Abstract
Mental health has worsened, and substance use has increased for some people during the coronavirus (COVID-19) pandemic. Some cross-sectional studies suggest that higher COVID-19 risk perceptions are related to poorer mental health and greater risk behaviours (e.g. substance use). However, longitudinal and genetic data are needed to help to reduce the likelihood of reverse causality. We used cross-sectional, longitudinal, and polygenic risk score (PRS; for anxiety, depression, wellbeing) data from the Avon Longitudinal Study of Parents and Children (ALSPAC). We examined cross-sectional and prospective longitudinal associations between COVID-19 risk perceptions (i.e. cognitive, affective, self, other, and a combined ‘holistic’ measure) and mental health (i.e. anxiety, depression), wellbeing, and risk behaviours. Pandemic (April–July 2020) and pre-pandemic (2003–2017) data (ns = 233–5,115) were included. Higher COVID-19 risk perceptions (holistic) were associated with anxiety (OR 2.78, 95% confidence interval [CI] 2.20 to 3.52), depression (OR 1.65, 95% CI 1.24 to 2.18), low wellbeing (OR 1.76, 95% CI 1.45 to 2.13), and increased alcohol use (OR 1.46, 95% CI 1.24 to 1.72). Higher COVID-19 risk perceptions were also associated with self-isolating given a suspected COVID-19 infection (OR 1.74, 95% CI 1.13 to 2.68), and less face-to-face contact (OR 0.83, 95% CI 0.70 to 0.98) and physical contact (OR 0.83, 95% CI 0.68 to 1.00). Pre-pandemic anxiety (OR 1.64, 95% CI 1.29 to 2.09) and low wellbeing (OR 1.41, 95% CI 1.15 to 1.74) were associated with higher COVID-19 risk perceptions. The depression PRS (b 0.21, 95% CI 0.02 to 0.40) and wellbeing PRS (b − 0.29, 95% CI −0.48 to −0.09) were associated with higher and lower COVID-19 risk perceptions, respectively. Poorer mental health and wellbeing are associated with higher COVID-19 risk perceptions, and longitudinal and genetic data suggest that they may play a causal role in COVID-19 risk perceptions.
Introduction
The coronavirus (COVID-19) pandemic was declared in March 2020 (World Health Organisation Citation2021a). As of November 2021, there have been over 250 million confirmed cases, including over 5 million deaths globally (World Health Organisation Citation2021b). The pandemic and mitigation measures have impacted mental health (Byrne, Barber, and Lim Citation2021); 60% of UK adults report that their mental health has deteriorated, and 36% report using alcohol or illegal drugs to cope (Mind Citation2020). Wellbeing has reduced, anxiety has almost doubled (from 13% to 24%) (Kwong et al. Citation2021), and approximately 25% of people report drinking alcohol and smoking more (Garnett et al. Citation2021; Tzu-Hsuan Chen Citation2020). Risk perceptions are subjective judgements about the characteristics, severity, and probability of a risk (Darker Citation2013). They can influence emotions and behaviours (Ferrer and Klein Citation2015; Paek and Hove Citation2017), and impact how governments and individuals respond to the pandemic (McCloskey and Heymann Citation2020). COVID-19 risk perceptions refer to the perceived likelihood of SARS-CoV-2 infection (cognitive COVID-19 risk perceptions) and worries about SARS-CoV-2 infection (affective COVID-19 risk perceptions) with holistic COVID-19 risk perceptions referring to these measures combined (Dryhurst et al. Citation2020; Schneider et al. Citation2021). COVID-19 risk perceptions may have contributed to the changes in mental health (e.g. anxiety, depression), wellbeing, and risk behaviours (e.g. alcohol use, smoking) observed during the pandemic.
In the opposite temporal direction, mental health, wellbeing, and risk behaviours could also influence COVID-19 risk perceptions. According to valence approaches, negative emotions lead to higher risk perceptions (Lerner and Keltner Citation2000). Therefore, pre-pandemic anxiety, depression, and low wellbeing may lead to increased risk perceptions about a new global pandemic. Furthermore, according to self-perception theory, behaviours affect thoughts and attitudes (Bem Citation1972). People may adjust their perception of risk to align with their behaviour if they cannot (or choose not to) adjust their behaviour, in order to reduce cognitive dissonance (Festinger Citation1957). For example, going to work rather than self-isolating following a COVID-19 diagnosis (e.g. for financial reasons) may lead to reduced risk perceptions. Understanding COVID-19 risk perceptions and their possible bidirectional associations with mental health, wellbeing, and risk behaviours is therefore crucial for informing pandemic preparedness and response efforts. This research has implications for risk communication and public health messaging during the current and future pandemics.
Mental health and wellbeing
Mental health conditions, such as anxiety and depression, are disorders characterised by a combination of abnormal thoughts, emotions, and behaviours (World Health Organisation Citation2019). Cross-sectional studies have found associations between higher COVID-19 risk perceptions and poorer mental health. For example, Zhong et al. (Citation2021) and Liu, Zhang, and Huang (Citation2020) found that COVID-19 risk perceptions (likelihood of infection) were associated with higher depressive states and anxiety levels, respectively. Similarly, COVID-19 risk perceptions (likelihood of infection or economic consequences from COVID-19, and COVID-19 threat) have been associated with feeling anxious, nervous, depressed, and stressed (Han et al. Citation2021; Li and Lyu Citation2020). However, the temporal direction of the relationship is unclear in these studies. Poorer mental health may precede risk perceptions (rather than vice versa). The authors of another cross-sectional study argued for this direction, reporting that anxiety and depression influence higher COVID-19 risk perceptions (Orte et al. Citation2020). However, longitudinal studies are required to better understand possible causal pathways.
Wellbeing is defined as the positive aspect of mental health; it is more than the absence of mental illness (Warwick Medical School Citation2020). To the best of our knowledge, previous studies have not examined associations between COVID-19 risk perceptions and wellbeing, specifically. Given its distinction from anxiety and depression, and the UK government’s recognition of wellbeing being critical to health policy (Department of Health and Social Care Citation2014), we think that there are insights to be gained by examining these constructs separately.
Risk behaviours
Smoking
Cross-sectional studies have found associations between COVID-19 risk perceptions and smoking behaviours, although the direction of the relationship is unclear. For example, Jackson et al. (Citation2021) found that higher COVID-19 risk perceptions (stress about becoming seriously ill from COVID-19) were associated with smoking less than usual among smokers with post-16 qualifications. Higher COVID-19 risk perceptions (worries about catching COVID) were also associated with smoking more than usual, and these associations were stronger for smokers without post-16 qualifications than those with. Shepherd et al. (Citation2021) found that COVID-19 worries (about contracting COVID-19, related symptoms, and associated health consequences) were positively associated with coping motives for smoking and perceived barriers for smoking cessation. Smokers also report lower adherence to COVID-19 prevention guidelines than never smokers, despite greater worries about infection (Jackson et al. Citation2021).
Electronic cigarette use
Electronic cigarettes (e-cigarettes), which can aid smoking cessation, are often used in conjunction with cigarettes (dual use) or as a replacement for cigarettes and are rarely used by people who have not smoked before (Hartmann-Boyce et al. Citation2021; Action on Smoking and Health Citation2020). Smoking and e-cigarette use should be considered separately because they may have different associations with COVID-19 risk perceptions. There is some research examining the associations between COVID-19 risk perceptions and e-cigarette use. For example, higher COVID-19 risk perceptions (beliefs that e-cigarette users are at greater risk from COVID-19 versus non-users) are associated with more frequent e-cigarette cessation considerations (Kelly, Pawson, and Vuolo Citation2021) and reductions in e-cigarette use (White et al. Citation2021). Furthermore, more frequent e-cigarette use was also associated with reduced beliefs that e-cigarette users are at greater risk from COVID-19 (Kelly, Pawson, and Vuolo Citation2021).
Alcohol use
Cross-sectional studies suggest that there is a relationship between COVID-19 risk perceptions and alcohol use, and this relationship may depend on how COVID-19 risk perceptions are operationalised. For example, Panno et al. (Citation2020) found an association between COVID-19 distress (an affective measure) and alcohol problems. Alpers et al. (Citation2021) found that COVID-19 economic (not health) worries were associated with increased drinking. Furthermore, Garnett et al. (Citation2021) found stress about catching COVID-19, becoming seriously ill, and financial stress were associated with drinking more than usual. However, the former was also associated with drinking less. Therefore, higher COVID-19 risk perceptions may motivate some people to reduce the amount they drink, smoke, or use e-cigarettes due to health concerns, and motivate others to drink, smoke, or use e-cigarettes more as a coping strategy (Yingst et al. Citation2021).
COVID-19 transmission-related behaviours
Risk perceptions are central to protection motivation theory, which explains how protective behaviours are initiated and maintained (Rogers Citation1975; Floyd, Prentice-Dunn, and Rogers Citation2000). Higher COVID-19 risk perceptions (e.g. likelihood of infection) are associated with protective behaviours that reduce virus transmission, such as hand washing, social distancing, and wearing face coverings (Wise et al. Citation2020; Bruine de Bruin and Bennett Citation2020; Savadori and Lauriola Citation2020; Schneider et al. Citation2021; Dryhurst et al. Citation2020). Conversely, lower COVID-19 risk perceptions (perceived severity) are associated with riskier social behaviour during the pandemic (i.e. greater number of social contacts) (Wambua et al. Citation2022). It is therefore important to examine the associations between COVID-19 risk perceptions and social contact and self-isolating when infected, as these behaviours impact virus transmission (Atchison et al. Citation2021).
Current study
Previous research on this topic has predominantly been cross-sectional. Although some researchers have investigated longitudinal predictors of COVID-19 risk perceptions (Schneider et al. Citation2021), to the best of our knowledge no studies have examined the role of mental health (i.e. anxiety and depression), wellbeing, and substance use as predictors of COVID-19 risk perceptions. We were particularly interested in the question of whether poorer mental health and wellbeing may be causal risk factors for COVID-19 risk perceptions. Whilst observational data offer a relatively weak basis for causal inference, longitudinal (versus cross-sectional) data support somewhat stronger causal inference by providing clarity on the temporal relationship between exposures and outcomes (i.e. which comes first). In addition, polygenic risk scores (PRS) for anxiety, depression, and wellbeing (single scores that capture genetic liability to a trait or condition by combining multiple genetic variants) (Choi, Mak, and O’Reilly Citation2020) can also support stronger causal inference by reducing the potential for confounding variables. Because PRS are determined at conception and are stable over time, their association with an outcome should not be affected by confounders over the life course. By triangulating results from cross-sectional, longitudinal, and genetic studies, which have different limitations and sources of potential bias, we can build on insights from previous research (Lawlor, Tilling, and Davey Smith Citation2016). Consistency of findings from different approaches improves the reliability of the evidence (Lawlor, Tilling, and Davey Smith Citation2016; Hill Citation2015). Furthermore, stronger inferences regarding whether these associations reflect causal pathways would support risk communication.
We examined the bidirectional associations between COVID-19 risk perceptions and mental health, wellbeing, and risk behaviours using combined data from mothers and young people in the Avon Longitudinal Study of Parents and Children (ALSPAC), making our study one of the largest and most comprehensive studies on this topic. We included five risk perception variables, including those that were thought-related (‘cognitive’ e.g. likelihood of infection), feeling-related (‘affective’ e.g. worries about infection), self-related, other-related, and a holistic measure combining all items. These distinctions have not always been studied, but they matter as there are implications for pandemic risk communication. For example, if cognitive risk perceptions were most strongly related to negative outcomes, then public health messaging could focus on communicating more personalised risk information. If affective risk perceptions were most strongly related to negative outcomes, such risk communications could focus on reducing affective biases by providing appropriate context for the risk numbers being communicated, for example by making use of risk comparator information. This would help people to make meaning of the level of risk they are exposed to (Freeman et al. Citation2021).
First, we investigated cross-sectional associations between COVID-19 risk perceptions (exposures) and mental health (i.e. anxiety and depression), wellbeing, and risk behaviours (i.e. alcohol use, smoking, e-cigarette use, lack of self-isolating given a suspected COVID-19 infection, and face-to-face and physical contact outside the household) (outcomes). Cross-sectional data were used to answer this first question because longitudinal data were not available (i.e. risk perceptions were assessed in the most recent COVID-19 questionnaire, at the same time point as the outcomes).
Second, we investigated prospective longitudinal associations between pre-pandemic mental health (i.e. anxiety and depression), wellbeing, and risk behaviours (alcohol use, smoking, e-cigarette use) and early pandemic risk behaviours (lack of self-isolating, social contact) (exposures) and COVID-19 risk perceptions (outcomes). Third, we investigated whether genetic propensities for anxiety, depression, and wellbeing (exposures) are associated with COVID-19 risk perceptions (outcomes). As described above, we used longitudinal and genetic data here to expand on previous studies that have examined similar research questions with cross-sectional data, to triangulate findings.
We hypothesised that (1) COVID-19 risk perceptions would be positively associated with anxiety, depression, low wellbeing, alcohol use, and self-isolating, and negatively associated with social contact, (2) pre-pandemic anxiety, depression, low wellbeing and early pandemic self-isolating would be positively associated with COVID-19 risk perceptions, and pre-pandemic alcohol use and early pandemic social contact would be negatively associated with COVID-19 risk perceptions, and (3) anxiety and depression PRS and wellbeing PRS would be positively and negatively associated with COVID-19 risk perceptions, respectively. We had no directional hypotheses for smoking and e-cigarette use, given the mixed findings.
Methods
Design
We conducted cross-sectional and prospective longitudinal analyses of secondary data from ALSPAC, a UK population-based birth cohort study (Boyd et al. Citation2013; Fraser et al. Citation2013; Northstone et al. Citation2019). The sample was broadly representative of the region at the time (Boyd et al. Citation2013). Ethics approval was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees (http://www.bristol.ac.uk/alspac/researchers/research-ethics/). Informed consent for the use of data collected via questionnaires and clinics was obtained following recommendations of the ALSPAC Ethics and Law Committee. Consent for biological samples was collected in accordance with the Human Tissue Act (2004). Our study protocol was pre-registered on the Open Science Framework (https://osf.io/qan65/).
Participants
ALSPAC recruited pregnant women living in Avon with expected delivery dates between April 1991–December 1992, and 14,541 pregnancies were initially enrolled. We used data from mothers (G0) and the original children (G1; ‘young people’) to maximise sample size. We could not include G0 partner data (mothers’ partners who were predominantly males), as identities cannot be linked across questionnaires. For example, a partner completing a prepandemic questionnaire may not be the same partner completing a pandemic questionnaire. Data from G1 participants at ≥22 years were collected and managed using REDCap (Harris et al. Citation2009). The ALSPAC study website contains the data dictionary and variable search tool (http://www.bristol.ac.uk/alspac/researchers/our-data).
Polygenic risk scores
Summary statistics from genome-wide association studies (GWAS) for anxiety (Purves et al. Citation2020), depression (Howard et al. Citation2019), and wellbeing (Baselmans et al. Citation2019) were used to derive corresponding PRS among participants with genetic data. We calculated PRS using a threshold of p < .05 to increase the percentage of variance explained in each phenotype while trying to minimise pleiotropy. This increased our statistical power to detect an effect, given our sample size (relatively small for exploring genetic associations), but potentially at the expense of specificity. Genotype data were available for 8,196 mothers and 8,237 young people. Full details are available in the Supplementary Information.
Self-report measures
The data dictionary describes all self-report measures (Supplementary Table S1). Variables were binary, except for the continuous COVID-19 risk perception variables that were used to test hypothesis 3. Time points of pre-pandemic measures (2003–2017) were selected based on the most recent and valid measures available (i.e. standardised scales preferred over single items). Therefore, follow-up periods varied from 3 to 17 (median 5) years (Supplementary Figure S1). Other studies using ALSPAC have used pre-pandemic measures from similar time points (Kwong et al. Citation2021). Separate variables were created for mothers, young people, and the whole sample combined, where possible.
Figure 1. Cross-sectional associations between COVID-19 holistic risk perceptions and mental health, wellbeing, and risk behaviours.
Note. Whole sample. Forest plot shows the fully adjusted odds ratios (circles) and 95% confidence intervals (bars). Fully adjusted = adjusted for age, gender, education, keyworker status, pre-pandemic anxiety, depression, high-risk drinking, smoking, and early pandemic suspected COVID-19 infection.
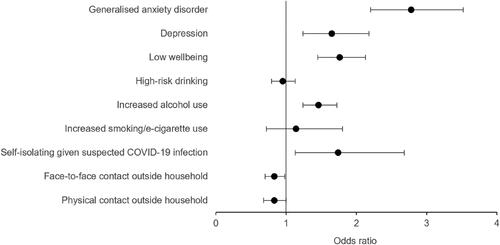
Table 1. Cross-sectional associations between COVID-19 risk perceptions and mental health, wellbeing, and risk behaviours (whole sample).
Risk perceptions
COVID-19 risk perceptions (five variables) were assessed in ALSPAC’s second COVID-19 questionnaire (26 May 2020 to 5 July 2020) (Northstone, Smith, et al. Citation2020). COVID-19 cognitive risk perceptions (i.e. thought-related risk perceptions) were measured by three summed items that assessed perceptions of COVID-19 impact, likelihood of infection, and severity of infection from 1 ‘strongly disagree’ to 5 ‘strongly agree’. COVID-19 affective risk perceptions (i.e. feeling-related risk perceptions) were measured by five summed items that assessed worries about COVID-19 infection (with respect to themselves [self] or other people [others]), transmission, and death (self/others) from 1 ‘not at all worried’ to 5 ‘very worried’. A holistic measure of COVID-19 risk perceptions was calculated by summing all eight items (mothers: Cronbach’s α = .82; young people: Cronbach’s α = .80). COVID-19 self- and other-risk perceptions combined items concerning oneself versus others, respectively. Binary variables were created by dichotomising continuous variables at the median. These binary variables were exposure variables for hypothesis 1, and outcome variables for hypothesis 2. The continuous variables were outcome variables for hypothesis 3.
Mental health and wellbeing
Outcomes: Current anxiety (generalised anxiety disorder; GAD) and depression (mental health variables), and wellbeing were assessed in the second COVID-19 questionnaire, using the Generalised Anxiety Disorder Assessment (GAD-7) (Spitzer et al. Citation2006), Short Mood and Feelings Questionnaire (SMFQ) (Angold et al. Citation1995), and Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) (Tennant et al. Citation2007), respectively. These measures have recommended binary cut-offs for examining the proportion of individuals with probable GAD (≥10) (Kroenke et al. Citation2007), likely depression (≥12) (Child Outcomes Research Consortium Citation2021; Jarbin et al. Citation2020), and low wellbeing (≤40) (Warwick Medical School Citation2021).
Exposures: Pre-pandemic anxiety, depression, and low wellbeing were assessed at different time points before the COVID-19 pandemic (2003–2017). For mothers, single items separately assessed pre-pandemic anxiety, depression, and low wellbeing (no/yes). For young people, pre-pandemic GAD and depression (mild episode) (no/yes) were derived from the Clinical Interview Schedule – Revised (CIS-R), and low wellbeing (no/yes) was derived from the WEMWBS.
Risk behaviours
Outcomes: High-risk drinking (no/yes), increased alcohol use since lockdown (no/yes), increased smoking/e-cigarette use (no/yes), self-isolating given a suspected or confirmed COVID-19 infection (no/yes), and face-to-face and physical contact with individuals outside one’s household (none/at least one person) were assessed in the second COVID-19 questionnaire. The Alcohol Use Disorders Identification Test – Consumption (AUDIT-C) has a recommended cut-off for high-risk drinking (≥5) (Kelly et al. Citation2009).
Exposures: Pre-pandemic high-risk drinking, smoking (no/yes), and e-cigarette use (no/yes; young people only), were assessed at different time points (2012–2017). Early pandemic transmission-related behaviours (self-isolating, social contact) were assessed in the first COVID-19 questionnaire (9 April 2020 to 15 May 2020) (Northstone, Howarth, et al. Citation2020).
Covariates
Age, sex, education, and keyworker status (partially adjusted models), and additionally, pre-pandemic anxiety, depression, high-risk drinking, smoking, and early pandemic suspected COVID-19 infection (fully adjusted models), were included as covariates. Covariates were selected based on their a priori relevance and/or their associations with risk perceptions, mental health, and/or risk behaviours in the literature (i.e. their potential to be a confounder). By using a categorical age variable (Supplementary Table S2), the age adjustment accounted for the bimodal age distribution.
Table 2. Longitudinal associations between pre-pandemic mental health, wellbeing, and risk behaviours and COVID-19 risk perceptions (whole sample).
Statistical analyses
Analyses were conducted in Stata SE (Version 15.0). We used logistic regression to examine cross-sectional and prospective longitudinal associations (hypotheses 1 and 2). We assessed the impact of potential confounding variables by comparing unadjusted and adjusted models. We planned to use multiple regression for hypothesis 2 and model all exposures simultaneously; however, to avoid reductions in sample size (due to pre-pandemic measures at different time points), we ran separate regressions for each exposure. We used linear regression for the PRS analyses (hypothesis 3) and adjusted for the top ten genetic principal components of ancestry (McVean Citation2009).
We analysed data from the whole sample (i.e. combining available data from mothers and young people), accounting for relatedness (i.e. by specifying that the standard errors allow for intragroup correlation, relaxing the independence of observations assumption). We also stratified analyses by generational cohort to explore differences. For example, older age is associated with higher risk perceptions of dying from COVID-19, but lower risk perceptions of being infected, and lower depression and anxiety (Bruine de Bruin and Bennett Citation2020). These stratified analyses were exploratory. We performed complete case analyses for hypotheses 1 and 2, to tease apart possible effects of confounding variables versus reductions in sample size between unadjusted and adjusted models. We report fully adjusted results for COVID-19 holistic risk perceptions unless stated otherwise. Results are interpreted in terms of the strength of evidence against the null hypothesis (e.g. p < .05 provides modest evidence whilst p < .001 provides strong evidence), direction of effect estimates, and consistency of evidence across sensitivity analyses (Sterne and Davey Smith Citation2001).
Results
Participant characteristics
A total of 5,319 mothers and young people completed the second COVID-19 questionnaire, and 5,064 had complete data on COVID-19 risk perceptions. Sample sizes ranged from 413–5,115 for cross-sectional analyses, 233–4,243 for prospective longitudinal analyses, and 3,615–3,672 for PRS analyses. Age ranged from 27 to 29 years for young people (M = 27.7, SD = 0.6), and from 44 to 72 years for mothers (M = 58.1, SD = 4.4); 85% of the whole sample were female (71% of young people), and 98% were of a White ethnic group. Participant characteristics are summarised in Supplementary Tables S2–S7.
Cross-sectional associations (Hypothesis 1)
Whole sample
Cross-sectional results are presented in and . There was strong evidence of a positive association between COVID-19 risk perceptions and GAD (OR 2.78, 95% confidence interval [CI] 2.20 to 3.52, p < .001), depression (OR 1.65, 95% CI 1.24 to 2.18, p < .001), and low wellbeing (OR 1.76, 95% CI 1.45 to 2.13, p < .001). Associations were consistent across risk perception dimensions, except cognitive, where associations with depression and low wellbeing were attenuated in fully adjusted models.
There was no clear evidence of an association between COVID-19 risk perceptions and high-risk drinking (OR 0.95, 95% CI 0.79 to 1.13, p = .54), or increased smoking/e-cigarette use (OR 1.14, 95% CI 0.72 to 1.80, p = .59). There was strong evidence that COVID-19 risk perceptions and increased alcohol use were positively associated (OR 1.46, 95% CI 1.24 to 1.72, p < .001), except for cognitive risk perceptions, which was not robust to adjustment for confounders. There were positive associations between some COVID-19 risk perceptions (holistic, cognitive) and self-isolating given a suspected COVID-19 infection (OR 1.74, 95% CI 1.13 to 2.68, p = .012). There were negative associations between some COVID-19 risk perceptions (holistic, affective, self) and face-to-face contact (OR 0.83, 95% CI 0.70 to 0.98, p = .027), and all COVID-19 risk perceptions and physical contact (OR 0.83, 95% CI 0.68 to 1.00, p = .049).
Sensitivity analyses
Results stratified by cohort are presented in Supplementary Tables S8–S9. Results were largely similar across generations, except for increased alcohol use (positive associations for mothers only), and face-to-face contact (some negative associations for mothers only). Complete case results are presented in Supplementary Tables S10–S12. There were strong positive associations between COVID-19 risk perceptions (except cognitive) and GAD, depression, low wellbeing, and increased alcohol use (Table S10). Positive associations between some risk perceptions and self-isolating remained, as did negative associations between some risk perceptions and social contact.
Prospective longitudinal associations (Hypothesis 2)
Whole sample
Results from prospective analyses with pre-pandemic measures are presented in and . There was strong evidence that pre-pandemic anxiety (OR 1.64, 95% CI 1.29 to 2.09, p < .001) and low wellbeing (OR 1.41, 95% CI 1.15 to 1.74, p = .001) were positively associated with COVID-19 risk perceptions, except cognitive. There was no clear evidence that pre-pandemic depression was associated with COVID-19 risk perceptions (OR 0.94, 95% CI 0.73 to 1.22, p = .65). Pre-pandemic high-risk drinking was negatively associated with COVID-19 self-risk perceptions only (OR 0.78, 95% CI 0.65 to 0.92, p = .004). There was no clear evidence that pre-pandemic smoking (OR 1.14, 95% CI 0.72 to 1.80, p = .59) or e-cigarette use (OR 1.49, 95% CI 0.72 to 3.09, p = .29; Supplementary Table S13) were associated with COVID-19 risk perceptions.
Figure 2. Longitudinal associations between pre-pandemic and early pandemic variables and COVID-19 holistic risk perceptions.
Note. Whole sample. Forest plot shows the fully adjusted odds ratios (circles) and 95% confidence intervals (bar). Fully adjusted = adjusted for age, gender, education, keyworker status, pre-pandemic anxiety, depression, high-risk drinking, smoking, and early pandemic suspected COVID-19 infection.
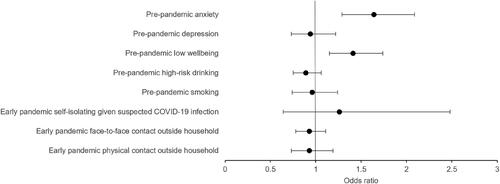
Results from prospective analyses with early pandemic measures are presented in and . There was no clear evidence that early pandemic self-isolating given a suspected COVID-19 infection (OR 1.26, 95% CI 0.64 to 2.48, p = .50), face-to-face contact (OR 0.93, 95% CI 0.78 to 1.11, p = .43), or physical contact (OR 0.93, 95% CI 0.73 to 1.19, p = .56) were associated with later COVID-19 risk perceptions.
Table 3. Longitudinal associations between early pandemic risk behaviours and COVID-19 risk perceptions (whole sample).
Sensitivity analyses
Results stratified by cohort are presented in Supplementary Tables S13–S16. Results were largely similar across generations, except for pre-pandemic high-risk drinking (negative associations with self-risk perceptions for young people only) and smoking (positive associations with self-risk perceptions for mothers only). Results from the complete case analyses are presented in Supplementary Tables S17–S22. Positive associations between pre-pandemic anxiety and low wellbeing and COVID-19 risk perceptions remained, and the negative association between pre-pandemic high-risk drinking and COVID-19 self-risk perceptions remained (Supplementary Table S17).
Polygenic risk score associations (Hypothesis 3)
There was no clear evidence that the anxiety PRS was associated with COVID-19 risk perceptions (b 0.12, 95% CI −0.08 to 0.31, p = .24). The depression PRS was positively associated with COVID-19 holistic, affective, and other-risk perceptions (b 0.21, 95% CI 0.02 to 0.40, p = .029), whilst the wellbeing PRS was negatively associated with COVID-19 risk perceptions (except cognitive) (b − 0.29, 95% CI −0.48 to −0.09, p = .004). PRS results are shown in .
Table 4. Prospective longitudinal associations between mental health and wellbeing polygenic risk scores and COVID-19 risk perceptions.
Attrition
Post hoc analyses to explore differential attrition revealed that the anxiety and depression PRS were negatively associated with completion of the first COVID-19 questionnaire (OR 0.92, 95% CI 0.89 to 0.96, p < .001; OR 0.93, 95% CI 0.90 to 0.97, p < .001, respectively) and the second COVID-19 questionnaire (OR 0.95, 95% CI 0.92 to 0.99, p = .02; OR 0.95, 95% CI 0.91 to 0.98, p = .006, respectively). The wellbeing PRS was positively associated with completion of the first (OR 1.12, 95% CI 1.07 to 1.16, p < .001) and second (OR 1.10, 95% CI 1.05 to 1.14, p < .001) COVID-19 questionnaires.
Discussion
In support of hypothesis 1, higher COVID-19 risk perceptions (except cognitive) were cross-sectionally associated with higher anxiety, depression, lower wellbeing, and increased alcohol use. For some risk perception measures, higher COVID-19 risk perceptions were associated with self-isolating given a suspected COVID-19 infection, and less social contact. Our findings support studies that have found associations between higher COVID-19 risk perceptions and worse mental health (Han et al. Citation2021; Li and Lyu Citation2020; Yin et al. Citation2021; Zhong et al. Citation2021), drinking more than usual (Garnett et al. Citation2021), and increased COVID-19 prevention behaviours (Dryhurst et al. Citation2020; Schneider et al. Citation2021). COVID-19 risk perceptions were not associated with high-risk drinking or increased smoking/e-cigarette use.
In support of hypothesis 2, pre-pandemic anxiety and low wellbeing were associated with higher COVID-19 risk perceptions (except cognitive), indicating a temporal relationship consistent with a causal effect of anxiety and wellbeing on later risk perceptions. However, pre-pandemic depression was only associated with higher COVID-19 risk perceptions in the unadjusted analyses, and there was no clear evidence of an association in the adjusted analyses (which included pre-pandemic anxiety as a covariate). Anxiety and depression are frequently comorbid (Lamers et al. Citation2011), therefore, comorbid anxiety may have been driving the unadjusted associations for pre-pandemic depression. Pre-pandemic high-risk drinking was associated with lower COVID-19 self-risk perceptions. Pre-pandemic smoking and e-cigarette use, and early pandemic self-isolating and social contact were not associated with COVID-19 risk perceptions. These analyses with longitudinal data extend previous findings with cross-sectional data, by helping to determine the temporal direction of associations.
There were differences between COVID-19 risk perception dimensions. Mental health and wellbeing were associated with affective (not cognitive) dimensions, perhaps unsurprisingly as worries are a common feature across anxiety disorders and depression (Rabner et al. Citation2017). Pre-pandemic anxiety was also more strongly associated with COVID-19 worries than pre-pandemic depression, a distinction supported elsewhere (Wright, Steptoe, and Fancourt Citation2021). Cognitive models of anxiety and depression suggest that anxiety is future oriented and predictive of threat, whereas depression is past oriented (Dobson Citation1985), which may explain these differences. Odds of increased alcohol use (measure excluded non-drinkers) were higher among individuals with higher risk perceptions, suggesting a possible drinking to cope mechanism.
In support of hypothesis 3, the wellbeing PRS was negatively associated with COVID-19 risk perceptions (except cognitive), and the depression PRS was positively associated with COVID-19 risk perceptions (except cognitive and self). However, there was no clear evidence of an association for the anxiety PRS. This could be due to limited statistical power; the anxiety PRS was the weakest genetic instrument and explained less variance in the phenotype compared to the depression and wellbeing PRS. Stronger instruments could be created as larger GWAS of more precisely measured phenotypes become available. Furthermore, cohorts with larger samples than ALSPAC would have more power to detect genetic associations. The lack of clear statistical evidence for self-reported pre-pandemic depression (versus depression PRS) may be due to measurement differences. The self-report measure represented participants who reported a mild depressive episode, whereas the genome-wide meta-analysis of depression included individuals reporting clinical diagnoses of, and meeting standard criteria for, major depressive disorder. Furthermore, given that anxiety and depression are frequently comorbid (Lamers et al. Citation2011), there may have been statistical overadjustment in models where the other was included as a covariate. Despite some limitations, this is the first study to have used PRS data to understand the relationship between pre-pandemic mental health and wellbeing and COVID-19 risk perceptions. Again, these analyses extend previous findings by helping to support stronger causal inference by reducing the potential for confounding variables.
Results were largely similar across generational cohorts, although exploratory analyses suggested some differences across age groups. First, among mothers, COVID-19 risk perceptions and increased alcohol use were cross-sectionally positively associated, but we did not see evidence of this among young people. This is consistent with evidence of increased alcohol consumption among older (versus younger) individuals during the pandemic (Sallie et al. Citation2020), and drinking to cope is common among older adults (Gilson, Bryant, and Judd Citation2017). However, differences may have been driven by biological sex, because older participants were mothers (i.e. categorised as females). For example, women are more likely than men to drink to cope (Peltier et al. Citation2019). Second, some negative associations between COVID-19 risk perceptions and face-to-face contact only held in mothers, which may be explained by age/employment differences; 20% of mothers were retired, potentially making reduction of social contact easier. Third, pre-pandemic high-risk drinking was negatively associated with COVID-19 self-risk perceptions in young people only. It is plausible that people who engage in any risky behaviours perceive lower risks to themselves generally. But this association may not have held in older adults, who may be aware of the disproportionate negative effects of COVID-19 on their health (Mueller, McNamara, and Sinclair Citation2020). Finally, pre-pandemic smoking was positively associated with COVID-19 self-risk perceptions in mothers only, again possibly due to age-related risk. Stratified analyses were exploratory; future studies could test the robustness of these findings, which should be considered hypothesis-generating, in other samples.
Our study has limitations. First, the sample was predominantly female and of a White ethnic group, which may impact the generalisability of results. Males report lower COVID-19 risk perceptions (Rodriguez-Besteiro et al. Citation2021; Dryhurst et al. Citation2020). However, we did adjust for biological sex, and we also presented results separately for mothers and young people, with the latter cohort having a greater proportion of males than in the combined cohort. Furthermore, people from Black, Asian, and Minority Ethnic communities are nearly twice as likely to die from COVID-19 than people of a White ethnic group (White and Ayoubkhani Citation2020). Therefore, ethnicity may influence COVID-19 risk perceptions. Second, we combined two generational cohorts, which resulted in a bimodal age distribution. However, we adjusted for age and additionally we conducted analyses stratified by generational cohort. Third, we used pandemic data from one time point, which cannot capture changes as a pandemic evolves (Zhong et al. Citation2021; Brown, Coventry, and Pepper Citation2021). Changes in policies, vaccine development, knowledge, and personal experiences may influence risk perceptions and behaviours. Longitudinal studies with repeated assessments during and after pandemics are required to examine bidirectionality. Fourth, we adjusted for suspected COVID-19 infection because this is associated with lower risk perceptions and higher risk behaviours (Smith et al. Citation2020), however we could not include COVID-19 severity (hospital admission), which likely influences risk perceptions, due to participant disclosure risk. Therefore, there may be unmeasured confounding variables. Fifth, risk perception is a heterogeneous construct, and there is no standardised measure (Lanciano et al. Citation2020). Future studies should also include work/economic and social/relationship risk perceptions to reflect the pervasive impact of a pandemic. For example, work/economic COVID-19 risk perceptions are reportedly higher than those concerning health (Lanciano et al. Citation2020), and increased drinking is more frequent among people reporting economic (versus health) COVID-19 worries (Alpers et al. Citation2021). Sixth, there was evidence of differential attrition; people at a higher risk of anxiety and depression were less likely to have completed the COVID-19 questionnaires. The properties of these missing individuals remain unknown, and hence the bias is difficult to predict. However, this pattern of attrition may have attenuated our associations (e.g. for the anxiety PRS) towards the null (i.e. the true associations may be stronger than reported). Finally, smoking and e-cigarette use were conflated in the COVID-19 questionnaires but should be examined separately. Smokers with higher COVID-19 risk perceptions could have switched to using e-cigarettes, but this would not have been captured in the data.
Our study also has strengths. First, longitudinal data helped to determine the temporal direction of associations, extending findings from previous cross-sectional studies, although cause and effect cannot be established in observational studies. Second, we adjusted analyses for various potential covariates, to reduce the chance of reverse causation and confounding bias. Third, the large sample (albeit relatively small for exploring genetic associations) increased the power to detect associations in the observational analyses. Fourth, we conducted extensive complete case analyses to help tease apart the influence of sample size reductions and potential confounding variables. Fifth, we explored differences between thought-related, feeling-related, self-related, and other-related COVID-19 risk perceptions, which has not been examined previously and has implications for risk communication. Finally, genetic analyses were consistent with the possibility that low wellbeing and depression may play a causal role in COVID-19 risk perceptions, building on insights from previous research that only used self-report data. Although this research question was causal, and we used the best data and methods available to us to answer this, inferences must be cautious. Mendelian Randomization (MR) analyses in larger samples are needed to test the causality question fully. Genetic variants can be used in MR analyses to provide (under certain assumptions) unconfounded causal estimates (Davey Smith and Ebrahim Citation2003). MR typically uses single-nucleotide polymorphisms (SNPs) that reach genome-wide significance (i.e. p < 5 × 10−8) (Richardson et al. Citation2019). PRS can be derived using more liberal p-value thresholds, which capture more genetic variance but can reduce the specificity of the PRS to the exposure of interest (e.g. by including more variants with pleiotropic effects).
COVID-19 risk perceptions were associated with poorer mental health, lower wellbeing, and increased alcohol use, and pre-pandemic anxiety and low wellbeing increased COVID-19 risk perceptions. This is concerning, given the increase in alcohol-related deaths in 2020 (Holmes and Angus Citation2021), and because worries about adversities can be as detrimental for mental health as actually experiencing adversities (Wright, Steptoe, and Fancourt Citation2021). However, some risk perceptions were also associated with COVID-19 transmission-related behaviours. A balanced approach to risk communication and public health messaging, in the context of the current pandemic and during future pandemics, is therefore required. As well as promoting public awareness of pandemic-related physical health risks to maintain rational risk perceptions and adherence to government guidelines, political and public health officials must also promote mental health and wellbeing for example by providing reassurance, adaptive coping strategies, and remote interventions to help people manage their worries (Zhong et al. Citation2021; Orte et al. Citation2020; Han et al. Citation2021; Bruine de Bruin and Bennett Citation2020). COVID-19 will be prevalent for years to come, with many scientists predicting that the virus that causes COVID-19 (SARS-CoV-2) will become endemic (Phillips Citation2021; Li et al. Citation2020). Furthermore, these findings about the interplay between COVID-19 risk perceptions, mental health, wellbeing, and risk behaviours will be valuable for future pandemics, informing broader pandemic preparedness efforts.
Conclusions
Higher COVID-19 risk perceptions were associated with anxiety, depression, low wellbeing, increased alcohol use, and COVID-19 transmission-related behaviours. Pre-pandemic anxiety and low wellbeing were associated with higher COVID-19 risk perceptions, and pre-pandemic high-risk drinking was associated with lower COVID-19 risk perceptions regarding oneself. Associations were most robust for anxiety and low wellbeing given the consistency across risk perception dimensions (except cognitive), cross-sectional and prospective analyses, and complete case analyses. Genetic analyses were consistent with the possibility that low wellbeing and depression may play a causal role in COVID-19 risk perceptions, but formal MR analyses in larger samples are warranted. This study offers a novel contribution to the field because of its use of longitudinal and genetic data, inclusion of different components of COVID-19 risk perceptions, and relatively large sample size. These findings have implications for the understanding and management of COVID-19 in the long-term, and of future pandemics.
Contributors
MLD wrote the study protocol and co-designed the study with all authors. HMS extracted the genetic data and created the polygenic risk scores. MLD extracted the self-report data, cleaned the data, and performed all the analyses. HMS and JNK performed quality control checks of data extraction, data cleaning, and analysis code. All authors discussed and interpreted the results. MLD wrote the manuscript with contributions from all authors. All authors approved the final version.
rjrr_a_2127849_sm0921.docx
Download MS Word (538 KB)Acknowledgements
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses. We would also like to thank Dr Anna Blackwell for some early comments on the protocol.
Disclosure statement
No potential competing interest was reported by the authors.
Data availability statement
The analysis code is available from the University of Bristol’s Research Data Repository, data.bris, at https://doi.org/10.5523/bris.34bmhh800n6pb25aeva7qucjre. GWAS summary statistics used to create the PRS are available from the original publications. The informed consent obtained from ALSPAC participants does not allow the data to be made freely available through any third party maintained public repository. However, data used for this submission can be made available on request to the ALSPAC Executive. The ALSPAC data management plan describes in detail the policy regarding data sharing, which is through a system of managed open access. Full instructions for applying for data access can be found here: http://www.bristol.ac.uk/alspac/researchers/access/. The ALSPAC study website contains details of all the data that are available (http://www.bristol.ac.uk/alspac/researchers/our-data/).
Additional information
Funding
References
- Action on Smoking and Health. 2020. “Use of e-Cigarettes (Vapes) among Adults in Great Britain.”
- Alpers, Silvia Eiken, Jens Christoffer Skogen, Silje Maeland, Ståle Pallesen, Åsgeir Kjetland Rabben, Linn-Heidi Lunde, and Lars Thore Fadnes. 2021. “Alcohol Consumption during a Pandemic Lockdown Period and Change in Alcohol Consumption Related to Worries and Pandemic Measures.” International Journal of Environmental Research and Public Health 18 (3): 1220. doi:10.3390/ijerph18031220.
- Angold, A., E. J. Costello, S. C. Messer, and A. Pickles. 1995. “Development of a Short Questionnaire for Use in Epidemiological Studies of Depression in Children and Adolescents.” International Journal of Methods in Psychiatric Research 5 (4): 237–249.
- Atchison, C., L. R. Bowman, C. Vrinten, R. Redd, P. Pristera, J. Eaton, and H. Ward. 2021. “Early Perceptions and Behavioural Responses during the COVID-19 Pandemic: A Cross-Sectional Survey of UK Adults.” BMJ Open 11 (1): e043577. doi:10.1136/bmjopen-2020-043577.
- Baselmans, B. M. L., R. Jansen, H. F. Ip, J. van Dongen, A. Abdellaoui, M. P. van de Weijer, Y. Bao, Bios consortium, Consortium Social Science Genetic Association, et al. 2019. “Multivariate Genome-Wide Analyses of the Well-Being Spectrum.” Nature Genetics 51 (3): 445–451. doi:10.1038/s41588-018-0320-8.
- Bem, D. J. 1972. “Self-Perception Theory.” Advances in Experimental Social Psychology 6: 1–62. doi:10.1016/S0065-2601(08)60024-6.
- Boyd, A., J. Golding, J. Macleod, D. A. Lawlor, A. Fraser, J. Henderson, L. Molloy, A. Ness, S. Ring, and G. Davey Smith. 2013. “Cohort Profile: The ‘Children of the 90s’–The Index Offspring of the Avon Longitudinal Study of Parents and Children.” International Journal of Epidemiology 42 (1): 111–127. doi:10.1093/ije/dys064.
- Brown, R., L. Coventry, and G. Pepper. 2021. “COVID-19: The Relationship between Perceptions of Risk and Behaviours during Lockdown.” Z Gesundh Wiss 1–11. doi:10.1007/s10389-021-01543-9.
- Bruine de Bruin, W, and D. Bennett. 2020. “Relationships between Initial COVID-19 Risk Perceptions and Protective Health Behaviors: A National Survey.” American Journal of Preventive Medicine 59 (2): 157–167. doi:10.1016/j.amepre.2020.05.001.
- Byrne, A., R. Barber, and C. H. Lim. 2021. “Impact of the COVID-19 Pandemic – A Mental Health Service Perspective.” Progress in Neurology and Psychiatry 25 (2): 27–33. doi:10.1002/pnp.708.
- Child Outcomes Research Consortium. 2021. “Mood and Feelings Questionnaire (MFQ).” https://www.corc.uk.net/outcome-experience-measures/mood-and-feelings-questionnaire-mfq/.
- Choi, S. W., T. S. Mak, and P. F. O’Reilly. 2020. “Tutorial: A Guide to Performing Polygenic Risk Score Analyses.” Nature Protocols 15 (9): 2759–2772. doi:10.1038/s41596-020-0353-1.
- Darker, C. 2013. “Risk Perception.” In Encyclopedia of Behavioral Medicine, edited by M. D. Gellman and J. R. Turner, New York: Springer.
- Davey Smith, G, and S. Ebrahim. 2003. “Mendelian Randomization’: Can Genetic Epidemiology Contribute to Understanding Environmental Determinants of Disease?” International Journal of Epidemiology 32 (1): 1–22. doi:10.1093/ije/dyg070.
- Department of Health and Social Care. 2014. “Wellbeing and Health Policy.”
- Dobson, K. S. 1985. “The Relationship between Anxiety and Depression.” Clinical Psychology Review 5 (4): 307–324. doi:10.1016/0272-7358(85)90010-8.
- Dryhurst, S., C. R. Schneider, J. Kerr, A. L. J. Freeman, G. Recchia, A. M. van der Bles, D. Spiegelhalter, and S. van der Linden. 2020. “Risk Perceptions of COVID-19 around the World.” Journal of Risk Research 23 (7-8): 994–1006. doi:10.1080/13669877.2020.1758193.
- Ferrer, R., and W. M. Klein. 2015. “Risk Perceptions and Health Behavior.” Current Opinion in Psychology 5: 85–89. doi:10.1016/j.copsyc.2015.03.012.
- Festinger, L. 1957. A Theory of Cognitive Dissonance. Stanford, CA: Stanford University Press.
- Floyd, D. L., S. Prentice-Dunn, and R. W. Rogers. 2000. “A Meta-Analysis of Research on Protection Motivation Theory.” Journal of Applied Social Psychology 30 (2): 407–429. doi:10.1111/j.1559-1816.2000.tb02323.x.
- Fraser, A., C. Macdonald-Wallis, K. Tilling, A. Boyd, J. Golding, G. Davey Smith, J. Henderson, et al. 2013. “Cohort Profile: The Avon Longitudinal Study of Parents and Children: ALSPAC Mothers Cohort.” International Journal of Epidemiology 42 (1): 97–110. doi:10.1093/ije/dys066.
- Freeman, A. L. J., J. Kerr, G. Recchia, C. R. Schneider, A. C. E. Lawrence, L. Finikarides, G. Luoni, S. Dryhurst, and D. Spiegelhalter. 2021. “Communicating Personalized Risks from COVID-19: Guidelines from an Empirical Study.” Royal Society Open Science 8 (4): 201721. doi:10.1098/rsos.201721.
- Garnett, C., S. Jackson, M. Oldham, J. Brown, A. Steptoe, and D. Fancourt. 2021. “Factors Associated with Drinking Behaviour during COVID-19 Social Distancing and Lockdown among Adults in the UK.” Drug and Alcohol Dependence 219: 108461. doi:10.1016/j.drugalcdep.2020.108461.
- Gilson, K. M., C. Bryant, and F. Judd. 2017. “Understanding Older Problem Drinkers: The Role of Drinking to Cope.” Addictive Behaviors 64: 101–106. doi:10.1016/j.addbeh.2016.08.032.
- Han, Q., B. Zheng, M. Agostini, J. J. Belanger, B. Gutzkow, J. Kreienkamp, A. M. Reitsema, J. A. van Breen, P. Collaboration, and N. P. Leander. 2021. “Associations of Risk Perception of COVID-19 with Emotion and Mental Health during the Pandemic.” Journal of Affective Disorders 284: 247–255. doi:10.1016/j.jad.2021.01.049.
- Harris, P. A., R. Taylor, R. Thielke, J. Payne, N. Gonzalez, and J. G. Conde. 2009. “Research Electronic Data Capture (REDCap)–A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support.” Journal of Biomedical Informatics 42 (2): 377–381. doi:10.1016/j.jbi.2008.08.010.
- Hartmann-Boyce, J., H. McRobbie, N. Lindson, C. Bullen, R. Begh, A. Theodoulou, C. Notley, et al. 2021. “Electronic Cigarettes for Smoking Cessation.” The Cochrane Database of Systematic Reviews 4: CD010216. doi:10.1002/14651858.CD010216.pub5.
- Hill, A. B. 2015. “The Environment and Disease: Association or Causation? (Reprinted from JRSM, Vol 58, 1965).” Journal of the Royal Society of Medicine 108 (1): 32–37. doi:10.1177/0141076814562718.
- Holmes, J., and C. Angus. 2021. “Alcohol Deaths Rise Sharply in England and Wales.” BMJ 372: n607. doi:10.1136/bmj.n607.
- Howard, D. M., M. J. Adams, T. K. Clarke, J. D. Hafferty, J. Gibson, M. Shirali, J. R. I. Coleman, Major Depressive Disorder Working Group of the Psychiatric Genomics Consortium, et al. 2019. “Genome-Wide Meta-Analysis of Depression Identifies 102 Independent Variants and Highlights the Importance of the Prefrontal Brain Regions.” Nature Neuroscience 22 (3): 343–352. doi:10.1038/s41593-018-0326-7.
- Jackson, S. E., J. Brown, L. Shahab, A. Steptoe, and D. Fancourt. 2021. “COVID-19, Smoking and Inequalities: A Study of 53 002 Adults in the UK.” Tobacco Control 30 (e2): e111–e121. doi:10.1136/tobaccocontrol-2020-055933.
- Jarbin, H., T. Ivarsson, M. Andersson, H. Bergman, and G. Skarphedinsson. 2020. “Screening Efficiency of the Mood and Feelings Questionnaire (MFQ) and Short Mood and Feelings Questionnaire (SMFQ) in Swedish Help Seeking Outpatients.” PloS One 15 (3): e0230623. doi:10.1371/journal.pone.0230623.
- Kelly, T. M., J. E. Donovan, T. Chung, O. G. Bukstein, and J. R. Cornelius. 2009. “Brief Screens for Detecting Alcohol Use Disorder among 18–20 Year Old Young Adults in Emergency Departments: Comparing AUDIT-C, CRAFFT, RAPS4-QF, FAST, RUFT-Cut, and DSM-IV 2-Item Scale.” Addictive Behaviors 34 (8): 668–674. doi:10.1016/j.addbeh.2009.03.038.
- Kelly, B. C., M. Pawson, and M. Vuolo. 2021. “Beliefs on COVID-19 among Electronic Cigarette Users: Behavioral Responses and Implications for COVID Prevention and E-Cigarette Interventions.” Journal of Drug Issues 51 (2): 284–300. doi:10.1177/0022042620977828.
- Kroenke, K., R. L. Spitzer, J. B. Williams, P. O. Monahan, and B. Lowe. 2007. “Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection.” Annals of Internal Medicine 146 (5): 317–325. doi:10.7326/0003-4819-146-5-200703060-00004.
- Kwong, A. S. F., R. M. Pearson, M. J. Adams, K. Northstone, K. Tilling, D. Smith, C. Fawns-Ritchie, et al. 2021. “Mental Health before and during the COVID-19 Pandemic in Two Longitudinal UK Population Cohorts.” The British Journal of Psychiatry 218 (6): 334–343. doi:10.1192/bjp.2020.242.
- Lamers, F., P. van Oppen, H. C. Comijs, J. H. Smit, P. Spinhoven, A. J. van Balkom, W. A. Nolen, F. G. Zitman, A. T. Beekman, and B. W. Penninx. 2011. “Comorbidity Patterns of Anxiety and Depressive Disorders in a Large Cohort Study: The Netherlands Study of Depression and Anxiety (NESDA).” The Journal of Clinical Psychiatry 72 (3): 341–348. doi:10.4088/JCP.10m06176blu.
- Lanciano, T., G. Graziano, A. Curci, S. Costadura, and A. Monaco. 2020. “Risk Perceptions and Psychological Effects during the Italian COVID-19 Emergency.” Frontiers in Psychology 11: 580053. doi:10.3389/fpsyg.2020.580053.
- Lawlor, D. A., K. Tilling, and G. Davey Smith. 2016. “Triangulation in Aetiological Epidemiology.” International Journal of Epidemiology 45 (6): 1866–1886. doi:10.1093/ije/dyw314.
- Lerner, J. S, and D. Keltner. 2000. “Beyond Valence: Toward a Model of Emotionspecific Influences on Judgement and Choice.” Cognition & Emotion 14 (4): 473–493. doi:10.1080/026999300402763.
- Li, X, and H. Lyu. 2020. “Epidemic Risk Perception, Perceived Stress, and Mental Health during COVID-19 Pandemic: A Moderated Mediating Model.” Frontiers in Psychology 11: 563741. doi:10.3389/fpsyg.2020.563741.
- Li, R., S. Pei, B. Chen, Y. Song, T. Zhang, W. Yang, and J. Shaman. 2020. “Substantial Undocumented Infection Facilitates the Rapid Dissemination of Novel Coronavirus (SARS-CoV-2).” Science (New York, N.Y.) 368 (6490): 489–493. doi:10.1126/science.abb3221.
- Liu, M., H. Zhang, and H. Huang. 2020. “Media Exposure to COVID-19 Information, Risk Perception, Social and Geographical Proximity, and Self-Rated Anxiety in China.” BMC Public Health 20 (1): 1649. doi:10.1186/s12889-020-09761-8.
- McCloskey, B, and D. L. Heymann. 2020. “SARS to Novel Coronavirus – Old Lessons and New Lessons.” Epidemiology and Infection 148: e22. doi:10.1017/S0950268820000254.
- McVean, G. 2009. “A Genealogical Interpretation of Principal Components Analysis.” PLoS Genetics 5 (10): e1000686. doi:10.1371/journal.pgen.1000686.
- Mind. 2020. The Mental Health Emergency: How Has the Coronavirus Pandemic Impacted Our Mental Health? London: Mind.
- Mueller, A. L., M. S. McNamara, and D. A. Sinclair. 2020. “Why Does COVID-19 Disproportionately Affect Older People?” Aging 12 (10): 9959–9981. doi:10.18632/aging.103344.
- Northstone, K., S. Howarth, D. Smith, C. Bowring, N. Wells, and N. J. Timpson. 2020. “The Avon Longitudinal Study of Parents and Children – A Resource for COVID-19 Research: Questionnaire Data Capture April-May 2020.” Wellcome Open Research 5: 127. doi:10.12688/wellcomeopenres.16020.2.
- Northstone, K., M. Lewcock, A. Groom, A. Boyd, J. Macleod, N. Timpson, and N. Wells. 2019. “The Avon Longitudinal Study of Parents and Children (ALSPAC): An Update on the Enrolled Sample of Index Children in 2019.” Wellcome Open Research 4: 51. doi:10.12688/wellcomeopenres.15132.1.
- Northstone, K., D. Smith, C. Bowring, N. Wells, M. Crawford, S. Haworth, and N. J. Timpson. 2020. “The Avon Longitudinal Study of Parents and Children – A Resource for COVID-19 Research: Questionnaire Data Capture May–July 2020.” Wellcome Open Research 5: 210. doi:10.12688/wellcomeopenres.16225.2.
- Orte, C., L. Sanchez-Prieto, D. C. Dominguez, and A. Barrientos-Baez. 2020. “Evaluation of Distress and Risk Perception Associated with COVID-19 in Vulnerable Groups.” International Journal of Environmental Research and Public Health 17 (24): 9207. doi:10.3390/ijerph17249207.
- Paek, H.-J, and T. Hove. 2017. “Risk Perceptions and Risk Characteristics.” In Oxford Research Encyclopedia of Communication. USA: Oxford University Press.
- Panno, A., G. A. Carbone, C. Massullo, B. Farina, and C. Imperatori. 2020. “COVID-19 Related Distress is Associated with Alcohol Problems, Social Media and Food Addiction Symptoms: Insights from the Italian Experience during the Lockdown.” Frontiers in Psychiatry 11: 577135. doi:10.3389/fpsyt.2020.577135.
- Peltier, M. R., T. L. Verplaetse, Y. S. Mineur, I. L. Petrakis, K. P. Cosgrove, M. R. Picciotto, and S. A. McKee. 2019. “Sex Differences in Stress-Related Alcohol Use.” Neurobiology of Stress 10: 100149. doi:10.1016/j.ynstr.2019.100149.
- Phillips, N. 2021. “The Coronavirus is Here to Stay – Here’s What That Means.” Nature 590 (7846): 382–384. doi:10.1038/d41586-021-00396-2.
- Purves, Kirstin L., Jonathan R. I. Coleman, Sandra M. Meier, Christopher Rayner, Katrina A. S. Davis, Rosa Cheesman, Marie Baekvad-Hansen, et al. 2020. “A Major Role for Common Genetic Variation in Anxiety Disorders.” Molecular Psychiatry 25 (12): 3292–3303. doi:10.1038/s41380-019-0559-1.
- Rabner, J., N. D. Mian, D. A. Langer, J. S. Comer, and D. Pincus. 2017. “The Relationship between Worry and Dimensions of Anxiety Symptoms in Children and Adolescents.” Behavioural and Cognitive Psychotherapy 45 (2): 124–138. doi:10.1017/S1352465816000448.
- Richardson, T. G., S. Harrison, G. Hemani, and G. Davey Smith. 2019. “An Atlas of Polygenic Risk Score Associations to Highlight Putative Causal Relationships across the Human Phenome.” eLife 8. doi:10.7554/eLife.43657.
- Rodriguez-Besteiro, S., J. F. Tornero-Aguilera, J. Fernandez-Lucas, and V. J. Clemente-Suarez. 2021. “Gender Differences in the COVID-19 Pandemic Risk Perception, Psychology, and Behaviors of Spanish University Students.” International Journal of Environmental Research and Public Health 18 (8): 3908. doi:10.3390/ijerph18083908.
- Rogers, R. D. 1975. “A Protection Motivation Theory of Fear Appeals and Attitude Change.” The Journal of Psychology 91 (1): 93–114. doi:10.1080/00223980.1975.9915803.
- Sallie, S. N., V. Ritou, H. Bowden-Jones, and V. Voon. 2020. “Assessing International Alcohol Consumption Patterns during Isolation from the COVID-19 Pandemic Using an Online Survey: Highlighting Negative Emotionality Mechanisms.” BMJ Open 10 (11): e044276. doi:10.1136/bmjopen-2020-044276.
- Savadori, L., and M. Lauriola. 2020. “Risk Perception and Protective Behaviors during the Rise of the COVID-19 Outbreak in Italy.” Frontiers in Psychology 11: 577331. doi:10.3389/fpsyg.2020.577331.
- Schneider, C. R., S. Dryhurst, J. Kerr, A. L. J. Freeman, G. Recchia, D. Spiegelhalter, and S. van der Linden. 2021. “COVID-19 Risk Perception: A Longitudinal Analysis of Its Predictors and Associations with Health Protective Behaviours in the United Kingdom.” Journal of Risk Research 24 (3–4): 294–313. doi:10.1080/13669877.2021.1890637.
- Shepherd, J. M., B. Fogle, L. Garey, A. G. Viana, and M. J. Zvolensky. 2021. “Worry about COVID-19 in Relation to Cognitive-Affective Smoking Processes among Daily Adult Combustible Cigarette Smokers.” Cognitive Behavioral Therapy 50 (4): 336–350. doi:10.1080/16506073.2020.1866657.
- Smith, L. E., A. L. Mottershaw, M. Egan, J. Waller, T. M. Marteau, and G. J. Rubin. 2020. “The Impact of Believing You Have Had COVID-19 on Self-Reported Behaviour: Cross-Sectional Survey.” PLoS One 15 (11): e0240399. doi:10.1371/journal.pone.0240399.
- Spitzer, R. L., K. Kroenke, J. B. Williams, and B. Lowe. 2006. “A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7.” Archives of Internal Medicine 166 (10): 1092–1097. doi:10.1001/archinte.166.10.1092.
- Sterne, J. A., and G. Davey Smith. 2001. “Sifting the Evidence-What’s Wrong with Significance Tests?” BMJ (Clinical Research ed.) 322 (7280): 226–231. doi:10.1136/bmj.322.7280.226.
- Tennant, R., L. Hiller, R. Fishwick, S. Platt, S. Joseph, S. Weich, J. Parkinson, J. Secker, and S. Stewart-Brown. 2007. “The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): Development and UK Validation.” Health and Quality of Life Outcomes 5: 63. doi:10.1186/1477-7525-5-63.
- Tzu-Hsuan Chen, D. 2020. “The Psychosocial Impact of the COVID-19 Pandemic on Changes in Smoking Behavior: Evidence from a Nationwide Survey in the UK.” Tobacco Prevention & Cessation 6: 59. doi:10.18332/tpc/126976.
- Wambua, J., L. Hermans, P. Coletti, F. Verelst, L. Willem, C. I. Jarvis, A. Gimma, et al. 2022. “The Influence of Risk Perceptions on Close Contact Frequency during the SARS-CoV-2 Pandemic.” Scientific Reports 12 (1): 5192. doi:10.1038/s41598-022-09037-8.
- Warwick Medical School. 2020. “What is Mental Wellbeing?.” https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/mentalwellbeing/.
- Warwick Medical School. 2021. “Collect, Score, Analyse and Interpret WEMWBS.” https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/using/howto/.
- White, C, and D. Ayoubkhani. 2020. Rates of Deaths Involving the Coronavirus (COVID-19) by Ethnic Group, England and Wales. edited by Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/ratesofdeathsinvolvingthecoronaviruscovid19byethnicgroupenglandandwales
- White, Augustus M., Dongmei Li, L. Morgan Snell, Richard O’Connor, Cosima Hoetger, Daniel Croft, Rebecca. C. Lester, et al. 2021. “Perceptions of Tobacco Product-Specific COVID19 Risk and Changes in Tobacco Use Behaviors among Smokers, e-Cigarette Users, and Dual Users.” Nicotine & Tobacco Research 23 (9): 1617–1622. doi:10.1093/ntr/ntab053.
- Wise, T., T. D. Zbozinek, G. Michelini, C. C. Hagan, and D. Mobbs. 2020. “Changes in Risk Perception and Self-Reported Protective Behaviour during the First Week of the COVID-19 Pandemic in the United States.” Royal Society Open Science 7 (9): 200742. doi:10.1098/rsos.200742.
- World Health Organisation. 2019. “Mental Disorders.” https://www.who.int/news-room/fact-sheets/detail/mental-disorders.
- World Health Organisation. 2021a. “Timeline: WHO’s COVID-19 Response.” https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline/#!
- World Health Organisation. 2021b. “WHO Coronavirus (COVID-19) Dashboard.” https://covid19.who.int/.
- Wright, L., A. Steptoe, and D. Fancourt. 2021. “Does Thinking Make It so? Differential Associations between Adversity Worries and Experiences and Mental Health during the COVID-19 Pandemic.” Journal of Epidemiology and Community Health 75 (9): 817–823. doi:10.1136/jech-2020-215598.
- Yin, Q., A. Chen, X. Song, G. Deng, and W. Dong. 2021. “Risk Perception and PTSD Symptoms of Medical Staff Combating against COVID-19: A PLS Structural Equation Model.” Front Psychiatry 12 (607612). doi:10.3389/fpsyt.2021.607612.
- Yingst, J. M., N. M. Krebs, C. R. Bordner, A. L. Hobkirk, S. I. Allen, and J. Foulds. 2021. “Tobacco Use Changes and Perceived Health Risks among Current Tobacco Ssers during the COVID-19 Pandemic.” International Journal of Environmental Research and Public Health 18 (4): 1795. doi:10.3390/ijerph18041795.
- Zhong, Y., W. Liu, T. Y. Lee, H. Zhao, and J. Ji. 2021. “Risk Perception, Knowledge, Information Sources and Emotional States among COVID-19 Patients in Wuhan, China.” Nursing Outlook 69 (1): 13–21. doi:10.1016/j.outlook.2020.08.005.
