Abstract
Objective
Anxious distress (ANXD), which is common in major depressive disorder (MDD), is associated with poor outcomes. We investigated clinical characteristics of MDD patients with the DSM-5 ANXD specifier and only mild residual symptoms without comorbid anxiety disorders in the continuation/maintenance phase.
Methods
We recruited 110 outpatients with MDD without comorbid anxiety disorders. They were interviewed; the presence of the DSM-5 ANXD specifier was assessed. They completed the Quick Inventory of Depressive Symptomatology (QIDS), the Eysenck Personality Questionnaire (S-EPQ), the Temperament Evaluation of Memphis, Pisa, Paris and San Diego-Autoquestionnaire (TEMPS-A).
Results
The mean QIDS total score was 9.7 ± 5.5. The DSM-5 ANXD specifier was identified in 73 patients (66.4%). A univariate analysis indicated ANXD was significantly associated with younger age; unmarried status; living alone; higher QIDS total score; higher S-EPQ neuroticism score; and higher TEMPS-A cyclothymic, depressive and irritable scores. After covariate adjustment, a multivariable linear regression analysis revealed a significant association between the QIDS total score and ANXD (three different models).
Conclusion
The DSM-5 ANXD was also common among MDD patients without comorbid anxiety disorders in the continuation/maintenance phase; it was significantly associated with greater depression severity and might be related to temperament associated with bipolar disorder.
DSM-5 anxious distress is common among MDD patients without comorbid anxiety disorders in the continuation/maintenance phase and correlated with some of their socio-demographic and clinical characteristics. • The presence of DSM-5 anxious distress was significantly associated with greater severity of depression and might be related to temperament associated with bipolar disorder.
• The evaluation of the DSM-5 anxiety distress was revealed to have some significance not only in the acute phase but also in the continuation/maintenance phase of MDD.
Key points
Introduction
The importance of anxiety in patients with major depressive disorder (MDD) has been recognised and discussed for nearly a century. Compared to depressed patients without anxiety, depressed patients with high levels of anxiety are characterised by higher levels of suicidal ideation and suicide attempts (Fava et al. Citation2006; Seo et al. Citation2011; Goes et al. Citation2012), poorer functioning (Fichter et al. Citation2009; Lin et al. Citation2014), poorer health-related quality of life (Lin et al. Citation2014; Rhebergen et al. Citation2011), and greater chronicity (Coryell et al. Citation1988; Melartin et al. Citation2002; Fichter et al. Citation2009; Rhebergen et al. Citation2011). In recognition of the clinical significance of anxiety in depressed patients, the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5) (American Psychiatric Association [APA] 2013) introduced an anxious distress specifier as a method of subtyping MDD.
Several studies have supported the validity of the DSM-5's anxious distress specifier (McIntyre et al. Citation2016a, Citation2016b; Shim et al. Citation2016; Gaspersz et al. Citation2017a, Citation2017b; Maneeton et al. Citation2017; Zimmerman et al. Citation2019), but in some of these studies (McIntyre et al. Citation2016a, Citation2016b; Shim et al. Citation2016), not all of the criteria of the DSM-5 anxious distress specifier were assessed, and in other studies (Gaspersz et al. Citation2017a, Citation2017b), the authors noted that some of the proxy items that were part of an already existing database may not have been accurate representations of a DSM-5 criterion.
Zimmerman et al. (Citation2017) examined the validity of the DSM-5 anxious distress specifier for MDD by administering the DSM-5 Anxious Distress Specifier Interview (DADSI). They reported that approximately three-quarters of their depressed patients met the criteria for the anxious distress specifier. The patients with anxious distress had a higher frequency of anxiety disorder as well as higher scores on measures of anxiety and depression, higher rates of drug use disorders, and poorer functioning during the week before the evaluation.
Some investigators have suggested that anxious distress in MDD has some relationships with bipolarity (Sugawara et al. Citation2019; Tundo et al. Citation2019). For example, psychomotor agitation has been defined as a severe form of anxious distress (APA Citation2013), and psychomotor agitation in MDD is reportedly related to bipolarity (Iwanami et al. Citation2015). The clarification of the boundaries between anxious distress and bipolarity could also have important implications for the treatment of depression, primarily in terms of the use of antidepressants.
To the best of our knowledge, most of the reported studies included MDD patients with comorbid anxiety disorders in the acute phase (McIntyre et al. Citation2016a, Citation2016b; Shim et al. Citation2016; Maneeton et al. Citation2017; Gaspersz et al. Citation2017a, Citation2017b; Zimmerman et al. Citation2017, Citation2019). It is difficult to determine whether anxiety disorder or anxious distress has a greater influence on the present symptoms and outcome of MDD when anxiety disorder and anxious distress are present at the same time. We wanted to discern the meaning of anxious distress in MDD independently of comorbid anxiety disorders and the meaning of anxious distress in the continuation/maintenance phase of MDD patients with only mild residual symptoms. It is not well understood how anxious distress among MDD patients without comorbid anxiety disorders in the continuation/maintenance phase is related to socio-demographic and clinical characteristics. If the relationships between these parameters and anxious distress can be established, it could improve the treatment of MDD patients with anxious distress. We conducted the present study to examine the socio-demographic and clinical characteristics (including temperament associated with bipolar disorder) of patients with DSM-5 anxious distress among MDD patients without comorbid anxiety disorders in the continuation/maintenance phase.
We hypothesised that the assessment of the DSM-5 anxious distress specifier may also be significant among MDD patients without other anxiety disorders in the continuation/maintenance phase.
Patients and methods
Patients
The patients were recruited from the pool of general outpatients at the Department of Psychiatry of JCHO Tokyo Shinjuku Medical Centre during the period from October 2016 to March 2017. To be included in the study, the patient had to be: (i) aged 20–79 years, (ii) Japanese, (iii) meeting the DSM-5 criteria for MDD, (iv) able to provide written consent, (v) treated for >6 months since the first visit, and (vi) prescribed a fixed dose of a psychotropic agent for ≥3 months. We planned to conduct this study among MDD patients who were confirmed to be in the continuation/maintenance phase with only mild residual symptoms.
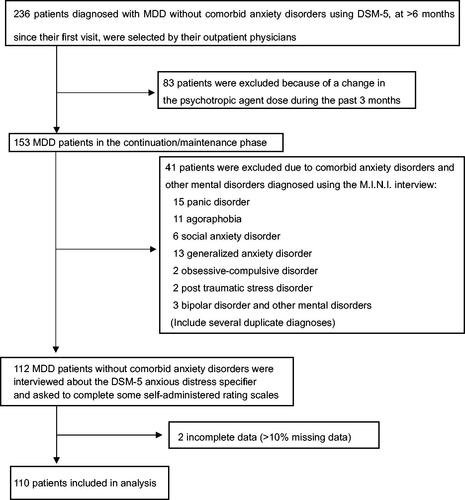
The exclusion criteria were the presence of: (i) a mood disorder due to a medical condition and/or substance; (ii) psychotic or bipolar disorder; (iii) anxiety disorder (panic disorder, agoraphobia, social anxiety disorder, generalised anxiety disorder); (iv) obsessive–compulsive disorder; (v) post-traumatic stress disorder; (vi) substance abuse or dependence; (vii) clinically significant cognitive impairment; (vii) organic brain damage; (viii) antisocial personality; (ix) severe physical problems; and (x) severe suicidality. The patient selection process is illustrated in .
Procedures
The patients were interviewed by four trained psychiatrists to obtain their clinical history and diagnostic assessment. For the diagnostic assessment, we used the Mini International Neuropsychiatric Interview (M.I.N.I.) (Sheehan et al. Citation1998; Otsubo et al. Citation2005). We collected the patients' socio-demographic and retrospective clinical data, information on their family history of mood disorders in first-degree relatives, divorce history, illness duration, number of previous episodes, suicide attempts in current or previous episodes, hospitalisation, and alcohol and/or tobacco use. Whenever possible, we used secondary clinical data obtained from other informants as well as available past medical records to support each patient's information.
We used a semi-structured interview format to assess the DSM-5 anxious distress specifier in accordance with the Japanese version of the DSM-5, which requires the presence of at least two of the following five symptoms for the majority of the patient's depressive episode: (1) feeling ‘keyed up’ or tense, (2) feeling unusually restless, (3) difficulty concentrating because of worry, (4) fear that something awful might happen, and (5) feeling that the individual might lose control of himself or herself. In this study, if a symptom was observed during more than half of the current depressive episode, it was considered ‘present’. Several training sessions were conducted for the raters regarding how to ask questions and make judgments.
Instruments
The patients completed the Quick Inventory of Depressive Symptomatology (QIDS) (Trivedi et al. Citation2004), the short form of the Eysenck Personality Questionnaire (S-EPQ) (Miyaoka et al. Citation1999), the short version of the Temperament Evaluation of Memphis, Pisa, Paris and San Diego-Autoquestionnaire (TEMPS-A) (Erfurth et al. Citation2005; Nakato et al. Citation2016), and the Sheehan Disability Scale (SDS) (Sheehan et al. Citation1996).
Quick inventory of depressive symptomatology (QIDS)
The QIDS contains 16 items and was designed to measure the overall severity of the depressive syndrome (in this case, MDD) by assessing each of the nine symptom domains that define the syndrome (Trivedi et al. Citation2004). Four items are used to assess the sleep domain (initial, middle, and late insomnia, as well as hypersomnia). Two items are used to gauge psychomotor activity (agitation and retardation). Four items assess the appetite/weight domain (e.g., appetite increase and decrease, weight increase and decrease). For each of these three domains, the highest rating on any one relevant item is used to score the domain (range 0–3). Only one item is used to score the remaining six criterion domains (each rated 0–3: sad mood, concentration, energy, interest, guilt, and suicidal ideations/intent). The QIDS total score ranges from 0 to 27.
Short form of the Eysenck personality questionnaire (S-EPQ)
The S-EPQ is an instrument developed by J.H. Eysenck to assess personality, especially the traits of neuroticism (N) and extroversion (E) (Miyaoka et al. Citation1999). The S-EPQ, containing only 12 questions (six for N and six for E), can be completed in 3 min. The original S-EPQ comprises yes–no questions. The Japanese version was slightly modified, using four response choices. The respondent is asked to what degree he or she agrees with each of the statements with respect to their personality (4 = markedly, 3 = moderately, 2 = slightly, 1 = never). The scores for the S-EPQ-N and the S-EPQ-E each range from 6 to 24.
Temperament evaluation of Memphis, Pisa, Paris and San Diego-Autoquestionnaire (TEMPS-A)
Temperament was assessed using the short version of the TEMPS-A (Erfurth et al. Citation2005). This self-report questionnaire includes 39 items rated on a Likert scale ranging from 1 to 5 (1 = not at all, 2 = a little, 3 = moderately, 4 = much, 5 = very much) that evaluate affective temperaments, including predominantly cyclothymic, depressive, irritable, hyperthymic, and anxious subtypes. The original 39-item short version of the TEMPS-A was extracted from the full English version and developed by H.S. Akiskal et al. and then translated into French, Italian, Chinese, and Japanese (Nakato et al. Citation2016).
Sheehan Disability Scale (SDS)
The SDS was used to measure the patients' functioning. The SDS is a brief self-report inventory with three domains of functioning: work/school, social life, and family life. On each domain, the patient rates his/her functioning from 0 to 10 (Sheehan et al. Citation1996). Anchor scores are 0 = no impairment, 1–3 = mild impairment, 4–6 = moderate impairment, 7–9 = marked impairment, and 10 = extreme impairment. The level of global functioning was determined using the sum of the three domains.
Statistical analyses
The continuous variables in this study are presented as the mean ± SD. The categorical variables are presented as the number (%). The differences between groups were analysed using independent Student's t-tests for normally distributed variables, and the Chi-square test for categorical data. We performed a multiple linear regression analysis with adjustment for potential predictors to assess the relationship between the QIDS total score and anxious distress in three different models.
The potential predictors included in the multiple linear regression analysis were the anxious distress specifier only (model 1); model 1 plus gender, age, number of depressive episodes, and living with family (model 2); model 2 plus the scores on the S-EPQ-N, the TEMPS-A cyclothymic, hyperthymic, and anxious subtypes, and the SDS total score (model 3). The number of variables input to the general linear model was adjusted by the number of patients analysed. The scores of N and E in the S-EPQ were highly correlated, and we thus selected the N score. The scores of the cyclothymic, depressive, and irritable subtypes in the TEMPS-A were highly correlated; we thus selected the cyclothymic score. The scores of work/school, social life, and family life/home responsibilities in the SDS were highly correlated, and we therefore used the total score of the SDS. All analyses were conducted using SPSS software ver. 24 J for Windows (SPSS, Chicago, IL).
Ethical considerations
This study was approved by the institutional review committee at JCHO Tokyo Sinjuku Medical Centre and conducted in accord with the Helsinki Declaration of 1975. Written informed consent for the anonymous use of clinical records and publication of this study was obtained from all patients prior to their inclusion in this study. This study is registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN 000029417).
Results
The patient series was 110 patients; 62.7% were female and 48.2% were employed. The mean age was 55.6 ± 14.4 years, the mean educational level was 14.4 ± 2.3 years, the mean QIDS total score was 9.7 ± 5.5, and the mean SDS total score was 7.3 ± 7.2.
The DSM-5 anxious distress specifier occurred in 66.4% (73/110) of the patients with MDD without comorbid anxiety disorders. The frequencies of the five individual specifier items ranged from 35.5% to 73.6%, and psychomotor agitation was identified in 22.3% of the patients (). In the entire sample, the most common symptom was difficulty concentrating due to worry; the least common symptom was feeling that individual might lose control of him- or herself (). The Cronbach's alpha coefficients were as follows: the anxious distress specifier (0.73); the QIDS (0.84); the S-EPQ-N (0.82); the S-EPQ-E (0.75); the cyclothymic (0.81), depressive (0.71), irritable (0.70), hyperthymic (0.74), and anxious (0.56) items of the TEMPS-A, and the SDS (0.85). All of these values exceeded the threshold of internal consistency (0.70), with the exception of the anxious score on the TEMPS-A.
Table 1. The DSM-5 anxious distress specifier in patients with MDD (n = 110).
Based on the results of the univariate analysis, the socio-demographic and clinical characteristics significantly associated with anxious distress were younger age; unmarried status; living with no family (living alone); higher QIDS total score; higher S-EPQ-N score; higher cyclothymic, depressive, and irritable scores on the TEMPS-A; and higher dose of antidepressant/antipsychotic ().
Table 2. Socio-demographic factors in MDD patients with and without anxious distress.
Table 3. Clinical differences in MDD patients with and without anxious distress.
Table 4. Pharmacotherapy in MDD patients with and without anxious distress.
demonstrates the significant association between the QIDS total score and anxious distress. After the adjustment for covariates, a multivariable linear regression analysis consistently showed a significant association between the QIDS total score and anxious distress, in all three models. In model 3, the S-EPQ N-score, the cyclothymic score on the TEMPS-A, and the total score on the SDS were also significantly associated with the QIDS total score.
Table 5. Results of multivariable linear regression analysis with QIDS total score as the dependent variable in three models.
Discussion
Our findings suggest that DSM-5 anxious distress is common in and correlated with some socio-demographic and clinical characteristics of Japanese MDD patients without comorbid anxiety disorders in the continuation/maintenance phase. The mean QIDS total score was 9.7 ± 5.5, which is considered to reflect mild to moderate residual symptoms. Anxious distress was associated with younger age, unmarried status, living alone, greater severity of depression, higher dose of antidepressants/antipsychotics, higher neuroticism personality, and higher cyclothymic temperament.
The prevalence of DSM-5 anxious distress in our patient series (66.4%) confirms previous reports that anxious distress is common among MDD patients. The percentage of MDD patients with anxious distress was 59.1% in a study by McIntyre et al. (Citation2016b), 54.2% as reported by Gaspersz et al. (Citation2017a), 74.8% in the series described by Maneeton et al. (Citation2017), and 78.1% in an investigation by Zimmerman et al. (Citation2019). In these studies, with the exception of the Zimmerman et al. (Citation2019) study, the authors noted that some of the proxy items that were part of an already existing database may not have been accurate representations of the DSM-5 criteria (Gaspersz et al. Citation2017a, Citation2017b; Maneeton et al. Citation2017). In the present analyses, we accurately assessed the DSM-5 criteria of the anxious distress specifier, and the results revealed a high prevalence rate of anxious distress in Japanese patients with MDD alone in the continuation/maintenance phase. Moreover, in the above-cited studies, except that of Zimmerman et al. (Citation2019), the proxy assessment of the DSM-5 criteria was cross-sectional based on symptom presence during the past week. We assessed all symptoms according to the DSM-5 definition, and if the symptom was observed during more than half of the current depressive episode, we judged the symptom as present. Although this is a retrospective confirmation, it is important to check whether the symptoms were present during more than half of the current episode.
In our entire sample, the most common symptom was difficulty concentrating due to worry. Gaspersz et al. (Citation2017a) stated that the most common symptom in their patient series was feeling keyed up or tense. In our sample, the Cronbach's α of this specifier was moderate (0.73) and almost the same as that reported by Gasperz et al. (2017b) at 0.71 and slightly lower than the 0.79 reported by Zimmerman et al. (Citation2014).
Our patients with anxious distress were significantly younger than those without anxious distress. Maneeton et al. (Citation2017) also observed that their patients with anxious distress were significantly younger than those without it. Conversely, McIntyre et al. (Citation2016b) and Gaspersz et al. (Citation2017a) reported that their patients with anxious distress were older than those without anxious distress. According to the famous STAR*D study (Husain et al. Citation2005), symptoms of anxiety and irritability are more frequent in younger adults with MDD compared to older individuals.
We observed herein that anxious distress was associated with unmarried status and with living alone. Zimmerman et al. (Citation2019) noted that in their patient population, the rate of married status was lower among the patients with anxious distress compared to those without it. However, there was no significant difference in marital status between the patients with and without anxious distress in the study by McIntyre et al. (Citation2016b), and Tundo et al. (Citation2019) noted that their patients with anxious distress were more frequently married compared to those without anxious distress. After controlling for demographic variables and other sources of distress, Beutel et al. (Citation2017) reported that loneliness (i.e., living alone) was associated with depression, generalised anxiety, and suicidal ideation. Unmarried status and/or living alone thus appear to be associated with anxious distress in patients with MDD. It is likely that younger age, unmarried status, and living alone are highly correlated with each other, and it is possible that the risk of anxious distress is driven by one or more of these variables.
In the present study, the presence of anxious distress was consistently associated with greater depression and illness severity as measured by the QIDS. To the best of our knowledge, this study is the first to show a significant association between the QIDS total score and anxious distress by using a multivariable linear regression analysis in three models. Anxious distress was linked to a greater severity of depression in our patients, as was also observed by McIntyre et al. (Citation2016b), Shim et al. (Citation2016), Zimmerman et al. (Citation2017, Citation2019), and Gaspersz et al. (Citation2017a).
The antidepressant or antipsychotic doses were higher in our patients with anxious distress compared to those without anxious distress; this result indicates a poor response to antidepressants and more frequently used antipsychotics for augmentation therapy, because the condition was more severe in the patients with anxious distress than those without it. Several studies conducted after the introduction of the DSM-5 anxious distress specifier criteria provided consistent evidence of poor responses to antidepressants (Ionescu et al. Citation2014; Gaspersz et al. Citation2017a).
Anxious distress is associated with a higher degree of neuroticism and higher cyclothymic, depressive, and irritable temperament. McIntyre et al. (Citation2016b) documented that MDD with anxious distress is associated with a higher neuroticism score assessed by the NEO Five-Factor Inventory. Neuroticism may increase the risk of anxious and depressive symptoms via specific links involving worry or brooding, respectively (Merino et al. Citation2016). Liao et al. (Citation2019) proposed that neuroticism may contribute to anxiety in patients with early-onset and either chronic or recurrent MDD. In the present series, neuroticism was significantly associated with the severity of depression in a multivariable linear regression analysis. Neuroticism and anxious distress may both be associated with the severity of depression.
A few studies have investigated the correlation between anxious distress and temperament assessed by the TEMPS-A. The MDD patients with anxious distress in the Tundo et al. (Citation2019) study had higher scores for hyperthymic temperament and mania symptoms, and bipolar patients with anxious distress had higher cyclothymic temperament scores. In our study, the anxious distress patients had higher cyclothymic, depressive, and irritable temperament scores in the univariate analysis. The scores on the cyclothymic, depressive, and irritable subtypes were highly correlated, and we thus selected the cyclothymic subtype in the multivariate analysis; cyclothymic temperament remained as the sole significant candidate associated with the severity of depression.
Mendlowicz et al. (Citation2005) stated that the cyclothymic subscale scores were significantly elevated in their group of bipolar patients compared to the unipolar depressive group. A potential relationship between anxious distress and bipolar spectrum disorder was also apparent in their unipolar patients, in which the presence of anxious distress was related to cyclothymic and hyperthymic temperament, which have been reported as markers of bipolarity (Ghaemi Citation2013). In addition, as mentioned earlier, psychomotor agitation has been defined as a severe form of anxious distress (APA Citation2013), and psychomotor agitation in MDD is reportedly related to bipolarity (Iwanami et al. Citation2015). These results seem not to rule out the possibility that anxious distress may have a relationship with temperament associated with bipolar disorder.
MDD with anxious distress has been suggested to be associated with functional impairment (McIntyre et al. Citation2016b; Gaspersz et al. Citation2017a; Maneeton et al. Citation2017). Our present findings do not support a significant correlation between anxious distress and functional impairment in the univariate analysis. The results were related to the fact that (i) the mean QIDS total score was 9.7 ± 5.5, which is considered mild to moderate, (ii) each item on the SDS indicated mild impairment, (iii) half of the present patients were either unemployed or housewives, and (iv) all were in the continuation/maintenance phase. Tundo et al. (Citation2019) did not observe significant differences in functioning between their patients with and without anxious distress. It is reasonable that the total score on the SDS in our multivariable analysis was significantly associated with the severity of depression.
Our analyses revealed that anxiety distress was clinically relevant in MDD patients without comorbid anxiety disorders in the continuation/maintenance phase. This result supports the suggestions by Gaspersz et al. (Citation2017a) that (1) anxious distress would be a more generic marker for anxiety than the anxiety disorders and (2) anxious distress may capture a somewhat distinct, but clinically valid, construct.
The strength of our present investigation is that it is the first study to evaluate the DSM-5 anxious distress specifier in Japanese outpatients with MDD without comorbid anxiety disorders in the continuation/maintenance phase, and the first to validate the specifier in such a patient population. Several study limitations should be recognised. The study was (i) cross-sectional in design and (ii) conducted at a single clinical practice. (iii) The number of subjects was relatively small (n = 110). (iv) We did not assess an observer-rated scale of the severity of depressive mood. It should be noted that in general, among patients who have higher anxiety, there is a tendency to have a higher score on a self-rating scale such as the QIDS (Rane et al. Citation2010). (v) We did not check the interrater reliability of the interview format to assess the DSM-5 anxious distress specifier. (vi) We did not assess the frequency of medication-related side effects. (vii) We assessed patients 6 months after they initially sought treatment, and we could not evaluate the relationship between the dropout rate and anxiety distress.
Conclusions
Despite the above-mentioned limitations, the present findings confirm that DSM-5 anxious distress is correlated with a greater severity of depression, higher doses of antidepressants and antipsychotics, socio-demographics (younger age, unmarried status, living alone), neuroticism personality, and cyclothymic temperament. The DSM-5 anxious distress specifier may be another severe form of MDD without comorbid anxiety disorders in the continuation/maintenance phase and might have some relationship with temperament associated with bipolar disorder. Further studies of larger patient populations are warranted to address the unresolved issues concerning anxious distress among MDD patients and bipolarity.
Acknowledgements
The authors thank Dr Ko Tanaka, Dr Anzu Takahashi, and Dr Kazune Sasaki for collecting the data.
Disclosure statement
The authors declare no conflicts of interest in this work.
Additional information
Funding
References
- American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington (VA): American Psychiatric Publication. ISBN-13: 978-0890425558.
- Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, Michal M, Wiltink J, Wild PS, Münzel T, Lackner KJ, et al. 2017. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 17(1):97.
- Coryell W, Endicott J, Andreasen NC, Keller MB, Clayton PJ, Hirschfeld RM, Scheftner WA, Winokur G. 1988. Depression and panic attacks: the significance of overlap as reflected in follow-up and family study data. Am J Psychiatry. 145(3):293–300.
- Erfurth A, Gerlach AL, Hellweg I, Boenigk I, Michael N, Akiskal HS. 2005. Studies on a German (Münster) version of the temperament auto-questionnaire TEMPS-A: construction and validation of the briefTEMPS-M. J Affect Disord. 85(1–2):53–69.
- Fava M, Rush AJ, Alpert JE, Carmin CN, Balasubramani GK, Wisniewski SR, Trivedi MH, Biggs MM, Shores-Wilson K. 2006. What clinical and symptom features and comorbid disorders characterize outpatients with anxious major depressive disorder: a replication and extension. Can J Psychiatry. 51(13):823–835.
- Fichter MM, Quadflieg N, Fischer UC, Kohlboeck G. 2009. Twenty-five-year course and outcome in anxiety and depression in the Upper Bavarian Longitudinal Community Study. Acta Psychiatr Scand. 122(1):75–85.
- Gaspersz R, Lamers F, Kent JM, Beekman AT, Smit JH, van Hemert AM, Schoevers RA, Penninx BW. 2017a. Longitudinal predictive validity of the DSM-5 anxious distress specifier for clinical outcomes in a large cohort of patients with major depressive disorder. J Clin Psychiatry. 78(02):207–213.
- Gaspersz R, Lamers F, Kent JM, Beekman ATF, Smit JH, van Hemert AM, Schoevers RA, Penninx BWJH. 2017b. Anxious distress predicts subsequent treatment outcome and side effects in depressed patients starting antidepressant treatment. J Psychiatr Res. 84:41–48.
- Ghaemi SN. 2013. Bipolar spectrum: a review of the concept and a vision for the future. Psychiatry Investig. 10(3):218–224.
- Goes FS, McCusker MG, Bienvenu OJ, Mackinnon DF, Mondimore FM, Schweizer B, Depaulo JR, Potash JB, National Institute of Mental Health Genetics Initiative Bipolar Disorder Consortium. 2012. Co-morbid anxiety disorders in bipolar disorder and major depression: familial aggregation and clinical characteristics of co-morbid panic disorder, social phobia, specific phobia and obsessive-compulsive disorder. Psychol Med. 42(7):1449–1459.
- Husain MM, Rush AJ, Sackeim HA, Wisniewski SR, McClintock SM, Craven N, Holiner J, Mitchell JR, Balasubramani GK, Hauger R. 2005. Age-related characteristics of depression: a preliminary STAR*D report. Am J Geriatr Psychiatry. 13(10):852–860.
- Ionescu DF, Niciu MJ, Richards EM, Zarate CA Jr. 2014. Pharmacologic treatment of dimensional anxious depression: a review. Prim Care Companion CNS Disord. 16:13r01621.
- Iwanami T, Maeshima H, Baba H, Satomura E, Namekawa Y, Shimano T, Suzuki T, Arai H. 2015. Psychomotor agitation in major depressive disorder is a predictive factor of mood-switching. J Affect Disord. 170:185–189.
- Liao A, Walker R, Carmody TJ, Cooper C, Shaw MA, Grannemann BD, Adams P, Bruder GE, McInnis MG, Webb CA, et al. 2019. Anxiety and anhedonia in depression: associations with neuroticism and cognitive control. J Affect Disord. 245:1070–1078.
- Lin CH, Wang FC, Lin SC, Chen CC, Huang CJ. 2014. A comparison of inpatients with anxious depression to those with nonanxious depression. Psychiatry Res. 220(3):855–860.
- Maneeton N, Suttajit S, Maneeton B, Likhitsathian S, Eurviyanukul K, Udomratn P, Chan ES, Si TM, Sulaiman AH, Chen CH, et al. 2017. Clinical and socio-demographic correlates of anxious distress in Asian outpatients with major depressive disorder. Nord J Psychiatry. 71(7):503–508.
- McIntyre RS, Weiller E, Zhang P, Weiss C. 2016a. Brexpiprazole as adjunctive treatment of major depressive disorder with anxious distress: results from a post-hoc analysis of two randomised controlled trials. J Affect Disord. 201:116–123.
- McIntyre RS, Woldeyohannes HO, Soczynska JK, Vinberg M, Cha DS, Lee Y, Gallaugher LA, Dale RS, Alsuwaidan MT, Mansur RB, et al. 2016b. The prevalence and clinical characteristics associated with Diagnostic and Statistical Manual Version-5-defined anxious distress specifier in adults with major depressive disorder: results from the International Mood Disorders Collaborative Project. Ther Adv Chronic Dis. 7(3):153–159.
- Melartin TK, Rytsälä HJ, Leskelä US, Lestelä-Mielonen PS, Sokero TP, Isometsä ET. 2002. Current comorbidity of psychiatric disorders among DSM-IV major depressive disorder patients in psychiatric care in the Vantaa Depression Study. J Clin Psychiatry. 63(2):126–134.
- Mendlowicz MV, Akiskal HS, Kelsoe JR, Rapaport MH, Jean-Louis G, Gillin JC. 2005. Temperament in the clinical differentiation of depressed bipolar and unipolar major depressive patients. J Affect Disord. 84(2–3):219–223.
- Merino H, Senra C, Ferreiro F. 2016. Are worry and rumination specific pathways linking neuroticism and symptoms of anxiety and depression in patients with generalized anxiety disorder, major depressive disorder and mixed anxiety-depressive disorder? PLoS One. 11(5):e0156169.
- Miyaoka H, Otsubo T, Yoshimura Y, Kamijima K, Miyaoka Y. 1999. Reliability and validity of the modified Japanese version of short-form Eysenck Personality Questionnaire. Showa Univ Med Sci. 11(1):33–36.
- Nakato Y, Inoue T, Nakagawa S, Kitaichi Y, Kameyama R, Wakatsuki Y, Kitagawa K, Omiya Y, Kusumi I. 2016. Confirmation of the factorial structure of the Japanese short version of the TEMPS-A in psychiatric patients and general adults. Neuropsychiatr Dis Treat. 12:2173–2179.
- Otsubo T, Tanaka K, Koda R, Shinoda J, Sano N, Tanaka S, Aoyama H, Mimura M, Kamijima K. 2005. Reliability and validity of Japanese version of the Mini-International Neuropsychiatric Interview. Psychiatry Clin Neurosci. 59(5):517–526.
- Rane LJ, Fekadu A, Wooderson S, Poon L, Markopoulou K, Cleare AJ. 2010. Discrepancy between subjective and objective severity in treatment-resistant depression: prediction of treatment outcome. J Psychiatr Res. 44(15):1082–1087.
- Rhebergen D, Batelaan NM, de Graaf R, Nolen WA, Spijker J, Beekman AT, Penninx BW. 2011. The 7-year course of depression and anxiety in the general population. Acta Psychiatr Scand. 123(4):297–306.
- Seo HJ, Jung YE, Kim TS, Kim JB, Lee MS, Kim JM, Lim HW, Jun TY. 2011. Distinctive clinical characteristics and suicidal tendencies of patients with anxious depression. J Nerv Ment Dis. 199(1):42–48.
- Sheehan DV, Harnett-Sheehan K, Raj BA. 1996. The measurement of disability. Int Clin Psychopharmacol. 11:89–95.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. 1998. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 59:22–33.
- Shim IH, Woo YS, Bahk WM. 2016. Associations between immune activation and the current severity of the "with anxious distress" specifier in patients with depressive disorders. Gen Hosp Psychiatry. 42:27–31.
- Sugawara H, Tsutsumi T, Inada K, Ishigooka J, Hashimoto M, Takebayashi M, Nishimura K. 2019. Association between anxious distress in a major depressive episode and bipolarity. Neuropsychiatr Dis Treat. 15:267–270.
- Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, Crismon ML, Shores-Wilson K, Toprac MG, Dennehy EB, et al. 2004. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med. 34(1):73–82.
- Tundo A, Musetti L, de Filippis R, Grande CD, Falaschi V, Proietti L, Dell'Osso L. 2019. Is there a relationship between depression with anxious distress DSM-5 specifier and bipolarity? A multicenter cohort study on patients with unipolar, bipolar I and II disorders. J Affect Disord. 245:819–826.
- Zimmerman M, Chelminski I, Young D, Dalrymple K, Walsh E, Rosenstein L. 2014. A clinically useful self-report measure of the DSM-5 anxious distress specifier for major depressive disorder. J Clin Psychiatry. 75(06):601–607.
- Zimmerman M, Clark H, McGonigal P, Harris L, Holst CG, Martin J. 2017. Reliability and validity of the DSM-5 Anxious Distress Specifier Interview. Compr Psychiatry. 76:11–17.
- Zimmerman M, Martin J, McGonigal P, Harris L, Kerr S, Balling C, Kiefer R, Stanton K, Dalrymple K. 2019. Validity of the DSM-5 anxious distress specifier for major depressive disorder. Depress Anxiety. 36(1):31–38.