Abstract
Objective
The aim of this study was to complete a scoping review of the published literature describing the relationship between mental fatigue and various psychiatric disorders, to better understand its frequency and clinical impact, and to provide recommendations for future clinical research.
Methods
A scoping review using PubMed/MEDLINE, Cochrane and PsychArticles databases was conducted using the keywords ‘mental fatigue’, ‘mental tiredness’ or ‘mental exhaustion’, and completed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols Extension for Scoping Reviews 2018 checklist.
Results
We extracted 10 studies fulfilling our inclusion criteria from a total of 2937 publications. Mental fatigue was studied within mood disorders, anxiety disorders, obsessive compulsive disorder and obsessive-compulsive personality disorder. A commonly used tool to measure mental fatigue in these samples was the Multidimensional Fatigue Inventory-20. Specific cognitive factors (unhelpful beliefs about sleep, symptom-focussed rumination) and personality risk factors (harm avoidance, self-directedness, cooperativeness, persistence) were relevant to predicting mental fatigue symptoms and rates of mental fatigue may vary with gender and diagnosis.
Conclusion
Research into mental fatigue in adult psychiatric sample was limited to a few psychiatric disorders and requires further investigation.
A commonly used tool to measure mental fatigue was the Multidimensional Fatigue Inventory-20. However, more research into the validity and reliability for illness specific instruments to measure mental fatigue in psychiatric population is required.
Reduction of mental fatigue was associated with improvement on quality of life.
Specific cognitive factors (unhelpful beliefs about sleep, symptom-focussed rumination) and personality risk factors (harm avoidance, self-directedness, cooperativeness, persistence) were relevant to predicting mental fatigue symptoms and rates of mental fatigue may vary with gender.
Reviewed articles indicated that mental fatigue presence was associated with lower odds of OCD. In addition, the results suggested that mental fatigue symptoms were more common in individuals with OCPD rather than OCD.
Research into mental fatigue in adult psychiatric sample was limited to a few psychiatric disorders and requires further investigation to prevent potential misattribution as mental fatigue symptoms overlap between different psychiatric disorders.
Key points
Introduction
Mental fatigue reflects a psychobiological state characterised by subjective feelings of tiredness and lack of motivation (Herlambang et al., Citation2019; Lorist, Citation2008; Morris & Christie, Citation2020; van Cutsem et al., Citation2017), alongside poor cognitive and behavioural performance leading to diminished attention and concentration (Boksem et al., Citation2005; de Raaf et al., Citation2013; Guo et al., Citation2016; Morris & Christie, Citation2020), poor executive planning (Lorist et al., Citation2000; Qi et al., Citation2019) and difficulties focussing on the task at hand (Boksem & Tops, Citation2008). It can be differentiated from other recognised forms of fatigue by key aspects of its symptom-profile. Thus, unlike mental fatigue, physical fatigue is characterised as a decrease in physical performance due to physical inability to maintain the required level of strength (Abd-Elfattah et al., Citation2015) and social fatigue by increased withdrawal from social relationships (Nagy et al., Citation2018).
Mental fatigue is considered a common core symptom of various psychiatric disorders, especially anxiety and mood disorders (AMD), such as generalised anxiety disorder and depression. Fifth edition of Diagnostic and statistical manual of mental disorders (DSM-5) includes fatigue as a core symptom for both depression and generalised anxiety disorder (American Psychiatric Association, Citation2013). People with AMD complain of easy fatiguability (Sharma et al., Citation1990), which is not associated with previous exertion of effort (van der Linden, Citation2011) and tends to persist even after a positive clinical response to an adequate course of treatment. For example, a review by Fava and colleagues revealed that rates of residual fatigue reached up to 91% in some patient samples that included partial responders and remitters (Fava et al., Citation2014). However, despite its ubiquity, mental fatigue is a relatively under-researched field, and there is still no universally accepted definition.
Due to the gap of knowledge about mental fatigue, individuals with psychiatric disorders who suffer from mental fatigue may not gain adequate treatment and continue to suffer its long-term effects, including difficulties in engaging in everyday activities, such as work productivity, diminished psychosocial functioning (Fava et al., Citation2014), and may also be at increased risk of illness relapse (Targum & Fava, Citation2011).
A key challenge that besets the studies of mental fatigue in psychiatric disorders is the potential difficulty differentiating mental fatigue from other similar symptom domains. For example, in AMD, symptoms of anhedonia may resemble mental fatigue and be mistaken for it (Ghanean et al., Citation2018). Indeed a recent review comparing fatigue and anhedonia showed that many studies treated fatigue and anhedonia as indistinguishable constructs (Billones et al., Citation2020). However, unlike anhedonia, it is proposed that those suffering from mental fatigue can remain interested in activities and derive pleasure from them, but not have sufficient ‘mental energy’ to seek out or complete them (Ghanean et al., Citation2018).
In contrast, a considerable amount of research examining mental fatigue has been performed in samples comprising individuals with chronic noncommunicable diseases such as cancer, multiple sclerosis, heart disease, and renal disease (Demyttenaere et al., Citation2005). Examination of different chronic conditions showed that various health outcomes correlate with mental fatigue. In individuals with oncological diagnoses, mental fatigue was found to be one of the main persisting symptoms (van der Linden et al., Citation2020), associated with sleep problems and pain levels (de Raaf et al., Citation2013). In traumatic brain injury group, mental fatigue was present regardless the severity of injury and had a negative impact on employment status (Palm et al., Citation2017). In individuals with multiple sclerosis, higher levels of mental fatigue were associated with poor sleep quality (Berard et al., Citation2019; Trojan et al., Citation2007), suicidal ideation (Mikula et al., Citation2020) and lower self-efficacy (Trojan et al., Citation2007). Higher levels of anxiety and depression correlated with the presence of mental fatigue in individuals with a cardiac pacemaker (Polikandrioti et al., Citation2018), cancer (de Raaf et al., Citation2013), multiple sclerosis (Arnett et al., Citation2008; Takeda et al., Citation2021; Trojan et al., Citation2007) and after traumatic brain injury (Johansson, Citation2021; Lindstedt et al., Citation2019).
It is important to highlight the role that the Coronavirus disease 2019 (COVID-19) may have had on mental fatigue. It has been proposed that mental fatigue might represent a specific psychological response to pandemic conditions (Morgul et al., Citation2021). In a study by Bartoszek and colleagues (Citation2020), adult citizens reported experiencing greater levels of mental fatigue, compared with other forms of fatigue such as physical or social fatigue. In another general population study, mental fatigue was found to negatively impact emotional symptoms, predicting depressive symptoms (Torrente et al., Citation2021). Health professionals have been particularly affected by COVID-19 and higher levels of mental fatigue in this population were found to correlate with greater levels of anxiety and depression (Teng et al., Citation2020; Zhan et al., Citation2020). To sum up, mental fatigue is commonly associated with various health-related conditions and adversely impacts emotional status and functional capacity.
However, surprisingly little is known about the causes and consequences of mental fatigue in the context of psychiatric disorders, or its response to treatment and the impact it has on health-related quality of life. Due to such circumstances, a scoping review can be a perfect tool to help examine the emerging evidence and provide an overview of evidence for an unclear topic before addressing in with a more precise systematic review (Munn et al., Citation2018). The current study aims to complete a scoping review of the existing peer reviewed literature on mental fatigue in adults with psychiatric disorders, to derive new insights into its causes and impacts, as well as to identify aspects requiring further research.
Methods
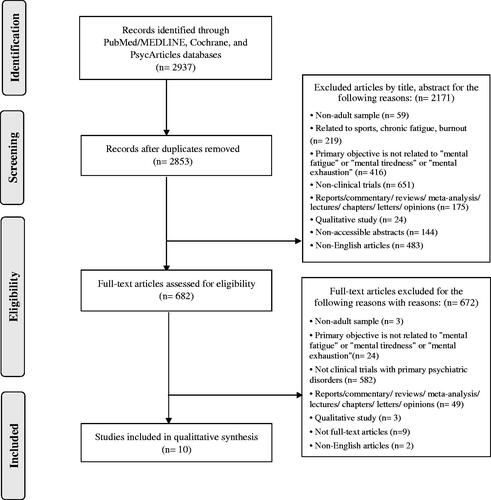
The scoping review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) (Tricco et al., Citation2018). A narrative data synthesis method was applied. A descriptive synthesis was also implemented by text and tables to provide a summary, explanation of study characteristics and findings ().
Table 1. Characteristics of selected studies.
Search strategy
Two authors (KM and AS) independently searched PubMed/MEDLINE Cochrane, and PsycArticles databases from the 14th till the 17th of January 2021. Keywords used in the current scoping review included: ‘mental fatigue’ or ‘mental tiredness’ or ‘mental exhaustion’. To ensure validity, selected studies were independently evaluated by two reviewers (KM and AS) for inclusion, exclusion criteria. Authors’ preliminary screened the titles and then abstracts for eligibility, and later comprehensively reviewed the full-text articles that were retrieved and independently verified for eligibility by the same authors in accordance with the criteria.
Eligibility criteria
The inclusion criteria used for the study: (1) the studied sample – adults with psychiatric disorders, as defined by any operational defined criteria (e.g., DSM-IV, DSM–IV–TR, DSM-5, Research Diagnostic criteria), (2) articles aiming to measure ‘mental fatigue’ or ‘mental tiredness’ or ‘mental exhaustion’, (3) observational and experimental studies were included, (4) no requirements for having a comparator group, (5) published peer-reviewed work, (6) clinical studies, (7) English written articles.
The exclusion criteria that were followed for the study: (1) healthy population, (2) non-adult sample, (3) articles on solely chronic fatigue, and other somatic disorders, (4) qualitative studies, reviews, meta-analyses, commentaries, editorials, opinion pieces, and others not reporting empirical data, (5) not full-text articles.
Data extraction and management
Two authors (AS and KM) independently extracted the data from the eligible articles following: study design; methodology; participants demographic information; mental fatigue scores and mental fatigue assessment tools. Discrepancies between authors were resolved through consensus. When a consensus was not reached, two other reviewers (JB and JGS) were consulted. In the case of missing information, the authors contacted study investigators for unreported data or additional details. Data were recorded in excel spreadsheets. In addition, a flowchart following the PRISMA guidelines (Moher et al., Citation2009) was created to demonstrate the different phases of the selection process ().
Figure 1. PRISMA-P 2009 Flow Chart of Study Selection. Query: (‘mental fatigue’ OR ‘mental tiredness’ OR ‘mental exhaustion’). Copyright: © 2009 Moher et al. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. PLoS Med 6(7):e1000097. doi: 10.1371/journal.pmed1000097.
Risk of bias (quality) assessment
Critical appraisal was conducted by two independent reviewers (KM and AS, see Appendix 1). They used Joanna Briggs Institute (JBI) Critical Appraisal Checklist for analytical cross sectional studies (Joanna Briggs Institute, Citation2020a) and for randomised controlled trials (Joanna Briggs Institute, Citation2020b).
Results
The research yielded 2937 studies, out of which 10 were included in the final analysis (). All 10 articles had an adequate methodological quality, as defined by JBI critical appraisal checklists. Three themes were retrieved from the selected studies, namely (1) Mental Fatigue within Mood Disorders, (2) Mental Fatigue within Anxiety Disorders and (3) Mental Fatigue within Obsessive Compulsive Disorder and Obsessive-Compulsive Personality Disorder (OCPD). Findings provide an overview of the existing empirical research on mental fatigue in an adult psychiatric population, focussing on the frequency, clinical impact and instruments used to measure mental fatigue.
The main characteristics of the selected articles are displayed in . Two studies were conducted in Canada (Carney et al., Citation2014; Dritsa et al., Citation2009), two in Japan (Jiang et al., Citation2003; Kaiya et al., Citation2008), one in China (Chung et al., Citation2014), one in Australia (Li et al., Citation2020) and the remaining four in European countries: United Kingdom (Wessely & Powell, Citation1989), Greece (Ferentinos et al., Citation2010), Italy (Pasquini et al., Citation2015), Lithuania (Gecaite-Stonciene et al., Citation2020). All included studies were quantitative in design with three having control groups including other psychiatric disorders or healthy controls. Two out of the 10 studies were randomised clinical trials, and eight cross-sectional. Half of the studies investigated individuals with primary depression in the categorisation of major depression disorder and postpartum depression (Carney et al., Citation2014; Chung et al., Citation2014; Dritsa et al., Citation2009; Ferentinos et al., Citation2010; Wessely & Powell, Citation1989). Three studies included subjects’ presenting with different forms of anxiety, including generalised anxiety disorder (Li et al., Citation2020) and panic disorder (Kaiya et al., Citation2008; Pasquini et al., Citation2015). One research paper was analysing mental fatigue in OCD population (Pasquini et al., Citation2015). One additional study explored anxiety within a cluster of different psychiatric disorders (Jiang et al., Citation2003) and one study explored OCDP within AMD (Gecaite-Stonciene et al., Citation2020). In addition, two research articles investigated mental fatigue measuring instruments of MFI-20 (Chung et al., Citation2014) and FQ-14 (Ferentinos et al., Citation2010) reliability and validity in a group of individuals with MDD. Within the studies, sample sizes ranged from 28 to 1364 participants. Individuals with affective disorders ranged in age from 32.67 to 49.6 years old on average (SD= 3.36–50.19). Furthermore, individuals with anxiety mean ages ranged from 19.55 to 47.5 (SD= 3.86–16), whereas individuals with OCD mean age ranged from 29.5 to 41.5 (SD= 23.7–41.5). Most of the participants in the selected publications were female, accounting from 32 to 100%of the total sample sizes.
The term ‘mental fatigue’ was used differently throughout the review. Nine out of 10 studies used the term ‘mental fatigue’, whereas one study used the term ‘psychological fatigue’, defining it as ‘difficulty concentrating the spirit’ (Jiang et al., Citation2003). The operational definition for mental fatigue was not consistently stated in included publications, and one study defined it by utilising the MFI-20 founders’ description of ‘cognitive symptoms, such as difficulties concentrating’. (Kaiya et al., Citation2008; Smets et al., Citation1995). Other studies, which used other questionnaires, did not provide a definition of mental fatigue, and covered a variety of mental fatigue-related topics. Questions on speech difficulties, such as slips of the tongue or difficulty finding the perfect word, were included in a research by Ferentinos et al. (Citation2010). A question on eyestrain was incorporated by Wessely and Powell (Citation1989).
The review findings are described in the sections below.
Mental fatigue within mood disorders
Psychometrics used to measure mental fatigue
Five articles reported using self-reported questionnaires of MFI-20 (Carney et al., Citation2014; Chung et al., Citation2014; Dritsa et al., Citation2009), FQ-14 (Ferentinos et al., Citation2010) or authors constructed 13 item questionnaire measuring different aspects of fatigue divided into eight ‘physical’ and five ‘mental’ complaints to measure mental fatigue in individuals with mood disorder (Wessely & Powell, Citation1989). The prevalence across research papers for MFI-20 ranged up to 16 with mean varying between 11.9–15.10 (SD= 3.52–4.54), for FQ-14 up to 18, with mean 11.9 (SD= 3.6) and the authors constructed questionnaire ranged up to 10 with mean 5.5 (SD= 4.4–6.6).
There were two research articles that investigated reliability and validity of instruments used to measure mental fatigue within individuals with MDD. Questionnaire MFI-20 (Chung et al., Citation2014) was assessed in 137 participants and FQ-14 (Ferentinos et al., Citation2010) in 81 participants. Results presented that both the Chinese version of MFI-20 and the FQ-14 had good internal consistency (αMFI-20= 0.89; αFQ-14= 0.924) and test–retest reliability (rMFI-20= 0.73; *ICCFQ-14= 0.978). Furthermore, Ferentinos et al. (Citation2010) found a two-factor structure of physical and mental fatigue in the FQ-14, which is similar to the original structure; however, items 3 (sleepiness), 4 (difficulty starting tasks) and 14 (loss of interest) did not load on the expected factor. It was seen that if these items removed, the derived 11-item version of the scale would show a ‘purer’ measure of fatigue in individuals experiencing depression symptoms, independent of the severity of depression and comorbid sleepiness. Thus, potentially being more helpful when following-up on fatigue-related complains in individuals with MDD. In addition, Chung et al. (Citation2014) study for MFI-20 indicated that mental fatigue has reported a stronger correlation to depression symptoms (*rHDRS17= 0.36; *rHADS= 0.45) rather than to anxiety (*rHDRS17= 0.29; *rHADS= 0.37), insomnia (*rHDRS= 0.04; *rISI= 0.13) or quality of life (*rSF-36= −0.46 to −0.26) measures. What is more, the reported significant negative correlations between the change scores of mental fatigue and SF-36 domains suggest that reduction of mental fatigue was related with an increase in quality of life.
Major depression disorder and mental fatigue
Researchers Wessely and Powell (Citation1989) investigated 47 unexplained chronic fatigue syndrome cases together with control groups of 33 neuromuscular illness and 26 individuals with MDD. The results showed that all three groups were severely physically fatigued and that there was no difference in total fatigue scores between CFS (M = 11.82 (10.8–13.03)) and MDD group (M = 10.35 (9.14–11.56), but both were significantly more fatigued than the neuromuscular cases (M = 8.28 (6.66–9.9). However, mental fatigue was equally prominent in the CFS and MDD groups (M = 5.84 (4.96–6.72), M = 5.5 (4.4–6.6), respectively), but less in the neuromuscular controls (M = 2.42 (1.46–3.38)). This suggests that mental fatigue and fatigability were as common in individuals with CFS and MDD as they were in individuals with neuromuscular disorders.
In addition, author Carney with colleagues (2014) investigated relationships between mental fatigue and sleep within 62 individuals with MDD with insomnia. Research results indicated that some of the predictors of mental fatigue symptom severity were cognitive factors, such as unhelpful beliefs about sleep measured by *DBAS-16 (Step 4: β = 0.40, p= <0.003) and symptom-focussed rumination (how often participants engaged in repetitive thought about how they were feeling in response to feeling tired) measured by *DISRS (Step 4: β = 0.38, p= <0.009). In addition, study found that some of the *DBAS-16 scale beliefs about sleep (poor sleep interferes with the ability to function (r = 0.446) and to enjoy life (r = 0.471); attribute poor functioning due to poor sleep (r = 0.277); negative mood is due to poor sleep (r = 0.310); when sleep is poor one should avoid or cancel obligations [r = 0.341]) were somewhat related to mental fatigue with low-medium correlation and could be important to investigate during clinical assessment.
Postpartum depression and mental fatigue
One research article by Dritsa et al. (Citation2009) investigated the effectiveness of home-based exercise to reduce mental fatigue within 88 women in the postpartum period (4–38 weeks) with possible to severe depression scores. The results indicated that low physical fatigue (MFI-20: ≤17 out of 20), higher mental fatigue (MFI-20: >17 out of 20) and more severe depressed mood (*EPDS: >12 out of 30) showed improvement in mental fatigue with home-based exercise. Furthermore, regression analyses concluded that the intervention was significantly effective in alleviating mental fatigue with women in later postpartum period (9.4 weeks postdelivery; β = 0.518) and with higher depression scores (*EPDS > 12; β = 0.374). In addition, social support was not a significant factor in the exercise group (β= −0.326). What is more, multiparous women (M= −3.75 (4.28)) and women delivering vaginally (M= −4.21 (4.35)) showed somewhat larger improvements in mental fatigue with exercise than primiparous participants (M= −1.89 (4.32)) and women delivering with a C-section (M= −1.03 (4.17)).
Mental fatigue within anxiety disorders
Psychometrics used to measure mental fatigue
For measuring mental fatigue in individuals with anxiety disorders, three articles reported using self-reported instruments of MFI-20 (Kaiya et al., Citation2008; Pasquini et al., Citation2015) and FES-11 (Li et al., Citation2020). Mental fatigue was prevalent in MFI-20 with a mean of 10.8–13.0 (SD= 3.6–16.0) and FES-11 measures with a mean of 7.02–7.67 (SD= 2.45–2.89). In addition, one article investigated mental fatigue within non-specific groups of psychiatric disorders and used FSC (Jiang et al., Citation2003). The prevalence within participants ranged up to 10 (M = 4.5, SD= 3.4).
Panic disorder and mental fatigue
Kaiya et al. (Citation2008) study researched fatigue characteristics of 360 individuals with PD. The findings implied that the characteristics of fatigue differed depending on gender. Scores of general fatigue, mental fatigue and reduced activity were significantly higher in 113 males with PD than in the 809 general population control group (F = 8.87, F = 4.66, F = 6.4, respectively). On the other hand, 247 females with PD showed no significant differences in their mental fatigue levels when compared with 195 controls, with the exception of physical fatigue (F = 4.07).
Generalised anxiety disorder and mental fatigue
Li et al. (Citation2020) evaluated mental fatigue in women with (n = 18) and without (n = 20) generalised anxiety disorder throughout the early-follicular (lower ovarian hormones) and mid-luteal (higher ovarian hormones) phases of a single menstrual cycle, while adjusting for sleep disruption. In addition, the link between mental fatigue and hormones was investigated. Mental fatigue increased significantly from the early follicular to the mid-luteal phase in non-anxious women (t = 2.23, p = 0.038, Cohen’s d = 0.50), whereas there was no difference in women with GAD (p > 0.05). Furthermore, non-anxious women’s mental fatigue increased to levels comparable to their GAD counterparts, indicating that in the early follicular phase, mental fatigue was significantly higher in the GAD group compared with the non-anxious group (t = 5.14, Cohen’s d = 1.67), but there was no difference in mental fatigue between the groups in the mid-luteal phase (p > 0.05). Physical fatigue, on the other hand, was consistent throughout both phases. Furthermore, the study discovered some contradictory findings on the relationship between oestrogen, progesterone and mental fatigue. In the early follicular and mid-luteal phases of the menstrual cycle, neither oestradiol nor progesterone were significant predictors of mental exhaustion (p > 0.05), according to hierarchical linear regressions. However, ANCOVA analyses revealed that only in the early follicular phase (t=4.14) oestrogen and progesterone were significant predictors of mental fatigue.
Anxiety and personality risk factors of mental fatigue
An article by Jiang et al. (Citation2003) investigated the relationship between anxiety and fatigue to discover personality risk factors for fatigue within 101 outpatients with psychiatric disorders. Study results showed that trait anxiety (F = 0.735) and state anxiety (F = 0.694) had strong positive correlations with mental fatigue. Furthermore, mental fatigue also exhibited a strong positive correlation with the personality risk factors of harm avoidance (F = 0.629), as well as strong negative correlation with self-directedness (F= −0.617) and a weak negative correlation with cooperativeness (F = 0.299) and persistence (F = 0.338).
Mental fatigue within obsessive-compulsive disorder and obsessive-compulsive personality disorder
Within the research, two articles investigated mental fatigue in individuals with OCD and OCDP (Gecaite-Stonciene et al., Citation2020; Pasquini et al., Citation2015). Self-reported MFI-20 instrument was used to measure mental fatigue. Respectively, the prevalence ranged with mean 10.0 (SD= 9.0–11.2) for individuals with OCD and with mean 15.9 (SD= 3.8) for individuals with OCPD.
Article by Pasquini et al. (Citation2015) presented research that compared 50 individuals with OCD and 50 with PD, to assess whether they perceived fatigue differently. Results indicated that mental fatigue (OR 0.138 [95% CI 0.049–0.326]) presence was associated with lower odds of OCD. Notably, individuals with OCD and OCPD co-morbidity reported higher scores of mental fatigue. Thus, suggesting that mental fatigue was more common within OCPD than OCD. Similar conclusions were made in Gecaite-Stonciene et al. (Citation2020) study further exploring a significant association between OCPD and mental fatigue (OR, 1.27; 95% CI, 1.02–1.58) within 85 individuals with comorbid anxiety and mood disorders, after adjusting for anxiety and depression symptoms, age, gender, education, medication use and smoking. However, other significant fatigue features, including as general fatigue, physical fatigue, reduced activity, and reduced motivation, as well as executive functioning, were not found to be associated with the existence of OCPD in the study.
Discussion
This scoping review found 10 studies on the relationship between mental fatigue and various psychiatric disorders. The main themes identified in the review were: 1) mental fatigue within mood disorders; 2) mental fatigue within anxiety disorders; 3) mental fatigue within obsessive-compulsive disorder and obsessive-compulsive personality disorder. After reviewing selected articles, several limitations were discovered and are further discussed together with recommendations for future studies.
Although there is no consensus on the terminology and definition of mental fatigue, our review highlighted the importance of establishing uniformed description of mental fatigue. With all of this in mind, another important question arises whether the terminology of mental fatigue appropriately reflects the current understanding of the investigated subclass of fatigue. The word ‘mental’ has a definition of ‘relating to the mind or the disorders of the mind’ (Oxford Advanced American Dictionary, Citation2022). However, it is often used as a derogatory term for people who suffer from psychiatric illnesses (Rose et al., Citation2007). Stigma towards psychiatric disorders and inexact terminology of this subclass of fatigue can create a stagnation in research and practical misunderstandings. As seen in reviewed literature, mental fatigue usually reflects on cognitive factors, therefore there may be a need to reconsider the term ‘mental fatigue’ and change it to more accurate term ‘cognitive fatigue’. However, more research is needed to solidify the more accurate term for the phenomenon that is mental fatigue.
Eight out of 10 studies in our review had a cross sectional design, outlining a lack of research using longitudinal studies. Dritsa et al. (Citation2009) identified some changes in mental fatigue state in studies that used randomised control trials over a short period of time (e.g., one-week test–retest), whereas Wessely and Powell (Citation1989) showed that length of illness was not connected with greater mental fatigue. Longitudinal studies could aid in the discovery of causal linkages rather than just correlations.
Furthermore, there were few studies that used biomarkers to report mental fatigue. Hormone measurements were only included in one research (Li et al., Citation2020). Studies in healthy people were more widespread, ranging from reaction times (van Cutsem et al., Citation2017), global brain activity (Yao et al., Citation2021) to nutrition (Tardy et al., Citation2020). Subclinical or marginal nutritional deficiencies have been shown to have negative effects on mental fatigue, as well as cognitive and psychological functions (Tardy et al., Citation2020). The link between nutrition and depression, in particular, has been found to have an impact on an individual’s psychological well-being (Rao et al., Citation2008). Because biomarker measures of mental fatigue in individuals with anxiety and mood disorders were limited, additional research into these measures is needed. Finally, due to the scarcity of replication studies in the field, comparisons are challenging.
Even though this research mostly concentrated on mental fatigue in anxiety and mood disorders, we noticed a lack of research on mental fatigue with other psychiatric disorders within adults. Only one study in our review included individuals with a variety of psychiatric disorders, including major depressive episode, anxiety disorders, OCD, schizophrenia and schizoaffective disorder, alcohol dependence, somatisation disorder, eating disorder, adjustment disorder and delusional disorder (Jiang et al., Citation2003). Mental fatigue has been studied in different psychiatric samples, such as anorexia nervosa in adolescents (Casper et al., Citation2020), internet addiction in students (Bachleda & Darhiri, Citation2018), and cocaine abuse (Moeller et al., Citation2012); however, research is limited by sample characteristics.
During the scoping review, it was discovered that there was a lack of knowledge on the topic of intervention approaches for mental fatigue in individuals with psychiatric disorders. Only one out of 10 articles investigated, and it focussed on the effectiveness of home-based exercise to reduce mental fatigue within women in the postpartum period. Although reviews have been published for mental fatigue treatments available for individuals with neurological disorders (Ulrichsen et al., Citation2016; Xu et al., Citation2017) and cancer (Corbett et al., Citation2019), there is still a need for a deeper understanding of tools that might be used in the psychiatric field.
Six out of 10 studies used mental fatigue inventory, whereas other four studies used different self-report questionnaires. Only two studies investigated the validity of MFI-20 and FQ-14 in individuals with major depression, emphasising the importance of validating mental fatigue psychometric tools. When a questionnaire has been developed and validated to measure mental fatigue in one clinical sample, the use of a particular tool in other clinical samples may not be supported. One of the main reasons for that would be different mechanisms involved in different clinical samples (Ghanean et al., Citation2018) that may trigger different aspects of the same construct. For example, Ferentinos et al. (Citation2010) reported that some items from the Fatigue Questionnaire did not load on the expected mental fatigue factor in the sample of individuals with MDD. Meanwhile, a study of fatigue in individuals undergoing haemodialysis confirmed the original factor structure in the same questionnaire (Picariello et al., Citation2016). Validation of questionnaires could aid in the identification of traits associated with mental fatigue in mood and anxiety disorders.
While conducting review analyses, it was discovered that the information provided on mental fatigue in individuals with psychiatric disorders was limited to the experiences of eight different countries/cultures. The lack of research raises a concern as the provided results would be difficult to apply in different regions and populations. In addition, as most of the studies in this review were conducted once per population, it is difficult to draw well-grounded conclusions due to the lack of research replication. Because observational indexes are random variables that require a certain number of samples to reveal their changing regularity, the repetition principle is important in scientific research. The repetition principle stabilises the mean and standard deviation, allowing sample statistics to accurately represent population parameters. As a result, the statistical inference will be trustworthy (Hu et al., Citation2011).
During the review, it was discovered that the majority of the research did not achieve gender balance. When utilising parametric approaches such as the t-test or ANOVA, homogeneity of variance is assumed because it produces superior findings when comparing. This suggests that each group’s score variability is similar (Pallant, Citation2010). Furthermore, because most studies featured more female participants, a more balanced sample provides more information about males, making it easier to compare outcomes based on gender.
Our study has some notable limitations. The scope of the review was restricted to a limited number of indexed English language, peer-reviewed studies that focussed on measuring mental fatigue in an adult population with psychiatric disorders. Although the search strategy reduced the risk of publication bias, some studies and salient work may have been overlooked. In addition, the research evaluated were limited to mood, anxiety, OCD and OCPD disorders. It is also worth noting that, though the selected articles vary in terms of content, sample size and methodology, they all addressed essential aspects of mental fatigue in individuals with mood, anxiety and OCD disorders. Reviewed research articles indicated different instruments used to measure mental fatigue as well as relationships between various aspects of mental fatigue with insomnia, postpartum depression, personality risk factors, PD, OCD and hormonal menstrual changes in women. However, a meta-analysis and a systematic literature review could not be carried out since there were insufficiently comparable outcomes across the investigations. In addition, after a rigorous systematic review process, there were a limited number of studies included in the review, and thus the conclusions of this review are very tentative.
In conclusion, the review of existing research on mental fatigue in adults with psychiatric disorders indicated relevance and frequency of mental fatigue among individuals with AMD, OCD and OCDP. The findings show that mental fatigue research in the field of psychiatry is confined to a few disorders and that more research is needed to prevent overlap between symptoms across mental fatigue and other psychiatric disorders which could lead to misattribution. Due to a scarcity of published data, it was difficult to make well-rounded conclusions on certain disorders. Furthermore, the findings implied that MFI-20 is a regularly used test for assessing mental fatigue. However, more research into the validity and reliability for illness specific instruments to measure mental fatigue in psychiatric population is required.
Disclosure statement
1) Julija Gecaite-Stonciene works as a consultant at FACITtrans. 2) Julius Burkauskas served as a consultant at Cogstate, Ltd. 3) Naomi A. Fineberg reports personal fees from Abbott, Taylor and Francis, Oxford University Press, Global Mental Health Academy and Elsevier; personal fees and non-financial support from Sun, WPA; non-financial support from RCPsych, CINP, Int Society of Behavioural Addiction, WHO, the International College of Obsessive-Compulsive Spectrum Disorders, the Int Forum of Mood and Anxiety Disorders, Wiley, and the Indian Association of Biological Psychiatry; grants from MRC, Wellcome, and NIHR; grants and non-financial support from EU COST Action, ECNP, and Shire; payment for consultancy from the UK MHRA, all outside of the submitted work. 4) Alessandro Serretti has served as a consultant or speaker for Abbott, Abbvie, Angelini, Astra Zeneca, Clinical Data, Boehringer, Bristol Myers Squibb, Eli Lilly, GlaxoSmithKline, Innovapharma, Italfarmaco, Janssen, Lundbeck, Naurex, Pfizer, Polipharma, Sanofi, Servier, Taliaz. The remaining authors declare no conflicts of interest.
Additional information
Funding
References
- Abd-Elfattah, H. M., Abdelazeim, F. H., & Elshennawy, S. (2015). Physical and cognitive consequences of fatigue: A review. Journal of Advanced Research, 6(3), 351–358. doi:10.1016/j.jare.2015.01.011
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. (5th ed.). Washington, D.C.: American Psychiatric Publishing, Inc. doi:10.1176/appi.books.9780890425596
- Arnett, P. A., Barwick, F. H., & Beeney, J. E. (2008). Depression in multiple sclerosis: Review and theoretical proposal. Journal of the International Neuropsychological Society : JINS, 14(5), 691–724. doi:10.1017/S1355617708081174
- Bachleda, C., & Darhiri, L. (2018). Internet addiction and mental and physical fatigue. The International Technology Management Review, 7(1), 25–33. doi:10.2991/itmr.7.1.3
- Bartoszek, A., Walkowiak, D., Bartoszek, A., & Kardas, G. (2020). Mental well-being (depression, loneliness, insomnia, daily life fatigue) during COVID-19 related home-confinement - A study from Poland. International Journal of Environmental Research and Public Health, 7(20), 7417. doi: 10.3390/ijerph17207417
- Berard, J. A., Smith, A. M., & Walker, L. A. S. (2019). Predictive models of cognitive fatigue in multiple sclerosis. Archives of Clinical Neuropsychology, 34(1), 31–38. doi:10.1093/arclin/acy014
- Billones, R. R., Kumar, S., & Saligan, L. N. (2020). Disentangling fatigue from anhedonia: a scoping review. Translational Psychiatry, 10(1), 273. doi:10.1038/s41398-020-00960-w
- Boksem, M. A. S., Meijman, T. F., & Lorist, M. M. (2005). Effects of mental fatigue on attention: and ERP study. Brain Research. Cognitive Brain Research, 25(1), 107–116. doi:10.1016/j.cogbrainres.2005.04.011
- Boksem, M. A. S., & Tops, M. (2008). Mental fatigue: Costs and benefits. Brain Research Reviews, 59(1), 125–139. doi:10.1016/j.brainresrev.2008.07.001
- Carney, C. E., Moss, T. G., Lachowski, A. M., & Atwood, M. E. (2014). Understanding mental and physical fatigue complaints in those with depression and insomnia. Behavioral Sleep Medicine, 12(4), 272–289. doi:10.1080/15402002.2013.801345
- Casper, R.C., Voderholzer, U., Naab, S., & Schlegl, S. (2020). Increased urge for movement, physical and mental restlessness, fundamental symptoms of restricting anorexia nervosa? Brain and Behavior, 10(3), e01556. (doi:10.1002/brb3.1556
- Chung, K.-F., Yu, B. Y.-M., Yung, K.-P., Yeung, W.-F., Ng, T. H., & Ho, F. Y.-Y. (2014). Assessment of fatigue using the multidimensional fatigue inventory in patients with major depressive disorder. Comprehensive Psychiatry, 55(7), 1671–1678. doi:10.1016/j.comppsych.2014.06.006
- Corbett, T. K., Groarke, A., Devane, D., Carr, E., Walsh, J. C., & McGuire, B. E. (2019). The effectiveness of psychological interventions for fatigue in cancer survivors: systematic review of randomised controlled trials. Systematic Reviews, 8(1), 324–354. doi:10.1186/s13643-019-1230-2
- de Raaf, P. J., de Klerk, C., & van der Rijt, C. C. D. (2013). Elucidating the behavior of physical fatigue and mental fatigue in cancer patients: a review of the literature. Psycho-oncology, 22(9), 1919–1929. doi:10.1002/pon.3225
- Demyttenaere, K., De Fruyt, J., & Stahl, S. M. (2005). The many faces of fatigue in major depressive disorder. The International Journal of Neuropsychopharmacology, 8(1), 93–105. doi:10.1017/S1461145704004729
- Dritsa, M., Dupuis, G., Lowensteyn, I., & Da Costa, D. (2009). Effects of home-based exercise on fatigue in postpartum depressed women: Who is more likely to benefit and why? Journal of Psychosomatic Research, 67(2), 159–163. doi:10.1016/j.jpsychores.2009.01.010
- Fava, M., Ball, S., Nelson, J. C., Sparks, J., Konechnik, T., Classi, P., Dube, S., & Thase, M. E. (2014). Clinical relevance of fatigue as a residual symptom in major depressive disorder. Depression and Anxiety, 31(3), 250–257. doi:10.1002/da.22199
- Ferentinos, P., Kontaxakis, V., Havaki-Kontaxaki, B., Dikeos, D., & Papadimitriou, G. (2010). The Fatigue Questionnaire: Standardization in patients with major depression. Psychiatry Research, 177(1-2), 114–119. doi:10.1016/j.psychres.2009.01.029
- Gecaite-Stonciene, J., Fineberg, N. A., Podlipskyte, A., Neverauskas, J., Juskiene, A., Mickuviene, N., & Burkauskas, J. (2020). Mental fatigue, but not other fatigue characteristics, as a candidate feature of obsessive compulsive personality disorder in patients with anxiety and mood disorders: An exploratory study. International Journal of Environmental Research and Public Health, 17(21), 8132. doi:10.3390/ijerph17218132
- Ghanean, H., Ceniti, A.K., & Kennedy, S.H. (2018). Fatigue in patients with major depressive disorder: Prevalence, burden and pharmacological approaches to management. CNS Drugs, 32(1), 65–74. doi:10.1007/s40263-018-0490-z
- Guo, Z., Chen, R., Zhang, K., Pan, Y., & Wu, J. (2016). The impairing effect of mental fatigue on visual sustained attention under monotonous multi-object visual attention task in long durations: An event-related potential based study. PLoS One, 11(9), e0163360. doi:10.1371/journal.pone.0163360
- Herlambang, M. B., Taatgen, N. A., & Cnossen, F. (2019). The role of motivation as a factor in mental fatigue. Human Factors, 31(7), 1171–1185. doi:10.1177/0018720819828569
- Hu, L-P., Bao, X-L., & Wang, Q. (2011). The repetition principle in scientific research. Zhong xi yi Jie he Xue Bao = Journal of Chinese Integrative Medicine, 9(9), 937–940. doi:10.3736/jcim20110903
- Jiang, N., Sato, T., Hara, T., Takedomi, Y., Ozaki, I., & Yamada, S. (2003). Correlations between trait anxiety, personality and fatigue. Journal of Psychosomatic Research, 55(6), 493–500. doi:10.1016/S0022-3999(03)00021-7
- Joanna Briggs Institute. (2020a). Checklist For Analytical Cross Sectional Studies. from shorturl.at/jBV03
- Joanna Briggs Institute. (2020b). Checklist For Randomized Controlled Trials. from shorturl.at/jBV03
- Johansson, B. (2021). Mental fatigue after mild traumatic brain injury in relation to cognitive tests and brain imaging methods. International Journal of Environmental Research and Public Health, 18(11), 5955. doi:10.3390/ijerph18115955
- Kaiya, H., Sugaya, N., Iwasa, R., & Tochigi, M. (2008). Characteristics of fatigue in panic disorder patients. Psychiatry and Clinical Neurosciences, 62(2), 234–237. doi:10.1111/j.1440-1819.2008.01760.x
- Li, S. H., Lloyd, A. R., & Graham, B. M. (2020). Physical and mental fatigue across the menstrual cycle in women with and without generalised anxiety disorder. Hormones and Behavior, 118, 104667. doi:10.1016/j.yhbeh.2019.104667
- Lindstedt, M., Johansson, J., Ygge, J., & Borg, K. (2019). Vision-related symptoms after acquired brain injury and the association with mental fatigue, anxiety and depression. Journal of Rehabilitation Medicine, 51(7), 499–505. doi:10.2340/16501977-2570
- Lorist, M. M. (2008). Impact of top-down control during mental fatigue. Brain Research, 1232, 113–123. doi:10.1016/j.brainres.2008.07.053
- Lorist, M. M., Klein, M., Nieuwenhuis, S., de Jong, R., Mulder, G., & Meijman, T. F. (2000). Mental fatigue and task control: Planning and preparation. Psychophysiology, 37(5), 614–625.
- Mikula, P., Timkova, V., Linkova, M., Vitkova, M., Szilasiova, J., & Nagyova, I. (2020). Fatigue and suicidal ideation in people with multiple sclerosis: The role of social support. Frontiers in Psychology, 11, 504. doi:10.3389/fpsyg.2020.00504
- Moeller, S. J., Tomasi, D., Honorio, J., Volkow, N. D., & Goldstein, R. Z. (2012). Dopaminergic involvement during mental fatigue in health and cocaine addiction. Translational Psychiatry, 2(10), e176. doi:10.1038/tp.2012.110
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G, PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical Research ed.), 339, b2535. doi:10.1136/bmj.b2535
- Morgul, E., Bener, A., Atak, M., Akyel, S., Aktaş, S., Bhugra, D., Ventriglio, A., & Jordan, T. R. (2021). COVID-19 pandemic and psychological fatigue in Turkey. International Journal of Social Psychiatry, 67(2), 128–135. doi:10.1177/0020764020941889
- Morris, A. J., & Christie, A. D. (2020). The effect of mental fatigue on neuromuscular function is similar in young and older women. Brain Sciences, 10(4), 191. doi:10.3390/brainsci10040191
- Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic review or scoping review approach. BMC Medical Research Methodology, 18(1), 143. doi:10.1186/s12874-018-0611-x
- Nagy, A., Szabados, E., Simon, A., Mezey, B., Sandor, B., Tiringer, I., Toth, K., Bencsik, K., & Csatho, A. (2018). Association of exercise capacity with physical functionality and various aspects of fatigue in patients with coronary artery disease. Behavioral Medicine (Washington, D.C.), 44(1), 28–35. doi:10.1080/08964289.2016.1189395
- Oxford Advanced American Dictionary (2022). Deffinition of mental adjective, https://www.oxfordlearnersdictionaries.com/definition/american_english/mental (assessed 2022-08-04).
- Pallant, J. (2010). SPSS survival manual: a step by step guide to data analysis using SPSS. Open University Press/McGraw-Hill.
- Palm, S., Ronnback, L., & Johansson, B. (2017). Long-term mental fatigue after traumatic brain injury and impact on employment status. Journal of Rehabilitation Medicine, 49(3), 228–233. doi:10.2340/16501977-2190
- Pasquini, M., Piacentino, D., Berardelli, I., Roselli, V., Maraone, A., Tarsitani, L., & Biondi, M. (2015). Fatigue experiences among OCD outpatients. The Psychiatric Quarterly, 86(4), 615–624. doi:10.1007/s11126-015-9357-3
- Picariello, F., Moss-Morris, R., Macdougall, I. C., & Chilcot, J. (2016). Measuring fatigue in haemodialysis patients: The factor structure of the Chalder Fatigue Questionnaire (CFQ). Journal of Psychosomatic Research, 84, 81–83. doi:10.1016/j.jpsychores.2016.03.124
- Polikandrioti, M., Tzirogiannis, K., Zyga, S., Koutelekos, I., Vasilopoulos, G., Theofilou, P., & Panoutsopoulos, G. (2018). Effect of anxiety and depression on the fatigue of patients with a permanent pacemaker. Archives of Medical Science – Atherosclerotic Diseases, 3(1), e8–e17. doi:10.5114/amsad.2018.73231
- Qi, P., Ru, H., Gao, L., Zhang, X., Zhou, T., Tian, Y., Thakor, N., Bezerianos, A., Li, J., & Sun, Y. (2019). Neural mechanisms of mental fatigue revisited: New insights from the brain connectome. Engineering, 5(2), 276–286. doi:10.1016/j.eng.2018.11.025
- Rao, T. S., Asha, M. R., Ramesh, B. N., & Rao, K. S. (2008). Understanding nutrition, depression and mental illnesses. Indian Journal of Psychiatry, 50(2), 77–82. doi:10.4103/0019-5545.42391
- Rose, D., Thornicroft, G., Pinfold, V., & Kassam, A. (2007). 250 labels used to stigmatise people with mental illness. BMC Health Services Research, 7 (1), 97–103. doi:10.1186/1472-6963-7-97
- Sharma, A. K., Agrawal, A., Agrawal, U., & Dubey, G. P. (1990). Influence of mentat on memory and mental fatigue in cases of anxiety neurosis and depression. Indian Journal of Cancer & Bioresearch, 3(1), 27–30.
- Smets, E. M., Garssen, B., Bonke, B., & de Haes, J. C. (1995). The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. Journal of Psychosomatic Research, 39(3), 315–325. doi:10.1016/0022-3999(94)00125-O
- Takeda, A., Minatani, S., Ishii, A., Matsuo, T., Tanaka, M., Yoshikawa, T., & Itoh, Y. (2021). Impact of depression on mental fatigue and attention in patients with multiple sclerosis. Journal of Affective Disorders Reports, 5, 100143. doi:10.1016/j.jadr.2021.100143
- Tardy, A. L., Pouteau, E., Marquez, D., Yilmaz, C., & Scholey, A. (2020). Vitamins and minerals for energy, fatigue and cognition: A narrative review of the biochemical and clinical evidence. Nutrients, 12(1), 228. doi:10.3390/nu12010228
- Targum, S. D., & Fava, M. (2011). Fatigue as residual symptom of depression. Innovations in Clinical Neuroscience, 8(10), 40–43.
- Teng, Z., Wei, Z., Qiu, Y., Tan, Y., Chen, J., Tang, H., Wu, H., Wu, R., & Huang, J. (2020). Psychological status and faitgue of frontline staff two months after the COVID-19 pandemic outbreak in China: A cross-sectional study. Journal of Affective Disorders, 275, 247–252. doi:10.1016/j.jad.2020.06.032
- Torrente, F., Yoris, A., Low, D., Lopez, P., Bekinschtein, P., Vázquez, G., & Cetkovich, M. (2021). Emotional symptoms, mental fatigue and behavioral adherence after 72 continuous days of strict lockdown during the COVID-19 pandemic in Argentina. medRxiv, 8(1), 1–9. doi:10.1101/2021.04.21.21255866
- Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E., et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. doi:10.7326/M18-0850
- Trojan, D. A., Arnold, D., Collet, J.-P., Shapiro, S., Bar-Or, A., Robinson, A., Le Cruguel, J.-P., Ducruet, T., Narayanan, S., Arcelin, K., Wong, A. N., Tartaglia, M. C., Lapierre, Y., Caramanos, Z., & Da Costa, D. (2007). Fatigue in multiple sclerosis: association with disease related, behavioral and psychosocial factors. Multiple Sclerosis Journal, 13(8), 985–995. doi:10.1177/1352458507077175
- Ulrichsen, K. M., Kaufmann, T., Dørum, E. S., Kolskår, K. K., Richard, G., Alnaes, D., Arneberg, T. J., Westlye, L. T., & Nordvik, J. E. (2016). Clinical utility of mindfulness training in the treatment of fatigue after stroke, traumatic brain injury and multiple sclerosis: A systematic literature review and meta-analysis. Frontiers in Psychology, 7, 912. doi:10.3389/fpsyg.2016.00912
- van Cutsem, J., Marcora, S., De Pauw, K., Bailey, S., Meeusen, R., & Roelands, B. (2017). The effects of mental fatigue on physical performance: A systematic review. Sports Medicine, 47(8), 1569–1588. doi:10.1007/s40279-016-0672-0
- van der Linden, D. (2011). The urge to stop: The cognitive and biological nature of acute mental fatigue [Paper presentation]. Paper Presented at the Decade of Behavior/Science Conference. Cognitive Fatigue: Multidisciplinary Perspectives on Current Research and Future Applications,.
- van der Linden, S. D., Gehring, K., Rutten, G. J. M., Kop, W. J., & Sitskoorn, M. M. (2020). Prevalence and correlates of fatigue in patients with meningioma before and after surgery. Neuro Oncology Practice, 7(1), 77–85. doi:10.1093/nop/npz023
- Wessely, S., & Powell, R. (1989). Fatigue syndromes: a comparison of chronic “postviral” fatigue with neuromuscular and affective disorders. Journal of Neurology, Neurosurgery, and Psychiatry, 52(8), 940–948. doi:10.1136/jnnp.52.8.940
- Xu, G. Z., Li, Y. F., Wang, M. D., & Cao, D. Y. (2017). Complementary and alternative interventions for fatigue management after traumatic brain injury: a systematic review. Therapeutic Advances in Neurological Disorders, 10(5), 229–239. doi:10.1177/1756285616682675
- Yao, L., Baker, J. L., Schiff, N. D., Purpura, K., & Shoaran, M. (2021). Predicting task performance from biomarkers of mental fatigue in global brain activity. Journal of Neural Engineering, 18(3), 036001. doi:10.1088/1741-2552/abc529
- Zhan, Y-x., Zhao, S-y., Yuan, J., Liu, H., Liu, Y-f., Gui, L-l., Zheng, H., Zhou, Y-m., Qiu, L-h., Chen, J-h., Yu, J-h., & Li, S-y. (2020). Prevalence and Influencing Factors on Fatigue of First-line Nurses Combating with COVID-19 in China: A descriptive cross-sectional study. Current Medical Science, 40(4), 625–635. doi:10.1007/s11596-020-2226-9
