the Leiden University Medical Centre (LUMC).
Patients and procedure
Subjects were outpatients who had been referred for treatment by their general practitioner to Rivierduinen, a regional mental healthcare provider, or the psychiatry department of the LUMC between January 2004 and October 2010. Inclusion criteria held that patients must be between ages 18 and 65, have adequate command of the Dutch language and meet DSM-IV-TR diagnostic criteria for one or more of the following disorders: PD, AP, SP or GAD; with moderate to severe anxiety. Moderate to severe anxiety severity was assessed using a self-report as well as an observational measure: the Dutch versions of the Brief Symptom Inventory-12 item version (BSI-12) (Roy-Byrne et al. Citation2010), a self-report anxiety measure derived from the BSI (Derogatis & Melisaratos Citation1983; De Beurs & Zitman Citation2006) and the observer-rated Brief Anxiety Scale (BAS) (Tyrer et al. Citation1984) (see ‘Measures’ section). Moderate to severe baseline severity was defined as ≥10.38 on the BAS (Tyrer et al. Citation1984; Schat et al. Citation2013), equalling the average BAS score in a group of general practice patients diagnosed with anxiety disorders (Tyrer et al. Citation1984), and ≥6 on the BSI-12 (Schat et al. Citation2013), with scores <6 signifying no- to mild anxiety (Roy-Byrne et al. Citation2010). Missing data resulting from the incidental failure to administer complete questionnaires and from large time intervals between administrations of questionnaires served as exclusion criteria.
Measures
In addition to patients’ age and gender, education level (low: primary-lower secondary versus high: higher secondary-university), living situation (with versus without partner), and employment status (full- or part-time employed versus unemployed) were assessed. The Dutch version of the MINI International Neuropsychiatric Interview-Plus (MINI-Plus) (Sheehan et al. Citation1998; Van Vliet & De Beurs Citation2007) was used to collect diagnostic information. The MINI-Plus has good psychometric properties (Lecrubier et al. Citation1997), and was used to determine the presence of DSM-IV-TR anxiety disorders, comorbid depressive or dysthymic disorders, alcohol abuse or -dependence and drug abuse or -dependence. The number of comorbid anxiety disorders (including comorbid specific phobia) was dichotomised into ‘single anxiety disorder’ versus ‘multiple anxiety disorders.’ Anxiety symptoms were assessed using the BAS (Tyrer et al. Citation1984). The BAS is a 10-item observer-rated scale, derived from the abbreviated Comprehensive Psychopathological Rating Scale (CPRS) (Asberg et al. Citation1978; Goekoop et al. Citation1992). The total score equals the sum-score of all 10 items on a 7-point Likert scale (0–6) (range 0–60). The BAS assesses the main components of all anxiety disorders, covering psychological and somatic components, a higher score corresponds to more severe anxiety. The 25-item CPRS, besides measuring anxiety on the BAS, also measures depressive symptoms (Montgomery–Åsberg Depression Rating Scale, MADRS) with 10 items. Items are measured on a 7-point Likert scale (0–6) and add up to a total score (range 0–60), with higher scores indicating more severe symptoms. The MADRS has good internal consistency with Cronbach’s alpha equalling 0.86 (Montgomery & Asberg Citation1979). The BSI (Derogatis & Melisaratos Citation1983; De Beurs & Zitman Citation2006) was used to assess a general psychiatric symptom profile. The BSI is a self-report measure consisting of 53 items on a 5-point Likert scale (0–4) (range 0–48). A total of nine subscales (somatisation, obsessive compulsive symptoms, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism) can be obtained by averaging the corresponding items. Generic health status was examined using the Dutch version of the Short Form-36 (SF-36) (Ware & Sherbourne Citation1992; Aaronson et al. Citation1998), a 36-item self-report survey screening eight domains of general health: physical functioning, social functioning, role limitations due to physical health problems, role limitations due to emotional problems, general mental health perception, vitality, bodily pain, and general health perception. Measurement scales vary per subscale, ranging from yes/no to answers on a 3-, 5- or 6-point Likert scale. All raw scores are linearly converted to 0–100 subscales, with higher scores representing higher levels of functioning or wellbeing. However, to facilitate comparability to other measures, SF-36 scores were inverted so that higher scores reflect poorer generic health.
Statistical analyses
Categorical characteristics are presented as number (percentage), continuous variables are presented as mean (M) (±SD). Comparisons between included and excluded patients were made using χ2 for categorical and independent samples t-tests for continuous variables. Based on previous studies, patients were divided into three cohorts: age 18–25; 26–40 and 41–65 (Robins et al. Citation1984; Regier et al. Citation1990; Somers et al. Citation2006; van Noorden et al. Citation2011). Age-groups were compared with regard to demographic variables, diagnostic variables, anxiety symptom profile (BAS), general psychiatric symptom profile (BSI) and generic health status (SF-36). Comparisons between the three age-groups were made using χ2 or ANOVA for categorical and continuous variables respectively, with pair-wise post-hoc comparisons. For overall comparisons Cramer’s V or Eta squared were calculated, for pair-wise post-hoc comparisons, phi and Cohen’s d were computed. To test whether associations fitted a linear shape, in addition, all variables were examined in linear regression. Significance level was set at p < .05; Bonferroni correction for multiple testing was applied. Data were analysed using SPSS version 20.0 (IBM Corp., Armonk, NY).
Results
Sample characteristics
Between January 2004 and October 2010, a total of 2214 patients met DSM-IV-TR diagnostic criteria for PD, AP, SP and GAD with at least moderate severity. 264 patients (11.9%) had to be excluded, as they had missing data, or a large time gap (more than 21 d) existed between completion of distinct questionnaires. The latter criterion was set to guarantee that all assessments had taken place at intake. Therefore, 1950 patients (88.1%) were included for analyses. Although differences between included and excluded patients with regard to BAS item ‘aches and pains,’ BSI subscales ‘cognitive distortion,’ ‘hostility,’ and ‘phobic anxiety’ and SF-36 subscale ‘bodily pain’ were significant at p < .05 after Bonferroni correction, these differences were very small, with eta squared ranging from 0.001 to 0.01 (results not shown). Of the total sample, 62.8% was female, mean age was 36.48. A total of 816 patients (42%) was diagnosed with PD, 433 (22%) patients with AP, 586 patients (30%) with SP, and 440 patients (23%) with GAD. Patients were divided according to age in early adult (age 18–25; n = 435), mid-adult (age 26–40; n = 788) and late adult (age 41–65; n = 727).
Differences between age-groups
Social demographic and clinical characteristics
Social demographic and clinical comparisons across the three age-groups with pairwise post-hoc analyses with Bonferroni correction as well as results for regression analyses are summarised in . Significant associations with age emerged for gender, employment, education level, living situation and comorbid depression. The percentage of men increased with age (28.0% in the early adult group, 36.5% in the mid-adult and 43.3% in the late adult group). The percentage of patients with a part-time or fulltime job decreased with age (46.6% in the early adult group, 47.0% in the mid-adult group and 37.7% in the late adult group), as did the number of patients with a high education level (65.5% in the early adult group, 60.8% in the mid-adult group and 47.9% in the late adult group). Older patients were more likely to live with a partner than younger patients (22.3% in the early adult group, 58.1% in the mid-adult group and 64.4% in the late adult group). Younger patients were less likely to have a comorbid depressive disorder (48.5% in the early adult group, 51.6% in the mid-adult group and 60.8% in the late adult group). The distribution of the four included DSM-IV-TR anxiety diagnoses (PD, AP, SP and GAD) across the three age-groups is shown in . AP was more prevalent with increasing age (17.2%) in the early adult group, 18.8% in the mid-adult group and 28.9% in the late adult group). The number of patients with SP on the other hand decreased with age (39.8% in the early adult group, 30.7% in the mid-adult group and 23.5% in the late adult group).
Figure 1. Anxiety diagnoses per age-group in 1950 outpatients diagnosed with DSM-IV-TR anxiety disorders. Anxiety diagnoses per age-group in 1950 outpatients diagnosed with DSM-IV-TR anxiety disorders (panic disorder with or without agoraphobia, agoraphobia without panic, social phobia and/or generalised anxiety disorder); DSM-IV-TR denotes Diagnostic Statistical Manual-fourth edition, text revision; *denotes significantly different from early adult (18–25; n = 435) and mid-adult (26–40; n = 788) post-hoc with Bonferroni correction for multiple testing; **denotes significantly different from early adult (18–25; n = 435) and late adult (41–65; n = 727) post-hoc with Bonferroni correction for multiple testing.
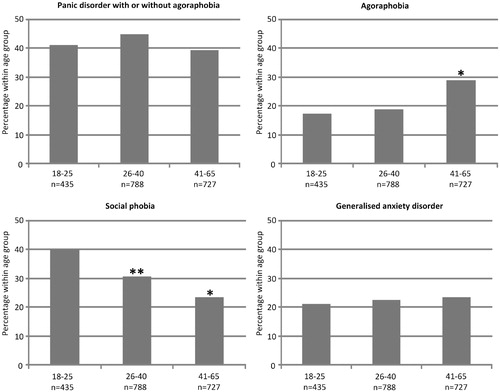
Table 1. Social demographic and clinical patient characteristics per age-group in 1950 outpatients diagnosed with DSM-IV-TR anxiety disorders.
Anxiety symptoms
Comparisons of anxiety symptoms across the three age-groups with pairwise post-hoc analyses with Bonferroni correction, as well as results for regression analyses are shown in . Significant differences between the three age-groups emerged on the items aches and pains, inner tension and reduced sleep. Complaints of aches and pains increased with age (early adult group M = 1.93, SD = 1.37; mid-adult group M = 2.09, SD = 1.45; late adult group M = 2.29, SD = 1.52), as did levels of inner tension (early adult group M = 3.03, SD = 1.00; mid-adult group M = 3.15, SD = 1.01; late adult group M = 3.29, SD = 1.00) and sleep problems (early adult group M = 1.81, SD = 1.59; mid-adult group M = 2.22, SD = 1.68; late adult group M = 2.43, SD = 1.74). Although group-wise comparisons were not statistically significant, regression analyses showed a decrease in hostility scores with age.
Table 2. Anxiety symptoms per age-group in 1950 outpatients diagnosed with DSM-IV-TR anxiety disorders.
Psychiatric symptoms
shows comparisons of psychiatric symptoms across the three age-groups with pairwise post-hoc analyses with Bonferroni correction, as well as results for regression analyses. With regard to psychiatric symptoms, significant differences between the three age-groups emerged on measures of interpersonal sensitivity, hostility and on observed depression. Levels of interpersonal sensitivity decreased with age (early adult group M = 2.06, SD = 1.08; mid-adult group M = 1.94, SD = 0.94; late adult group M = 1.73, SD = 1.06), as did levels of self-reported hostility (early adult group M = 1.18, SD = 8.30; mid-adult group M = 1.12, SD = 0.92; late adult group M = 0.95, SD = 0.85). Observed depression scores on the other hand, increased with age (early adult group M = 18.69, SD = 8.30; mid-adult group M = 20.38, SD = 8.31; late adult group M = 21.82, SD = 8.54).
Table 3. Psychiatric symptoms per age-group in 1950 outpatients diagnosed with DSM-IV-TR anxiety disorders.
Generic health status
Comparisons across the three age-groups with regard to generic health status with pairwise post-hoc analyses with Bonferroni correction, as well as results for regression analyses are summarised in . Significant differences emerged between the three age-groups with regard to physical functioning, role limitations due to physical problems, role limitations due to emotional problems, vitality and bodily pain. Physical functioning deteriorated with age (early adult group M = 20.05, SD = 20.42; mid-adult group M = 23.93, SD = 22.05; late adult group M = 30.77, SD = 24.40). Physical problems increased with age (early adult group M = 56.78, SD = 39.36; mid-adult group M = 64.78, SD = 38.48; late adult group M = 71.70, SD = 36.83), as did the level of role limitations due to emotional problems (early adult group M = 70.88, SD = 34.54; mid-adult group M = 80.16, SD = 30.43; late adult group M = 78.4, SD = 32.07). Levels of vitality decreased with age (early adult group M = 64.54, SD = 15.45; mid-adult group M = 67.26, SD = 15.93; late adult group M = 68.65, SD = 16.43), while the level of bodily pain increased with age (early adult group M = 32.77, SD = 24.38; mid-adult group M = 36.71, SD = 27.15; late adult group M = 39.95, SD = 28.22).
Table 4. Generic health status per age-group in 1950 outpatients diagnosed with DSM-IV-TR anxiety disorders.
Discussion
We identified a number of differences between the three age-groups of outpatients with anxiety disorders. A number of findings fit our hypotheses. The findings that older patients more often lived with a partner, were less often employed, and had lower education levels fit general demographics (Lutz & KC Citation2011). The finding of more physical symptoms in older patients is also in line with the process of aging (Aaronson et al. Citation1998), although it is of note that signs of significantly lower physical functioning were already observed in the mid-adult group relative to the early adult group. Possibly our results reflect the overall finding that people with anxiety disorders are at elevated risk for a number of physical conditions (Sareen et al. Citation2005) and that this risk increases with age (Brenes et al. Citation2008; Scott et al. Citation2008).
The shift in the male to female ratio towards a more equal distribution with increasing age was previously reported in the general population (Regier et al. Citation1990). With regard to anxiety diagnoses, we found a decrease in SP with age, which has also been found in the general population (Somers et al. Citation2006). AP on the other hand was more prevalent in the late adult group. This again confirms findings in the general population (Cairney et al. Citation2008), although prevalence of AP has also been found to be stable or even decline across age-groups (Somers et al. Citation2006). However, across all age-groups, mood-disorder comorbidity was common, but it was highest in the oldest group. This was not reflected in self-reported depression scores. Possibly, the increased prevalence of physical complaints with age may have inflated chances of meeting diagnostic criteria for depression. As such, the increased prevalence in our older adult group could be regarded as an artefact. Alternatively however, the older adult group may in fact have been more depressed and adequately diagnosed as such. Possibly, the absence of elevated self-report depression scores stems from a misattribution of psychiatric symptoms to general symptoms of ageing by depressed older adults (Knauper & Wittchen Citation1994). Overall, the increased prevalence of agoraphobia and mood comorbidity in older adults warrants special attention, as both have been associated with negative outcome (Angst & Vollrath Citation1991; Schat et al. Citation2013).
Both younger groups reported more interpersonal sensitivity and hostility. These may have emerged from the demands that are typically made of the younger age-groups, which may have a stronger social component, for example, in achieving independence, possible student life, dating and career development. In addition, increased interpersonal sensitivity fits our findings of higher prevalence of SP in the younger age-groups, although feelings of hostility do not. Interestingly, young adult patients’ hostility scores, which were measured through a subscale on the self-report BSI, as well as an item on the observer-rated BAS, were elevated only on the self-report measure, perhaps the single item of the BAS lacked sensitivity to detect the variation in hostility.
Our study has several strengths. To our knowledge, it is the first study to report on age-related characteristics of anxiety disorders across the ages 18 through 65. Furthermore, as we examined outpatients using data from a large, representative naturalistic sample, we ensured applicability to clinical practice. The inclusion of a broad set of patient characteristics further strengthens our study. However, several potential limitations exist. As our study was explorative in nature, we used unsubstantiated cut-offs to define the age-groups. Although our cut-offs have been used previously (Regier et al. Citation1990; Robins et al. Citation1984; Somers et al. Citation2006; van Noorden et al. Citation2011), alternative cut-offs may better fit the research question. Second, no information on primary diagnosis or physical comorbidity was available in our sample. In addition, it must be noted that although differences between groups were significant after correction for multiple testing, effect sizes indicated that differences were generally small. This does not imply they are not clinically important, but it does warrant moderation when interpreting results. Finally, we studied an outpatient group, therefore, our results may not generalise to inpatients or the general population.
In conclusion, our study has convincingly demonstrated that significant age related differences exist among outpatients with anxiety disorders. Although a number of these differences fit expectations related to development across the adult lifespan, these may still be of clinical relevance, as they relate to needs felt by patients and demands made of them. The finding of increased observed but not self-reported depression in the older adult group merits special attention in clinical practice as well as in future research. Similarly, elevated feelings of hostility and interpersonal sensitivity among younger adults, possibly reflecting strong social demands that are made of them, should be taken into account. Clinicians should be aware of these differences when providing treatment.
Acknowledgements
The authors would like to gratefully acknowledge the research nurses at Rivierduinen and the Leiden University Medical Centre involved in data collection for this study.
Disclosure statement
None to declare.
References
- Aaronson NK, Muller M, Cohen PDA, Essink-Bot ML, Fekkes M, Sanderman R, Sprangers MAG, Te velde A, Verrips E. 1998. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 51:1055–1068.
- American Psychiatric A. 2000. Diagnostic and statistical manual of mental disorders. 4th ed. Text Revision (DSM-IV-TR). Washington (DC): American Psychiatric Association.
- Angst J, Vollrath M. 1991. The natural history of anxiety disorders. Acta Psychiatr Scand. 84:446–452.
- Asberg M, Montgomery SA, Perris C, Schalling D, Sedvall G. 1978. Comprehensive psychopathological rating-scale. Acta Psychiatr Scand. 57:5–27.
- Brenes GA, Penninx BW, Judd PH, Rockwell E, Sewell DD, Wetherell JL. 2008. Anxiety, depression and disability across the lifespan. Aging Ment Health. 12:158–163.
- Cairney J, Corna LM, Veldhuizen S, Herrmann N, Streiner DL. 2008. Comorbid depression and anxiety in later life: patterns of association, subjective well-being, and impairment. Am J Geriatr Psychiatry. 16:201–208.
- De Beurs E, den Hollander-Gijsman ME, van Rood YR, van der Wee NJA, Giltay EJ, van Noorden MS, van der Lem R, van Fenema E, Zitman FG. 2011. Routine outcome monitoring in the Netherlands: practical experiences with a web-based strategy for the assessment of treatment outcome in clinical practice. Clin Psychol Psychother. 18:1–12.
- De Beurs E, Zitman FG. 2006. De Brief Symptom Inventory (BSI) De betrouwbaarheid van een handzaam alternatief voor de SCL-90. Maandblad Geestelijke Volksgezondheid. 61:120–141.
- Derogatis LR, Melisaratos N. 1983. The brief symptom inventory: an introductory report. Psychol Med. 13:595–605.
- Goekoop JG, Hoeksema T, Knoppert van der Klein EAM, Klinkhamer RA, Vangaalen HAE, Vanlonden L, Deweme R, Zwinderman AH. 1992. Multidimensional ordering of psychopathology – a factor-analytic study using the comprehensive psychopathological rating-scale. Acta Psychiatr Scand. 86:306–312.
- Husain MM, Rush AJ, Sackeim HA, Wisniewski SR, McClintock SM, Craven N, Holiner J, Mitchell JR, Balasubramani GK, Hauger R. 2005. Age-related characteristics of depression: a preliminary STAR*D report. Am J Geriatr Psychiatry. 13:852–860.
- Knauper B, Wittchen HU. 1994. Diagnosing major depression in the elderly: evidence for response bias in standardized diagnostic interviews? J Psychiatr Res. 28:147–164.
- Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, Janavs J, Dunbar GC. 1997. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. 12:224–231.
- Lenze EJ, Wetherell JL. 2011. A lifespan view of anxiety disorders. Dialogues Clin Neurosci. 13:381–399.
- Lutz W, KC S. 2011. Global human capital: integrating education and population. Science. 333:587–592.
- Montgomery SA, Asberg M. 1979. A new depression scale designed to be sensitive to change. Br J Psychiatry. 134:382–389.
- Regier DA, Narrow WE, Rae DS. 1990. The epidemiology of anxiety disorders: the Epidemiologic Catchment Area (ECA) experience. J Psychiatr Res. 24:3–14.
- Robins LN, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, Burke JD Jr, Regier DA. 1984. Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry. 41:949–958.
- Roy-Byrne P, Craske MG, Sullivan G, Rose RD, Edlund MJ, Lang AJ, Bystritsky A, Welch SS, Chavira DA, Golinelli D, et al. 2010. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 303:1921–1928.
- Sareen J, Houlahan T, Cox BJ, Asmundson GJ. 2005. Anxiety disorders associated with suicidal ideation and suicide attempts in the National Comorbidity Survey. J Nerv Ment Dis. 193:450–454.
- Schat A, van Noorden MS, Noom MJ, Giltay EJ, van der Wee NJ, Vermeiren RR, Zitman FG. 2013. Predictors of outcome in outpatients with anxiety disorders: the Leiden routine outcome monitoring study. J Psychiatr Res. 47:1876–1885.
- Schieman S, Van GK, Taylor J. 2001. Status, role, and resource explanations for age patterns in psychological distress. J Health Soc Behav. 42:80–96.
- Schneider G, Driesch G, Kruse A, Wachter M, Nehen HG, Heuft G. 2004. What influences self-perception of health in the elderly? The role of objective health condition, subjective well-being and sense of coherence. Arch Gerontol Geriatr. 39:227–237.
- Scott KM, Von Korff M, Alonso J, Angermeyer M, Bromet EJ, Bruffaerts R, de Girolamo G, de Graaf R, Fernandez A, Gureje O, et al. 2008. Age patterns in the prevalence of DSM-IV depressive/anxiety disorders with and without physical co-morbidity. Psychol Med. 38:1659–1669.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. 1998. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatr. 59:22–33.
- Somers JM, Goldner EM, Waraich P, Hsu L. 2006. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 51:100–113.
- Tyrer P, Owen RT, Cicchetti DV. 1984. The brief scale for anxiety – a subdivision of the comprehensive psychopathological rating-scale. J Neurol Neurosurg Psychiatry. 47:970–975.
- van Noorden MS, Minkenberg SE, Giltay EJ, den Hollander-Gijsman ME, van Rood YR, van der Wee NJ, Zitman FG. 2011. Pre-adult versus adult onset major depressive disorder in a naturalistic patient sample: the Leiden routine outcome monitoring study. Psychol Med. 41:1407–1417.
- Van Vliet IM, De Beurs E. 2007. Het MINI Internationaal Neuropsychiatrisch Interview (MINI) een kort gestructureerd diagnostisch psychiatrisch inerview voor DSM-IV- en ICD-10-stoornissen. Tijdschrift voor Psychiatrie. 49:393–397.
- Ware JE, Sherbourne CD. 1992. The Mos 36-Item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection . Med Care. 30:473–483.
- Wilkowska-Chmielewska J, Szelenberger W, Wojnar M. 2013. Age-dependent symptomatology of depression in hospitalized patients and its implications for DSM-5. J Affect Disord. 150:142–145.
- Wolitzky-Taylor KB, Castriotta N, Lenze EJ, Stanley MA, Craske MG. 2010. Anxiety disorders in older adults: a comprehensive review. Depress Anxiety. 27:190–211.
- Wong DW, Hall KH, Justice CA, Wong-Hernandez LW. 2015. Chapter 1, Human development through the lifespan. Counseling individuals through the lifespan. Thousand Oaks (CA): Sage Publications Inc.
- Zitman FG. 2012. [ROM in mood, anxiety and somatoform disorders: a promising technique with pleasing results]. Tijdschrift Voor Psychiatrie. 54:173–177.
