Abstract
Objective: To discuss the impact of depression on work and how depression-related sick leave duration could be a potential indicator and outcome for measuring functionality in depression.
Methods: Our review was based on a literature search and expert opinion that emerged during a virtual meeting of European psychiatrists that was convened to discuss this topic.
Results: Current evidence demonstrates that depression-related sick leave duration is influenced by multiple disease-, patient- and work-related factors, together with societal attitudes towards depression and socioeconomic conditions. A wide variety of pharmacological and non-pharmacological treatments and work-based interventions are effective in reducing depression-related sick leave duration and/or facilitating return to work. Recent real-world evidence showed that patients treated with antidepressant monotherapy appear to recover their working life faster than those receiving combination therapy. Although depression-related sick leave duration was found to correlate with severity of depressive symptoms, it cannot be used alone as a viable marker for disease severity.
Conclusions: Given its multifactorial nature, depression-related sick leave duration is not on its own a viable outcome measure of depression severity but could be used as a secondary outcome alongside more formal severity measures and may also represent a useful measure of functionality in depression.
Depression in the working population and depression-related sick leave have a profound economic impact on society
Depression-related sick leave duration is influenced by multiple disease-, patient- and work-related factors, together with societal attitudes towards depression and socioeconomic conditions
A wide variety of pharmacological and non-pharmacological treatments and work-based interventions have been shown to be effective in reducing depression-related sick leave duration and/or facilitating return to work
In terms of pharmacological intervention, recent real-world evidence has shown that patients treated with antidepressant monotherapy are able to recover their working life faster than those treated with combination therapy
Although depression-related sick leave duration has been shown to correlate with severity of depressive symptoms, it is not a viable outcome measure of depression severity on its own, but could be used as secondary outcome alongside more formal clinician- and patient-rated severity measures
Depression-related sick leave duration may, however, represent a viable outcome for measuring functionality in depression
Key points
Introduction
Depression is the most common mental illness worldwide and a major cause of disability (Liu et al., Citation2020). The Global Burden of Disease study found that the number of incident cases of depression rose 50% worldwide from 172 million in 1990 to 258 million in 2017 and the majority of these cases (>90%) were diagnosed with major depressive disorder (MDD) (Liu et al., Citation2020). In 2019, depressive disorders accounted for 1.8% of disability-adjusted life years (DALYs) globally among all age groups (GBD 2019 Diseases and Injuries Collaborators, Citation2020). Among those aged 25–49 years, depressive disorders accounted for 3.5% of DALYs, making it the sixth leading cause of disability, after road injuries, the human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS), ischaemic heart disease, low back pain and headache disorders (GBD 2019 Diseases and Injuries Collaborators, Citation2020). Increasing recognition of the societal burden of depression has led to proactive strategies to address mental health issues, including initiatives by the World Health Organisation (WHO, 2019), World Bank Group (Batada & Solano, Citation2019) and individual governments and health authorities.
In the workplace, depression influences productivity not only through absenteeism but also through its impact on the performance of individuals who remain at work (‘presenteeism’) (Evans-Lacko & Knapp, Citation2016). Indeed, a study into the extent and costs of depression-related absenteeism and presenteeism in the workplace across eight diverse countries (Brazil, Canada, China, Japan, South Korea, Mexico, South Africa and the USA) found that costs associated with presenteeism were generally 5–10 times higher than those associated with absenteeism (Evans-Lacko & Knapp, Citation2016). Evidence has also indicated that depression-related sick-leave increases the likelihood of early retirement due to permanent disability (Mittendorfer-Rutz et al., Citation2014; Wedegaertner et al., Citation2013). Depression in the working population and depression-related sick leave have a profound economic impact on society, both in terms of the direct costs on health authorities and health insurance, and the indirect costs associated with lost working hours, impaired productivity and early retirement (Ammerman et al., Citation2016; Caballero-Martínez et al., Citation2014; Geraedts et al., Citation2014; Rost et al., Citation2014; Wedegaertner et al., Citation2013). However, instigating effective treatments for depression has been shown to be an efficient way for governments and health authorities to spend their limited resources, with an appreciable return on investment (Chisholm et al., Citation2016). This contrasts with the substantial investment in new cancer medicines, often with very limited health gain (Cohen, Citation2017; Waters & Urquhart, Citation2019).
Severity of depressive symptoms has been shown to be significantly associated with both absenteeism and presenteeism (Beck et al., Citation2011; Clark et al., Citation2016; Jain et al., Citation2013; Johnston et al., Citation2019). Notably, the severity of depressive symptoms (assessed using the Patient Health Questionnaire-9 [PHQ-9]) was shown to be associated with work productivity loss (assessed using the Work Productivity and Activity Impairment questionnaire) even among workers who had not previously been formally diagnosed with the condition (Asami et al., Citation2015), illustrating that the impact of depression on work productivity and sick leave is likely to be much greater than that estimated from studies conducted only in those formally diagnosed with depression. Furthermore, work productivity was confirmed to be significantly higher in those diagnosed with depression who are treated versus untreated (Dewa et al., Citation2011; Trivedi et al., Citation2013), highlighting the importance of early detection and treatment, and an overall need for greater awareness of depressive symptoms in the workplace. A survey of over 500 psychiatric outpatients being treated for a major depressive episode (MDE) found that approximately three-quarters of respondents considered returning to their usual functioning level at work, home or school as ‘very important’ in determining remission (Zimmerman et al., Citation2006). Such findings indicate that the impact of depression on an individual’s ability to work is fundamental to their quality of life and functional recovery, supporting the concept of depression-related sick leave as a rational target for intervention to improve patient care.
A virtual meeting of European psychiatrists was convened in November 2020 in order to discuss the major impact depression has on work and evidence that depression-related sick leave duration could be a potential indicator and outcome for measuring functionality in depression. This article presents the results of a literature review of current evidence in this area and outlines the key themes and expert opinion that emerged during the meeting.
Literature review methodology
A search of PubMed was conducted in July 2020 using the following search terms: (depression[MeSH Terms]) AND ((sick leave[Title]) OR (work absence[Title]) OR (absenteeism[Title]) OR (medical leave[Title]) OR (return to work[Title]) OR (productivity[Title])). The search employed two filters: (1) the publication date of articles was restricted to the last 10 years and (2) the language of articles was restricted to English. The search retrieved a total of 176 articles, which were manually examined for relevance and a total of 82 articles were identified for further assessment. Reasons for excluding 94 articles from further assessment were: depression was not the primary condition/focus of the article (n = 90); duplicate references (n = 2); and no abstract/full text was available for assessment (n = 2). The remaining 82 articles were assessed and categorised in terms of primary content/focus: factors affecting sick leave duration/return to work (RTW; n = 25); impact of depression on work productivity (n = 21); impact of employer factors/work interventions on sick leave/RTW (including the attitudes/actions of employers to sick leave/RTW and formal work interventions designed to reduce sick leave duration and aid RTW; n = 18); impact of non-pharmacological interventions on functional recovery/RTW (n = 14); impact of pharmacological interventions on functional recovery/RTW (n = 7); factors relating to depression at work prior to sick leave (n = 6); and impact of sick leave on depression outcomes (n = 5) (note: some articles were included in more than one category). The results of this literature search were used to help inform discussion at the virtual meeting of European psychiatrists in November 2020. The remainder of this article utilises the results of the literature review in conjunction with the personal opinions of the authors expressed during the meeting.
Factors influencing depression-related sick leave duration and RTW
Depression-related sick leave duration exceeds that associated with other common conditions, as illustrated by a survey of over 4700 workers in The Netherlands (de Graaf et al., Citation2012). This found that MDD had a more significant impact on workplace absenteeism than most other chronic mental and physical disorders, resulting in 19.8 additional sick leave days per year and accounting for 8% of all sick leave days recorded in the study (de Graaf et al., Citation2012). Only one somatic condition (digestive disorders) was associated with a similarly high number of additional sick leave days per year (20.6 additional days) (de Graaf et al., Citation2012). The Impact of Depression at work in Europe Audit (IDEA) study, which comprised an online questionnaire completed by ∼7000 working adults in Europe who had taken time off work due to depression, demonstrated that the average duration of respondents’ most recent episode of sick leave due to depression was 36 days (Ipsos, Citation2012). Such findings raise questions as to why depression results in such lengthy absenteeism, in comparison with other conditions, and the factors that might influence depression-related sick leave duration and RTW.
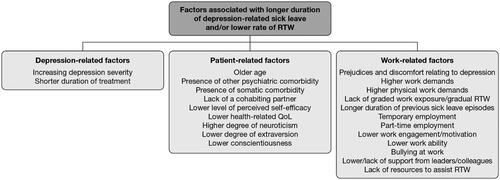
A systematic literature review of prognostic factors for RTW after depression-related work disability found that increasing severity of depression was associated with a decreasing rate of RTW (Ervasti et al., Citation2017). Several other risk factors associated with a decreased RTW rate were identified, including older age and the presence of other psychiatric and somatic comorbidities (Ervasti et al., Citation2015, Citation2017). Other studies have identified a range of additional factors associated with longer duration of depression-related sick leave and/or a lower rate of RTW, including disease-related factors (e.g., shorter duration of treatment), patient-related factors (e.g., older age, presence of other comorbidities, lack of a cohabiting partner) and work-related factors (e.g., prejudices and discomfort relating to depression, temporary/part-time employment, lack of resources to assist RTW, bullying at work; ; Arends et al., Citation2019; Bouwmans et al., Citation2014; Corbière et al., Citation2015; Endo et al., Citation2019; Ervasti et al., Citation2014; Flach et al., Citation2012; Hees et al., Citation2012; Huijs et al., Citation2017; Netterstrøm et al., Citation2015; Ogawa et al., Citation2013; Vlasveld et al., Citation2013). Other investigations have defined different outcome trajectories for individuals with depression-related sick leave (in terms of sick leave duration), based on socio-demographic and morbidity characteristics (Arends et al., Citation2019; Farrants et al., Citation2018). Taken together, these findings demonstrate the complexity of factors involved in depression-related sick leave and RTW, many of which are interconnected. Nevertheless, a correlation between the severity of depressive symptoms and duration of depression-related sick leave is a relatively consistent observation (Ervasti et al., Citation2017; Hees et al., Citation2012; Jain et al., Citation2013; Johnston et al., Citation2019; Wedegaertner et al., Citation2013).
Figure 1. Factors associated with longer duration of depression-related sick leave and/or lower rate of RTW. QoL, quality of life; RTW, return to work.
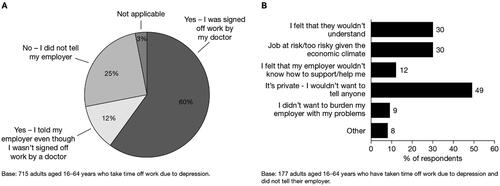
An important finding from the IDEA study was that 25% of respondents did not tell their employer the reason for their sick leave (; Ipsos, Citation2012). The most common reasons for individuals not informing their employer were ‘It’s private – I wouldn’t want to tell anyone’ (49%), ‘I felt that they wouldn’t understand’ (30%) and ‘Job at risk/too risky given the economic climate’ (30%) (; Ipsos, Citation2012). These findings illustrate the high degree of stigma that is still associated with depression (Arnaez et al., Citation2020; Saridi et al., Citation2017; Yokoya et al., Citation2018), which may result in patients avoiding seeking treatment for depressive symptoms and/or hiding the reason for taking sick leave due to fear of the negative attitudes they may experience from admitting to having such symptoms. Differences among countries in stigma and attitudes towards depression may also in part account for the variability between countries in the average duration of depression-related sick leave observed in the IDEA study, which ranged from ∼23 days in Italy to 41 days in Germany and the UK (Ipsos, Citation2012). However, this variability is also likely to have been influenced by other factors, such as differences between countries in systems for sick leave allowance and healthcare provision. Nevertheless, it is clear that the attitude of employers and colleagues towards individuals with depression, and the degree of support they receive during sick leave and RTW, are important factors affecting the duration of depression-associated sick leave (Corbière et al., Citation2015; Evans-Lacko & Knapp, Citation2018; de Vries et al., Citation2012). Furthermore (and as outlined in more detail below), specifically designed work-based interventions have proven to be effective in reducing depression-related sick leave duration and aiding RTW (Bhui et al., Citation2012; Hellerstein et al., Citation2015; Lagerveld et al., Citation2012; Lerner et al., Citation2015; Negrini et al., Citation2018; Nieuwenhuijsen et al., Citation2014; Poulsen et al., Citation2017; Streibelt et al., Citation2018; Trivedi, Citation2018; Volker et al., Citation2015; Wisenthal & Krupa, Citation2013; Wisenthal et al., Citation2019).
Figure 2. IDEA study: responses to the questions (A) ‘Did you tell your employer that the reason you needed to take time off work was because of your depression?’ and (B) ‘Why didn't you tell your employer about your depression?’. IDEA, Impact of Depression at work in Europe Audit. (Ipsos. IDEA: Impact of Depression at Work in Europe Audit. Ipsos Healthcare, 2012. Available at: https://www.europeandepressionday.eu/2019/04/11/idea/).
It is important to bear in mind that although patients with depression need time away from work in order to recover and, ideally, achieve remission, sick leave itself can have a detrimental impact on an individual’s mental health; for example, by decreasing feelings of self-worth and self-esteem (Nielsen et al., Citation2013). Indeed, studies have shown that sick leave increases the risk of suicide attempts, not only in patients with depressive disorders (Wang et al., Citation2015) but also in those with other health disorders (Wang et al., Citation2014). Such findings further illustrate the importance of providing support to individuals with depression during sick leave and RTW.
Impact of depression interventions on functional recovery/RTW
Several studies have investigated the effects of pharmacological and non-pharmacological interventions for depression on functional recovery/work productivity, sick leave and/or RTW, while others have assessed the impact of employer factors and work-based interventions on these outcomes.
Pharmacological interventions
The Assessment in Work Productivity and the Relationship with Cognitive Symptoms (AtWoRC) study investigated the association between patient-reported cognitive symptoms (assessed using the 20-item Perceived Deficits Questionnaire [PDQ-D-20]) and work productivity (assessed using the Work Limitations Questionnaire [WLQ]) in gainfully employed patients receiving vortioxetine in the course of a current MDE (Chokka et al., Citation2019). After 12 weeks of vortioxetine treatment, patients experienced significant improvements from baseline in all assessment scores (including measures of cognitive symptoms, disease severity, functional outcomes, work productivity and disability; Chokka et al., Citation2019). There was a significant correlation between PDQ-D-20 and WLQ scores, indicating that patients who had improved cognitive function also had improved workplace productivity (Chokka et al., Citation2019). In the Combining Medications to Enhance Depression Outcomes (CO-MED) trial, outpatients with MDD were treated with either escitalopram plus placebo, sustained-release bupropion plus escitalopram or extended-release venlafaxine plus mirtazapine (Rush et al., Citation2011). As in the AtWoRC study, a secondary analysis of the CO-MED trial demonstrated that antidepressant treatment resulted in improvement in self-reported work productivity, even after controlling for changes in severity of depressive symptoms (Jha et al., Citation2016). This study also found that early improvement in work productivity was significantly associated with an increased likelihood of subsequent remission, supporting the assessment of work productivity as a potential treatment outcome in clinical practice (Jha et al., Citation2016). Other studies have similarly demonstrated a significant association between improvement in depressive symptoms and improvement in productivity and/or reduction in absenteeism following antidepressant treatment (Beck et al., Citation2014; Woo et al., Citation2011).
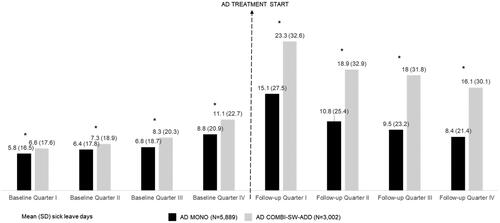
The aforementioned studies used antidepressant treatment that was not specifically directed at improving functional recovery and/or sick leave duration but, rather, aimed to influence depressive symptoms in general. Attempts to compare the specific effects of different types of antidepressants on work productivity, sick leave and RTW have yielded inconsistent findings (Nieuwenhuijsen et al., Citation2014; Trivedi, Citation2018). However, a real-world retrospective study conducted in Germany, which was designed to investigate the impact of antidepressant use on sick leave duration in patients with MDD, specifically compared the use of antidepressant monotherapy versus combination/switch/add-on treatment strategies (Kasper et al., Citation2021). Information on patients initiating treatment for MDD was gathered from general practitioners and analysed both descriptively and using multiple regression analyses. The cohort included 8891 patients, 66.2% of whom received monotherapy and 33.8% combination/switch/add-on treatments. Demographic and baseline characteristics were generally similar between the two treatment groups, although non-psychiatric comorbidities were more frequently observed in the monotherapy group and baseline anxiety and moderate-to-severe MDD were more common in the combination/switch/add-on group (Kasper et al., Citation2021). Sick leave requests were more frequently recorded for patients receiving combination/switch/add-on treatments than for those who received monotherapy, with more pronounced differences between groups after initiation of antidepressant treatment (). The proportion of patients with >30 days of sick leave was also higher in the combination/switch/add-on group than the monotherapy group (Kasper et al., Citation2021). Results of the multiple regression analyses showed that the variable that appeared to most strongly impact sick leave days after starting antidepressant treatment was the antidepressant therapeutic approach, followed by MDD severity and patient age. The expected number of sick days was 1.6× higher in the combination/switch/add-on group than in the monotherapy group (Kasper et al., Citation2021). Overall, this study demonstrated that patients treated with antidepressant monotherapy seem to recover their working life better than those receiving combination treatments. However, it should be considered in this context that MDD patients who were treated with antidepressant monotherapy might have experienced a relatively low severity of depressive symptoms, which might have been associated with faster response to the first-line antidepressant agent and, subsequently, faster recovery of their working life. By contrast, MDD patients receiving additional combination/switch/add-on treatments might have suffered from relatively severe depressive symptoms, requiring more complex psychopharmacotherapeutic approaches, which might have led to a longer duration of sick-leave periods, as well as a delay in recovering their working life. In addition, patients treated with monotherapy might have had greater treatment responsiveness than those treated with combination therapy, which again may have resulted in faster recovery, and it is important to bear in mind that severe depression can be very responsive to treatment. Within this context, it is also important to note that the use of combination therapy does not automatically result in a higher therapeutic effect, since a substantial proportion of patients with MDD may have genetic polymorphisms that cause them to be ultrarapid metabolisers (or their metabolism may be altered by other non-genetic factors, such as drug–drug interactions), meaning that they require a higher dose of antidepressant than the majority of the general population (Poolsup et al., Citation2000; Teo et al., Citation2015). In addition, it is important to ensure that patients adhere to monotherapy before adding other treatments, since treatment adherence is a major concern in patients with chronic conditions such as depression (Grenard et al., Citation2011). Finally, although the study included patients diagnosed with MDD, it is possible that some patients required combination therapy because they had been misdiagnosed with MDD and therefore did not respond to antidepressant monotherapy treatment.
Figure 3. German real-world retrospective study of antidepressant use and sick leave among patients with MDD: summary of sick leave days (mean and SD) in the year before and year after starting antidepressant treatment stratified by antidepressant therapeutic approach. AD, antidepressant; AD MONO, patients who had prescriptions of a single AD both at Index Date and during follow-up; AD COMBI-SW-ADD, patients who had prescription of more than one AD at Index Date, and patients who had prescriptions of a single AD at Index Date, but received prescriptions of different AD during follow-up; MDD, major depressive disorder; SD, standard deviation. *p-value from nonparametric Wilcoxon signed-rank test for differences between groups is statistically significant (Kasper S, et al. Predictors of sick leave days in patients affected by major depressive disorder receiving antidepressant treatment in general practice setting in Germany. International Journal of Psychiatry in Clinical Practice. Published online 20 September 2021. Taylor & Francis Group. Reprinted by permission of the publisher).
Non-pharmacological interventions
A Cochrane review of three studies found moderate-quality evidence that telephone or online cognitive behavioural therapy (CBT) was more effective in reducing sick leave duration than usual primary or occupational care (Nieuwenhuijsen et al., Citation2014; Trivedi, Citation2018). This review also found high-quality evidence (based on a single study) that a structured telephone outreach and care management programme was more effective in reducing sick leave duration than usual care (Nieuwenhuijsen et al., Citation2014; Trivedi, Citation2018).
The impact of occupational therapy on recovery and RTW was assessed in a study of 117 employees who were on sick leave due to MDD (median duration of sick leave, 4.8 months) (Hees et al., Citation2013). Participants were randomised to receive treatment as usual either with or without 18 sessions of occupational therapy. Although the groups did not differ significantly in their overall work participation (defined on the basis of absenteeism and duration until partial/full RTW), those who received occupational therapy experienced greater improvement in depressive symptoms, greater likelihood of long-term symptom remission, and greater likelihood of long-term RTW in good health than those who only received treatment as usual (Hees et al., Citation2013).
A study conducted in over 100 subjects who were on sick leave for ≥3 months due to a diagnosis of reaction to severe stress and/or an MDE compared the effects of 8, 12, and 24 weeks of nature-based rehabilitation on RTW after 1 year (Grahn et al., Citation2017). Rehabilitation was conducted in the Alnarp Rehabilitation Garden at the Swedish University of Agricultural Sciences, which was specifically designed for people with stress-related psychiatric disorders and/or depression. The study found that nature-based rehabilitation increased the likelihood of RTW, with up to 68% of participants working or participating in job training/work-oriented measures after 1 year (Grahn et al., Citation2017). Likelihood of RTW increased with increasing length of rehabilitation (Grahn et al., Citation2017).
Psychoeducation (Melin et al., Citation2018), physical exercise (Bhui et al., Citation2012; Kaldo et al., Citation2018; Morita et al., Citation2016) and lifestyle interventions (Block et al., Citation2008) have also demonstrated some effectiveness in reducing depression-related sick leave and/or increasing work functioning. For example, an email-based intervention designed to either (1) increase physical activity, (2) reduce the intake of saturated and trans fats and sugar, or (3) increase the consumption of fruit and vegetables was evaluated in a 3-month randomised controlled trial with almost 800 participants (Block et al., Citation2008). Participants could choose which of these three outcomes they wanted to pursue and then received weekly messages offering tailored small-step goals, tips for achieving those goals, and health information, together with opportunities for interaction and engagement (Block et al., Citation2008). The control group comprised a delayed control, in which participants were offered the programme 8 months after initial randomisation (Block et al., Citation2008). The study found that the intervention resulted in significant improvements in both presenteeism and health-related quality of life (assessed using the Short Form-8), as well as other behavioural outcomes (Block et al., Citation2008).
Employer factors and work-based interventions
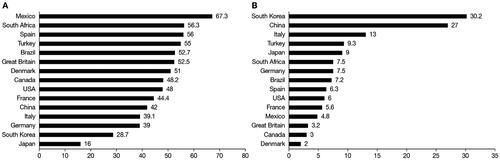
Several studies have demonstrated that the attitude of employers towards employees with depression can have a substantial impact on sick leave duration and RTW. A cross-sectional survey of >16,000 employees and managers from 15 diverse countries found that there was wide variation between countries in the degree to which managers avoided talking about depression with their employees, and the degree to which managers offered help to depressed employees (; Evans-Lacko & Knapp, 2018), illustrating cultural differences in attitudes towards and stigma associated with depression. Increasing gross domestic product was marginally associated with longer duration of depression-related sick leave, and, after controlling for gross domestic product, working in an environment where managers felt comfortable to offer help and support to employees with depression was independently associated with less absenteeism (Evans-Lacko & Knapp, 2018). A Canadian survey of supervisors working with employees who were either already back at work or still on sick leave due to depression found that although the majority of supervisors (almost 90%) encouraged their employees to focus primarily on their recovery before RTW, over 40% pressured their employees to RTW as soon as possible (Negrini et al., Citation2018). Cox regression analyses found that the only factor that significantly predicted RTW was ‘the supervisors' intention to take measures to facilitate their employees' RTW’; such measures included providing emotional support and assistance (Negrini et al., Citation2018). Another Canadian study investigated factors associated with RTW among employees on depression-related sick leave from the perspective of unions (Corbière et al., Citation2015). Major factors affecting RTW included the provision of support and follow-up during sick leave, provision of resources to assist employees with RTW, the existence of an organisational culture in which mental health issues and human aspects of work were central, and stakeholders’ discomfort and prejudices relating to depression (Corbière et al., Citation2015).
Figure 4. Country differences in managers' response to depression: (A) percentage of managers who offered help to employees with depression and (B) percentage of managers who avoided talking about depression with employees (Republished with permission of BMJ Publishing Group Ltd, from Is manager support related to workplace productivity for people with depression: a secondary analysis of a cross-sectional survey from 15 countries, Evans-Lacko S, Knapp M, 8, 2022; permission conveyed through Copyright Clearance Center, Inc.).
Other studies have assessed the effectiveness of work-based interventions specifically designed to reduce depression-related sick leave and facilitate RTW (Nieuwenhuijsen et al., Citation2014; Trivedi, Citation2018). Cognitive work hardening is a multi-element intervention designed to prepare individuals for RTW after depression-related sick leave (Wisenthal & Krupa, Citation2013, Citation2014). It is typically administered by an occupational therapist in a simulated work setting, and addresses key occupational performance issues previously identified by the client and matched to the work demands of their job description, including cognitive impairments (e.g., poor concentration), fatigue, interpersonal issues (e.g., conflict management, communication) and coping skills (e.g., time management) (Wisenthal & Krupa, Citation2013, Citation2014). Cognitive work hardening has been shown to enhance self-confidence, stamina and cognitive abilities, and to significantly improve work ability, fatigue and depression severity (Wisenthal et al., Citation2018, Citation2019).
A randomised controlled trial assessed the effectiveness of adding work-focussed telephone-based counselling to usual care in employees with depression and at-work limitations (as assessed using the WLQ; Lerner et al., Citation2015). The addition of this intervention significantly improved at-work productivity and severity of depressive symptoms, and significantly reduced duration of depression-related sick leave (Lerner et al., Citation2015). Another randomised controlled trial investigated the effectiveness of a blended eHealth intervention (ECO) versus usual care in reducing sick leave duration in employees with common mental disorders, including depression, who were absent from work for 4–26 weeks (Volker et al., Citation2015). ECO consisted of two parts: an eHealth module for the employee (comprising 16 sessions of psychoeducation, work-based CBT, pain/fatigue management, problem-solving skills training, and relapse prevention) and an emailed decision aid to advise the occupational physician regarding treatment and referral options, based on the employee’s progress during treatment (Volker et al., Citation2015). ECO was shown to significantly reduce duration until first RTW versus usual care, but there was no significant difference between groups in duration until full RTW (Volker et al., Citation2015). After 9 months, the proportion of participants in remission was significantly higher in the ECO group versus the usual care group (Volker et al., Citation2015). Similarly, an open-label randomised controlled trial assessed the effectiveness of a 12-week web-based programme (comprising structured interactive sessions and therapist support upon request), compared with unguided web-based psychoeducation, in reducing depressive symptoms and associated sick leave in adults with mild to moderate depression (Beiwinkel et al., Citation2017). Depressive symptoms (assessed using the PHQ-9 and Beck Depression Inventory [BDI]) improved significantly more in the former versus latter group, and there was a reduction in sick leave frequency in both groups, although there was no statistical difference in sickness absence between groups (Beiwinkel et al., Citation2017). A further randomised controlled trial assessed the effectiveness of Individual Placement and Support, in comparison with services as usual, on RTW/return to education among people with mood or anxiety disorders, including depression (Hellström et al., Citation2017). After 24 months, there were no significant differences between groups in terms of RTW/return to education, symptom severity, functioning or well-being (Hellström et al., Citation2017).
Additional work-based interventions that have been shown to reduce depression-related sick leave and facilitate RTW include job accommodations (e.g., offering temporary work or graded RTW; Muijzer et al., Citation2012; Streibelt et al., Citation2018), work-focussed CBT/psychotherapy (Hellerstein et al., Citation2015; Lagerveld et al., Citation2012), and worksite exercise initiatives (Bhui et al., Citation2012).
Use of sick leave duration as a predictor of depression and as a marker for treatment outcomes
Although attitudes towards depression have generally improved over time, there is still social stigma associated with the condition in many countries, exacerbated by chronic underfunding of services in this area (Batada & Solano, Citation2019; United Nations, Citation2020). Findings from the IDEA study demonstrate that many individuals with depression-related sick leave are reluctant to tell their employer the true reason for their work absence (Ipsos, Citation2012). Consequently, there is a rationale for considering sick leave in the absence of somatic conditions as a marker to identify individuals for screening for depressive symptoms, not only in the primary care setting, but also in the workplace. As previously illustrated, the attitudes of employers towards depression can have a substantial impact on depression-related sick leave and RTW, and if employers support and encourage employees to be open about their reasons for work absence, this is likely to help individuals to seek help and receive the treatment they need. Similarly, since severity of depressive symptoms has been shown to be associated with work productivity loss even among those not formally diagnosed with depression (Asami et al., Citation2015), a drop in work productivity without an obvious cause may signpost the need for screening of depressive symptoms.
Successful treatment of depression has been shown to improve functional recovery/work productivity and to reduce absenteeism (Beck et al., Citation2014; Chokka et al., Citation2019; Jha et al., Citation2016; Woo et al., Citation2011), and depression-related sick leave duration might potentially be considered as a marker of functional recovery. Since sick leave duration has also been shown to correlate with severity of depression (Ervasti et al., Citation2017; Hees et al., Citation2012; Jain et al., Citation2013; Johnston et al., Citation2019; Wedegaertner et al., Citation2013), it might also be argued that depression-related sick leave could be used as a surrogate marker for disease depression severity, but this requires careful consideration. As previously outlined, a wide range of factors have been shown to be associated with depression-related sick leave duration and many of these are unconnected, or not directly connected, to severity of depressive symptoms; for example, older age, the presence of other psychiatric and non-psychiatric comorbidities, the absence of a cohabiting partner, and a variety of work-related factors, including type of employment (full-time/part-time/temporary), level of work demands, and job accommodations/employer attitudes towards depression. It is also important to bear in mind that RTW may often precede full recovery, since patients may either themselves be keen to return to their workplace, or feel pressured or obliged to do so by the attitudes of their employer/colleagues and/or lack of adequate sick leave allowance and provision. Sick leave provision varies greatly not only among countries but also between the public and private sectors. In some instances, sick leave provision may be more secure in the public versus private sector; conversely, some private companies are more proactive than public sector companies in providing support and resources to help employees with RTW. Moreover, the socioeconomic climate at the local, national or international level can not only directly affect the resources available for sick leave provision, but also indirectly affect duration of sick leave through feelings of job insecurity and worries about losing employment and/or not being able to find alternative employment. Importantly, if individuals with depression have inadequate sick leave duration and/or do not receive appropriate treatment and support when absent from work, they are likely to go back to work with residual symptoms, which may cause substantial cognitive and functional impairment (Pedrelli et al., Citation2010; Romera et al., Citation2013), increasing the likelihood of subsequent presenteeism, absenteeism and relapse (Israel, Citation2010; Paykel, Citation2008).
Given that depression-related sick leave duration can be influenced by such a diverse range of factors, it is unlikely to represent a viable marker for severity of depression on its own, but could potentially be used as a secondary marker alongside formal clinical measures of depression severity, such as the Montgomery-Åsberg Depression Rating Scale (Montgomery & Asberg, Citation1979) and/or the Hamilton Depression Rating Scale (Hamilton, Citation1960). Self-rated scales, such as the 21-item BDI (Beck et al., Citation1961), 16-Item Quick Inventory of Depressive Symptomatology (Rush et al., Citation2003) and nine-item PHQ-9 (Spitzer et al., Citation1999), may offer practical alternatives, particularly when time and/or resources are limited. Some quality of life measures, such as the World Health Organisation Quality of Life questionnaire, also include assessment of depressive symptoms (WHO, 1998). Additionally, since suicidality represents a detrimental condition that frequently occurs in the course of MDD as well as in individuals suffering from severe depressive symptoms who are, however, not officially diagnosed and who are, consequently, under- or even untreated, the use of specific scales, such as the Columbia-Suicide Severity Rating Scale (Posner et al., Citation2011), might be of relevance. Residual symptoms of depression, such as cognitive impairment, insomnia, fatigue and anhedonia, may require additional clinical assessments and measures (Israel, Citation2010). Finally, it is important to point out that although depression-related sick leave duration might not be a viable marker for severity of depression on its own, it could potentially be useful as an endpoint to assess functional recovery.
Summary
Depression-related sick leave has a profound economic impact on society. However, the instigation of effective pharmacological and non-pharmacological treatments for depression, together with the implementation of targeted work-based interventions, can decrease the duration of depression-related sick leave and facilitate RTW, helping individuals to return to their usual functioning level at work, thereby increasing their quality of life. Depression-related sick leave duration is influenced by multiple disease-, patient- and work-related factors, together with the wider socioeconomic climate and societal attitudes towards depression and sick leave provision. Consequently, although depression-related sick leave duration is affected by the severity of depressive symptoms and/or responsiveness to treatment, it cannot be used alone as a viable marker for disease severity, but might be used as secondary indicator of disease severity alongside more formal clinician- and patient-rated instruments. Nevertheless, depression-related sick leave duration does appear to reflect patients’ functional ability and might, therefore, potentially represent a useful outcome measure to assess patient functioning, in both the research and clinical settings. In addition, sick leave in the absence of other obvious medical conditions might signpost the need for screening for depression.
Acknowledgements
Editorial assistance was provided by John Scopes of mXm Medical Communications.
Disclosure statement
HPV has served as a consultant or on advisory boards for Astra/Zeneca, Eli Lilly, Lundbeck, Pfizer, Schwabe, Janssen, Otsuka, Angelini and Sage and has served on speakers’ bureaus for Astra/Zeneca, Eli Lilly, Lundbeck, Schwabe, Janssen, Bayer, Recordati and Neuraxpharm. EB has received honoraria from Angelini. LB has received travel grants and consultant/speaker honoraria from AOP Orphan, Medizin Medien Austria, Vertretungsnetz, Schwabe Austria, Janssen and Angelini. JD is a consultant to Angelini. HK reports compensation by Angelini and Janssen for the delivery of lectures. ML has served as a consultant on advisory boards for Angelini and has received consulting and lecturing fees from Angelini, Gedeon Richter, Janssen and Servier in the last year. JL reports participating in an advisory role for Angelini. MR reports receiving grants from the European Union, the Spanish Ministry of Economy and Competitiveness and research funding or fees from Angelini, Janssen and Lundbeck. GU reports serving on advisory boards or providing consultancy for Abbott and Angelini and has received speaker’s fees/honoraria from Angelini, Servier, Lundbeck, Abbott, Pfizer/Viatris and Krka. He has also received travel support from Servier, Lundbeck, Abbott and Pfizer. SK has received grants/research support, consulting fees and/or honoraria within the last three years, including grant/research support from Lundbeck. He has also served as a consultant or on advisory boards for Celegne, IQVIA, Janssen, Lundbeck, Mundipharma, Recordati, Takeda and Schwabe, and on speaker’s bureaus for Angelini, Aspen Farmaceutica S.A., Janssen, Krka, Lundbeck, Medichem Pharmaceuticals Inc., Neuraxpharma, OM Pharma, Pierre Fabre, Sanofi, Servier, Schwabe, Sun Pharma. All authors received honoraria from Angelini for their consultant/advisory role in the advisory board meeting that led to the development of this manuscript.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Ammerman, R. T., Chen, J., Mallow, P. J., Rizzo, J. A., Folger, A. T., & Van Ginkel, J. B. (2016). Annual direct health care expenditures and employee absenteeism costs in high-risk, low-income mothers with major depression. Journal of Affective Disorders, 190, 386–394. doi:10.1016/j.jad.2015.10.025
- Arends, I., Almansa, J., Stansfeld, S. A., Amick, B. C., van der Klink, J. J. L., & Bültmann, U. (2019). One-year trajectories of mental health and work outcomes post return to work in patients with common mental disorders. Journal of Affective Disorders, 257, 263–270. doi:10.1016/j.jad.2019.07.018
- Arnaez, J. M., Krendl, A. C., McCormick, B. P., Chen, Z., & Chomistek, A. K. (2020). The association of depression stigma with barriers to seeking mental health care: A cross-sectional analysis. Journal of Mental Health, 29(2), 182–190. doi:10.1080/09638237.2019.1644494
- Asami, Y., Goren, A., & Okumura, Y. (2015). Work productivity loss with depression, diagnosed and undiagnosed, among workers in an Internet-based survey conducted in Japan. Journal of Occupational and Environmental Medicine, 57(1), 105–110. doi:10.1097/JOM.0000000000000310
- Batada, A., & Solano, R. L. (2019). Harnessing Technology to Address the Global Mental Health Crisis: An Introductory Brief. World Bank Group. Retrieved September 2021. https://openknowledge.worldbank.org/bitstream/handle/10986/31766/Harnessing-Technology-to-Address-the-Global-Mental-Health-Crisis.pdf?sequence=1&isAllowed=y
- Beck, A., Crain, A. L., Solberg, L. I., Unützer, J., Glasgow, R. E., Maciosek, M. V., & Whitebird, R. (2011). Severity of depression and magnitude of productivity loss. The Annals of Family Medicine, 9(4), 305–311. doi:10.1370/afm.1260
- Beck, A., Crain, L. A., Solberg, L. I., Unützer, J., Maciosek, M. V., Whitebird, R. R., & Rossom, R. C. (2014). The effect of depression treatment on work productivity. The American Journal of Managed Care, 20(8), e294–301.
- Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571. doi:10.1001/archpsyc.1961.01710120031004
- Beiwinkel, T., Eißing, T., Telle, N. T., Siegmund-Schultze, E., & Rössler, W. (2017). Effectiveness of a web-based intervention in reducing depression and sickness absence: Randomized controlled trial. Journal of Medical Internet Research, 19(6), e213. doi:10.2196/jmir.6546
- Bhui, K. S., Dinos, S., Stansfeld, S. A., & White, P. D. (2012). A synthesis of the evidence for managing stress at work: A review of the reviews reporting on anxiety, depression, and absenteeism. Journal of Environmental and Public Health, 2012, 515874. doi:10.1155/2012/515874
- Block, G., Sternfeld, B., Block, C. H., Block, T. J., Norris, J., Hopkins, D., Quesenberry, C. P. Jr., Husson, G., & Clancy, H. A. (2008). Development of Alive! (A Lifestyle Intervention Via Email), and its effect on health-related quality of life, presenteeism, and other behavioral outcomes: randomized controlled trial. Journal of Medical Internet Research, 10(4), e43. doi:10.2196/jmir.1112
- Bouwmans, C. A., Vemer, P., van Straten, A., Tan, S. S., & Hakkaart-van Roijen, L. (2014). Health-related quality of life and productivity losses in patients with depression and anxiety disorders. Journal of Occupational and Environmental Medicine, 56(4), 420–424. doi:10.1097/JOM.0000000000000112
- Caballero-Martínez, F., León-Vázquez, F., Payá-Pardo, A., & Díaz-Holgado, A. (2014). Use of health care resources and loss of productivity in patients with depressive disorders seen in Primary Care: INTERDEP Study. Actas Espanolas de Psiquiatria, 42(6), 281–291.
- Chisholm, D., Sweeny, K., Sheehan, P., Rasmussen, B., Smit, F., Cuijpers, P., & Saxena, S. (2016). Scaling-up treatment of depression and anxiety: A global return on investment analysis. The Lancet. Psychiatry, 3(5), 415–424. doi:10.1016/S2215-0366(16)30024-4
- Chokka, P., Bougie, J., Rampakakis, E., & Proulx, J. (2019). Assessment in work productivity and the relationship with cognitive symptoms (AtWoRC): primary analysis from a Canadian open-label study of vortioxetine in patients with major depressive disorder (MDD). CNS Spectrums, 24(3), 338–347. doi:10.1017/S1092852918000913
- Clark, M., DiBenedetti, D., & Perez, V. (2016). Cognitive dysfunction and work productivity in major depressive disorder. Expert Review of Pharmacoeconomics & Outcomes Research, 16(4), 455–463. doi:10.1080/14737167.2016.1195688
- Cohen, D. (2017). Cancer drugs: High price, uncertain value. BMJ (Clinical Research ed.), 359, j4543. doi:10.1136/bmj.j4543
- Corbière, M., Renard, M., St-Arnaud, L., Coutu, M. F., Negrini, A., Sauvé, G., & Lecomte, T. (2015). Union perceptions of factors related to the return to work of employees with depression. Journal of Occupational Rehabilitation, 25(2), 335–347. doi:10.1007/s10926-014-9542-5
- de Graaf, R., Tuithof, M., Dorsselaer, S., & ten Have, M. (2012). Comparing the effects on work performance of mental and physical disorders. Social Psychiatry and Psychiatric Epidemiology, 47(11), 1873–1883. doi:10.1007/s00127-012-0496-7
- de Vries, G., Koeter, M. W., Nabitz, U., Hees, H. L., & Schene, A. H. (2012). Return to work after sick leave due to depression; a conceptual analysis based on perspectives of patients, supervisors and occupational physicians. Journal of Affective Disorders, 136(3), 1017–1026. doi:10.1016/j.jad.2011.06.035
- Dewa, C. S., Thompson, A. H., & Jacobs, P. (2011). The association of treatment of depressive episodes and work productivity. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 56(12), 743–750. doi:10.1177/070674371105601206
- Endo, M., Haruyama, Y., Mitsui, K., Muto, G., Nishiura, C., Kuwahara, K., Wada, H., & Tanigawa, T. (2019). Durations of first and second periods of depression-induced sick leave among Japanese employees: The Japan sickness absence and return to work (J-SAR) study. Industrial Health, 57(1), 22–28. doi:10.2486/indhealth.2018-0023
- Ervasti, J., Joensuu, M., Pentti, J., Oksanen, T., Ahola, K., Vahtera, J., Kivimäki, M., & Virtanen, M. (2017). Prognostic factors for return to work after depression-related work disability: A systematic review and meta-analysis. Journal of Psychiatric Research, 95, 28–36. doi:10.1016/j.jpsychires.2017.07.024
- Ervasti, J., Vahtera, J., Pentti, J., Oksanen, T., Ahola, K., Kivekäs, T., Kivimäki, M., & Virtanen, M. (2015). Return to work after depression-related absence by employees with and without other health conditions: A cohort study. Psychosomatic Medicine, 77(2), 126–135. doi:10.1097/PSY.0000000000000138
- Ervasti, J., Vahtera, J., Virtanen, P., Pentti, J., Oksanen, T., Ahola, K., Kivimäki, M., & Virtanen, M. (2014). Is temporary employment a risk factor for work disability due to depressive disorders and delayed return to work? The Finnish Public Sector Study. Scandinavian Journal of Work, Environment & Health, 40(4), 343–352. doi:10.5271/sjweh.3424
- Evans-Lacko, S., & Knapp, M. (2016). Global patterns of workplace productivity for people with depression: Absenteeism and presenteeism costs across eight diverse countries. Social Psychiatry and Psychiatric Epidemiology, 51(11), 1525–1537. doi:10.1007/s00127-016-1278-4
- Evans-Lacko, S., & Knapp, M. (2018). Is manager support related to workplace productivity for people with depression: A secondary analysis of a cross-sectional survey from 15 countries. BMJ Open, 8(6), e021795. doi:10.1136/bmjopen-2018-021795
- Farrants, K., Friberg, E., Sjölund, S., & Alexanderson, K. (2018). Work disability trajectories among individuals with a sick-leave spell due to depressive episode ≥ 21 days: A prospective cohort study with 13-month follow up. Journal of Occupational Rehabilitation, 28(4), 678–690. doi:10.1007/s10926-017-9751-9
- Flach, P. A., Groothoff, J. W., Krol, B., & Bültmann, U. (2012). Factors associated with first return to work and sick leave durations in workers with common mental disorders. European Journal of Public Health, 22(3), 440–445. doi:10.1093/eurpub/ckr102
- GBD 2019 Diseases and Injuries Collaborators (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204–1222. doi:10.1016/S0140-6736(20)30925-9
- Geraedts, A. S., Fokkema, M., Kleiboer, A. M., Smit, F., Wiezer, N. W., Majo, M. C., van Mechelen, W., Cuijpers, P., & Penninx, B. W. (2014). The longitudinal prediction of costs due to health care uptake and productivity losses in a cohort of employees with and without depression or anxiety. Journal of Occupational and Environmental Medicine, 56(8), 794–801. doi:10.1097/JOM.0000000000000234
- Grahn, P., Pálsdóttir, A. M., Ottosson, J., & Jonsdottir, I. H. (2017). Longer nature-based rehabilitation may contribute to a faster return to work in patients with reactions to severe stress and/or depression. International Journal of Environmental Research and Public Health, 14(11), 1310. doi:10.3390/ijerph14111310
- Grenard, J. L., Munjas, B. A., Adams, J. L., Suttorp, M., Maglione, M., McGlynn, E. A., & Gellad, W. F. (2011). Depression and medication adherence in the treatment of chronic diseases in the United States: A meta-analysis. Journal of General Internal Medicine, 26(10), 1175–1182. doi:10.1007/s11606-011-1704-y
- Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23(1), 56–62. doi:10.1136/jnnp.23.1.56
- Hees, H. L., de Vries, G., Koeter, M. W., & Schene, A. H. (2013). Adjuvant occupational therapy improves long-term depression recovery and return-to-work in good health in sick-listed employees with major depression: Results of a randomised controlled trial. Occupational and Environmental Medicine, 70(4), 252–260. doi:10.1136/oemed-2012-100789
- Hees, H. L., Koeter, M. W., & Schene, A. H. (2012). Predictors of long-term return to work and symptom remission in sick-listed patients with major depression. The Journal of Clinical Psychiatry, 73(8), e1048–e1055. doi:10.4088/JCP.12m07699
- Hellerstein, D. J., Erickson, G., Stewart, J. W., McGrath, P. J., Hunnicutt-Ferguson, K., Reynolds, S. K., O’Shea, D., Chen, Y., Withers, A., & Wang, Y. (2015). Behavioral activation therapy for return to work in medication-responsive chronic depression with persistent psychosocial dysfunction. Comprehensive Psychiatry, 57, 140–147. doi:10.1016/j.comppsych.2014.10.015
- Hellström, L., Bech, P., Hjorthøj, C., Nordentoft, M., Lindschou, J., & Eplov, L. F. (2017). Effect on return to work or education of individual placement and support modified for people with mood and anxiety disorders: Results of a randomised clinical trial. Occupational and Environmental Medicine, 74(10), 717–725. doi:10.1136/oemed-2016-104248
- Huijs, J. J. J. M., Koppes, L. L. J., Taris, T. W., & Blonk, R. W. B. (2017). Work characteristics and return to work in long-term sick-listed employees with depressive symptoms. Journal of Occupational Rehabilitation, 27(4), 612–622. doi:10.1007/s10926-017-9696-z
- Ipsos (2012). IDEA: Impact of Depression at Work in Europe Audit. Ipsos Healthcare. Retrieved September 2021, from https://www.europeandepressionday.eu/2019/04/11/idea/
- Israel, J. A. (2010). The impact of residual symptoms in major depression. Pharmaceuticals, 3(8), 2426–2440. doi:10.3390/ph3082426
- Jain, G., Roy, A., Harikrishnan, V., Yu, S., Dabbous, O., & Lawrence, C. (2013). Patient-reported depression severity measured by the PHQ-9 and impact on work productivity: Results from a survey of full-time employees in the United States. Journal of Occupational & Environmental Medicine, 55(3), 252–258. doi:10.1097/JOM.0b013e31828349c9
- Jha, M. K., Minhajuddin, A., Greer, T. L., Carmody, T., Rush, A. J., & Trivedi, M. H. (2016). Early improvement in work productivity predicts future clinical course in depressed outpatients: Findings from the CO-MED trial. The American Journal of Psychiatry, 173(12), 1196–1204. doi:10.1176/appi.ajp.2016.16020176
- Johnston, D. A., Harvey, S. B., Glozier, N., Calvo, R. A., Christensen, H., & Deady, M. (2019). The relationship between depression symptoms, absenteeism and presenteeism. Journal of Affective Disorders, 256, 536–540. doi:10.1016/j.jad.2019.06.041
- Kaldo, V., Lundin, A., Hallgren, M., Kraepelien, M., Strid, C., Ekblom, Ö., Lavebratt, C., Lindefors, N., Öjehagen, A., & Forsell, Y. (2018). Effects of internet-based cognitive behavioural therapy and physical exercise on sick leave and employment in primary care patients with depression: Two subgroup analyses. Occupational and Environmental Medicine, 75(1), 52–58. doi:10.1136/oemed-2017-104326
- Kasper, S., Bonelli, A., Cattaneo, A., Comandini, A., Di Dato, G., Heiman, F., Pegoraro, V., Palao, D., Roca, M., & Volz, H. P. (2021). Predictors of sick leave days in patients affected by major depressive disorder receiving antidepressant treatment in general practice setting in Germany. International Journal of Psychiatry in Clinical Practice, 25(4), 393–402. doi:10.1080/13651501.2021.1972120
- Lagerveld, S. E., Blonk, R. W., Brenninkmeijer, V., Wijngaards-de Meij, L., & Schaufeli, W. B. (2012). Work-focused treatment of common mental disorders and return to work: A comparative outcome study. Journal of Occupational Health Psychology, 17(2), 220–234. doi:10.1037/a0027049
- Lerner, D., Adler, D. A., Rogers, W. H., Chang, H., Greenhill, A., Cymerman, E., & Azocar, F. (2015). A randomized clinical trial of a telephone depression intervention to reduce employee presenteeism and absenteeism. Psychiatric Services, 66(6), 570–577. doi:10.1176/appi.ps.201400350
- Liu, Q., He, H., Yang, J., Feng, X., Zhao, F., & Lyu, J. (2020). Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. Journal of Psychiatric Research, 126, 134–140. doi:10.1016/j.jpsychires.2019.08.002
- Melin, E. O., Svensson, R., & Thulesius, H. O. (2018). Psychoeducation against depression, anxiety, alexithymia and fibromyalgia: A pilot study in primary care for patients on sick leave. Scandinavian Journal of Primary Health Care, 36(2), 123–133. doi:10.1080/02813432.2018.1459225
- Mittendorfer-Rutz, E., Härkänen, T., Tiihonen, J., & Haukka, J. (2014). Association of socio-demographic factors, sick-leave and health care patterns with the risk of being granted a disability pension among psychiatric outpatients with depression. PLOS One, 9(6), e99869. doi:10.1371/journal.pone.0099869
- Montgomery, S. A., & Asberg, M. (1979). A new depression scale designed to be sensitive to change. The British Journal of Psychiatry, 134, 382–389. doi:10.1192/bjp.134.4.382
- Morita, G., Hori, H., Katsuki, A., Nishii, S., Shibata, Y., Kubo, T., Suga, K., Yoshimura, R., & Nakamura, J; STAND UP JOE Group (2016). Decreased activity at the time of return to work predicts repeated sick leave in depressed Japanese patients. Journal of Occupational and Environmental Medicine, 58(2), e56–e57. doi:10.1097/JOM.0000000000000649
- Muijzer, A., Brouwer, S., Geertzen, J. H., & Groothoff, J. W. (2012). Exploring factors relevant in the assessment of the return-to-work process of employees on long-term sickness absence due to a depressive disorder: A focus group study. BMC Public Health, 12, 103. doi:10.1186/1471-2458-12-103
- Negrini, A., Corbière, M., Lecomte, T., Coutu, M. F., Nieuwenhuijsen, K., St-Arnaud, L., Durand, M. J., Gragnano, A., & Berbiche, D. (2018). How can supervisors contribute to the return to work of employees who have experienced depression? Journal of Occupational Rehabilitation, 28(2), 279–288. doi:10.1007/s10926-017-9715-0
- Netterstrøm, B., Eller, N. H., & Borritz, M. (2015). Prognostic factors of returning to work after sick leave due to work-related common mental disorders: A one- and three-year follow-up study. BioMed Research International, 2015;2015:596572. doi:10.1155/2015/596572
- Nielsen, M. B., Rugulies, R., Hjortkjaer, C., Bültmann, U., & Christensen, U. (2013). Healing a vulnerable self: Exploring return to work for women with mental health problems. Qualitative Health Research, 23(3), 302–312. doi:10.1177/1049732312468252
- Nieuwenhuijsen, K., Faber, B., Verbeek, J. H., Neumeyer-Gromen, A., Hees, H. L., Verhoeven, A. C., van der Feltz-Cornelis, C. M., & Bültmann, U. (2014). Interventions to improve return to work in depressed people. The Cochrane Database of Systematic Reviews, 3(12), CD006237. doi:10.1002/14651858.CD006237.pub3.
- Ogawa, T., Shigemura, J., Yoshino, A., & Nomura, S. (2013). Interpersonal sensitivity associated with return to work status following sick leave: A cross-sectional study among Japanese workers with major depressive disorder. Asian Journal of Psychiatry, 6(2), 146–150. doi:10.1016/j.ajp.2012.10.006
- Paykel, E. S. (2008). Partial remission, residual symptoms, and relapse in depression. Dialogues in Clinical Neuroscience, 10(4), 431–437. doi:10.31887/DCNS.2008.10.4/espaykel.
- Pedrelli, P., Baer, L., Losifescu, D. V., & Fava, M. (2010). Relationship between residual symptoms of depression and self-reported cognitive impairment. CNS Spectrums, 15(1), 46–51. doi:10.1017/s1092852900000298
- Poolsup, N., Li Wan Po, A., & Knight, T. L. (2000). Pharmacogenetics and psychopharmacotherapy. Journal of Clinical Pharmacy and Therapeutics, 25(3), 197–220. doi:10.1046/j.1365-2710.2000.00281.x
- Posner, K., Brown, G. K., Stanley, B., Brent, D. A., Yershova, K. V., Oquendo, M. A., Currier, G. W., Melvin, G. A., Greenhill, L., Shen, S., & Mann, J. J. (2011). The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. The American Journal of Psychiatry, 168(12), 1266–1277. doi:10.1176/appi.ajp.2011.10111704
- Poulsen, R., Hoff, A., Fisker, J., Hjorthøj, C., & Eplov, L. F. (2017). Integrated mental health care and vocational rehabilitation to improve return to work rates for people on sick leave because of depression and anxiety (the Danish IBBIS trial): Study protocol for a randomized controlled trial. Trials, 18(1), 578. doi:10.1186/s13063-017-2272-1
- Romera, I., Pérez, V., Ciudad, A., Caballero, L., Roca, M., Polavieja, P., & Gilaberte, I. (2013). Residual symptoms and functioning in depression, does the type of residual symptom matter? A post-hoc analysis. BMC Psychiatry, 13, 51. doi:10.1186/1471-244X-13-51
- Rost, K. M., Meng, H., & Xu, S. (2014). Work productivity loss from depression: Evidence from an employer survey. BMC Health Services Research, 14, 597. doi:10.1186/s12913-014-0597-y
- Rush, A. J., Trivedi, M. H., Ibrahim, H. M., Carmody, T. J., Arnow, B., Klein, D. N., Markowitz, J. C., Ninan, P. T., Kornstein, S., Manber, R., Thase, M. E., Kocsis, J. H., & Keller, M. B. (2003). The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583. doi:10.1016/s0006-3223(02)01866-8
- Rush, A. J., Trivedi, M. H., Stewart, J. W., Nierenberg, A. A., Fava, M., Kurian, B. T., Warden, D., Morris, D. W., Luther, J. F., Husain, M. M., Cook, I. A., Shelton, R. C., Lesser, I. M., Kornstein, S. G., & Wisniewski, S. R. (2011). Combining medications to enhance depression outcomes (CO-MED): Acute and long-term outcomes of a single-blind randomized study. The American Journal of Psychiatry, 168(7), 689–701. doi:10.1176/appi.ajp.2011.10111645
- Saridi, M., Kordosi, A., Toska, A., Peppou, L. E., Economou, M., & Souliotis, K. (2017). Attitudes of health professionals towards the stigma surrounding depression in times of economic crisis. The International Journal of Social Psychiatry, 63(2), 115–125. doi:10.1177/0020764016685348
- Spitzer, R. L., Kroenke, K., & Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA, 282(18), 1737–1744. doi:10.1001/jama.282.18.1737
- Streibelt, M., Bürger, W., Nieuwenhuijsen, K., & Bethge, M. (2018). Effectiveness of graded return to work after multimodal rehabilitation in patients with mental disorders: A propensity score analysis. Journal of Occupational Rehabilitation, 28(1), 180–189. doi:10.1007/s10926-017-9709-y
- Teo, Y. L., Ho, H. K., & Chan, A. (2015). Metabolism-related pharmacokinetic drug-drug interactions with tyrosine kinase inhibitors: Current understanding, challenges and recommendations. British Journal of Clinical Pharmacology, 79(2), 241–253. doi:10.1111/bcp.12496
- Trivedi, D. (2018). Cochrane Review Summary: Interventions to improve return to work in depressed people. Primary Health Care Research & Development, 19(2), 107–109. doi:10.1017/S1463423617000482
- Trivedi, M. H., Morris, D. W., Wisniewski, S. R., Lesser, I., Nierenberg, A. A., Daly, E., Kurian, B. T., Gaynes, B. N., Balasubramani, G. K., & Rush, A. J. (2013). Increase in work productivity of depressed individuals with improvement in depressive symptom severity. The American Journal of Psychiatry, 170(6), 633–641. doi:10.1176/appi.ajp.2012.12020250
- United Nations. (2020). Policy brief: COVID-19 and the need for action on mental health. United Nations. Retrieved September 2021, from https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf
- Vlasveld, M. C., van der Feltz-Cornelis, C. M., Anema, J. R., van Mechelen, W., Beekman, A. T., van Marwijk, H. W., & Penninx, B. W. (2013). The associations between personality characteristics and absenteeism: A cross-sectional study in workers with and without depressive and anxiety disorders. Journal of Occupational Rehabilitation, 23(3), 309–317. doi:10.1007/s10926-012-9406-9
- Volker, D., Zijlstra-Vlasveld, M. C., Anema, J. R., Beekman, A. T., Brouwers, E. P., Emons, W. H., van Lomwel, A. G., & van der Feltz-Cornelis, C. M. (2015). Effectiveness of a blended web-based intervention on return to work for sick-listed employees with common mental disorders: Results of a cluster randomized controlled trial. Journal of Medical Internet Research, 17(5), e116. doi:10.2196/jmir.4097
- Wang, M., Alexanderson, K., Runeson, B., Head, J., Melchior, M., Perski, A., & Mittendorfer-Rutz, E. (2014). Are all-cause and diagnosis-specific sickness absence, and sick-leave duration risk indicators for suicidal behaviour? A nationwide register-based cohort study of 4.9 million inhabitants of Sweden. Occupational and Environmental Medicine, 71(1), 12–20. doi:10.1136/oemed-2013-101462
- Wang, M., Alexanderson, K., Runeson, B., & Mittendorfer-Rutz, E. (2015). Sick-leave measures, socio-demographic factors and health care as risk indicators for suicidal behavior in patients with depressive disorders-a nationwide prospective cohort study in Sweden. Journal of Affective Disorders, 173, 201–210. doi:10.1016/j.jad.2014.10.069
- Waters, R., Urquhart, L. EvaluatePharma® World Preview 2019, Outlook to 2024. Evaluate Ltd., (2019). Retrieved September 2021, from https://info.evaluate.com/rs/607-YGS-364/images/EvaluatePharma_World_Preview_2019.pdf
- Wedegaertner, F., Arnhold-Kerri, S., Sittaro, N. A., Bleich, S., Geyer, S., & Lee, W. E. (2013). Depression- and anxiety-related sick leave and the risk of permanent disability and mortality in the working population in Germany: A cohort study. BMC Public Health, 13, 145. doi:10.1186/1471-2458-13-145
- Wisenthal, A., & Krupa, T. (2013). Cognitive work hardening: a return-to-work intervention for people with depression. Work, 45(4), 423–430. doi:10.3233/WOR-131635
- Wisenthal, A., & Krupa, T. (2014). Using intervention mapping to deconstruct cognitive work hardening: A return-to-work intervention for people with depression. BMC Health Services Research, 14, 530. doi:10.1186/s12913-014-0530-4
- Wisenthal, A., Krupa, T., Kirsh, B. H., & Lysaght, R. (2018). Cognitive work hardening for return to work following depression: An intervention study: Le réentraînement cognitif au travail pour favoriser le retour au travail à la suite d'une dépression : étude d'intervention. Canadian Journal of Occupational Therapy, 85(1), 21–32. doi:10.1177/0008417417733275
- Wisenthal, A., Krupa, T., Kirsh, B., & Lysaght, R. (2019). Insights into cognitive work hardening for return-to-work following depression: Qualitative findings from an intervention study. Work (Reading, Mass.), 62(4), 599–613. doi:10.3233/WOR-192893
- Woo, J. M., Kim, W., Hwang, T. Y., Frick, K. D., Choi, B. H., Seo, Y. J., Kang, E. H., Kim, S. J., Ham, B. J., Lee, J. S., & Park, Y. L. (2011). Impact of depression on work productivity and its improvement after outpatient treatment with antidepressants. Value in Health, 14(4), 475–482. doi:10.1016/j.jval.2010.11.006
- World Health Organization (WHO) (2021). WHO special initiative for mental health (2019–2023). WHO, Retrieved September 2019, from https://www.who.int/initiatives/who-special-initiative-for-mental-health
- World Health Organization (WHO) (2021). WHOQOL user manual. WHO, Retrieved September 1998, from https://www.who.int/tools/whoqol
- Yokoya, S., Maeno, T., Sakamoto, N., Goto, R., & Maeno, T. (2018). A brief survey of public knowledge and stigma towards depression. Journal of Clinical Medicine Research, 10(3), 202–209. doi:10.14740/jocmr3282w
- Zimmerman, M., McGlinchey, J. B., Posternak, M. A., Friedman, M., Attiullah, N., & Boerescu, D. (2006). How should remission from depression be defined? The depressed patient's perspective. The American Journal of Psychiatry, 163(1), 148–150. doi:10.1176/appi.ajp.163.1.148
