Abstract
Objective
Aggressive behaviour is highly prevalent in long-term psychiatric inpatient care. We aimed to estimate the overall incidence of aggression, the time staff took to handle aggression incidents, and the weighted average financial costs thereof.
Methods
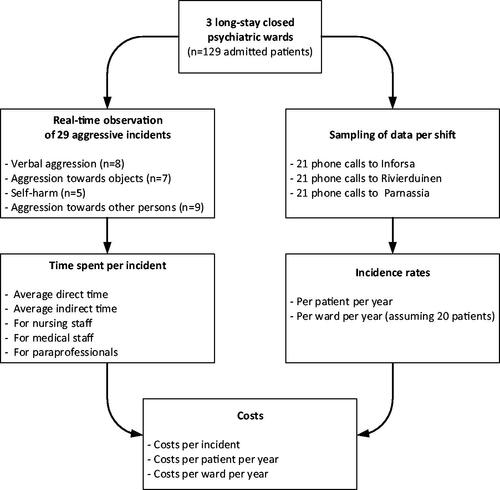
A random sampling procedure was conducted at long-term psychiatric inpatient care facilities. Nurses were asked to recall all incidents (i.e., verbal, physical towards objects, self, or others) of their shift. For the time spent on each type of incident, staff were monitored in real-time. Estimated costs were calculated by the time spent multiplied by hourly wages in addition to material-related costs.
Results
Incidence rates were 90 incidents per patient year. The average time spent per incident was 125 min but differed for each type of incident. Almost 80% of this time was consumed by nursing staff. The average cost per aggression incident was €78; extrapolated per patient year, the total costs were approximately €7000.
Conclusions
The current study found a high rate of aggression incidents in closed long-stay psychiatric wards. Reports of aggression on these types of wards are scarce. Nevertheless, aggression seems to have a severe impact on invested time and related costs, which suggests a need for aggression-prevention and de-escalating programs.
Aggression incidents are highly prevalent and are accompanied by high costs.
The effect of aggression incidents on the workload for staff members is high, especially for nursing staff.
Studies across countries on the incidence and the costs of aggression among psychiatric inpatients are needed to help model the effects of (new) strategies for aggression reduction.
Key points
Keywords:
Introduction
Despite the increased awareness and efforts to reduce violence in clinical care among healthcare workers (McDermott and Holoyda, Citation2014; Spelten et al. Citation2020) and policy-makers (Ministerie van Volksgezondheid, Welzijn en Sport, Minsterie van Binnenlandse Zaken en Koninkrijksrelaties, & Ministerie van Veiligheid en Justitie, 2012), aggression incidents remain prevalent in psychiatric inpatient facilities (Bowers et al. Citation2011). Aggression is expressed either verbally or physically or both, and can be directed at objects, patients themselves, other patients, and staff members. Consequences of aggression incidents are diverse and occasionally substantial. For instance, incidents may have physical consequences, may cause distress, and may be traumatic for patients and staff (Nijman, Bowers, et al. Citation2005; Bowers et al. Citation2011). Last year the highest percentages reported by mental health workers were for verbal aggression. For physical abuse, percentages between73% and 80% were reported (Nijman, Bowers, et al. Citation2005; Edward et al. Citation2016). These latter forms of aggression sometimes lead to severe injury (e.g., broken bones, loss of teeth), which was reported by 16% of psychiatric nurses. The exposure to aggression may also lead to acute stress disorder, and post-traumatic stress disorder (PTSD) in severe cases (14–17% of exposed staff members), but more frequently, it leads to subclinical symptoms which may include hyperarousal (Richter and Berger Citation2006; Lee et al. Citation2015). Besides violence directed at staff members, a survey among psychiatric inpatients revealed that 54% had been exposed to threats and aggression from other patients and 31% had been physically assaulted (Frueh et al. Citation2005).
Furthermore, aggression incidents have substantial financial consequences relating to, for example, damaged property, higher drug use, and more time spent by staff due to an increased work burden (Rubio-Valera et al. Citation2015), also relating to staff sick-leave due to the physical and psychological consequences that might follow a critical incident (Hillbrand et al. Citation1996; Farrell and Cubit Citation2005; Nijman, Bowers, et al. Citation2005). As far as we know, only two studies contain information on the costs of aggression in psychiatric inpatients. Annual economic costs of aggression incidents were substantial in both Spain (Serrano-Blanco et al. Citation2017) and the United Kingdom (Flood et al. Citation2008). Furthermore, these estimates may underestimate the actual costs because indirect costs were not taken into account. High indirect costs include lost staff work days, which range between 38 and 85 days per injured staff member (Hunter and Carmel Citation1992; Hillbrand et al. Citation1996; Nijman, Bowers, et al. Citation2005); longer hospital admissions; and more readmissions (Rubio-Valera et al. Citation2015).
Incidence rates for aggression in psychiatry vary, ranging from less than 1 to 60 incidents per patient year in two systematic reviews (Nijman, Palmstierna, et al. Citation2005; Bowers et al. Citation2011). The wide range of estimates may be explained by the fact that incidents are less often documented officially, compared to what is actually experienced by staff members, according to self-reported questionnaires and videos, particularly with regard to verbal aggression (Ferns Citation2006; Nolan and Citrome Citation2008; Archer et al. Citation2019). Furthermore, there are large variations in study design (e.g., prospective versus retrospective data collection), differences in how the studies’ authors defined aggression (e.g., including or excluding verbal aggression and self-harm), and emphases on different patient populations (e.g., these included acute or long stay wards; open or closed wards; and forensic, mixed, or psychiatric wards). While incidence estimates have often been based on data collected from (acute) admission wards (Nijman et al. Citation1997; Flood et al. Citation2008; Hankin et al. Citation2011) and (forensic) hospitals (Hunter and Carmel Citation1992; Hillbrand et al. Citation1996; Serrano-Blanco et al. Citation2017), data from long-stay facilities for psychiatric care is much more scarce. Yet, aggressive behaviour regularly leads to a referral to a long-term inpatient care (Daffern and Howells Citation2002). The severely ill and more complex patients residing in these facilities may show different patterns of aggressive behaviour than patients in acute-admission wards.
In this study, we aimed (i) to estimate the incidence rates of different types of aggression in closed long-stay psychiatric wards in the Netherlands, (ii) to estimate the time spent by staff members per aggression incident, and (iii) to estimate the direct costs associated with aggression in long-stay psychiatric wards.
Methods
Participants
The study was conducted in closed psychiatric long-stay wards belonging to three regional mental healthcare centres in urbanised areas of the Netherlands: Rivierduinen Psychiatric Centre in Oegstgeest, Parnassia Psychiatric Institute in The Hague, and Inforsa in Amsterdam. All three institutes provide long-term inpatient care. The psychiatric clinical capacity for long-stay (defined as an admission duration of more than 1 year) in the Netherlands in 2017 was 6250 beds, of which 23% (or about 1438 beds) are in a closed setting (Kroon et al. Citation2018). Although patients can be admitted or discharged during the year, the total number of admitted patients at any time stays close to 1438 – a rather high occupancy rate for long-stay clinical psychiatry. In all three centres, about two-thirds of the patients were male and had been diagnosed predominantly with psychosis spectrum disorders or severe personality disorders, with approximately 80% of patients meeting diagnostic criteria for either one of these disorders. Patients were mainly admitted involuntarily. The Medical Ethical Committee of Leiden University Medical Centre granted permission for this study. Considering the mostly descriptive nature of the current study, no sample size calculation was performed beforehand. Moreover, no recent reliable data were available for the proportion of interest from previous studies in the group of patients from long-stay wards, which is necessary for its calculation.
Definition of aggression incidents
We categorised aggression incidents into four categories, based on the Overt Aggression Scale (OAS) (Yudofsky et al. Citation1986). First, we defined ‘verbal aggression’ as yelling, shouting, using obscenities or swearwords, sexual remarks, and threatening others (with or without a threatening posture). Second, we defined ‘physical aggression towards an object’ as kicking, hitting, throwing objects (e.g., chairs, dishes, or cups), and slamming doors. Third, we defined ‘self-harm’ as any act of physical aggression towards the self, such as hitting, cutting, burning, strangulation, overdosing on medication, and jumping from heights (with or without suicidal intent). Fourth, we defined ‘physical aggression towards others’ as a physical assault on another person by means of hitting, pushing, pulling, holding, scratching, kicking, biting, spitting, touching inappropriately, strangulating, and/or attacking someone with an object (e.g., a chair or a knife). We did not categorise incidents based on severity. Case vignettes illustrating each of the categories are presented in Supplement 1.
Aggression incidence
To estimate the incidence of aggression across the four categories, we applied a random sampling procedure, which included 21 nursing shifts over a 6-month period (February–July 2014) at all three facilities (. All weekdays (Monday–Sunday) and shift types (day, evening, and night) were covered. At the end of each shift, one of the psychiatric nurses was interviewed via telephone; we asked him/her to recall all incidents during the preceding 8 h. If one patient caused several incidents, or if an incident escalated to a graver category, only the most severe incident was recorded for that shift. Using a random number generator, participating staff members were randomly selected from the total available ward staff per shift. The number of patients observed per shift was used to calculate the total number of observed patient years. This total, along with the observed incidents, was then used to calculate incidence rates per patient year. The ratio of the occurrence of the four types of aggression was used as a weight factor to calculate the time spent and the total cost of all aggression incidents.
Time spent on aggression
The time spent on each type of incident by staff members was monitored in real-time by a researcher who was present during day shifts and evening shifts over a period of one week at each of the three facilities. The researcher followed all incidents from start to finish to record all the activities by all staff members who handled the incident. Just as for the calculation of the incidence, if an incident escalated to a graver category, only the most severe incident, as experienced by nursing staff, was assigned to one of the four categories. These activities were collapsed into two categories: direct time (i.e., de-escalating conversation, restraining patients, checking up on isolated patients, administering medication, and tending to medical needs) and indirect time (i.e., administrative activities, discussing and evaluating the incident, information transfer, consultation, and transport).
Costs of aggression incidence
To estimate costs for each type of aggression incident from an institutional perspective, staff wages and material costs of both damaged property and immediate medical care were taken into account. We defined ‘nursing staff’ in a psychiatric ward as licenced nurses and psychiatric social workers whose responsibilities include the day-to-day care for patients. We labelled other assistive personnel as ‘paraprofessionals’, which included patient supporters, activity supervisors, and specially trained security personnel who support nursing staff during aggression incidents. Average yearly wages were derived from the Collective Labour Agreement for the Mental Health Sector (2017–2019) (GGZ Nederland Citation2017). Consistent with the guidelines of the Dutch Healthcare Authority, these wages were adjusted incrementally with the mandatory insurances provided by the employer. The same Collective Labour Agreement also provides the yearly number of available work hours per staff member, taking into account average days of sick leave and annual leave. Yearly salary costs were divided by the total available work hours, resulting in hourly wages for each staff category (Supplement 2). To account for the incidents occurring outside the standard 40-h working week, hourly wages were increased with a percentage surcharge for irregular shifts in proportion to the number of incidents taking place during evening and night shifts and during the weekend. Finally, staff costs were calculated by multiplying appropriate hourly wages with the average amount of time spent by each type of professional per incident type.
Material-related costs consisted of property damages caused by the patient (e.g., broken furniture or windows) and immediate medical expenses at the ward (e.g., costs of administering medication or necessary medical treatment of injured patients or members of staff as a direct consequence of the incident). The costs of non-immediate medical treatment or sick leave taken by staff members as a result of the incident could not be included, as it was impossible to link these to individual aggression incidents.
Adding the average personnel and material costs for each type of incident allowed us to calculate the average costs per incident for each of the four incident categories. Using the previously estimated number of incidents per patient year, we inferred the annual costs (i) per patient and (ii) per ward (assuming 20 patients per ward).
Results
Ward characteristics
shows the characteristics of the psychiatric wards; the psychiatric centre Inforsa in Amsterdam has the highest number of nurses and psychiatrists per patient. The average number of patients per ward was 23, and the average number of patients per nurse across all shifts was five. The proportion of patients admitted involuntarily was above 85% for all wards.
Table 1. Characteristics of the three included closed psychiatric wards.
Incidence rate of aggression
Data on aggression incidents for the three wards together are shown in . In total, 81 incidents occurred. The data were extrapolated to yield incidence rates per patient year, leading to an average of 90 incidents per patient per year. The incidence rates per patient year for the different categories were 63 for verbal aggression, 8 for physical aggression towards objects, 7 for self-harm, and 12 for physical aggression towards others. Eighty-eight per cent of incidents occurred during the day and evening (7:00–23:00). Incidents were roughly evenly divided among weekdays and weekends (31% occurred on the weekend).
Table 2. Characteristics and time- and material-related costs of four types of aggression incidents.
Time spent on aggression
While we measured personnel costs of time spent by members of staff dealing with aggression, we directly observed 29 incidents during three consecutive one-week observation periods (verbal aggression n = 8, physical aggression towards an object n = 7, self-harm n = 5, physical aggression towards others n = 9). In total, 5324 min were spent on the 29 incidents that we observed. shows that the average time spent on aggression incidents varied among the types of incidents. Of this time, 77% was spent by nursing staff, 6% by medical doctors, and 18% by paraprofessionals. For all aggression incidents, average total time spent was 125 min; 44% of that time (i.e., 55 min) was spent in contact with the patient during and after the incident, and 56% (i.e., 70 min) of that time was spent on ‘indirect’ consequences such as information transfer among staff, administrative activities, and care for involved personnel. Assuming a staff occupancy of five patients per nurse and 96 min per incident spent on nursing time, nurses spend 39 min on average per shift dealing with aggression.
Costs of aggression
The average hourly gross personnel costs for nursing staff are €26 (ranging between €17 and €29). At the psychiatric centre Rivierduinen, a security guard trained for healthcare receives an hourly wage of €33. Hourly costs for medical staff are €46 for doctors and €74 for psychiatrists. Average direct costs per incident are shown in . The average direct cost per incident was €78. Material costs were on average €3 per incident, with the highest direct costs in the category of physical aggression towards an object (€27). With 90 incidents per patient year, direct costs per patient amount to about €7000 annually. In a typical closed ward setting that supports 20 patients for long-term psychiatric care, the annual direct cost would amount to €140,000 annually.
Discussion
We found an incidence rate of 90 incidents per patient year, amounting to five incidents per day in an average ward with 20 inpatients. The average time spent was 125 min per incident, which indicates that (given average staff occupancy) each individual nurse spent more than half an hour per shift dealing with aggression. These direct costs related to incidents amounted to approximately €78 per incident. Based on our incidence rate, this would result in an estimate of €7000 per patient per year. The maximum cost for a psychiatric nursing day was €328.43 in 2018 (Nederlandse Zorgautoriteit Citation2017), implying that 6% of the total budget was earmarked for aggression.
The incidence rates we found for aggressive behaviour were higher than those reported in earlier studies (which range from less than 1 to 60 incidents per patient year), mostly in acute and forensic settings (Nijman, Palmstierna, et al. Citation2005; Bowers et al. Citation2011). These differences exist partly because these studies used retrospective data collection or data from officially reported incidents only (Bowers et al. Citation2011). Such designs have a risk of selective recall and underreporting for milder incidents. Furthermore, the varying incidence rates could be due to differences in how the aggression incidents and ward types were defined and which sampling methods were used. The current study used a broad definition that included verbal aggression; most previous studies did not include these incidents. Verbal aggression is the most common form of aggression (Foster et al. Citation2007; Stone et al. Citation2011), and can have a strong mental impact on other patients and staff, but it is often overlooked when reporting all types of aggressive behaviour. In line with existing literature, we found that verbal aggression occurred most often and aggression relating to self-harm occurred the least often (Stone et al. Citation2011; Li et al. Citation2019).
Interestingly, the current study found that time spent indirectly lasted longer than time spent in direct contact with patients (on average 55 versus 70 min). Around 85% of indirect time consisted of the transfer of information and consulting. Much of this indirect time was used for interpersonal support among colleagues and the venting of emotions by staff members, which reflect the emotional impact of aggression on the staff. Moreover, the time (and cost) spent on aggression cannot be invested in therapeutic and social activities. Among the different disciplines, nursing staff spent the majority of time (and cost) dealing with aggression. This confirms previous research, which states that nurses working in inpatient psychiatric wards are at high risk for experiencing aggression at work (Nijman, Bowers, et al. Citation2005; Campbell et al. Citation2011).
The largest contributors to total cost were verbal aggression (due to its highest incidence rate) and physical aggression towards others (due to the large amount of time needed to intervene in these incidents). That verbal aggression was expensive in absolute terms was also found in acute psychiatric wards (Flood et al. Citation2008). Further, staff members are often the target of both verbal aggression and aggression towards others; this could increase burnout and sick leave (Nijman, Bowers, et al. Citation2005; Bowers et al. Citation2009), meaning our estimated costs were likely conservative. Likewise, an incident sometimes took place during multiple shifts (and even days) and may have incurred costs long after the initial incident happened. Aggressive patients are more often secluded and consume higher doses of medication (Rubio-Valera et al. Citation2015). Like most other studies that focussed on healthcare costs (Flood et al. Citation2008; Serrano-Blanco et al. Citation2017), we did not include costs that were indirectly caused by aggression (e.g., staff absence, re-admissions, and assistance of police or ambulance). Training courses for staff, special designs of wards that reduces the risks of violence, and interventions to reduce aggression are costly. Interventions comprise medication and psychotherapy (Alpert and Spillmann Citation1997; Jones et al. Citation2011; Correll et al. Citation2017), and aggression management courses for staff (Farrell and Cubit Citation2005). One such programme is the Safewards model, providing 10 interrelated interventions (Bowers Citation2014; Bowers et al. Citation2014). Although several studies on Safewards showed significant reductions in conflict events, no cost-effective studies were performed (Bowers et al. Citation2015; Fletcher et al. Citation2017; Maguire et al. Citation2018; Baumgardt et al. Citation2019). Depending on the available staff capacity, costs in terms of money and budget may be smaller or larger than the costs we estimated in this analysis. When staff capacity is sufficient, a change in aggression level need not affect the budget but would be compensated by the time that is available for therapeutic and social activities. In that case the costs are intangible, in terms of reduced quality of care. But when personnel capacity is insufficient, aggression may require a full additional staff member in the ward. In that case the budget impact could be considerably larger than estimated.
To date, studies providing information on costs of aggression are scarce. Recently, a systematic review was conducted on health-service use and costs associated with aggressiveness and agitation in psychiatric care (Rubio-Valera et al. Citation2015). In the review, nine out of ten studies analysed the impact on care such as longer stay and more frequent re-admissions, but they did not quantify the costs. Only one study estimated the cost of conflict-related behaviour using a bottom-up approach similar to ours. They converted time involved in conflicts to a monetary amount using national unit cost data and found annual costs to be €182,616 per ward. Estimated costs per aggression incident ranged from £23 (€27) to £200 (€236) per incident (Flood et al. Citation2008; European Central Bank Citation2020), compared to an average of €78 per incident in the present study. However, due to differences in the organisation of mental healthcare between countries, it remains difficult to compare studies across countries (Raboch et al. Citation2010; Kalisova et al. Citation2014). To better estimate the costs of aggression, future studies in different settings and countries are needed.
To our knowledge, our study is the first that prospectively estimates aggression in closed long-stay psychiatric wards and suggests a methodology that can be employed in different settings. Real-time observation of incidents enabled us to make accurate assessments of the time invested by staff. Additionally, we sampled from three different centres, which moderated some of the differences between each location.
An important limitation of the current study is that we sampled a relatively small group of patients within a short amount of time. Studies show considerable variation in the prevalence of aggression between patients; a small number of patients is often responsible for a large proportion of aggression (Nijman, Bowers, et al. Citation2005; Foster et al. Citation2007). Likewise, we did not observe patients during all seasons, and studies have indicated that this could affect the incidence rate of aggression (Bader et al. Citation2014). Therefore, future studies should collect more data on incidents from more diverse wards and countries, and preferably use validated tools such as the Staff Observation Aggression Scale-revised (SOAS-R; Nijman et al. Citation1999). The SOAS-R quantifies the frequency and severity of aggression incidents, making it easier to compare the scarce studies on aggression. Furthermore, interviewing nurses at the end of their shift may have led to underreporting. We posit, however, that our method of asking specifically for all types of aggression that occurred over a recently completed 8-h shift may be more accurate than retrospective data collected over much longer time intervals. Another contributor to underreporting may be that only the most severe incident was registered even when a patient caused several incidents. However, we may have also overestimated the related costs. It is possible that mild incidents, which consumed no time, were included in calculating the incidence rate but were not taken into account in the time measurement, which would result in an overestimation of the time spent as well as the costs for aggression.
Conclusions
Incidence rates of aggression, the workload for staff members, and the associated direct costs in closed long-stay psychiatric wards are high. Aside from the financial perspective, reduction of aggression is highly valuable for both patients and staff. Aggression reduction already has a high priority in long-term psychiatric inpatient care (e.g., de-escalating programs, adequate pharmacotherapy), but more effective and innovative methods to prevent aggression are needed.
Supplemental Material
Download MS Word (30 KB)Acknowledgements
The authors thank all nurses who contributed to the current study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Alpert JE, Spillmann MK. 1997. Psychotherapeutic approaches to aggressive and violent patients. Psychiatr Clin North Am. 20:453–472.
- Archer S, Thibaut BI, Dewa LH, Ramtale C, D’Lima D, Simpson A, Darzi A. 2019. Barriers and facilitators to incident reporting in mental healthcare settings: a qualitative study. J Psychiatr Ment Health Nurs. 27:211–223.
- Bader S, Evans SE, Welsh E. 2014. Aggression among psychiatric inpatients: the relationship between time, place, victims, and severity ratings. J Am Psychiatr Nurses Assoc. 20:179–186.
- Baumgardt J, Jäckel D, Helber-Böhlen H, Stiehm N, Morgenstern K, Voigt A, Schöppe E, Mc Cutcheon A-K, Lecca EEV, Löhr M. 2019. Preventing and reducing coercive measures – an evaluation of the implementation of the safewards model in two locked wards in Germany. Front Psychiatry. 10:340.
- Bowers L. 2014. Safewards: a new model of conflict and containment on psychiatric wards. J Psychiatr Ment Health Nurs. 21:499–508.
- Bowers L, Alexander J, Bilgin H, Botha M, Dack C, James K, Jarrett M, Jeffery D, Nijman H, Owiti JA. 2014. Safewards: the empirical basis of the model and a critical appraisal. J Psychiatr Ment Health Nurs. 21:354–364.
- Bowers L, Allan T, Simpson A, Jones J, Van Der Merwe M, Jeffery D. 2009. Identifying key factors associated with aggression on acute inpatient psychiatric wards. Issues Ment Health Nurs. 30:260–271.
- Bowers L, James K, Quirk A, Simpson A, Stewart D, Hodsoll J, SUGAR. 2015. Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial. Int J Nurs Stud. 52:1412–1422.
- Bowers L, Stewart D, Papadopoulos C, Dack C, Ross J, Khanom H, Jeffery D. 2011. Inpatient violence and aggression: a literature review. London: Institute of Psychiatry. https://pdfs.semanticscholar.org/b98f/4ff17c264fd919542dcc14905b280c8776b8.pdf
- Campbell JC, Messing JT, Kub J, Agnew J, Fitzgerald S, Fowler B, Sheridan D, Lindauer C, Deaton J, Bolyard R. 2011. Workplace violence: prevalence and risk factors in the safe at work study. J Occup Environ Med. 53:82–89.
- Correll CU, Yu X, Xiang Y, Kane JM, Masand P. 2017. Biological treatment of acute agitation or aggression with schizophrenia or bipolar disorder in the inpatient setting. Ann Clin Psychiatry. 29:92–107.
- Daffern M, Howells K. 2002. Psychiatric inpatient aggression: a review of structural and functional assessment approaches. Aggression Viol Behav. 7:477–497.
- Edward KL, Stephenson J, Ousey K, Lui S, Warelow P, Giandinoto JA. 2016. A systematic review and meta-analysis of factors that relate to aggression perpetrated against nurses by patients/relatives or staff. J Clin Nurs. 25:289–299.
- European Central Bank. 2020 [accessed Feb 3]. http://www.ecb.europa.eu/stats/exchange/eurofxref/html/index.en.html
- Farrell G, Cubit K. 2005. Nurses under threat: a comparison of content of 28 aggression management programs. Int J Ment Health Nurs. 14:44–53.
- Ferns T. 2006. Under-reporting of violent incidents against nursing staff. Nurs Stand. 20:41–45.
- Fletcher J, Spittal M, Brophy L, Tibble H, Kinner S, Elsom S, Hamilton B. 2017. Outcomes of the Victorian Safewards trial in 13 wards: impact on seclusion rates and fidelity measurement. Int J Ment Health Nurs. 26:461–471.
- Flood C, Bowers L, Parkin D. 2008. Estimating the costs of conflict and containment on adult acute inpatient psychiatric wards. Nurs Econ. 26:325–330.
- Foster C, Bowers L, Nijman HLI. 2007. Aggressive behaviour on acute psychiatric wards: prevalence, severity and management. J Adv Nurs. 58:140–149.
- Frueh BC, Knapp RG, Cusack KJ, Grubaugh AL, Sauvageot JA, Cousins VC, Yim E, Robins CS, Monnier J, Hiers TG. 2005. Patients' reports of traumatic or harmful experiences within the psychiatric setting. Psychiatr Serv. 56:1123–1133.
- GGZ Nederland. 2017. Collectieve arbeidsovereenkomst GGZ 2017–2019. Amersfoort: GGZ Nederland.
- Hankin CS, Bronstone A, Koran LM. 2011. Agitation in the inpatient psychiatric setting: a review of clinical presentation, burden, and treatment. J Psychiatr Pract. 17:170–185.
- Hillbrand M, Foster HG, Spitz RT. 1996. Characteristics and cost of staff injuries in a forensic hospital. Psychiatr Serv. 47:1123–1125.
- Hunter M, Carmel H. 1992. The cost of staff injuries from inpatient violence. Psychiatric Serv. 43:586–588.
- Jones RM, Arlidge J, Gillham R, Reagu S, van den Bree M, Taylor PJ. 2011. Efficacy of mood stabilisers in the treatment of impulsive or repetitive aggression: systematic review and meta-analysis. Br J Psychiatry. 198:93–98.
- Kalisova L, Raboch J, Nawka A, Sampogna G, Cihal L, Kallert TW, Onchev G, Karastergiou A, Del Vecchio V, Kiejna A. 2014. Do patient and ward-related characteristics influence the use of coercive measures? Results from the EUNOMIA international study. Soc Psychiatry Psychiatr Epidemiol. 49:1619–1629.
- Kroon H, Michon H, Knispel A, Hulschbosch L, de Lange A, Boumans J, Oud M. 2018. Landelijke monitor ambulantisering en hervorming langdurige GGZ. Utrecht: Trimbos-instituut.
- Lee J, Daffern M, Ogloff JR, Martin T. 2015. Towards a model for understanding the development of post-traumatic stress and general distress in mental health nurses. Int J Ment Health Nurs. 24:49–58.
- Li W, Yang Y, Hong L, An FR, Ungvari GS, Ng CH, Xiang YT. 2019. Prevalence of aggression in patients with schizophrenia: a systematic review and meta-analysis of observational studies. Asian J Psychiatr. 47:101846.
- Maguire T, Ryan J, Fullam R, McKenna B. 2018. Evaluating the introduction of the safewards model to a medium- to long-term forensic mental health ward. J Forensic Nurs. 14:214–222.
- McDermott BE, Holoyda BJ. 2014. Assessment of aggression in inpatient settings. CNS Spectr. 19:425–431.
- Nederlandse Zorgautoriteit. 2017. Tariefbeschikking Generalistische basis-ggz – TB/REG-18608-01. [accessed 2020 Feb 3]. https://puc.overheid.nl/nza/doc/PUC_6196_22/
- Nijman HLI, Bowers L, Oud N, Jansen G. 2005. Psychiatric nurses' experiences with inpatient aggression. Aggress Behav. 31:217–227.
- Nijman HLI, Merckelbach HL, Allertz WF, A Campo JM. 1997. Prevention of aggressive incidents on a closed psychiatric ward. Psychiatr Serv. 48:694–698.
- Nijman HLI, Muris P, Merckelbach HLGJ, Palmstierna T, Wistedt B, Vos AM, Allertz WF. 1999. The staff observation aggression scale – revised (SOAS-R). Aggress Behav. 25:197–209.
- Nijman HLI, Palmstierna T, Almvik R, Stolker JJ. 2005. Fifteen years of research with the Staff Observation Aggression Scale: a review. Acta Psychiatr Scand. 111:12–21.
- van Volksgezondheid M, En Sport W, van Binnenlandse Zaken En Koninkrijksrelaties M, van Veiligheid En Justitie M. 2012. Actieplan Veilig werken in de zorg. [accessed 2020 Feb 3]. https://www.rijksoverheid.nl/documenten/rapporten/2012/03/22/actieplan-veilig-werken-in-de-zorg
- Nolan KA, Citrome L. 2008. Reducing inpatient aggression: does paying attention pay off? Psychiatr Q. 79:91–95.
- Raboch J, Kalisová L, Nawka A, Kitzlerová E, Onchev G, Karastergiou A, Magliano L, Dembinskas A, Kiejna A, Torres-Gonzales F. 2010. Use of coercive measures during involuntary hospitalization: findings from ten European countries. Psychiatr Serv. 61:1012–1017.
- Richter D, Berger K. 2006. Post-traumatic stress disorder following patient assaults among staff members of mental health hospitals: a prospective longitudinal study. BMC Psychiatry. 6:15.
- Rubio-Valera M, Luciano JV, Ortiz JM, Salvador-Carulla L, Gracia A, Serrano-Blanco A. 2015. Health service use and costs associated with aggressiveness or agitation and containment in adult psychiatric care: a systematic review of the evidence. BMC Psychiatry. 15:35.
- Serrano-Blanco A, Rubio-Valera M, Aznar-Lou I, Baladón Higuera L, Gibert K, Gracia Canales A, Kaskens L, Ortiz JM, Salvador-Carulla L. 2017. In-patient costs of agitation and containment in a mental health catchment area. BMC Psychiatry. 17:212.
- Spelten E, Thomas B, O'Meara PF, Maguire BJ, FitzGerald D, Begg SJ. 2020. Organisational interventions for preventing and minimising aggression directed towards healthcare workers by patients and patient advocates. Cochrane Database Syst Rev. 4:CD012662.
- Stone T, McMillan M, Hazelton M, Clayton EH. 2011. Wounding words: swearing and verbal aggression in an inpatient setting. Perspect Psychiatr Care. 47:194–203.
- Yudofsky SC, Silver JM, Jackson W, Endicott J, Williams D. 1986. The Overt Aggression Scale for the objective rating of verbal and physical aggression. Am J Psychiatry. 143:35–39.