Abstract
Introduction
Confabulations refer to the emergence of memories of experiences and events that are incorrect in place and time, or never took place. In alcoholic Korsakoff’s syndrome, confabulations have been frequently reported, but seldomly been investigated. Traditional reports on confabulations state that confabulations in KS mainly occur in the post-acute phase of the illness. The aim of the study was to investigate whether confabulations extinguish in KS.
Methods
An observational rating of confabulation behaviour (the NVCL-R) was completed for 172 KS patients with alcoholic KS. Post-acute and chronic KS patients were compared cross-sectionally in two centres.
Results
Provoked and spontaneous confabulations were present in post-acute and chronic patients. Patients residing in a long-term care facility more often presented themselves with spontaneous confabulations than patients in a diagnostic centre.
Conclusions
In contrast to the traditional view, confabulations may be present throughout the course of KS, and are possibly more frequently present in patients receiving care in specialised long-term care facilities than in patients who receive less intensive support.
Confabulations are a central characteristic of Korsakoff’s syndrome
In contrast to popular belief, confabulations may be present in acute and chronic Korsakoff’s syndrome
The severity of confabulations is related to an unfavourable disease outcome in KS
A longitudinal approach would help the confirmation of finding no decline in confabulations over time.
Key points
Introduction
Confabulations refer to the emergence of memories of experiences and events that are incorrect in place and time, or never took place at all, and that are produced unintentionally (Cooper et al. Citation2006; Kopelman Citation2015; Rensen et al. 2015). Different classifications of confabulations have been postulated (for an overview, see Schnider Citation2018). A widely used distinction is made between provoked and spontaneous confabulations (Kopelman Citation1987). Provoked confabulations represent incorrect verbal expressions to questions or situations in which an amnesic patient feels compelled to respond. They appear to be plausible and resemble the false memories produced by healthy individuals (Heidler and Eling Citation2015). In contrast, spontaneous confabulations often occur without any obvious trigger, and patients might act upon their ideas (Gilboa et al. Citation2006). Spontaneous confabulations are a relatively rare phenomenon in brain-damaged samples, often occurring in the context of a severe amnesic syndrome (Kopelman Citation1987).
Confabulations have been reported in a variety of neuropsychiatric disorders, such as schizophrenia, Alzheimer’s dementia, and Traumatic Brain Injury (Dalla Barba et al. Citation2019; Johnson et al. Citation2000). Yet, patients with Korsakoff’s syndrome (KS) are most noted for their confabulation behaviour. In addition, the Amnesic-Confabulatory Subtype of Major Neurocognitive Disorder is a classification subcategory in the DSM-5 (American Psychiatric Association Citation2013), which is used for individuals with KS. KS is a chronic neuropsychiatric disorder, characterised by severe declarative, anterograde amnesia, and confabulations (Arts et al. Citation2017). Patients that develop KS have a history of profound thiamine deficiency, usually following chronic alcoholism or other conditions that lead to malnutrition (Oudman et al. Citation2018, Citation2019). Because of the severity of cognitive and somatic problems, patients with KS are in need of lifelong specialised care. In the Netherlands, many chronic KS patients reside in long-term care facilities, such as nursing homes and other protected- or assisted-living facilities (Oudman and Zwart Citation2012; Arts et al. Citation2017).
Instruments developed for assessing confabulations include the Dalla Barba Confabulation Battery (Dalla Barba et al. Citation2019), the Provoked Confabulations Test (PCT, Cooper et al. Citation2006), and most recently the Nijmegen Venray Confabulation List (NVCL-R, Rensen et al. Citation2015; Rensen et al. 2020). Of interest, the NVCL-R covers both spontaneous and provoked confabulations through systematic behavioural observations by informants who know the patient well (e.g., members of the professional care staff), and has recently been used to index treatment efficiency for patients with KS in Errorless Learning treatment programs (Rensen et al. Citation2019a, Citation2019b). Important advantages of this instrument over earlier instruments are the inclusion of items assessing spontaneous confabulations, the short administration time, not having to burden the patient directly, and the validated factor structure (Rensen et al. 2020).
The existing anecdotal literature on confabulations in KS reports that confabulations in patients with KS are transient, and mainly occur in the acute phase of the illness (see Arts et al. Citation2017, for a review). Based on early case descriptions, Emil Kraepelin (Citation1910) observed that confabulations were particularly prominent in the first phase of the illness, yet subsequently disappeared. Later, Talland (Citation1961) also referred to the absence of confabulations in the majority of patients in the chronic stage of KS. More recently, Kopelman (Citation2015) reviewed the existing literature on spontaneous confabulations following thalamic infarctions and KS, and concluded that specifically spontaneous confabulations are prominent in acute Wernicke’s encephalopathy, but tend to be seen only in a selective subsample of patients in the chronic stage of KS. This was also reported by Kessels et al. (Citation2008), who reported that all patients included in their study (all acute KS patients; in their first six months after diagnosis), displayed spontaneous confabulation behaviour as well as provoked confabulation behaviour. One recent study included one KS patient as part of a sample of confabulating patients, and showed relative stability of confabulations in this patient (Dalla Barba et al. Citation2017). We will discuss this paper in the next paragraph. Since long-term care for chronic KS patients did not receive much attention in the academic literature so far, and patients are often discharged to their home or do not have access to long-term health-care facilities (see for example Kopelman et al. Citation2009; Isenberg-Grzeda et al. Citation2012), the actual time course of confabulations in KS has not been the topic of systematic investigation.
Although the time course of confabulations has not previously been systematically investigated in KS patients, three studies have examined the time course in other brain damaged populations. Schnider et al. (Citation2000) investigated the clinical course and recovery of spontaneous confabulations in eight brain-injured patients. Four were diagnosed with traumatic brain injury, three had a subarachnoid haemorrhage, and one an olfactory meningioma leading to spontaneous confabulations. One patient still showed signs of spontaneous confabulation two years post-onset, but seven stopped confabulating in a spontaneous manner within the two years post-onset. More recently, Dalla Barba et al. (2017) applied the Dalla Barba Confabulation Battery in a sample of 13 severely confabulating patients with diverse aetiologies, and 13 matched controls. Seven patients had cerebrovascular problems causing diffuse lesions, two patients had had anoxia, one patient had an intracranial tumour, and one patient had a diagnosis of KS. In this chronic sample, provoked confabulations were stable. Bajo et al. (Citation2017) investigated the chronicity of provoked confabulations in 46 patients with diverse aetiologies of brain injury between six months and fifteen months post-onset. They demonstrated a general tendency of decline of confabulations over time, although some patients still showed confabulations after 15 months.
To date, these early observations are still the leading view on chronicity of confabulations in KS in the post-acute phase, while empirical evidence on confabulations in post-acute KS is lacking in most systematic studies and case reviews. The aim of the present cross-sectional study is to assess the nature of confabulations over the course of alcoholic KS. We assessed confabulations in a large sample of post-acute and chronic patients diagnosed with KS. All post-acute patients were observed in a diagnostic expertise centre, and all chronic patients were residing in a 24/7-long-term care facility for KS patients.
Methods
Participants
The NVCL-R was completed for 172 patients with Korsakoff’s syndrome (133 men, Mage = 60 years old; range 36−82). The data were collected at the Centre of Excellence for Korsakoff and Alcohol-Related Cognitive Disorders of Vincent van Gogh Institute for Psychiatry in Venray, The Netherlands and Lelie Care group, Korsakoff Centre Slingedael, Rotterdam, The Netherlands. The Vincent van Gogh Centre is a diagnostic expertise centre. Patients who are admitted to the centre typically are in the post-acute phase of their illness (e.g., after hospitalisation because of malnutrition and/or confusion). On the other hand, chronic patients reside at a Korsakoff Centre Slingedael, a long-term 24/7-care facility for KS patients already diagnosed with KS. The mean time since admittance to Vincent van Gogh was 1.9 months (SD = 0.8), Patients were admitted to the rehabilitation unit within one to four weeks following admission to an acute hospital. The mean time since admittance to Lelie Care group was 66.5 months (SD = 36.7). The average time of admittance was 29 months (range 1 month to 162 months). Data were collected between March 2011 and March 2020. All patients were at least 6 weeks abstinent from alcohol when the NVCL-R was completed by professional caregivers (e.g., psychiatric nurses). Level of education was measured within the Dutch educational system using a 7-point rating scale, ranging from 1 (less than primary education) to 7 (university degree). The patients had a median education level of 4 (range 1 to 7).
To be eligible for inclusion, patients had to meet the DSM-5 criteria for Alcohol-induced Major Neurocognitive Disorder (American Psychiatric Association Citation2013) and be diagnosed as having Korsakoff’s syndrome in accordance with the criteria outlined in Kopelman (Citation2002), which includes evidence of a history of malnutrition or thiamine deficit. All patients were abstinent from alcohol for at least 6 weeks at the time of testing. None of the patients had any evidence of brain pathology other than alcohol use that would account for their memory deficit (e.g., stroke, tumour). None of the patients met the criteria for major depressive disorder. In addition, patients with evidence of other cognitive disorders (agnosia, aphasia or apraxia) were excluded. The data included in this manuscript were obtained as part of clinical routine and stored and analysed anonymously in accordance with the institutional guidelines, the Helsinki Declaration, and the EU General Data Protection Regulation (GDPR).
Materials and procedure
The NVCL–R is an observation scale consisting of 18 items (Rensen et al. 2020). The items cover various aspects of four factors: Spontaneous confabulations (items 1–6), Severity of spontaneous confabulations (items 7, 8), provoked confabulations (items 9–16), and distorted sense of reality (17, 18). The factor structure was confirmed in a recent study (Rensen et al. 2020). Professional caregivers (such as psychiatric nurses, primary responsible carers) who knew the patients well rated the confabulation behaviour on a 5-point rating scale, with higher scores reflecting more confabulations. The caregivers first carefully read the instruction, which emphasised the purpose of the instrument, namely to assess provoked and spontaneous confabulations. It took about 5–10 minutes to complete the observation scale.
Statistical analyses
Spontaneous confabulation is a rare phenomenon. Hence, when patients received a score of 1 or more on any of the questions tapping spontaneous confabulations, the patient was classified as a ‘spontaneous confabulator’. Patients were also divided into ‘provoked’ (score of 4 or more on the questions tapping provoked confabulations) and ‘non-provoked’ confabulators. Non-parametric analyses were performed (chi-square, two-tailed) to compare the number of ‘spontaneous’ and ‘non-spontaneous’ confabulators and the number of ‘provoked’ and ‘non-provoked’ confabulators. Spearman correlation coefficients (two-tailed) were calculated between the time of admittance and time since diagnosis and spontaneous and provoked confabulation scores on the NVCL-R. Alpha was set at .05 throughout.
Results
Spontaneous and provoked confabulations
The number of spontaneous and provoked confabulators and non-confabulators on the NVCL-R across the two Centres (Vincent van Gogh and Lelie Care group) are presented in . Out of the total sample of 172 patients, 112 patients were rated as ‘spontaneous confabulators’ (score ≥ 1 on the spontaneous confabulation scale of the NVCL-R). Moreover, 141 were rated as ‘provoked confabulators’ (score ≥ 4 on the provoked confabulation scale of the NVCL-R). In total, 101 patients were rated as both ‘spontaneous confabulators’ and ‘provoked confabulators’.
Table 1. The number of spontaneous and provoked confabulators and non-confabulators (% between brackets) on the NVCL-R in short-term and long-term care.
The spontaneous confabulators did not differ significantly from the non-spontaneous confabulating patients in age, educational level or sex distribution. However, the spontaneous confabulators showed longer admittance durations (M = 36.0 months) than the non-spontaneous confabulators (M = 15.7 months) (F(1,170) = 10.79, p = .001). Relatively more spontaneous confabulators (χ2(1, N = 172) = 10.76, p = .001) and provoked confabulators (χ2(1, N = 172) = 5.87, p < .05) were found in the Lelie Care Group sample compared with the Vincent van Gogh sample. These findings suggest more confabulations in the chronic than in the post-acute patients.
Correlations
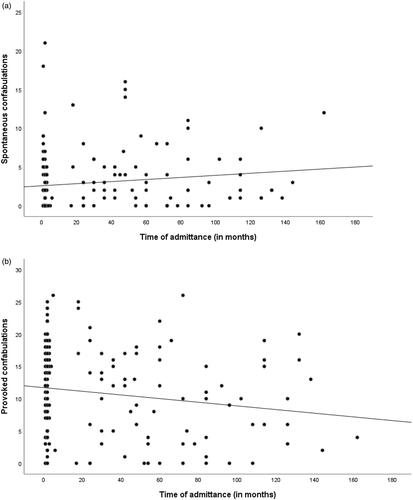
Correlations between duration of admittance and the extent of spontaneous and provoked confabulations are presented in . We found a small-to-medium, positive correlation between the duration of admittance and spontaneous confabulations on the NVCL-R (rs = .20, p = .010). Moreover, the severity of spontaneous confabulations on the NVCL-R was significantly related to the duration of admittance (rs = .175, p = .022). The duration of admittance was not related to the provoked confabulations (rs = −.113, p = .141) or the distorted sense of reality (rs = −.108, p = .158) on the NVCL-R.
Discussion
The aim of the present study was to assess the nature of confabulations in post-acute and chronic KS patients. We assessed spontaneous and provoked confabulations in a large cross-sectional sample of post-acute and chronic patients diagnosed with KS. Within the chronic group receiving long-term 24/7-care, more spontaneous and provoked confabulators were present than in the post-acute group. Moreover, the level of spontaneous confabulations was significantly related to the time since admittance in the correlational analysis. Of importance, the level of spontaneous and provoked confabulations in sub-acute KS patients was comparable to earlier studies on confabulations in KS (Rensen et al. 2015; Rensen et al. Citation2019b). Together, these results suggest that provoked and spontaneous confabulations do not extinguish in all KS patients, but are often found in patients receiving intensive long-term care because of the severity of the syndrome.
Our finding that patients with KS showed provoked and spontaneous confabulations, even in the chronic stage of KS is in contrast to the traditional finding that confabulations tend to become less prominent over time (Kraepelin Citation1910; Talland Citation1961; Kopelman Citation2015). Earlier research in patients with traumatic brain injury suggested that provoked confabulations may be chronic, while spontaneous confabulations are more likely to diminish over time (Schnider et al. Citation2000; Bajo et al. Citation2017; Dalla Barba et al. 2017).
Remarkedly, in the present study, the patients with chronic KS residing in a long-term care facility displayed even more spontaneous and provoked confabulations than the post-acute patients in an expertise centre for diagnostics. We do not assume that confabulations progressively get worse over time, but that this might partly be the result of the selected patient groups. In the expertise centre for diagnostics, the Korsakoff sample is more heterogenous with regards to the level of cognitive (dys)functioning. Some patients with KS are higher functioning and able to return to their homes with the help of a spouse and organised daytime activities, or might move to assisted living facilities. On the other hand, the cognitively lower-functioning patients are in need of 24/7 professional care and are admitted to nursing homes, such as the Korsakoff Centre Slingedael. Hence, the chronic KS group in this study likely consists of a relatively less autonomous and more severely cognitively compromised group than patients seen at the diagnostic centre. For future studies, it would be relevant to include a measure of cognitive functioning. Multiple studies have showed that the MoCA is a valuable tool in differentiating patients with KS from healthy subjects and patients with chronic alcohol use with cognitive disorders (Oudman et al. Citation2014; Bruijnen et al. Citation2019). ; Moreover, it would be relevant to monitor confabulations over time in the same sample of patients.
In earlier literature, the existence of provoked confabulations seems likely to be driven by faulty memory in individuals with amnesia, while spontaneous confabulations may represent a distorted reality and the tendency to act on this distortion (Schnider Citation2008). In neuropsychiatric disorders, it is important to note that spontaneous confabulations are functionally discrepant from delusions, most specifically because the produced statements or behaviours in confabulations could actually have been true, and the nature of confabulations is less rigid than in delusions (Fotopoulou Citation2010). Although delusions and confabulations both are factually incorrect, confabulations often have a changing nature based on the context while delusions tend to generalise over multiple contexts (Kopelman Citation2010; Lorente-Rovira et al. Citation2011). Moreover, delusion is commonly defined as a false belief and associated with psychiatric disorders like schizophrenia, whereas confabulation is typically described as a false memory and associated with neurological disorders such as alcoholic Korsakoff’s syndrome (Langdon and Turner Citation2010). Whether confabulations and delusions are on the same continuum, or whether these are two largely independent concepts remains unclear. Of importance, our present findings highlight the chronic nature of provoked and spontaneous confabulations, suggesting a chronicity that is also common for untreated delusions (Velligan et al. Citation1997).
A limitation of the present study is that we included two different samples of KS patients, adopting a cross-sectional approach. In follow-up longitudinal research a general sample of patients with KS diagnosed in one facility could be systematically observed to establish the course of confabulation behaviour over time. A second limitation is the lack of background neuropsychological variables for or sample. One of the strengths of this study is that we applied a robust and reliable index of confabulations that has recently been validated in a large group of KS patients (Rensen et al. 2020). Also, we included a relatively large sample of KS patients, supporting the notion that confabulations are prominent throughout KS.
In conclusion, in contrast to the traditional view, confabulations form an integral aspect of KS over the course of the disease, and are still present even years after the syndrome’s onset. We suggest that KS patients with a more unfavourable outcome are likely to display more confabulations.
Author contributions
E.O. designed the study and acquired the data, which all authors analysed. All authors wrote the article and revised it. All authors contributed to and have approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders. 5th ed. Washington (DC): APA.
- Arts NJM, Walvoort SJW, Kessels RPC. 2017. Korsakoff's syndrome: a critical review. NDT. 13:2875–2890.
- Bajo A, Fleminger S, Metcalfe C, Kopelman MD. 2017. Confabulation: what is associated with its rise and fall? A study in brain injury. Cortex. 87:31–43.
- Bruijnen CJWH, Jansen M, Dijkstra BAG, Walvoort SJW, Lugtmeijer S, Markus W, de Jong CAJ, Kessels RPC. 2019. The Montreal Cognitive Assessment (MoCA) as a cognitive screen in addiction health care: a validation study for clinical practice. Journal of Substance Use. 24:47–54.
- Cooper JM, Shanks MF, Venneri A. 2006. Provoked confabulations in Alzheimer's disease. Neuropsychologia. 44:1697–1707.
- Dalla Barba G, Brazzarola M, Marangoni S, Barbera C, Zannoni, I. 2017. A longitudinal study of confabulation. Cortex 87:44–51.
- Dalla Barba G, Guerin B, Brazzarola M, Marangoni S, Barbera C, La Corte V. 2019. The confabulation battery: instructions and international data from normal participants. Neuropsychol Rehabil. 29:1625–1636.
- Fotopoulou A. 2010. The affective neuropsychology of confabulation and delusion. Cogn Neuropsychiatry. 15:38–63.
- Gilboa A, Alain C, Stuss DT, Melo B, Miller S, Moscovitch M. 2006. Mechanisms of spontaneous confabulations: a strategic retrieval account. Brain. 129:1399–1414.
- Heidler MD, Eling PATM. 2015. Puzzling confabulations: an overview of classifications and theories. Zeitschrift Für Neuropsychologie. 26:257–270.
- Isenberg-Grzeda E, Kutner HE, Nicolson SE. 2012. Wernicke-Korsakoff-Syndrome: under-recognized and under-treated. Psychosomatics. 53(6):507–516. doi:10.1016/j.psym.2012.04.008.
- Johnson MK, Hayes SM, d'Eposito MD, Raye CL. 2000. Confabulation. Handbook of Neuropsychol. 2(2): 383–407. Elsevier: Amsterdam, The Netherlands.
- Kessels RPC, Kortrijk HE, Wester AJ, Nys GMS. 2008. Confabulation behavior and false memories in Korsakoff's syndrome: role of source memory and executive functioning. Psychiatry Clin Neurosci. 62:220–225.
- Kopelman MD. 1987. Two types of confabulation. J Neurol Neurosurg Psychiatry. 50:1482–1487.
- Kopelman MD. 2002. Disorders of memory. Brain. 125:2152–2190.
- Kopelman MD. 2010. Varieties of confabulation and delusion. Cogn Neuropsychiatry. 15:14–37.
- Kopelman MD. 2015. What does a comparison of the alcoholic Korsakoff syndrome and thalamic infarction tell us about thalamic amnesia? Neurosci Biobehav Rev. 54:46–56.
- Kopelman MD, Thomson AD, Guerrini I, Marshall EJ. 2009. The Korsakoff syndrome: clinical aspects, psychology and treatment. Alcohol Alcohol. 44:148–154.
- Kraepelin E. 1910. Psychiatrie: Ein Lehrbuch für Studierende und Ärzte. Achte, vollständig umgearbeitete Auflage. II. Band. Klinische Psychiatrie. I. Teil. Leipzig (Germany): Barth.
- Langdon R, Turner M. 2010. Delusion and confabulation: overlapping or distinct distortions of reality? Cogn Neuropsychiatry. 15:1–13.
- Lorente-Rovira E, Berrios G, McKenna P, Moro-Ipola M, Villagrán-Moreno JM. 2011. Confabulations (I): concept, classification and neuropathology. Actas Esp Psiquiatr. 39:251–259.
- Oudman E, Zwart E. 2012. Quality of life of patients with Korsakoff's syndrome and patients with dementia: a cross-sectional study. J Am Med Dir Assoc. 13:778–781.
- Oudman E, Postma A, Van der Stigchel S, Appelhof B, Wijnia JW, Nijboer TCW. 2014. The Montreal Cognitive Assessment (MoCA) is superior to the Mini Mental State Examination (MMSE) in detection of Korsakoff's syndrome. Clin Neuropsychol. 28:1123–1132.
- Oudman E, Wijnia JW, Oey M, van Dam M, Painter RC, Postma A. 2019. Wernicke's encephalopathy in hyperemesis gravidarum: a systematic review. Eur J Obstet Gynecol Reprod Biol. 236:84–93.
- Oudman E, Wijnia JW, van Dam M, Biter LU, Postma A. 2018. Preventing Wernicke encephalopathy after bariatric surgery. Obes Surg. 28:2060–2068.
- Rensen YCM, Egger JIM, Westhoff J, Walvoort SJW, Kessels RPC. 2019a. Errorless (re)learning of everyday activities in patients with Korsakoff's syndrome: a feasibility study. Neuropsychol Rehabil. 29:1211–1225.
- Rensen YCM, Egger JIM, Westhoff J, Walvoort SJW, Kessels RPC. 2019b. The effect of errorless learning on psychotic and affective symptoms, as well as aggression and apathy in patients with Korsakoff's syndrome in long-term care facilities. Int Psychogeriatr. 31:39–47.
- Rensen YC, Oosterman JM, van Damme JE, Griekspoor SI, Wester AJ, Kopelman MD, Kessels RP. 2015. Assessment of confabulation in patients with alcohol-related cognitive disorders: The Nijmegen–Venray Confabulation List (NVCL-20). Clin Neuropsychol. 29(6):804–823.
- Rensen YCM, Oudman E, Oosterman JM, Kessels RPC 2020. Confabulations in alcoholic Korsakoff's syndrome: a factor analysis of the Nijmegen-Venray Confabulation List. Assessment. 1073191119899476.
- Schnider A. 2008. The confabulating mind. How the brain creates reality. Oxford: Oxford University Press.
- Schnider A. 2018. The confabulating mind: how the brain creates reality. Oxford (UK): Oxford University Press.
- Schnider A, Ptak R, von Däniken C, Remonda L. 2000. Recovery from spontaneous confabulations parallels recovery of temporal confusion in memory. Neurology. 55:74–83.
- Talland GA. 1961. Confabulation in the Wernicke-Korsakoff syndrome. J Nerv Ment Dis. 132:361–381.
- Velligan DI, Mahurin RK, Diamond PL, Hazleton BC, Eckert SL, Miller AL. 1997. The functional significance of symptomatology and cognitive function in schizophrenia. Schizophr Res. 25:21–31.