Abstract
Objective
The objective of this study was to explore the determinants of adherence in the EFFORT-D (EFFect Of Running Therapy) study in a specialised mental health care hospital setting.
Methods
Patients with major depressive disorder (MDD) were given treatment as usual and half were randomised to an exercise intervention. Adherence was measured at 3 months (T3) and 6 months (T6) and was defined as participation in the overall study protocol (total n = 42, adhered n = 28) or intervention (total n = 24, adhered n = 9). Potential determinants were age, BMI, tobacco and alcohol use, severity of depression, anxiety, fitness (VO2max kg−1 and Wmax kg−1) and personality traits at baseline. ANOVA, Chi-square tests and block-wise logistic regression were performed, and reliability of the scales was determined.
Results
Numbers were found too low for analyses on smoking, drinking and anxiety. Higher agreeableness was significantly associated with better adherence to the overall study protocol (OR 1.2; p = 0.03; 95% CI: 1.01–1.4) and severity of depression was negatively associated with adherence in the intervention group (OR 0.70; p = 0.046;95% CI: 0.49–0.99).
Conclusions
To adhere to a study protocol involving exercise or to a clinical exercise programme, MDD patients need substantial personal support. Measurement of personality traits and the severity of depression as potential predictors of adherence could be considered for this purpose.
Adherence to exercise and study protocols in a randomised controlled trial was low
Patients with severe major depressive disorder need substantial personal support
Measurement of personality traits could be considered
Keypoints
Introduction
Poor adherence or non-adherence to prescribed medication is a worldwide problem, with rates as high as 50% in developed countries (World Health Organisation) (Sabate Citation2003). Adherence is defined as ‘the process in which a person follows rules, guidelines, or standards, especially as a patient follows a prescription and recommendations for a regimen of care’ (Mosby's Dictionary of Medicine, Nursing & Health Professions Citation2013). In patients with major depressive disorder (MDD), medication is frequently prescribed, but adherence is low (21–41%) (Keyloun et al. Citation2017). In this population, poor adherence is associated with higher medical costs (Cantrell et al. Citation2011) and an increased risk of mortality (Krivoy et al. Citation2016). Relatively few studies on the treatment of affective disorders have focussed on adherence problems in MDD (Lingam and Scott Citation2002). A narrative review of depressed older patients (Zivin and Kales Citation2008) reported the following determinants of adherence to depression treatment: co-morbid anxiety, substance use, cognitive status, polypharmacy, medical co-morbidity, social support, costs of treatment, gender and race.
Besides medication, MDD of inpatients could in theory be treated with an add-on exercise regime (Kruisdijk et al. Citation2012). However, poor adherence to the intervention and to the study protocol has also been reported in exercise trials. Several authors analysed drop-out and poor adherence in their studies with the aim of identifying factors determining adherence to exercise in MDD patients. They identified the following determinants of non-adherence: anxiety (higher)(Herman et al. Citation2002), age (higher) (Krogh et al. Citation2014) baseline severity of MDD (higher) (Busch et al. Citation2016), tobacco use (smoking) and alcohol consumption (hazardous drinking) and work flexibility (less flexible) (Helgadottir et al. Citation2018).
In our study of the EFFORT-D (Effect of Running Therapy in Depression) randomised controlled trial (Kruisdijk et al. Citation2012), we also observed high levels of drop-out and poor adherence to the exercise intervention. In a separate qualitative process evaluation, we described several factors that influenced the results of the EFFORT-D trial (Kruisdijk et al. Citation2018): the observed poor adherence was associated with the severity of MDD, low motivation and the duration of the intervention.
Personality traits may also influence adherence to therapy and other interventions. However, no studies have yet addressed personality traits as possible determinants of therapy and study adherence in MDD exercise interventions. If this association was shown, this could lead to more effective interventions by selecting patients who would benefit from more support.
We found a Japanese study that describes the relationships of exercise adherence and personality factors in a (general) hospital medical fitness (MF) programme (Yamashita et al. Citation2017). They report that: ‘In persons with subjective exercise adherence, “Conscientiousness” was significantly lower (p = 0.003) among men and “Neuroticism” was significantly higher (p = 0.018) among women when compared to persons with subjective exercise adherence”. Their conclusion is among others that ‘It is essential to consider personality and gender differences when devising exercise adherence support measures for the MF program’. Also, Courneya et al. (Citation2002) describe exercise adherence in cancer survivors using a personality factor model and the theory of planned behaviour model. They find that independent predictors were sex, extraversion, normative beliefs, and perceived behavioural control. So, the role of personality factors on (exercise) adherence remains still unclear.
Since antiquity, personality traits have been assumed to be linked with mental disorders (Kotov et al. Citation2010), but consensus on personality taxonomy began to emerge only in the 1980s. One important model consisted of hierarchically ordered traits (Goldberg Citation1993), leading to the ‘Big Five model’ of personality traits: Neuroticism, Extraversion, Agreeableness, Openness and Conscientiousness (McCrae and Costa Citation1987). These personality traits are assumed to have a solid genetic base (Lewis and Bates Citation2014). Moreover, the five factors were proven to be stable during adulthood (Costa and McCrae Citation1994), over a lifespan of 50 years (Judge et al. Citation1999) and across cultures and languages (McCrae Citation2001). This genetic and psychological stability of the Big Five model enabled investigation of the expected response of patients in various therapies. Low neuroticism and high conscientiousness, for instance, have been associated with better therapy outcomes (Miller Citation1991). Lower conscientiousness has been associated with a poor therapy response, whereas lower agreeableness was shown to reflect scepticism and antagonistic tendencies in patients, leading to uncooperative behaviour that frustrated the therapy (Hoekstra et al. Citation2007). A study of patients with MDD suggested that neuroticism is affected by depressive states and by anxiety states (Lewis et al. Citation2014). Another study showed that extraversion and conscientiousness are affected by depressive disorders, but not by anxiety disorders, and that agreeableness and openness are influenced by neither (Karsten et al. Citation2012).
We therefore analysed adherence in the EFFORT-D study with a quantitative statistical approach based on the ‘Big Five’ model of personality traits. To the best of our knowledge, this is the first time that personality traits have been investigated in relation to adherence in patients with MDD who were treated with an exercise intervention.
Aims of the study
To explore possible determinants of adherence, we analysed two aspects of adherence using data from the EFFORT-D study: (1) participation in the study protocol as a whole, which included both the intervention group and control group, and (2) participation in the exercise intervention. In addition to the ‘Big Five’ factor personality traits, we had data on the following potential determinants: age, gender, Body Mass Index (BMI), tobacco and alcohol use, severity of MDD, anxiety, and fitness (maximum oxygen uptake VO2max kg−1; maximal external power output Wmax kg−1).
Methods
Sample
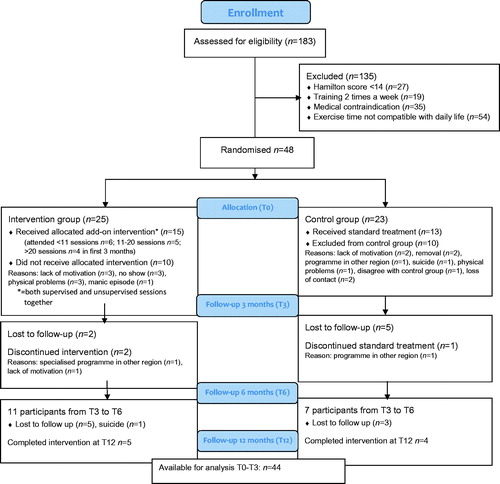
The EFFORT-D (EFFect Of Running Therapy) randomised controlled trial included 48 MDD inpatients (see flow scheme in ). All participants received treatment as usual (TAU), and half were randomly assigned to a six-month, add-on exercise intervention (outdoor Running or Nordic Walking; one weekly session guided in a group and one non-guided session). The intervention group was then compared to the group that received TAU only. The in- and exclusion criteria, the details of exercise interventions and the calculated required sample size of the EFFORT-D study have been extensively described in a full open access design article by Kruisdijk et al. (Citation2012). Measurements were performed at T0 (baseline), after 3 months (T3), after 6 months (T6), and after 12 months (T12). Results of the EFFORT-D study are described elsewhere by Kruisdijk et al. in an open access article (Kruisdijk et al. Citation2019).
Measures
Age and gender information was derived from the study dataset.
BMI: a bio-impedance scale was used to measure weight (Omron HBF-510, Omron Healthcare Europe BV, the Netherlands) and height was measured according to protocol (Seca 214, Hamburg, Germany). BMI was calculated by the standard formula.
Participants were asked about their tobacco and alcohol use at baseline using an online electronic questionnaire. Aggregated variables were smoking: 1 = never smoked, 2 = current smoker, 3 = smoking in the past; drinking: 1 = never-several times a month, 2 = 2 times a week or more.
Severity of depression: the primary outcome variable of the EFFORT-D study was the severity of depressive symptoms measured with the Hamilton depression scale with 17 items (HAM-D17). This instrument has been shown to have good interrater reliability of .92 (Pearson) and internal consistency of .82 (Cronbach’s alpha) if used by trained and experienced outcome assessors (Hermans et al. Citation1981). It is the most frequently used instrument to measure changes in depressive symptoms in clinical trials, especially in patients with more severe depression (Hoencamp et al. Citation1992). The HAM-D17 in our study showed a reliability (Cronbach’s alpha) of 0.65 at T0 (n = 44), 0.81 at T3 (n = 20) and 0.82 at T6 (n = 18).
Fitness parameters: a submaximal Åstrand bicycle test (this is an aerobic fitness test that estimates based on the relationship between heart rate during submaximal cycling and submaximal power output – the maximal oxygen uptake) was performed on a stationary bicycle ergometer (Examiner, Lode BV, the Netherlands). During this test, the heart rate was registered with a heart rate monitor (Polar RS 800, Electro Oy, Finland). The mean heart rate of the last two minutes of the submaximal bicycle test, combined in a formula with the submaximal workload (approximately 60% of the estimated maximal external power that the patient could reach in theory), was used to estimate the maximal oxygen uptake (VO2max) and the maximal external power output (Wmax).
The estimated VO2max in ml min−1 and the estimated Wmax in Watts, both related to body weight (VO2max kg−1 and Wmax kg−1, respectively), were used.
Co-morbid symptoms of anxiety were measured by the Beck Anxiety Inventory (BAI), a 21-item multiple-choice self-report inventory that measures the severity of generalised anxiety and panic symptoms in adults and adolescents. The BAI has been shown to be highly internally consistent (Cronbach's alpha = 0.94) and was scored as sufficient on tests of convergent and discriminant validity (Fydrich et al. Citation1992). In our study, at T0, the BAI anxiety questionnaire showed a reliability of 0.97 (Cronbach’s alpha), which is very high. Correlation of the BAI with the HAM-D17 was 0.39 (p = 0.07 different from zero).
Personality: the Neuroticism-Extraversion-Openness Five-Factor Inventory (NEO-FFI) is a 60-item personality questionnaire measuring the five personality traits (factors) making up the Big Five model for personality: Neuroticism, Extraversion, Agreeableness, Openness and Conscientiousness. The questionnaire has a sufficient internal and temporal reliability from 0.75 to 0.87 across scales (Murray et al. Citation2003). The total scores of the five factors were used. At T0 in our study, the NEO-FFI (n = 44) showed the following Cronbach’s alpha values: Neuroticism 0.77; Extraversion 0.73; Openness 0.54; Agreeableness 0.72; and Conscientiousness 0.75. Except for Openness, these are acceptable values.
Adherence
Adherence to the study protocol was operationalised using participation in the HAMD-17 measurements at T3 and/or T6 (some participants had no T3 measurement but did have measurements at T6). Members of the intervention group that participated more than 10 times (ratio of overall sessions in the first three months) in the Running therapy or the Nordic walking intervention (total counts of once a week guided and once a week non-guided sessions) were regarded as adherent to the intervention. This cut-off point was chosen following the per-protocol analyses described in Kruisdijk et al. (Citation2019) An overview of the numbers of adherent patients is given in : attended <11 sessions n = 6; 11–20 sessions n = 5; >20 sessions n = 4. These numbers are the total of guided and non-guided sessions as been reported by the guiding running therapists in the first three months (T6 and T12 were not available due to low numbers). We were not able to split further down. The adherence was unexpectedly very low despite great efforts of all people involved (researchers and co-workers). This was the main reason that we looked at possible determinants of this behaviour.
Statistical analysis
ANOVA, Chi-square tests and logistic regression were performed on available data using SPSS version 24 (IBM Citation2012). Participants were divided into adherent (value 1) and non-adherent (value 0) groups. Analysis of adherence was performed for the total group (intervention plus control group; n = 44 available for analyses) when studying the adherence to the study protocol, and for the intervention group alone when studying the adherence to the intervention group. Stepwise logistic regression analyses (method Block wise Enter) in both the total group and the intervention group were performed to identify determinants of adherence. Block variables were identified after analysing group differences with ANOVA and Chi-square tests and checking the number of valid cases to avoid low numbers in the analyses. Blocks were divided into background variables, mental state variables, fitness variables, and personality traits. Factors of the NEO-FFI were added in a block only if the difference in the ANOVA analyses had a significance of p < 0.10. This p-value has been chosen to avoid the early exclusion of NEO variables before checking in the model corrected for other relevant variables. In the model, however, we used a value of p < 0.05 to explore significant relationships.
Ethical approval
The EFFORT-D study protocol was approved by the Medical Ethical Committee for Mental Health (Metigg Kamer Noord), CCMO (Central Committee on Research Involving Human Subjects) protocol number: NL.26169.097.08 and registered in the Netherlands Trial Register (NTR): NTR1894 on 2 July 2009. All participants gave their written informed consent for participation in the study.
Results
After removing participants with a feasible reason for non-adherence (n = 4; see footnote in ), 44 subjects remained for analysis. Due to very low numbers at T12 (n = 9), those measurements could not be used.
Table 1. Characteristics and comparisons of groups: adherence to study protocol or adherence to intervention, and total groups.
Chi-square and ANOVA analyses showed differences in age (p = 0.09), agreeableness (p = 0.047), openness (p = 0.09) and conscientiousness (p = 0.07) between the adherent and the non-adherent subgroups, and these variables with p-values <0.10 were used in the regression analysis on study protocol adherence. The HAM-D17 scores were lower in the adherence subgroup of the intervention (p = 0.04) and openness was higher (p = 0.08); these variables were also used in the regression analysis.
and show the results of stepwise logistic regression with four blocks (background variables, mental health, fitness, and the significantly different personality factors). As the numbers of valid cases were too low for smoking, drinking and anxiety, these variables had unfortunately to be omitted in the logistic regressions. In Blocks 1 and 2 (see ) age appeared at borderline significance (p < 0.10) but disappeared when fitness was added in Block 3 (now BMI appeared at borderline level p < 0.10). Mental health (depression only) did not add to the model. In Block 4, which added the NEO FFI factors agreeableness, openness and conscientiousness, only agreeableness showed a significant result with an odds ratio (OR) of 1.2 (p = 0.03); this was a small effect, with the 95% confidence interval just above 1. Conscientiousness had borderline significance (p = 0.07), showing a trend that less conscientiousness was associated with more adherence in this sample. The total model in Block 4 showed an Omnibus Chi-square p value of 0.056.
Table 2. Block-wise logistic regression to predict adherence after 3/6 months in EFFORT-D study (total n = 42, intervention arm n = 28).
Table 3. Block-wise logistic regression to predict adherence after 3 months in Effort-D exercise intervention (total n = 24, adherence n = 9).
shows the results of the regression analyses with adherence to the exercise intervention. In this model, depression was the only significant predictor: less depression was associated with more adherence (OR = 0.699, Confidence Interval (CI) 0.49–0.99; p = 0.046). The model omnibus Chi-square was 13.1 (p=.069). After inspection of the correlation matrices of both models we saw no signs of multicollinearity. Only the fitness variables had a correlation higher than −0.8.
Discussion
We conclude that in this explorative study adherence to the research protocol of the EFFORT-D study was positively associated with the level of agreeableness, (OR 1.2; p = 0.03; 95%; CI: 1.01–1.4). Adherence to the exercise intervention was negatively associated with the severity of depression as measured with the HAM-D17 (OR 0.70, p = 0.046; 95% CI: 0.49–0.99). Both results were corrected for background variables, fitness and other personality factors. Although the regression models did not reach full significance (p values between 0.05 and 0.10), the addition of personality factors in the last regression blocks improved the total explained variance with almost 20% in both models. These were promising findings.
To our present knowledge, this was the first study to investigate personality factors as possible determinants for adherence in an add-on exercise study in MDD inpatients in regular clinical practice. Although previous research in MDD patients indicated that age (Krogh et al. Citation2014), anxiety (Herman et al. Citation2002) and tobacco and alcohol use (Helgadottir et al. Citation2018) are negative determinants for adherence, we were unable to confirm these findings. This was probably due in part to the low numbers of cases in our analyses. Moreover, the analyses did not show that BMI and fitness (VO2max kg−1 and Wmax kg−1 were specific determinants for this RCT) determine adherence. The negative association of adherence in the exercise intervention with depression was in accordance with previous research (Stubbs et al. Citation2016).
Overall, the means of the NEO-FFI scores in the total research group showed significant differences on all personality traits and even 30% more neuroticism compared to the scores of a ‘general’ population in an age group between 25 and 49 years (Hoekstra et al. Citation2007). However, compared with an MDD-affected population (N = 800) in the Netherlands Study of Depression and Anxiety (Karsten et al. Citation2012), the mean of the scores in the EFFORT-D study are largely comparable (see ), except that agreeableness is somewhat lower in our sample. This demonstrated the validity of our findings.
Table 4. Comparison of NEO-FFI scores of the EFFORT-D study sample with the general Dutch population and the NESDA study sample.
In the total research group agreeableness was found to be a predictor of adherence to the study protocol. Together with the finding that agreeableness showed a reasonable Cronbach’s alpha of 0.72 in this sample, and that this personality domain is not state dependent in MDD (Costa and McCrae Citation1994; Judge et al. Citation1999; McCrae Citation2001; Lewis and Bates Citation2014), this suggests that it could be an independent predictor of adherence in other MDD studies as well. As NEO-FFI is easily accessible, short (15–20 minutes), self-rating questionnaire, replicating this finding would not be difficult. If the use of the NEO-FFI in MDD studies can be replicated, then the agreeableness score of a patient could perhaps indicate measures to ensure that participants adhere to a study protocol as long as possible.
In the intervention group, adherence was clearly associated with HAM-D17 scores: the higher the depression scores, the lower the adherence to exercise. This association was described previously (Stubbs et al. Citation2016) and was also shown in the EFFORT-D process evaluation (Kruisdijk et al. Citation2018). For future research and for exercise programmes as an add-on to MDD treatment protocols, this means that severe MDD patients need even more personal support maintaining exercise than was offered in our study. This category of patients may have a medical indication to exercise to prevent cardiovascular problems (Vancampfort et al. Citation2017), so an even greater effort of supporting staff is needed, perhaps comparable with intensive physiotherapeutic revalidation programmes. For example, adaptation of the surroundings – such as a training programme in a physio-fitness equipped room – could have advantages above regular clinical facilities. This approach is supported by the findings of Kerling et al. (Citation2015). Their 6-weeks study involved exercising with MDD inpatients in an inside fitness environment, and their results were superior to ours, where patients received guided and unguided sessions outside. Furthermore, the poor exercise adherence (even if only 10 sessions were required to be labelled as adherent) of most depressed patients seems to originate from the lack of motivation, which is assumed to be a part of the negativism and anhedonia in MDD. This association was also found in medication adherence, as described above (Keyloun et al. Citation2017). Therefore, the entire MDD treatment trajectory with various therapeutic modalities requires an intensive and watchful attitude of the clinician with frequent monitoring of motivation.
A limitation to our study was the rather small sample of patients (n = 44). The results should therefore be interpreted cautiously. Due to this lack of power, we could have missed important predicting variables that were reported in previous studies. Also, we did not look at cross-cultural factors. Furthermore, the reliability score of the HAM-D17 at baseline was rather low (0.65) and increased at T3 and T12 (>0.80). An explanation for this effect could be that the group of blind assessors was larger with more turnover at the start of the study. One inclusion region left the study within six months after the start, leaving a smaller and more consistent team of blind assessors.
Lessons learned
In conclusion, this quantitative analysis agrees with our qualitative analysis and underlines the previous conclusion that severe MDD patients need extensive personal support from staff to maintain an exercise programme. These patients are at higher risk for cardiovascular complications, so their need for exercise is even higher than patients with a milder depression. Finally, besides replicating the present study, we recommend that future MDD studies examine the impact of NEO-FFI personality traits on adherence. This is because personality traits – in particular agreeableness – appear to be possible predictors of study adherence. This could mean that patients with low levels of agreeableness need a lot more guidance and support to enter and adhere to a study protocol than patients with higher agreeableness levels.
Acknowledgements
The authors wish to thank all patients who participated in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Busch AM, Ciccolo JT, Puspitasari AJ, Nosrat S, Whitworth JW, Stults-Kolehmainen M. 2016. Preferences for exercise as a treatment for depression. Ment Health Phys Act. 10:68–72.
- Cantrell CR, Priest JL, Cook CL, Fincham J, Burch SP. 2011. Adherence to treatment guidelines and therapeutic regimens: a US claims-based benchmark of a commercial population. Popul Health Manag. 14(1):33–41.
- Costa PT, McCrae RR. 1994. Stability and change in personality from adolescence through adulthood. In: Halverson J, Kohnstamm GA, Martin RP, editor. The developing structure of temperament and personality from infancy to adulthood. Hillsdale: Erlbaum; p. 139–150.
- Courneya KS, Friedenreich CM, Sela RA, Quinney HA, Rhodes RE. 2002. Correlates of adherence and contamination in a randomized controlled trial of exercise in cancer survivors: an application of the theory of planned behavior and the five factor model of personality. Ann Behav Med. 24(4):257–268.
- Fydrich T, Dowdall D, Chambless DL. 1992. Reliability and validity of the Beck anxiety inventory. J Anxiety Disord. 6(1):55–61.
- Goldberg LR. 1993. The structure of phenotypic personality traits. Am Psychol. 48(1):26–34.
- Helgadottir B, Hallgren M, Kullberg CLE, Forsell Y. 2018. Sticking with it? Factors associated with exercise adherence in people with mild to moderate depression. Psychology of Sport & Exercise. 35:104–110.
- Herman S, Blumenthal JA, Babyak M, Khatri P, Craighead WE, Krishnan KR, Doraiswamy PM. 2002. Exercise therapy for depression in middle-aged and older adults: predictors of early dropout and treatment failure. Health Psychol. 21(6):553–563.
- Hermans PJ, Ree F, Betgem P. 1981. Betrouwbaarheid en validiteit van het Hamilton Interview. Tijdschrift Voor Psychologie. 9:219–233.
- Hoekstra HA, Ormel J, Fruyt F. 2007. NEO-PI-R/NEO-FFI Handleiding. Amsterdam: Hogrefe Uitgevers B.V.
- Hoencamp E, Betten I, Haffmans P. 1992. Interrater reliability of the Hamilton Rating Scale for Depression. Acta Neuropsychiatr. 4(4):86–89.
- IBM. 2012. SPSS, version 24. https://www.ibm.com/analytics/data-science/predictive-analytics/spss-statistical-software
- Judge TA, Higgins CA, Thoresen CJ, Barrick MR. 1999. The Big Five personality traits, general mental ability and career success across the life span. Personnel Psychol. 52(3):621–652.
- Karsten J, Penninx BW, Riese H, Ormel J, Nolen WA, Hartman CA. 2012. The state effect of depressive and anxiety disorders on big five personality traits. J Psychiatr Res. 46(5):644–650.
- Kerling A, Tegtbur U, Gützlaff E, Kück M, Borchert L, Ates Z, von Bohlen A, Frieling H, Hüper K, Hartung D, et al. 2015. Effects of adjunctive exercise on physiological and psychological parameters in depression: a randomized pilot trial. J Affect Disord. 177:1–6.
- Keyloun KR, Hansen RN, Hepp Z, Gillard P, Thase ME, Devine EB. 2017. Adherence and persistence across antidepressant therapeutic classes: a retrospective claims analysis among insured US patients with Major Depressive Disorder (MDD). CNS Drugs. 31(5):421–432.
- Kotov R, Gamez W, Schmidt F, Watson D. 2010. Linking ‘big’ personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. 136(5):768–821.
- Krivoy A, Balicer RD, Feldman B, Hoshen M, Zalsman G, Weizman A, Shoval G. 2016. Adherence to antidepressants is associated with lower mortality: a 4-year population-based cohort study. J Clin Psychiatry. 77(5):e566–e572.
- Krogh J, Lorentzen AK, Subhi Y, Nordentoft M. 2014. Predictors of adherence to exercise interventions in patients with clinical depression – a pooled analysis from two clinical trials. Mental Health Physical Activity. 7(1):50–54.
- Kruisdijk F, Hendriksen I, Tak E, Beekman A-J, Hopman-Rock M. 2018. EFFORT‑D study process evaluation: challenges in conducting a trial into the effects of running therapy in patients with major depressive disorder. Ann Gen Psychiatry. 17(1)
- Kruisdijk F, Hendriksen IJ, Tak EC, Beekman AT, Hopman-Rock M. 2012. Effect of running therapy on depression (EFFORT-D). Design of a randomised controlled trial in adult patients [ISRCTN 1894]. BMC Public Health. 12:50.
- Kruisdijk F, Hopman-Rock M, Beekman ATF, Hendriksen I. 2019. EFFORT-D: results of a randomised controlled trial testing the effect of running therapy on depression. BMC Psychiatry. 19(1):170.
- Lewis G, Bates TC. 2014. How genes influence personality: evidence from multi-facet twin analyses of the HEXACO dimensions. J Res Personality. 51:9–17.
- Lewis GJ, Bates TC, Posthuma D, Polderman TJ. 2014. Core dimensions of personality broadly account for the link from perceived social support to symptoms of depression and anxiety. J Pers. 82(4):329–339.
- Lingam R, Scott J. 2002. Treatment non-adherence in affective disorders. Acta Psychiatr Scand. 105(3):164–172.
- McCrae RR, Costa PT. Jr. 1987. Validation of the five-factor model of personality across instruments and observers. J Pers Soc Psychol. 52(1):81–90.
- McCrae RR. 2001. Trait psychology and culture: exploring intercultural comparisons. J Pers. 69(6):819–846.
- Miller TR. 1991. The psychotherapeutic utility of the five-factor model of personality: a clinician's experience. J Pers Assess. 57(3):415–433.
- Murray G, Rawlings D, Allen NB, Trinder J. 2003. NEO five factor inventory scores: psychometric properties in a community sample. Measure Eval Counsel Dev. 36(3):140–149.
- Sabate E. 2003. Adherence to long-term therapies – evidence for action. Geneva: WHO.
- Stubbs B, Vancampfort D, Rosenbaum S, Ward PB, Richards J, Soundy A, Veronese N, Solmi M, Schuch FB. 2016. Dropout from exercise randomized controlled trials among people with depression: a meta-analysis and meta regression. J Affect Disord. 190:457–466.
- Mosby’s Dictionary of Medicine, Nursing & Health Professions. 9th ed. St. Louis, USA: Elsevier; 2013.
- Vancampfort D, Rosenbaum S, Schuch F, Ward PB, Richards J, Mugisha J, Probst M, Stubbs B. 2017. Cardiorespiratory fitness in severe mental illness: a systematic review and meta-analysis. Sports Med. 47(2):343–352.
- Yamashita Y, Seki N, Umeda K, Tanabe N, Shinoda K, Konishi I, Sekiya A, Sekii A, Ohta T. 2017. [Relationship between exercise adherence and personality characteristics in persons experienced in the Medical Fitness program]. Nihon Koshu Eisei Zasshi. 64(11):664–671.
- Zivin K, Kales HC. 2008. Adherence to depression treatment in older adults: a narrative review. Drugs Aging. 25(7):559–571.