Abstract
Nowadays, there is an increased availability of online health risk calculators aimed at providing people with personalized risk estimates of experiencing a medical disease. Despite being deemed as more relevant and useful than generic risk estimates, personalized risks are intrinsically imperfect and inherently uncertain, arising from limitations in the reliability, credibility, and accuracy of probability estimates (i.e. epistemic uncertainty). However, whether epistemic uncertainty around personalized risk estimates should be communicated to people is a topic of debate. In this pre-registered and conceptual replication study, participants (N = 239) were randomized to a 2 [Type of risk: personalized, generic] x 2 [Uncertainty: yes, no] between-subject design, in which they read a hypothetical scenario of a person who wanted to know his/her risk of developing colorectal cancer. Half of the participants used an online risk calculator for receiving a personalized risk, and half received a generic (non-personalized) risk of colon cancer. Furthermore, half of the participants received uncertainty information through a range estimate (‘5% to 13%’), and the other half received no uncertainty information by using a point estimate (‘9%’). Primary outcome measures were perceived risk and cancer-related worry. Perceived credibility was measured as a potential mediating variable, while subjective numeracy and health literacy were serving as control variables. People who received personalized cancer risk estimates reported lower risk perceptions and cancer worry compared to people who received generic cancer risk estimates. However, communicating risks with epistemic uncertainty led to higher risk perceptions than communicating risks without uncertainty, but only for those who received personalized risks. Such an interplay was not found for generic risk estimates. Overall, these interaction effects were not mediated by perceived credibility. In conclusion, psychological effects of disclosing epistemic uncertainty around risk estimates may only be applicable to individualized disease risk information.
Introduction
Nowadays, there is an increased availability of online health risk calculators for people to access (Trevena et al. Citation2021; Waters et al. Citation2020; Witteman et al. Citation2011). These risk calculators provide people the opportunity to enter unique individual characteristics (e.g. demographics, lifestyle, medical history, or family history) for generating personalized risks estimates of experiencing various medical diseases (e.g. ‘Your personal lifetime chance of developing colorectal cancer is 9%’). Compared to generic or non-personalized risks, personalized risks are deemed more relevant (Lustria et al. Citation2016; Vromans et al. Citation2020) and useful for medical decision-making (Vromans, Pauws, et al. Citation2022), and may help patients make better informed and deliberative decisions facilitated by increased knowledge and more realistic risk perceptions (Albada et al. Citation2009; Edwards et al. Citation2013; Scherer et al. Citation2013). The added value of personalized risk information is also reflected in the increased integration of individualized risk estimates in web-based tools for supporting shared decision-making and promoting patient-centred care in various disease contexts (Ankersmid et al. Citation2022; Harrison et al. Citation2019; Hochstenbach et al. Citation2023).
However, personalized risk estimates are intrinsically imperfect and inherently uncertain (van der Bles et al. Citation2019). Following the integrative model of uncertainty tolerance (Han, Babrow, et al. Citation2019), these uncertainties may arise from two different sources. The first source, aleatory uncertainty (also known as first-order uncertainty or ‘risk’) relates to the unpredictability of future events. For instance, when an online risk calculator shows a person a personalized risk of 9% of developing colorectal cancer, that estimate cannot say whether that person will eventually develop the disease. The second source, epistemic uncertainty (also known as second-order uncertainty or ‘ambiguity’) relates to limitations in our knowledge to predict certain outcomes arising from limitations in the reliability, credibility, and adequacy of risk estimates, and is typically expressed through ranges or confidence intervals (‘Your personal lifetime chance of developing colorectal cancer is between 5% and 13%’). Importantly, epistemic uncertainty becomes even more prominent when risk estimates are individualized. That is, when calculating specific risks, one must use a smaller subset of population-based data that matches with individual characteristics of the patient, resulting in a smaller reference group. This, in turn, means that a personalized risk might be more uncertain and less reliable from a statistical point of view. While there is ample research on the psychological effects of disclosing aleatory uncertainty, less attention has been paid to epistemic uncertainty in the context of personalized risk communication (Bonner et al. Citation2021; Han, Babrow, et al. Citation2019; van der Bles et al. Citation2019, Citation2020).
Whether epistemic uncertainty around personalized risk estimates should be communicated to people is a topic of debate. Some scholars believe that statistical uncertainty around personalized risks should always be disclosed to people for ethical reasons. For instance, for the sake of transparency, disclosing epistemic uncertainty may help patients prevent them from attributing an unrealistic degree of certainty to or faith in their personalized risk estimate (Waters et al. Citation2009, Citation2006; Engelhardt et al. Citation2017). Moreover, a full understanding of the limitations and uncertainties of online risk calculators may help people make well-informed and deliberate decisions (Bonner et al. Citation2021). Others, however, believe that such statistical uncertainty information may overwhelm people and lead to ‘ambiguity-averse’ psychological responses (Han et al. Citation2011; Han, Babrow, et al. Citation2019), consisting of heightened perceptions of risk, worry, fear, anxiety, and emotional distress, which in turn can prevent people from taking action (i.e. ambiguity aversion). Moreover, while some healthcare professionals are reluctant to disclose uncertainty information to patients (Engelhardt et al. Citation2017; Bansback et al. Citation2017), some patients still ask for uncertainties around personalized risk estimates (Vromans et al. Citation2021; Vromans, Pauws, et al. Citation2022), or perceive personalized risk still as imperfect or inapplicable to individual patients (Vromans, Pauws, et al. Citation2022). However, systematic knowledge about the psychological effects of communicating uncertainty associated with risk information is needed.
A relative underexplored area is whether the psychological effects of uncertainty communication are universal or not, and whether ambiguity-averse responses depend on whether the risk estimates are personalized towards the situation of an individual patient or not. Arguably, the adverse effects of disclosing uncertainty information may only be found when risks are individualized and perceived as more personally relevant. Indeed, following theoretical models on tailored health communication (Lustria et al. Citation2016; Rimer and Kreuter Citation2006), communicating personalized risk estimates increase people’s perceived personal relevance and the likelihood of being processed more deeply, resulting in better information recall and increased (accuracy of) risk perceptions and affective responses (Emmons et al. Citation2004). Generic risks, on the other hand, may be perceived as less relevant and receive less attention and information processing (Vromans et al. Citation2020), which may cause the effect of epistemic uncertainty communication of people’s risk perceptions and levels of worry to disappear. As such, outcomes of previous studies hint towards a moderating role of personalization in the psychological effects of epistemic uncertainty communication around risk estimates, but empirical evidence for this moderation is currently lacking.
In the present research, we attempted to address this gap by investigating whether the psychological effects of communicating epistemic uncertainty depend on the type of risk that is being given to people (personalized vs. generic risk estimates). We tested the following three pre-registered hypotheses:
H1: Compared to generic cancer risk estimates, communicating personalized cancer risk estimates leads to higher risk perceptions and cancer-related worry.
H2: Compared to cancer risk estimates without epistemic uncertainty, communicating cancer risk estimates with epistemic uncertainty leads to higher risk perceptions and cancer-related worry.
H3: Personalization of cancer risk estimates moderates the psychological impact of communicating epistemic uncertainty: Risk perceptions and cancer-related worry only increase when epistemic uncertainty is communicated around personalized risk estimates (and not for generic cancer risks).
RQ1: To what extent are the effects of the communication of uncertainty and personalization of risk estimates on risk perception and cancer worry mediated by perceived credibility?
Materials and methods
Design and sample
The study design, hypotheses, exploratory objectives, power analysis, and analysis plan were pre-registered prior to data collection and analysis within the Open Science Framework (https://osf.io/7yhkp/). This study partially conceptually replicated experiment 1 of Han et al. (Citation2011) in which the effects of epistemic uncertainty (referred to ‘ambiguity’ by the authors) and representational format (comparing textual and visual representations) on perceived risk and cancer-related worry was examined. In the current study, we used the same independent variable (i.e. epistemic uncertainty), stimulus materials, and outcome measures, but replaced the variable ‘representational format’ by type of risk. We thus adopted a 2 [risk type: personalized vs. generic risk] × 2 [epistemic uncertainty: uncertainty vs. no uncertainty] between-subject design. The primary outcome variables were perceived cancer risk and cancer-related worry. Perceived credibility of risk was the potential mediating variable, and subjective numeracy and health literacy were included as covariates. Qualtrics software (https://www.qualtrics.com) was used to control the experiment in which participants were randomly assigned to one of the four experimental conditions. Ethical approval was acquired from the Research Ethics and Data Management Committee of Tilburg University (REDC.2019.26a).
Dutch adults aged 45 or older were recruited for the current study. This age criterion was established because the development of colon cancer under the age of 45 is very rare in the Netherlands (only 2% of all Dutch cases are younger than 45; (Netherlands Comprehensive Cancer Organisation (IKNL)) Citation2020)). Participants were recruited through convenience sampling with the use of the personal networks of the researchers and via private and public Facebook groups (e.g. groups with information about cancer, health and diet groups, lifestyle groups, and groups where help is offered to others). Some of the approached participants shared the online experiment with their personal network, which resulted in a snowball effect. As part of the pre-registration, a power analysis was performed using G*Power 3.1.9.2 (Faul et al. Citation2007). This power analysis was based on the main effect of epistemic uncertainty on cancer-related worry, as found by Han et al. (Citation2011; see page 359). Since the authors did not report effect sizes or descriptive statistics in their paper (i.e. means and standard deviations), we assumed a medium-sized effect (f = 0.25) with a power of 0.95 (numerator df = 1, number of groups = 4, α = .05) for testing ‘Fixed effects, special, main effects, and interactions’ with analysis of variances (ANOVA). For this, a sample size of 210 participants was needed.
Materials
Hypothetical scenario
All participants read a hypothetical scenario of a person (with information about that person’s age, lifestyle, medical, and family history) visiting a webpage of the Netherlands Cancer Institute for knowing his/her risk of developing colon cancer, and they were instructed to imagine how they would feel if they experienced the provided scenario. The use of such scenarios is common within health risk communication research among a healthy population (Han et al. Citation2011; Vromans, Pauws, et al. Citation2022). The characteristics that were described in this scenario corresponded to the risk level of 9% that was communicated in the estimates of the current study, to avoid a discrepancy between the scenario and the communicated risk level. Afterwards, participants were asked to indicate how easy or difficult it was for them to imagine themselves in the scenario.
Cancer risk estimates
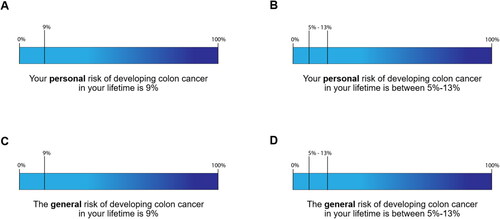
All participants were shown information about the risk of developing colon cancer in their lifetime in one of the four experimental conditions (). Half of the participants received a personalized risk by using an online risk calculator (a Dutch version of the NCI Colorectal Cancer Risk Assessment Tool) and by entering personal characteristics of the hypothetical person (i.e. items about lifestyle and medical and family history) and receiving a result that was then displayed (‘Your personal risk of developing colon cancer in your lifetime is 9%’). The other half did not use a risk calculator and only saw the generic risk of colon cancer (‘The general risk of developing colon cancer in your lifetime is 9%’) displayed on the webpage. Furthermore, half of the participants received uncertainty information through a range estimate (‘5% to 13%’), and the other half received no uncertainty information by using a point estimate (‘9%’). All participants received the risk information (and associated uncertainty information) numerically and visually (visual number line ‘with solid borders to depict point estimates and confidence intervals’, Han et al. Citation2011, p. 357). The risk communication tool, risk estimate, associated range intervals, and message format were adapted from Han et al. (Citation2011).
Measures
Perceived cancer risk
Perceived cancer risk was measured with two items, including ‘Based on this risk estimation, how would you describe your chances of developing colon cancer in your lifetime? Would you say your chances of getting colon cancer are…’ and ‘If I received these results, I would feel that I’m going to get colon cancer’ (Han et al. Citation2011). Both items were translated into Dutch. Answer options ranged from 1 (very low/strongly disagree) to 5 (very high/strongly agree), of which mean scores were calculated (α = .89).
Cancer-related worry
Cancer-related worry was measured with four items. The first item was adopted from Han et al. (Citation2011), ‘If you received these results, to what extent would you feel worried about developing colon cancer?’, measured on scale from 1 (not at all) to 5 (extremely). The other three items were adopted from Lipkus et al. (Citation2005), including ‘How worried/fearful/anxious are you about developing colon cancer throughout your life?’, measured on a scale from 1 (not at all) to 5 (very much). These four items were also translated into Dutch, and responses to these four items were averaged (α = .95).
Perceived credibility
Perceived credibility of the risk estimate was measured with two items, including ‘How accurate do these results seem to you?’, and ‘How much would you trust the communicated risk estimates?’ (Han et al. Citation2011), measured on a scale from 1 (not at all accurate/not at all) to 5 (very/completely). Both items were translated into Dutch, and responses to both items were averaged (α = .80).
Individual differences
Subjective numeracy was measured using the Subjective Numeracy Scale (α = .86; SNS) (Fagerlin et al. Citation2007), as this scale has been validated to correlate with objective numeracy levels (Zikmund-Fisher et al. Citation2007). This scale consists of eight items that are measured on 6-point Likert scales from least numerate to most numerate. A Dutch version of this scale was used (Vromans et al. Citation2020), and responses to these eight items were averaged with higher scores indicating higher numeracy skills.
Health literacy was assessed with Dutch version of the Short Assessment of Health Literacy (SAHL) test (Maat et al. Citation2014). This test consists of thirteen health-related concepts of which participants are asked to indicate what they mean choosing one out of three possible meanings. Each answer was coded as 1 (correct) or 0 (incorrect), and a sum score was calculated (range: 0-13) with higher scores representing higher health literacy skills.
Manipulation check
Perceived personal relevance was measured with two items (Lustria et al. Citation2016). The items comprised ‘The risk estimate was made personally for me’ and ‘The way the risk estimate was being presented was relevant to me’ (α = .83). Both items were measured on a scale from 1 (completely disagree) to 5 (completely agree).
Statistical analyses
Chi-square tests and factorial analyses of variance (ANOVAs) were conducted to check for unequal distribution of background and individual difference variables over the four experimental conditions. The check whether personalized risks were perceived as more personally relevant than generic risks (i.e. manipulation check), an independent t-test was conducted. In addition, two separate independent t-tests were conducted for both items of perceived relevance for which we adjusted for multiple comparisons. To test the effects of risk type and uncertainty on perceived risk and cancer-related worry (H1-H3), a multivariate analysis of variance (MANOVA) was conducted. Additional simple effect analyses were performed to examine differences between conditions within the risk type. As part of our preregistration, we also run a multivariate analysis of covariance (MANCOVA) with the same variables while adjusting for subjective numeracy and health literacy. As an exploratory analysis, we also run the MANCOVA while controlling for gender and education. To explore the mediating role of perceived credibility (RQ1), we first conducted a factorial ANOVA to examine the effects of risk type and uncertainty on perceived credibility, followed by a moderated mediation analysis (model 7) using Hayes’ PROCESS Macro (Hayes Citation2022). All statistical analyses were performed using SPSS version 27.0 (IBM Corporation, Somers, NY, USA), and and were created using Jamovi Software version 2.3 (The jamovi project Citation2023). Tests were two-sided and considered statistically significant at p < .05.
Results
Sample characteristics
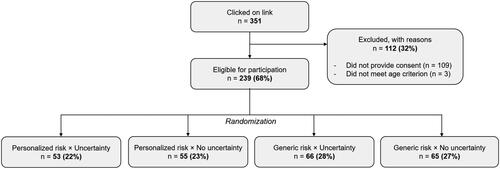
Of the 351 participants who clicked on the link of the experiment, 242 provided consent. Three participants were aged younger than 45 and were excluded from the sample, resulting in a total of 239 (68%) Dutch participants for the data analyses (). The mean age was 56.2 years (SD = 6.6, range: 45-75) and the majority identified themselves as female (82%). The experimental conditions did not differ in terms of age, gender, education level, subjective numeracy, health literacy, and personal experience with cancer ().
Table 1. Participant background characteristics (n = 239).
Manipulation check
Although participants perceived personalized risks as more personally relevant (M = 2.85, SD = .11) than those who received generic risks (M = 2.59, SD = 0.10), this difference was not statistically significant, t(237) = 1.75, p = .082. When looking at the two items separately, participants who received personalized risks were more likely to think that these risk estimates were made personally for them (M = 2.69, SD = 1.30) compared to those who received generic risks (M = 2.33, SD = 1.29), t(237) = 2.12, p = .035, but this was not significant after correcting for multiple comparisons. In both personalized (M = 3.02, SD = 1.18) and generic (M = 2.85, SD = 1.18) risk conditions, the way the risk estimate was being presented was perceived as equally relevant to participants, t(237) = 1.07, p = .286. Finally, participants found it moderately easy/hard to imagine themselves in the scenario (M = 2.30, SD = 1.24), but there were no difference between the personalized (M = 2.13, SD = 1.23) and generic (M = 2.44, SD = 1.24) risk condition, t(237) = 1.95, p = .053.
Effects on perceived risk and cancer-related worry (H1-H3)
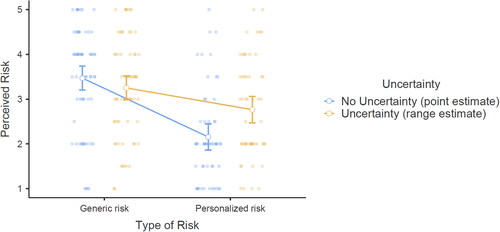
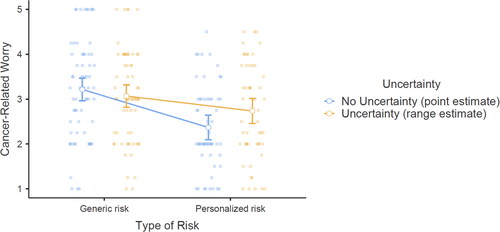
Descriptive statistics for perceived risk and cancer-related worry are presented in .
Table 2. Means and standard deviations for perceived risk, cancer-related worry, and perceived credibility for all four experimental conditions (n = 239).
The MANOVA showed a significant effect of personalization on the combined dependent variable of perceived risk and cancer-related worry (V = 0.85, F(2, 234) = 20.17, p < .001), and univariate tests showed a significant effect of risk type on perceived risk (F(1, 235) = 40.30, p < .001, partial η2 = .145) and cancer-related worry (F(1, 235) = 19.46, p < .001, partial η2 = .076). When looking at the mean scores (), participants who received personalized risk estimates reported significantly lower risk perceptions (i.e. low to moderate perceived chance of getting colon cancer) and cancer-related worry (i.e. low to moderate levels of worry about getting colon cancer) than those who received generic risk estimates (i.e. moderate levels for both perceived chance of and levels of worry about getting colon cancer). The results did not change while controlling for subjective numeracy and health literacy in the MANCOVA (V = .85, F(2, 232) = 20.01, p < .001, partial η2 = .147; effect of risk type on perceived risk, F(1, 233) = 39.95, p < .001, partial η2 = .146, and cancer-related worry, F(1, 233) = 19.40, p < .001, partial η2 = .077), nor while controlling for gender and education (all ps < .001). Thus, H1 was not supported by the data, as the opposite effect was found.
Furthermore, the MANOVA did not show a significant main effect of uncertainty communication on the two outcome variables, V = 0.99, F(2, 234) = 0.60, p = .550, and univariate tests did not show an effect of uncertainty on perceived risk (F(1, 235) = 1.20, p = .275, partial η2 = .008) and cancer-related worry (F(1, 235) = .41, p = .523, partial η2 = .003). On average, participants, who received uncertainty ranges around their risk estimate reported similar risk perceptions and levels of cancer-related worry. The results did not change while controlling for subjective numeracy and health literacy in the MANCOVA (V = .99, F(2, 232) = .95, p = .389, partial η2 = .008; effect of uncertainty on perceived risk, F(1, 233) = 1.89, p = .170, partial η2 = .008, and cancer-related worry, F(1, 233) = .63, p = .430, partial η2 = .003), nor while controlling for gender and education (all ps > .05). As such, H2 was not supported by the data.
However, the MANOVA did reveal a significant interaction effect between risk type and uncertainty on the combined dependent variables, V = .97, F(2, 234) = 4.24, p = .016, partial η2 = .035. Separate univariate analysis showed that this risk type × uncertainty interaction was significant for perceived risk (F(1, 235) = 8.45, p =.004, partial η2 = .035). Personalized risk estimates with uncertainty ranges were perceived as higher than personalized risks without uncertainty ranges (p = .004); such an interaction was not found for generic risks (p = .254). The interaction effect was non-significant for cancer-related worry (F(1, 235) = 3.69, p = .056, partial η2 = .015), although a similar trend was found: Personalized risk estimates with uncertainty ranges led to increased (but borderline significant) levels of cancer-related worry compared to personalized risk estimates without uncertainty ranges (p = .065), while there were no differences for generic risk estimates (p = .415). These results were also found while controlling for subjective numeracy and health literacy in the MANCOVA (V = .97, F(2, 232) = 4.24, p = .016, partial η2 = .035; interaction effects on perceived risk, F(1, 233) = 8.51, p =.004, partial η2 = .035, and cancer-related worry, F(1, 233) = 3.72, p = .055), and gender and education. As such, H3 was partially supported by the data. displays these interaction effects for perceived risk, and for cancer-related worry.
Mediating effect of perceived credibility (RQ1)
A two-way ANOVA showed an effect of type of risk on perceived credibility (F(1, 235) = 23.86, p < .001, partial η2 = .092, such that personalized risks were perceived as less credible (M = 2.85, SD = 1.01) than generic risks (M = 3.47, SD = 0.84). However, risk estimates with uncertainty ranges were not perceived as less credible than point risk estimates (F(1, 235) = 1.21, p = .273, partial η2 = .005), nor was there an interaction between type of risk and uncertainty on perceived credibility (F(1, 235) = 0.05, p = .824, partial η2 = .000; see for full descriptives).
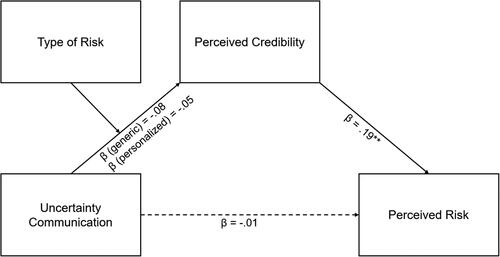
As communicating uncertainty around personalized risk estimates had an impact on perceived risk (H3), an exploratory mediated moderation analysis was conducted to explore whether this interplay could be mediated by perceived credibility (RQ1). However, the analysis did not show an overall indirect effect of uncertainty communication on perceived risk via perceived credibility (b = −0.03, SE = 0.03, β = −0.01, p = .295), and this was found for both personalized (b = −0.01, SE = 0.02, β = −0.00, p = .582) and generic risk estimates (b = −0.06, SE = 0.06, β, −0.02, p = .331). Communicating uncertainty also had no significant impact on perceived credibility (b = −0.14, SE = 0.12, β = −0.07, p = .267) and this was not different for personalized (b = −0.11, SE = 0.18, β = −0.05, p = .550) and generic risks (b = −0.17, SE = 0.17, β = −0.08, p = .321). The outcome of the mediated moderation analysis is displayed in .
Discussion
This pre-registered experimental study tested the effects of disclosing epistemic uncertainty (i.e. confidence intervals vs. point estimates) for generic and personalized cancer risk estimates on people’s psychological responses (i.e. characteristics of ambiguity aversion). Our main findings were threefold. First, contrary to our expectation (H1), people who received personalized cancer risk estimates reported significantly lower risk perceptions and cancer worry than people who received generic cancer risk estimates. Second, although we did not find an overall effect of uncertainty communication on ambiguity aversion (H2), we did find that layperson’s ambiguity aversive psychological responses to the communication of epistemic uncertainty are different for personalized and generic cancer risk information. More specifically, and as hypothesized (H3), communicating statistical uncertainty ranges around personalized risk estimates led to heightened risk perceptions, and to a certain extent higher feelings of worry; Such negative psychological effects were not found when uncertainty was being disclosed around generic, non-personalized risk estimates. Third and finally, this moderated effect of personalization was not explained by lower levels of perceived credibility (RQ1).
Our findings are in line with the assumption that the psychological effect of uncertainty communication is a highly moderated phenomenon, and may be influenced by several situational (e.g. presentation format) and individual factors (e.g. dispositional optimism or uncertainty tolerance) (Han et al. Citation2011; Han, Babrow, et al. Citation2019; van der Bles et al. Citation2019, Citation2020). Compared to those who received generic risk information, participants in our study who received personalized risks reported low to moderate risk perceptions and worry, and were to a certain extent also more likely to think that these risk estimates were made personally for them (Vromans et al. Citation2020), and were therefore possibly more motivated to process the relevant risk information more deeply and with more attention (Petty and Cacioppo Citation1986; Rimer and Kreuter Citation2006). This could lead them to engage more in deliberative processing, reflecting in moderate to high risk perceptions when taking a closer look at the interval ranges around the individualized cancer risk statistic (Lustria et al. Citation2016). Although we did not measure people’s other cognitive responses (i.e. understanding/recall of uncertainty information or accuracy of their risk perceptions), our study adds to recent insights indicating that personalized risks are processed and perceived differently than generic cancer risk information (Han, Babrow, et al. Citation2019; Vromans et al. Citation2020; Krahmer et al. Citation2022), which is important for understanding its role in shared and informed decision-making about various health outcomes (Edwards et al. Citation2013). At the same time, we must also acknowledge that risk perceptions are subjective by nature, indicating that people’s (and especially non-expert) perceptions of inaccuracies around individualized disease risk information may differ from reality and how experts perceive uncertainty around risk estimates.
The exact mechanisms that underlie people’s response to uncertainty information around personalized (and not generic) risks remain unclear. We reasoned that uncertainty associated with personalized risk estimates may be discounted or distrusted by people, hence leading to ambiguity aversive responses. However, similar to earlier studies, we did not find evidence for a potential mediating role of perceptions of credibility that could explain why people show these psychologically aversive responses to uncertainty communication for personalized cancer risk information (Han et al. Citation2011; Lipkus, Klein, and Rimer Citation2001). Although speculatively, the confidence intervals around personalized estimates could have created confusion among some participants, because they expected to receive more precise, accurate, and specific risk information. These contradictory thoughts and beliefs about expecting precise vs. receiving imprecise information could have been translated into heightened risk perception and cancer-related worry. Regardless of uncertainty was being disclosed or not, personalized risk estimates were perceived as less credible, which could also be a reason for the lower risk perceptions and affective responses (Scherer et al. Citation2013), as people also could have different (i.e. heightened) baseline levels of their personalized colon cancer risk based on the information provided in the hypothetical scenario. Underlying mechanisms that might explain the effects of epistemic uncertainty communication around personalized risks such as perceived relevance, motivated reasoning, or (conflicting) prior knowledge and beliefs should be explored further (Damman et al. Citation2017).
Importantly, one could still wonder how ‘bad’ these aversive psychological responses to uncertainty information for personalized risks really are. Although risk perceptions and cancer-related worry were higher in the uncertainty condition for personalized risks, a critical look at the descriptive statistics suggest no alarming consequences, as the mean scores were low to moderate and relatively comparable with perceptions and affective responses to generic cancer risk estimates. As suggested elsewhere, increased levels of risk perceptions and worry may also help people better understand the limitations and issues with individualized risk estimates obtained via web-based risk calculators, resulting in more deliberative and informed decision-making (Harrison et al. Citation2019). In that light, risk communicators and online tool developers should consider disclosing uncertainty information, as it may lead to more complete and informed decision-making. Future research could extend this study by investigating other cognitive, emotional, and especially behavioural outcomes. These outcomes may be, for instance, related (but not limited) to other aspects of ambiguity aversion such as understanding, perceived usefulness, satisfaction with the risk information, or treatment/screening intention (Han, Babrow, et al. Citation2019), or may focus on how people’s beliefs about the reliability of risk information relate to the objective inadequacies of personalized risk estimates they receive.
The results must be interpreted in the context of some limitations. First, we did not investigate the effects of uncertainty and personalization among different risk levels (i.e. high vs. low risk estimates), uncertainty magnitudes (i.e. comparing small vs. big confidence interval ranges), or severity levels. In the present study, risk perceptions and cancer-related worry were relatively moderate for the specific height of the risk estimate (i.e. 9% risk) that we conceptually replicated from Han et al. (Citation2011), and we could not assess whether the psychological effects arising from uncertainty communication also exist when the individualized risk estimate was high due to practical reasons (i.e. people would have used the risk calculator twice). This thus means that we cannot draw any conclusions about changes in risk perceptions (i.e. higher vs. lower) within people who received personalized risk estimates. Also, our study risk specified the probability of an averse medical event happening (i.e. risk of developing colorectal cancer), but we do not know whether participants were aware about the severity of the diagnosis. The specific impact of a medical event on a person’s life seems pivotal in reasoning about worrying for a particular risk. Therefore, for future research it is recommended that the psychological effects of epistemic uncertainty communication for personal risks is investigated for different risk levels uncertainty magnitudes, as well as manipulating the impact of risks by using diagnoses that vary in severity or impact on life.
Second, the majority of our convenience sample was female with either a medium or high education level. Although these imbalances in gender and education levels were consistent across experimental conditions, previous research on risk perception has shown differences between men and women in their estimates of risk (see for instance Xiao and McCright Citation2015); men tend to evaluate risks as smaller and less problematic than women do (van der Linden Citation2015). In addition to gender, formal education background is also often identified as a stable predictor of risk perception, where people who are having limited education background typically show increased risk perceptions compared to their counterparts (van der Linden Citation2015; Akerlof et al. Citation2013). Moreover, although our sample size closely matches with the sample size of experiment 1 from Han et al. (Citation2011), we cannot rule out the possibility that our study is somewhat underpowered. Therefore, we recommend future studies to address this issue of generalizability by attempting to examine layperson’s response to the communication of epistemic uncertainty in personalized risk information among a large nationally representative sample.
A final limitation relates to the format that was being used for conveying the risk estimate (i.e. bar chart with a percentage or percentage range). It is well-documented that percentages as risks are difficult to understand by the general public, and that other formats such as natural frequencies (i.e. 9 out of 100 people) or visual aids (i.e. icon arrays) are more suitable formats for communicating complex health risk information (Bonner et al. Citation2021; Gigerenzer et al. Citation2008; Spiegelhalter Citation2017; Fagerlin, Zikmund-Fisher, and Ubel Citation2011). Given that we aimed at conceptually replicating the experimental study of Han et al. (Citation2011), we decided to use the exact same stimulus materials. However, these materials were also limited by the lack of an experimental condition in which the point estimate is combined with the confidence intervals. As previous research has shown that representation format moderates the effects of uncertainty communication on ambiguity aversion (Han et al. Citation2012), future research is encouraged to find out how best to communicate epistemic uncertainty information in more suitable and evidence-based risk communication formats for both numerical and visual information (Recchia, Lawrence, and Freeman Citation2022; Raphael et al. Citation2020).
The findings of this experimental study have implications for risk and uncertainty communication research in an era of precision medicine. Personalized risk estimates, whether obtained via online risk calculators or offline clinical prediction models, are an increasingly common form of information being used during informed decision-making (Harrison et al. Citation2019). However, important questions remain about their accuracy and reliability, and to what extent such limitations and uncertainties need to be communicated to the people who are receiving these individualized risk estimates, and what people’s beliefs and perceptions are of those inaccuracies. Our findings show that uncertainty around personalized risks is perceived differently compared to uncertainty around generic, non-personalized risk estimates, and underline the importance of finding optimal methods for adequately communicating these uncertainties, as well as getting a better understanding of how people process and use uncertainty information around personalized disease risk information. At the same time, whether such psychological effects (i.e. heightened risk perceptions and affective responses) are truly alarming or undesirable is difficult to judge, especially considering the many different factors that are involved such as the specific disease context, its communication purpose (i.e. informing vs. persuading), the height of the risk estimate (i.e. low, medium, high risk), and the magnitude of the uncertainty ranges (Freeman Citation2019). Developers of risk prediction models or tools must therefore consider and test these aspects before deciding whether and how to disclose epistemic uncertainty information associated with individualized disease risk estimates.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data can be accessed via https://osf.io/7yhkp.
References
- Akerlof, Karen, Edward W. Maibach, Dennis Fitzgerald, Andrew Y. Cedeno, and Amanda Neuman. 2013. “Do People ‘Personally Experience’ Global Warming, and If so How, and Does It Matter?” Global Environmental Change 23 (1): 81–91. https://doi.org/10.1016/j.gloenvcha.2012.07.006.
- Albada, Akke, Margreet G. E. M. Ausems, Jozien M. Bensing, and Sandra van Dulmen. 2009. “Tailored Information about Cancer Risk and Screening: A Systematic Review.” Patient Education and Counseling 77 (2): 155–171. https://doi.org/10.1016/j.pec.2009.03.005.
- Ankersmid, Jet Wies, Sabine Siesling, Luc J. A. Strobbe, Johanna M. Meulepas, Yvonne E. A. van Riet, Noel Engels, Janine C. M. Prick, et al. 2022. “Supporting Shared Decision-Making about Surveillance after Breast Cancer with Personalized Recurrence Risk Calculations: Development of a Patient Decision Aid Using the International Patient Decision AIDS Standards Development Process in Combination with.” JMIR Cancer 8 (4): e38088. https://doi.org/10.2196/38088.
- Bansback, Nick, Madelaine Bell, Luke Spooner, Alysa Pompeo, Paul K. J. Han, and Mark Harrison. 2017. “Communicating Uncertainty in Benefits and Harms: A Review of Patient Decision Support Interventions.” The Patient 10 (3): 311–319. https://doi.org/10.1007/s40271-016-0210-z.
- Bles, Anne Marthe van der., Sander van der Linden, Alexandra L. J. Freeman, and David J. Spiegelhalter. 2020. “The Effects of Communicating Uncertainty on Public Trust in Facts and Numbers.” Proceedings of the National Academy of Sciences 117 (14): 7672–7683. https://doi.org/10.1073/pnas.1913678117.
- Bles, Anne Marthe van der., Sander van der Linden, Alexandra L. J. Freeman, James Mitchell, Ana B. Galvao, Lisa Zaval, and David J. Spiegelhalter. 2019. “Communicating Uncertainty about Facts, Numbers and Science.” Royal Society Open Science 6 (5): 181870. https://doi.org/10.1098/rsos.181870.
- Bonner, Carissa, Lyndal J. Trevena, Wolfgang Gaissmaier, Paul K. J. Han, Yasmina Okan, Elissa Ozanne, Ellen Peters, Daniëlle Timmermans, and Brian J. Zikmund-Fisher. 2021. “Current Best Practice for Presenting Probabilities in Patient Decision Aids: Fundamental Principles.” Medical Decision Making: An International Journal of the Society for Medical Decision Making 41 (7): 821–833. https://doi.org/10.1177/0272989X21996328.
- Damman, Olga C., Nina M. M. Bogaerts, Maaike J. van den Haak, and Danielle R. M. Timmermans. 2017. “How Lay People Understand and Make Sense of Personalized Disease Risk Information.” Health Expectations: An International Journal of Public Participation in Health Care and Health Policy 20 (5): 973–983. https://doi.org/10.1111/hex.12538.
- Edwards, Adrian Gk., G. Naik, H. Ahmed, Glyn Elwyn, T. Pickles, K. Hood, and R. Playle. 2013. “Personalised Risk Communication for Informed Decision Making about Taking Screening Tests.” Cochrane Database of Systematic Reviews 2: CD001865. doi:10.1002/14651858.CD001865.pub3. www.cochranelibrary.com.
- Emmons, Karen M., Mei Wong, Elaine Puleo, Neil Weinstein, Robert Fletcher, and Graham Colditz. 2004. “Tailored Computer-Based Cancer Risk Communication: Correcting Colorectal Cancer Risk Perception.” Journal of Health Communication 9 (2): 127–141. https://doi.org/10.1080/10810730490425295.
- Engelhardt, Ellen G., Arwen H. Pieterse, Paul K. J. Han, Nanny van Duijn-Bakker, Frans Cluitmans, Ed Maartense, Monique M. E. M. Bos, et al. 2017. “Disclosing the Uncertainty Associated with Prognostic Estimates in Breast Cancer: Current Practices and Patients’ Perceptions of Uncertainty.” Medical Decision Making 37 (3): 179–192. https://doi.org/10.1177/0272989X16670639.
- Fagerlin, Angela, Brian J. Zikmund-Fisher, and Peter A. Ubel. 2011. “Helping Patients Decide: Ten Steps to Better Risk Communication.” Journal of the National Cancer Institute 103 (19): 1436–1443. https://doi.org/10.1093/jnci/djr318.
- Fagerlin, Angela, Brian J. Zikmund-Fisher, Peter A. Ubel, Aleksandra Jankovic, Holly A. Derry, and Dylan M. Smith. 2007. “Measuring Numeracy without a Math Test: Development of the Subjective Numeracy Scale.” Medical Decision Making: An International Journal of the Society for Medical Decision Making 27 (5): 672–680. https://doi.org/10.1177/0272989X07304449.
- Faul, F., E. Erdfelder, A.-G. Lang, and A. Buchner. 2007. “G * Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences.” Behavior Research Methods 39 (2): 175–191. https://doi.org/10.3758/bf03193146.
- Freeman, Alexandra L. J. 2019. “How to Communicate Evidence to Patients.” Drug and Therapeutics Bulletin 57 (8): 119–124. https://doi.org/10.1136/dtb.2019.000008.
- Gigerenzer, Gerd, Wolfgang Gaissmaier, Elke Kurz-Milcke, Lisa M. Schwartz, and Steven Woloshin. 2008. “Helping Doctors and Patients Make Sense of Health Statistics.” Psychological Science in the Public Interest: A Journal of the American Psychological Society 8 (2): 53–96. https://doi.org/10.1111/j.1539-6053.2008.00033.x.
- Han, Paul K. J., Austin Babrow, Marij A. Hillen, Pål Gulbrandsen, Ellen M. Smets, and Eirik H. Ofstad. 2019. “Uncertainty in Health Care: Towards a More Systematic Program of Research.” Patient Education and Counseling 102 (10): 1756–1766. https://doi.org/10.1016/j.pec.2019.06.012.
- Han, Paul K. J., William M. P. Klein, Bill Killam, Tom Lehman, Holly Massett, and Andrew N. Freedman. 2012. “Representing Randomness in the Communication of Individualized Cancer Risk Estimates: Effects on Cancer Risk Perceptions, Worry, and Subjective Uncertainty about Risk.” Patient Education and Counseling 86 (1): 106–113. https://doi.org/10.1016/j.pec.2011.01.033.
- Han, Paul K. J., William M. P. Klein, Thomas C. Lehman, Holly Massett, Simon C. Lee, and Andrew N. Freedman. 2009. “Laypersons’ Responses to the Communication of Uncertainty regarding Cancer Risk Estimates.” Medical Decision Making: An International Journal of the Society for Medical Decision Making 29 (3): 391–403. https://doi.org/10.1177/0272989X08327396.
- Han, Paul K. J., William M. P. Klein, Tom Lehman, Bill Killam, Holly Massett, and Andrew N. Freedman. 2011. “Communication of Uncertainty regarding Individualized Cancer Risk Estimates: Effects and Influential Factors.” Medical Decision Making: An International Journal of the Society for Medical Decision Making 31 (2): 354–366. https://doi.org/10.1177/0272989X10371830.
- Han, Paul K. J., Christine Lary, Adam Black, Caitlin Gutheil, Hayley Mandeville, Jason Yahwak, and Mayuko Fukunaga. 2019. “Effects of Personalized Risk Information on Patients Referred for Lung Cancer Screening with Low-Dose CT.” Medical Decision Making: An International Journal of the Society for Medical Decision Making 39 (8): 950–961. https://doi.org/10.1177/0272989X19875966.
- Harrison, Mark, Paul K. J. Han, Borsika Rabin, Madelaine Bell, Hannah Kay, Luke Spooner, Stuart Peacock, and Nick Bansback. 2019. “Communicating Uncertainty in Cancer Prognosis: A Review of Web-Based Prognostic Tools.” Patient Education and Counseling 102 (5): 842–849. https://doi.org/10.1016/j.pec.2018.12.009.
- Hayes, A. F. 2022. Introduction to Mediation, Moderation, and Conditional Process Analysis. New York: Guilford Press.
- Hochstenbach, L. M. J., D. Determann, R. R. R. Fijten, E. J. Bloemen-Van Gurp, and R. Verwey. 2023. “Taking Shared Decision Making for Prostate Cancer to the Next Level: Requirements for a Dutch Treatment Decision Aid with Personalized Risks on Side Effects.” Internet Interventions 31: 100606. https://doi.org/10.1016/j.invent.2023.100606.
- Johnson, Branden B., and Paul Slovic. 1995. “Explaining Uncertainty in Health Risk Assessment: Effects on Risk Perception and Trust.” Risk Analysis 15 (4): 1539–6924. https://illiad.mst.edu/illiad/illiad.dll?Action=10&Form=75&Value=244723.
- Krahmer, Emiel, Steffen Pauws, Lonneke van de Poll-Franse, and Ruben Vromans. 2022. “Gepersonaliseerde Gezondheidsinformatie Communiceren.” Nederlands Tijdschrift Voor Geneeskunde 166: 1–5.
- Linden, Sander van der. 2015. “The Social-Psychological Determinants of Climate Change Risk Perceptions: Towards a Comprehensive Model.” Journal of Environmental Pstchology 41: 112–124. https://doi.org/10.1080/13504622.2015.1108391.
- Lipkus, Isaac, William Klein, Celette Sugg Skinner, and Barbara Rimer. 2005. “Breast Cancer Risk Perceptions and Breast Cancer Worry: What Predicts What?” Journal of Risk Research 8 (5): 439–452. https://doi.org/10.1080/1366987042000311018.
- Lipkus, Isaac M., William M. P. Klein, and Barbara K. Rimer. 2001. “Communicating Breast Cancer Risks to Women Using Different Formats.” Cancer Epidemiology Biomarkers and Prevention 10 (8): 895–898.
- Lustria, Mia Liza A., Juliann Cortese, Mary A. Gerend, Karla Schmitt, Ying Mai Kung, and Casey McLaughlin. 2016. “A Model of Tailoring Effects: A Randomized Controlled Trial Examining the Mechanisms of Tailoring in a Web-Based STD Screening Intervention.” Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association 35 (11): 1214–1224. https://doi.org/10.1037/hea0000399.
- Maat, Henk Pander, Marie-Louise Essink-Bot, Karlijn E. F. Leenaars, and Mirjam P. Fransen. 2014. “A Short Assessment of Health Literacy (SAHL) in The Netherlands.” BMC Public Health 14: 990. https://doi.org/10.1186/1471-2458-14-990.
- Netherlands Comprehensive Cancer Organisation (IKNL). 2020. “NKR Cijfers.” https://www.iknl.nl/nkr-cijfers.
- Petty, Richard E., and John T. Cacioppo. 1986. “The Elaboration Likelihood Model of Persuasion.” Advances in Experimental Social Psychology 19: 123–205. https://doi.org/10.1016/S0065-2601(08)60214-2.
- Raphael, D. B., N. S. Russell, J. M. Immink, P. G. Westhoff, M. C. Stenfert Kroese, M. R. Stam, L. M. Van Maurik, et al. 2020. “Risk Communication in a Patient Decision Aid for Radiotherapy in Breast Cancer: How to Deal with Uncertainty?” Breast (Edinburgh, Scotland) 51: 105–113. https://doi.org/10.1016/j.breast.2020.04.001.
- Recchia, Gabriel, Alice C. E. Lawrence, and Alexandra L. J. Freeman. 2022. “Investigating the Presentation of Uncertainty in an Icon Array: A Randomized Trial.” Pec Innovation 1: None. https://doi.org/10.1016/j.pecinn.2021.100003.
- Rimer, Barbara K., and Matthew W. Kreuter. 2006. “Advancing Tailored Health Communication: A Persuasion and Message Effects Perspective.” Journal of Communication 56 (suppl_1): S184–S201. https://doi.org/10.1111/j.1460-2466.2006.00289.x.
- Scherer, Laura D., Peter A. Ubel, Jennifer McClure, Sarah M. Greene, Sharon Hensley Alford, Lisa Holtzman, Nicole Exe, and Angela Fagerlin. 2013. “Belief in Numbers: When and Why Women Disbelieve Tailored Breast Cancer Risk Statistics.” Patient Education and Counseling 92 (2): 253–259. https://doi.org/10.1016/j.pec.2013.03.016.
- Spiegelhalter, David. 2017. “Risk and Uncertainty Communication.” Annual Review of Statistics and Its Application 4 (1): 31–60. https://doi.org/10.1146/annurev-statistics-010814-020148.
- The jamovi project. 2023. "jamovi (Version 2.3)." [Computer Software]. https://www.jamovi.org
- Trevena, Lyndal J., Carissa Bonner, Yasmina Okan, Ellen Peters, Wolfgang Gaissmaier, Paul K. J. Han, Elissa Ozanne, Danielle Timmermans, and Brian J. Zikmund-Fisher. 2021. “Current Challenges When Using Numbers in Patient Decision Aids: Advanced Concepts.” Medical Decision Making: An International Journal of the Society for Medical Decision Making 41 (7): 834–847. https://doi.org/10.1177/0272989X21996342.
- Vromans, Ruben D., S. C. Pauws, N. Bol, L. V. van de Poll-Franse, and E. J. Krahmer. 2020. “Communicating Tailored Risk Information of Cancer Treatment Side Effects: Only Words or Also Numbers?” BMC Medical Informatics and Decision Making 20 (1): 277. https://doi.org/10.1186/s12911-020-01296-7.
- Vromans, Ruben D., Mies C. H. J. van Eenbergen, Gijs Geleijnse, Steffen C. Pauws, Lonneke V. van de Poll-Franse, and Emiel J. Krahmer. 2021. “Exploring Cancer Survivor Needs and Preferences for Communicating Personalized Cancer Statistics from Registry Data: Qualitative Multimethod Study.” JMIR Cancer 7 (4): e25659. https://doi.org/10.2196/25659.
- Vromans, Ruben D., Steffen C. Pauws, Lonneke V. van de Poll-Franse, and Emiel J. Krahmer. 2022. “Effects of Comparative Information When Communicating Personalized Risks of Treatment Outcomes: An Experimental Study.” Journal of Risk Research 26 (3): 324–343. https://doi.org/10.1080/13669877.2022.2128392.
- Vromans, Ruben D., Corinne N. Tillier, Steffen C. Pauws, Henk G. Van Der Poel, Lonneke V. Van De Poll-Franse, and Emiel J. Krahmer. 2022. “Communication, Perception, and Use of Personalized Side-Effect Risks in Prostate Cancer Treatment-Decision Making: An Observational and Interview Study.” Patient Education and Counseling 105 (8): 2731–2739. https://doi.org/10.1016/j.pec.2022.04.017.
- Vromans, Ruben, S. Hommes, F. J. Clouth, D. N. N. Lo-Fo-Wong, X. A. A. M. Verbeek, L. V. van de Poll-Franse, S. Pauws, and E. J. Krahmer. 2022. “Need for Numbers: Assessing Cancer Survivors’ Needs for Personalized and Generic Statistical Information.” BMC Medical Informatics and Decision Making 22 (1): 260. https://doi.org/10.1186/s12911-022-02005-2.
- Waters, Erika A., Helen W. Sullivan, Wendy Nelson, and Bradford W. Hesse. 2009. “What is My Cancer Risk? How Internet-Based Cancer Risk Assessment Tools Communicate Individualized Risk Estimates to the Public: Content Analysis.” Journal of Medical Internet Research 11 (3): e1222. https://doi.org/10.2196/jmir.1222.
- Waters, Erika A., Neil D. Weinstein, Graham A. Colditz, and Karen Emmons. 2006. “Formats for Improving Risk Communication in Medical Tradeoff Decisions.” Journal of Health Communication 11 (2): 167–182. https://doi.org/10.1080/10810730500526695.
- Waters, Erika A., Jennifer M. Taber, Amy Mcqueen, Ashley J. Housten, L. Jamie, and Laura D. Scherer. 2020. “Translating Cancer Risk Prediction Models into Personalized Cancer Risk Assessment Tools: Stumbling Blocks and Strategies for Success.” Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology 29 (12): 2389–2394. https://doi.org/10.1158/1055-9965.EPI-20-0861.Translating.
- Witteman, Holly O., Brian J. Zikmund-Fisher, Erika A. Waters, Teresa Gavaruzzi, and Angela Fagerlin. 2011. “Risk Estimates from an Online Risk Calculator Are More Believable and Recalled Better When Expressed as Integers.” Journal of Medical Internet Research 13 (3): e54. https://doi.org/10.2196/jmir.1656.
- Xiao, Chenyang, and Aaron M. McCright. 2015. “Gender Differences in Environmental Concern: Revisiting the Institutional Trust Hypothesis in the USA.” Environment and Behavior 47 (1): 17–37. https://doi.org/10.1177/0013916513491571.
- Zikmund-Fisher, Brian J., Dylan M. Smith, Peter A. Ubel, and Angela Fagerlin. 2007. “Validation of the Subjective Numeracy Scale: Effects of Low Numeracy on Comprehension of Risk Communications and Utility Elicitations.” Medical Decision Making: An International Journal of the Society for Medical Decision Making 27 (5): 663–671. https://doi.org/10.1177/0272989X07303824.