Abstract
The causes, symptoms and treatment options for andropause have been well documented; however, not enough is known about the primary care physicians' (PCPs) knowledge in this therapeutic area. This study assesses the PCPs' awareness and knowledge of andropause in Victoria, British Columbia, Canada.
Methods. Self-administered questionnaires were developed for family physicians and general practitioners. Each questionnaire included questions in three domains: 1) General knowledge, beliefs and exposure; 2) Knowledge of diagnostic and treatment options and; 3) General demographics.
Results. A very high percentage of PCPs had heard of andropause (96.3%). Of the physicians who completed the survey, 92.6% agreed that men experience something similar to women's menopause when they age and 98.0% agreed that andropause is associated with an increased risk of osteoporosis. Almost all PCPs (91.5%) agreed that prostate cancer is a contraindication to treatment while around one-third (33.9%) agreed that breast cancer was a contraindication. Slightly more than half of physicians (57.4%) felt that they encountered obstacles to their investigation of andropause with the most prevalent complaint being a lack of access to education resources. There is a need for improved continuing medical education (CME) programmes in the Greater Victoria region to give PCPs the skills to diagnose and manage andropause with confidence.
Introduction
A rapidly growing elderly population has accompanied a recent increase in the interest towards hormonal changes for aging males. One of the health concerns in this aging demographic is low levels of free serum testosterone which have been shown to decrease with age at a rate of 2.8% per year in men aged 40–70 Citation[1]. The Canadian Society for the Study of the Aging Male estimates that 30% of men in their 50s have testosterone levels low enough to be causing or increasing the risk of erectile dysfunction, decreased libido, osteoporosis, a lack of energy and decreased muscle mass Citation[2-3]. These widely varying symptoms create difficulties for physicians making a diagnosis of andropause. The ADAM questionnaire has been developed to help aid physicians identify men at a higher risk for andropause Citation[4]. There is considerable overlap between andropause, depression and erectile dysfunction making the diagnosis difficult in some patients and a challenge for a PCP.
Low testosterone in males is most often referred to as andropause or male menopause. Even though these terms communicate the emotional and physical changes that occur, they are biologically incorrect and clinically inappropriate Citation[5]. Up until last year, androgen decline in the aging male (ADAM) or partial androgen decline in the aging male (PADAM) were the most suitable terms. Symptomatic late onset hypogonadism (SLOH) is now the accepted term for this disorder. The timing of SLOH onset is unpredictable and its manifestations are often slight and inconsistent causing diagnostic difficulties Citation[6]. Andropause doesn't exclusively occur in elderly men; a man of any age is considered to have andropause when his testosterone is below the normal range for his age group. Examples of possible causes of andropause in younger men include cancer chemotherapy, testicular trauma or a pituitary tumour.
In the past, members of the medical community have sometimes met the idea of andropause with scepticism. However, in recent years many well-designed studies and research papers have been published. To what extent the conclusions of these studies are being accepted by doctors is to be determined through assessment of the knowledge of primary care physicians (PCPs) about the presentation and treatment of this condition. Family physicians' awareness of andropause has been poorly documented and this study attempts to provide insight into this topic for the geographic area of Victoria, British Columbia, Canada. Victoria has a large aging demographic with 49% of the population over the age of 45 compared to a provincial average of 38%Citation[7]. Due to the aging population in this city andropause should be more prevalent here than in other parts of the country providing physicians in this city significant exposure to this disorder. The overall knowledge base will be analysed and possible solutions for improvement, if necessary, will be considered.
Methods
Self-administered questionnaires were developed for primary care physicians. Each questionnaire included questions in three main domains: 1) General knowledge, beliefs and exposure; 2) Knowledge of diagnostic and treatment options and; 3) General demographics. Most sections included a combination of yes or no, Likert scale and ‘check all that apply’ formats of questions. The questionnaires were reviewed by urologists, primary care physicians and statisticians. The review indicated that all known important factors and topics were included and that the questions were easily understood and answered.
Potential subjects for this survey were the 565 family physicians and general practitioners in the Victoria Physicians and Surgeons Directory. In order to generate a random sample group, all of the physicians in the directory were numbered and Microsoft Excel was used to generate a set of 125 random integers in the range of 1 to 565. Each number that was produced was matched back to a specific physician and the list of 125 physicians was complied. The surveys along with instructions were left with the selected PCPs' secretaries and completed surveys were requested to be returned by fax.
Statistical analysis of the quantitative data was carried out by the means of SPSS for Windows (version 13). Frequency distribution of variables was displayed and the appropriate tables and figures were produced. All relationships were determined to be statistically significant with a p value of less than 0.05.
Results
Questionnaires were returned by 84 physicians, a response rate of 67%. Results were accurate to within 9.8% for physician data, 95% of the time.
General knowledge, beliefs and exposure
The familiarity with different terms used to describe the condition of low testosterone in men was widely varying. A very high percentage of physicians had heard of male menopause (97.6%) and andropause (96.3%). The next two most recognized terms were ADAM (50.8%) and PADAM (9.8%). There was a significant difference in prior knowledge of these two terms despite their similarity. Only 3.3% of physicians had encountered Symptomatic Late Onset Hypogonadism (SLOH) previously most likely due to the recent introduction of this term.
Of the physicians surveyed, 92.6% correctly agreed that men experience something similar to women's menopause when they age while 63.3% incorrectly agreed that andropause is similar in its natural history to female menopause. Few physicians correctly responded to the question about the age of onset of andropause with only 21.3% responding that there was no predictable age of onset. Most answered that the symptoms manifest themselves in specific age groups: 40–49 (31.1%), 50–59 (34.4%) and 60–69 (13.1%).
The vast majority of doctors agreed with the statements: ‘andropause is a real medical condition and has negative long-term health effects’ and ‘there is a need to raise the awareness of andropause amongst physicians and the general population’, 94.1% and 91.4% respectively. There was significant agreement (79.2%), with the statement ‘a change in lifestyle can reduce the symptoms of andropause.’
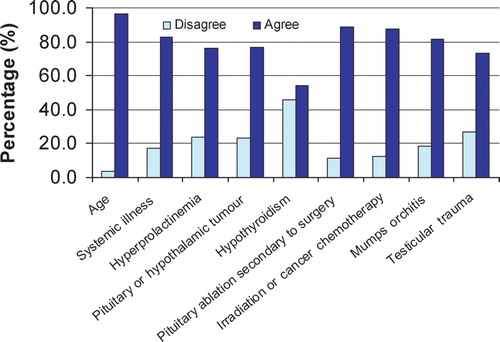
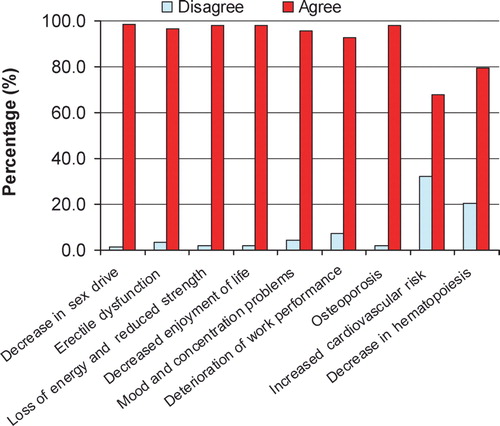
Most physicians agreed with the accepted causes and symptoms of andropause ( and ). The lowest levels of agreement were for hypothyroidism being a possible cause of andropause and an increased risk of cardiovascular disease being associated with andropause.
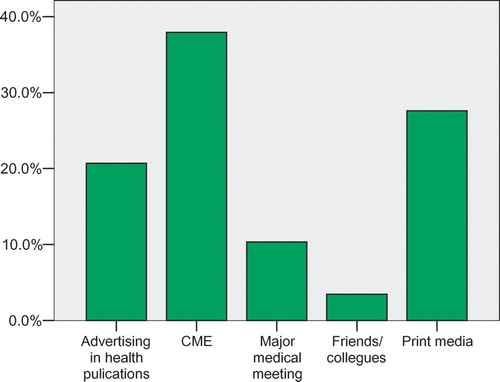
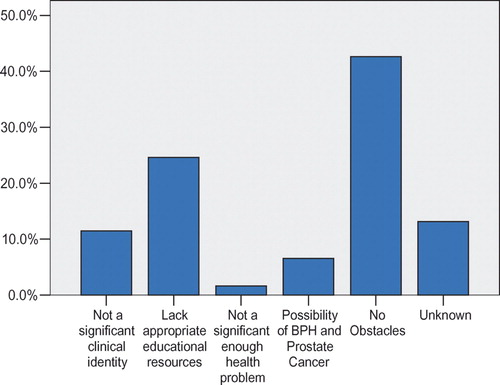
Most doctors first encountered the term andropause at Continuing Medical Education (CME) meetings (). Unfortunately, many doctors felt that they had obstacles in dealing with andropause in their practice with the most prevalent obstacle being a lack of appropriate educational resources ().
Demographics
Of the physicians sampled, 71.4% were male and 28.6% were female. The means and standard deviations were 49.6 ± 8.4 for the age of the physician and 21.4 ± 8.8 for the number of years practicing medicine. No statistically significant relationships could be determined between gender, age or number of years practising medicine and the knowledge indicators. The awareness of andropause in PCPs between the regions was compared based on the knowledge of the causes, the symptoms, the treatment options, the biochemical tests and the contraindications. No statistically significant relationships could be found between the different geographic areas.
Knowledge of treatment and diagnostic options
Almost all physicians agreed that ‘andropause is treatable’ (98.2%) and that ‘andropause left untreated can have an impact on a patient's quality of life’ (97.5%). On the other hand, the responses to the question about appropriate length of testosterone treatment required to improve the patient's quality of life were widely varying ().
Table I. Duration of testosterone treatment to improve the patient's quality of life.
Almost all PCPs (96.7%) felt that andropause should be treated, and either referred or treated patients themselves. The majority (70.5%) of physicians treated patients themselves (). There was a positive correlation 0.267 (p = 0.038) between physicians treating patients themselves and answering that they have no obstacles to their investigation of andropause.
Table II. Referral of patients presenting with symptoms of andropause.
Before treatment is initiated it is vital that the necessary criteria be fulfilled for an effective and safe treatment. Most physicians (76.3%) responded that both symptoms and biochemical tests should indicate andropause before initiating treatment. Another important step for the safe administration of hormone replacement therapy (HRT) is ensuring that no contraindications are present. The strongest contraindication to the treatment of andropause, prostate carcinoma, had almost all physicians (91.5%) agree that it was a reason to refrain from initiating therapy. Prostate obstruction/benign prostatic hyperplasia (BPH) (55.9%) and urinary retention (39.7%) were also recognized by physicians as contraindications to treatment. A lower proportion recognized breast cancer (33.9%) and a family history of prostate cancer (19.1%) as contraindications.
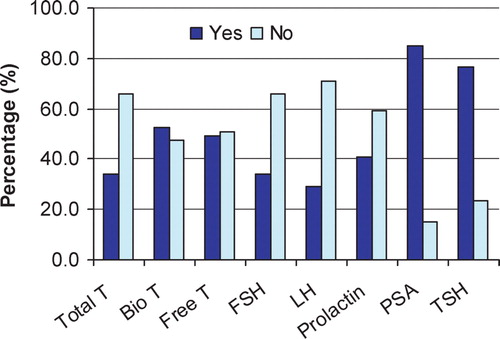
There was a large difference between the utilization rates of the different biochemical tests (). Bioavailable testosterone (Bio T), free testosterone (Free T) and total serum testosterone (Total T) were the tests used to analyse testosterone levels. Almost all physicians (98.3%) used at least one of these tests. The combined use of the different tests was analysed by bivarate correlation analysis and some tests were discovered to be significantly correlated. The use of FSH and LH (0.888, p < 0.01), FSH and prolactin (0.573, p < 0.01), and prolactin and LH (0.616, p < 0.01), were all strongly positively correlated. FSH, LH and prolactin tests are all used in the detection of secondary hypogonadism. Even though the majority of physicians did not use these three tests, these correlations show that physicians that did use these tests used them all appropriately.
The efficient use of these biochemical tests is important. 3.4% of family physicians ordered tests for andropause at routine annual physicals and 88.1% ordered biochemical tests when symptoms of andropause were present. Many physicians (83.1%) ordered tests when low libido or ED were present while significantly fewer (27.6%) ordered tests when the patient had a history of testicular surgery, infection or mumps orchitis.
Of the four main methods of supplementing testosterone, three were very well recognized: intramuscular injections (84.2%), topical gels (83.1%) and oral capsules (86.4%). There was less familiarity among family physicians with transdermal patch (57.6%).
Discussion
Our study concentrated on the level of knowledge and awareness of primary care physicians in Victoria, British Columbia. An extensive search including PubMed did not yield any previous publications specifically about PCPs' knowledge of andropause in North America. However, one article from Illinois, USA dealt with the knowledge and perceptions of the general public and health care professionals towards andropause Citation[8]. An Angus Reid Group Survey of family and general practitioners in Canada in 1999 was the only source of PCPs' awareness about andropause Citation[9]. This survey consisted of a random sample of 200 primary care physicians from across Canada. Our research study is not only examining the change in family physicians' perceptions and knowledge about andropause but also examining previously unexplored areas of PCPs' knowledge. Improved treatment methods and better diagnostic options have increased the ability of physicians to treat this condition effectively and safely. Since many family physicians undergo the treatment of andropause themselves, their knowledge and understanding of the condition is vital for the proper and safe treatment of patients. Our survey's results give a detailed overview of PCPs' knowledge in our specific geographic region.
The first term used to describe the condition of low testosterone in males, male menopause, has led many physicians to make incorrect assumptions about SLOH. In comparison to female menopause where there is an abrupt deficiency of the hormone estrogen, males suffer from a gradual decline in testosterone levels with symptoms manifesting themselves at no specific age and appearing as early as 40 years old Citation[10]. Only 21.3% of primary care physicians responded that andropause has no predictable age of onset and 63.3% incorrectly agreed that andropause is similar in its natural history to female menopause. Currently, there is a very significant gap between the awareness of the terms SLOH (3.3%) and male menopause (97.6%). These misconceptions show the necessity for the increased use and further propagation of a more clinically appropriate term such as SLOH.
In spite of these differences there are similarities between SLOH and female menopause. Depending on the extent of testosterone deficiency, men can exhibit similar signs and symptoms to menopausal women Citation[11]. Almost all of the PCPs surveyed agreed that men experience something similar to female menopause when they age and that andropause can affect the quality of a man's life as much as menopause can affect a woman's life.
Practically all physicians agreed that andropause is treatable but awareness of diagnostic criteria and methods was not unanimous. For the safe use of testosterone replacement therapy (TRT) appropriate steps must be taken before treatment is initiated. The International Society for the Study of the Aging Male (ISSAM) and the International Society of Andrology (ISA) recommends that a clear indication based on a clinical picture together with biochemical evidence of low serum testosterone should exist prior to the initiation of testosterone substitution Citation[12]. Most physicians (76.3%) understood these criteria must be met prior to treatment.
PCPs clearly realized the importance of undertaking serum testosterone tests but many did not understand which tests are most reliable. Several different testosterone tests for measuring serum testosterone exist which have widely varying levels of accuracy. Bioavailable testosterone is the most accurate test for the biochemical assessment of andropause Citation[13]. This test is available in British Columbia at no cost to the patient yet not all physicians used this test. A substantial percentage of PCPs used the measurement of free testosterone by radioimmunoassay in spite of this test being unreliable and not recommended for the diagnosis of andropause Citation[13]. A third of family physicians used the total testosterone test which is not very accurate, especially in older adults and the obese Citation[13]. Biochemical assessments other than serum testosterone tests need to be completed prior to initiation of TRT. If treatment is being considered, Little (2004) recommends that a complete endocrine profile should be undertaken, including thyroid-stimulating hormone (TSH), LH, FSH, and prolactin Citation[14]. Less than half of physicians in our sample used tests for LH, FSH and prolactin. In addition to these tests prostate specific antigen (PSA) levels should be assessed since PSA can be an indicator for the presence of early prostate cancer; almost all PCPs understood the importance of this test.
After the symptoms and biochemical tests indicate andropause, there must be an absence of contraindications; the ISA and ISSAM considered both breast and prostate cancer absolute contraindications to testosterone treatment.12 The family physicians were very aware of prostate carcinoma being a contraindication but this was not the case for breast cancer with only 33.9% recognizing it as a contraindication to treatment. Even though breast cancer is rare in males it should still be understood as a contraindication. Severe BPH and lower urinary tract symptoms were also recognized by the ISSAM as contraindications to treatment while moderate obstruction being a relative contraindication Citation[12]. Only half of PCPs recognized these two conditions as contraindications.
The knowledge of different treatment methods was high, especially for oral capsules, topical gels and intramuscular injections. This high level of awareness is probably due to a combination of advertising in health care publications and pharmaceutical company representatives detailing physicians. However, less than half of the PCPs agreed that testosterone supplementation in the treatment of andropause is life long. The treatment of andropause is generally for life Citation[11] and knowledge of this fact is important for physicians to understand and discuss with their patients for optimal outcomes.
In comparison to our findings, the Angus Reid Group Citation[9] in 1999 recorded significantly lower levels of awareness among PCPs in Canada: 78% indicated that men may experience something similar to female menopause when they age, compared to 92.6% of our respondents. In addition, 71% of the family physicians in Canada in the Angus Reid Survey agreed that andropause can affect the quality of a man's life as much as menopause can affect a woman's life, compared to 94.2% in our survey. More specific questions about the signs and symptoms of andropause had even higher differences between the two studies. Canadian PCPs had a small percentage agree (29%) that andropause was associated with an increased cardiovascular risk while 67.7% of physicians in our study agreed with this association. The most significant increase in the awareness of family physicians was the association of osteoporosis with andropause; less than half of Canadian PCPs (44%) agreed that there was an association while 98% of our respondents agreed. Overall there was a significantly higher level of knowledge about andropause in PCPs practising in Victoria in 2005 compared to PCPs practising in Canada in 1999.
In spite of this increase in awareness about andropause, misconceptions still existed among PCPs in Victoria as shown in this study. Physicians responded that the two most prevalent obstacles to their investigation of andropause were a belief that andropause was not a significant clinical identity and a lack of appropriate educational resources. Since better educational programmes could address both of these issues, improved CME programmes specifically designed to focus on these unmet needs could increase physicians' overall awareness of andropause.
The PCPs' overall awareness of andropause was satisfactory but there were obvious gaps in the depth of knowledge and understanding of the management of this condition. The comparison of our study and the Angus Reid Group Survey shows that advances in PCPs' perceptions about andropause have been occurring. However, in order to overcome the current misconceptions there is a need for improved CME programmes in the Greater Victoria region to give PCPs the skills to diagnose and manage andropause with confidence.
Acknowledgement
This study was supported by Solvay Pharma Inc.
References
- Feldman H A, Longcope C, Derby C A, et al. Age trends in the level of serum testosterone and other hormones in middle-aged men: Longitudinal results from the Massachusetts Male Aging Society. J Clin Endocrinol Metab 2002; 87: 589–598
- Canadian Society for the Study of the Aging Male. About andropause: The role of testosterone, http://www.andropausesociety.ca/roleoftron.htm
- Kaiser F E, Viosca S P, Morley J E, et al. Impotence and aging: Clinical and hormonal factors. J Am Geriatr Soc 1988; 36: 511–519
- Morley J E, Charlton E, Patrick P, et al. Validation of screening questionnaire for androgen deficiency in aging male. Metabolism: Clin Exper 2000; 49: 1239–1242
- Morales A, Lunenfeld B. Investigation, treatment and monitoring of late-onset hypogonadism in males. The Aging Male 2002; 5: 74–86
- Morales A, Heaton J P, Carson C C. Andropause: A misnomer for a true clinical identity. J Urol 2000; 163(3)705–712
- The Government of British Columbia Statistics. 2001 Census Profile, http://www.bcstats.gov.bc.ca/data/cen01/profiles/csd_txt.htm
- Anderson J K, Faulkner S, Cranor C, et al. Andropause: Knowledge and perceptions among general public and health care professionals. J Gerontol A Biol Sci Med Sci 2002; 57(12)M793–M796
- Angus Reid Group Inc. Physicians recognized male ‘andropause’ similar to female's menopause, http://www.ipsos-na.com/news/pressrelease.cfm?id=730. Accessed: Ipsos-Reid Canada Polls and Research: www.ipsos.ca
- WHO Fact Sheet No. 135. September, 1998
- Morales A. Andropause (or symptomatic late-onset hypogonadism): Facts, fiction and controversies. The Aging Male 2004; 7: 297–303
- Nieschlag E, Swerdloff R, Behre H M, et al. Investigation, treatment and monitoring of late-onset hypogonadism in males. The Aging Male 2005; 8(2)56–58
- Tremblay R. Measurement of testosterone. Mechanisms in andropause, J Bain. Mechanisms in Medicine Inc., Toronto 2003; 42–48
- Little D. Andropause: Identifying, treating, and following the patient. Geriatrics and Aging Nov/Dec, 2004; 7(10)13–16