Abstract
Objective: To conduct a systematic review and Meta-analysis of the literature on the efficacy and safety of B-TURP versus HoLEP for the treatment of benign prostatic hyperplasia (BPH) in terms of demographic and clinical baseline characteristics, peri-operative variables, and postoperative outcomes and complications.
Methods: Trials comparing B-TURP and HoLEP were identified systematically using Pubmed, Embase, CNKI, Web of Science and the Cochrane Library. Primary outcomes were the peak urinary flow rate (Qmax), post-void residual volume (PVR) and international prostate symptom score (IPSS). Secondary outcomes were operation time, irrigation duration, catheterization duration, resected tissue and complications.
Results: Four trials assessing B-TURP and HoLEP were considered eligible for Meta-analysis, including three randomized controlled trials (RCTs) and one retrospective study. There was no statistically significant difference between B-TURP and HoLEP in terms of Qmax, IPSS, PVR at 3–6 months follow-up, operation duration, catheterization duration, resected tissue and complications (p > 0.05). HoLEP was associated with a significantly shorter irrigation time as compared with B-TURP (p < 0.05).
Conclusion: Both B-TURP and HoLEP are safe and minimally invasive techniques that are similar in terms of symptomatic relief, although these findings need further validation in larger RCTs involving larger numbers of patients and over a longer follow-up duration for B-TURP or HoLEP before a new gold standard procedure emerges for surgical treatment of BPH.
Introduction
Benign prostatic hyperplasia (BPH) is the major etiology of lower urinary tract symptoms in men older than 50 years [Citation1]. Sex hormones and metabolic syndrome also have an impact on BPH and LUTS [Citation2–5]. Transurethral resection of the prostate (TURP) remains the “‘gold standard” surgical treatment for BPH-related bladder outlet obstruction [Citation6]. Ample evidence has supported its therapeutic efficacy in improving urinary flow rates and alleviating obstructive voiding symptoms, offering an 85–90% success rate [Citation7]. Nevertheless, 15–20% patients who undergo TURP develop significant complications such as bleeding urine, transurethral resection syndrome (TURS), bladder neck stricture, incontinence or retrograde ejaculation, and 10–15% patients require a second intervention within 10 years [Citation8,Citation9]. In recent years, several alternative techniques have been reported for minimizing these adverse effects.
One of the alternatives is bipolar TURP (B-TURP) in saline (TURis). In this technique, electricity runs between an active and a passive electrode, converting the irrigation solution (i.e. physiologic saline) into a plasma layer that disintegrates tissue on contact [Citation10]. The major advantage of bipolar energy systems in contrast to mono-polar systems such as TURP is the use of saline as irrigation fluid, thus eliminating the risk of TUR syndrome. There are minor technical differences in the various bipolar devices with respect to the type and arrangement of the electrodes, which have led to the use of different terminologies such as bipolar TURP, plasma kinetic resection, plasma kinetic vaporization and TUR in saline [Citation11].
Another alternative is holmium laser resection of the prostate (HoLRP), which was first reported in 1995 by Chun and Gilling and their coworkers [Citation12,Citation13]. Combined with transurethral tissue morcellation, it evolved into holmium laser enucleation of the prostate (HoLEP). Clinical experience since then has shown that HoLEP offers an efficient alternative to TURP [Citation14–16]. Holmium laser has shown potential therapeutic advantages for BPH, especially for the treatment of a large prostate gland.
Both B-TURP and HoLEP have many more advantages than TURP. So many authors believe that both of them are promising procedures and would replace TURP. We conducted a systematic review and Meta-analysis of the literature on the efficacy and safety of B-TURP versus HoLEP for the treatment of BPH patients in terms of demographic and clinical baseline characteristics, peri-operative variables, and postoperative outcomes and complications.
Methods
Objectives, search strategies, study selection criteria, and methods for determining eligibility, abstraction and study quality assessment were defined. Two independent reviewers completed either step or resolved disagreements by consensus.
Literature search
A systematic review of the literature was performed to identify articles published up to 1 December 2016 on the management of symptomatic prostatic obstruction. We conducted a systematic search of the electronic databases, including Pubmed, EMBASE, Web of Science, China National Knowledge Infrastructure (CNKI) and the Cochrane Library, using the terms: holmium laser enucleation (or HoLEP), bipolar transurethral resection (TUR), bipolar TURP, plasma kinetic resection, plasma kinetic vaporization and TUR in saline, the prostate. No regional, publication status was set, and language restrictions were set in English and Chinese. In addition, a full manual search of the references in each relevant article was also conducted. These search strategies were performed iteratively until no new potential citations could be found on review of the reference lists of retrieved articles.
Studies election, inclusion criteria and exclusion criteria
The reference lists of all traced articles and general reviews of this topic were examined manually, with reviews and commentaries excluded. Studies were included if they: (1) contained patients with symptomatic prostatic obstruction at baseline; (2) compared B-TURP with HoLEP and (3) reported on at least one outcome of interest mentioned below. Studies were excluded if: (1) the inclusion criteria were not met, (2) no outcomes of interest were reported or it was impossible to calculate or extrapolate the necessary data for either B-TURP with HoLEP from the published results.
Data extraction
Two reviewers (Xiaoqiang Qian and Hailong Liu) extracted data independently and reached consensus on all items. The following variables were recorded: the first author, journal and year of publication, study design, number of patients who underwent B-TURP or HoLEP, age, international prostate symptom score (IPSS), quality of life (QoL), prostate volume, post-void residual volume (PVR), prostate-specific antigen (PSA), International Index of Erectile Function-5 (IIEF-5), peak urinary flow rate (Qmax), duration of operation, bladder irrigation, resected weight, catheterization duration, hospital stay, and the overall complications including blood transfusion, TUR syndrome, re-catheterization, transitory urge incontinence, stress incontinence, urinary tract infection (UTI), retrograde ejaculation and urethral stricture. If necessary, the primary authors were contacted to retrieve further information.
Assessment of study quality
The methodological quality of the studies included in the Meta-analysis was scored using the Jadad Composite Scale (). This was a five-point scale, with low-quality studies having a score of 2 or less and high-quality studies having a score of at least 3.
Table 1. Jadad score calculation for in included studies.
Data analysis
The present Meta-analysis was performed according to the recommendations of the Cochrane Collaboration and the Quality of Reporting of Meta-Analyses guidelines [Citation17]. The weighted mean differences (WMDs) and the odds ratios (OR) were used to compare continuous and dichotomous variables, respectively. All outcomes were reported with 95% confidence intervals (CI). For continuous variables, we calculated the difference in mean values and the 95% CI. This method required that the study reported the standard errors of the mean, the standard deviations or the CI. For dichotomous variables derived from contingency tables, the OR and 95% CI were computed. An OR significantly <1 favored B-TURP, whereas an OR significantly >1 favored HoLEP. All p values are two-tailed with a significant level at 0.05.
A fixed-effects Meta-analysis was performed, and the quantity of heterogeneity was assessed using X2 and I2 statistics with significance set at p < 0.05 providing evidence of significant heterogeneity. For outcomes detected with higher values of I2 and the X2 statistic signified increasing levels of inconsistency between studies and significant inter-study heterogeneity, then a random-effects Meta-analysis model was adopted. Because the quantity of the manuscripts (only four manuscripts) was very few, we did not carry on the funnel plot analysis. Data analysis was performed by using RevMan version 5.1 (The Nordic Cochrane Centre, The Cochrane Collaboration, 2011). And the incidence of adverse events was analyzed using Pearson’s X2-test or Fisher exact test by using SPSS® statistical software, version 18.0.1 (SPSS, Armonk, NY) for Windows®. A p values < 0.05 was considered to be statistically significant.
Results
Characteristics of the eligible studies
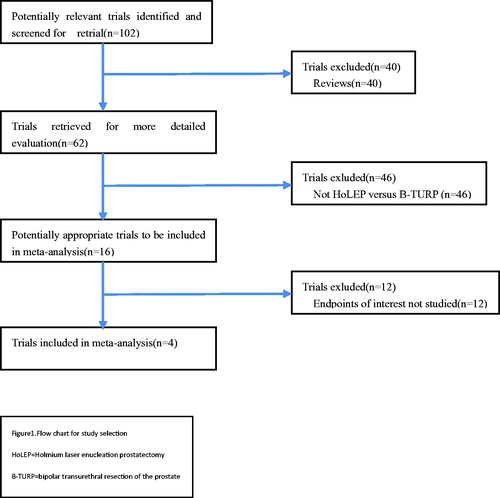
A total of 102 potentially relevant trials were identified and screened for retrieval. Of them, 40 reviews were excluded, and the remaining 62 trials were retrieved for more detailed evaluation. Among them, 46 trials were excluded because they did not involve the comparison between HoLEP and B-TURP. The remaining 16 potentially appropriate trials were further evaluated. After reading the full texts, 12 trials were excluded for no endpoints of interest studied. So in the end, four trials assessing B-TURP versus HoLEP were considered suitable for Meta-analysis including three randomized controlled trials (RCTs) and one retrospective study (). We used the Jadad composite scale to assess the quality of the four studies included in our Meta-analysis and found that the three RCTs studies [Citation18–20] scored 3, and the retrospective study [Citation21] scored 0.
Figure 1. Flow chart for study selection. HoLEP: holmium laser enucleation prostatectomy; B-TURP: bipolar transurethral resection of the prostate.
Also, the number of patients, age, prostate volume, PSA level, and preoperative estimates of baseline Qmax, PVR, QoL, IPSS and IIEF-5 of B-TURP versus HoLEP, and follow-up duration were extracted individually from each study and listed in .
Table 2. Baseline characteristics of the included studies.
Outcomes of postoperative efficacy variables including Qmax, PVR and IPSS
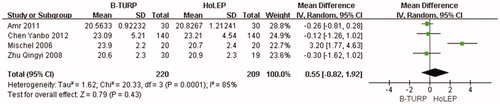
Qmax
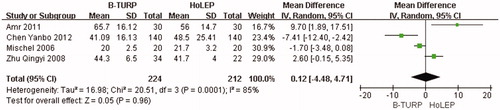
No significant difference was observed in the pooled data between B-TURP and HoLEP about Qmax (WMD: 0.55; 95% CI, −0.8 2 ∼1.92; p = 0.43) during the postoperative 3–6 months follow-up period ().
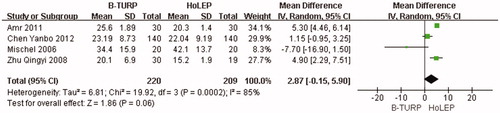
PVR
There was no significant difference in PVR between B-TURP and HoLEP (WMD: 2.87; 95% CI, −0.1 5 ∼5.90; p = 0.06) during the postoperative 3–6 months follow-up period ().
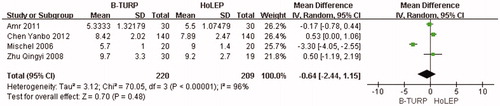
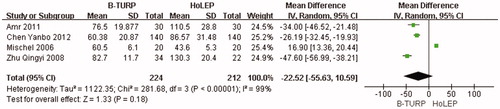
Outcomes of peri-operative variables
Operation duration
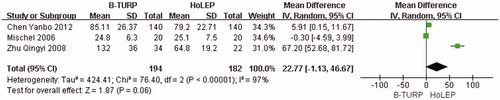
The pooled data from the four studies did not show significant difference in operation duration between B-TURP and HoLEP (WMD: −22.52; 95% CI, −55.6 3 ∼10.59; p = 0.18) in the peri-operative variables ().
Catheterization duration
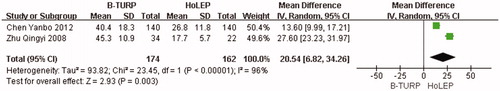
There was no significant difference in catheterization duration between B-TURP and HoLEP (WMD: 22.77; 95% CI, −1.1 3 ∼46.67; p = 0.06) in the peri-operative variables ().
Irrigation time
There was significant difference in irrigation time between B-TURP and HoLEP (WMD: 20.54; 95% CI, 6.8 2 ∼34.26; p = 0.003) in the peri-operative variables. The irrigation time in HoLEP group was significantly shorter (p < 0.01) ().
Outcomes and complications
The table shows the postoperative adverse events. There was no statistically significant difference in blood transfusion, reoperation, re-catheterization, incontinence and UTI between B-TURP and HoLEP groups ().
Table 3. The postoperative adverse events.
Discussion
BPH-related voiding symptoms are not uncommon, medicines as alpha-blocker, 5α-reductase inhibitors may alleviate it, but endoscopic TUR of the obstructing tissue remains the “gold standard” [Citation22,Citation23]. However, TURS, prostate membrane perforation, bleeding and other morbidities are likely to occur after TURP [Citation24,Citation25]. In recent years, several techniques, especially B-TURP and HoLEP, have shown promise in replacing TURP as the standard procedure for the treatment of BPH [Citation26–29].
We named B-TURP for different terminologies such as bipolar TURP, plasma kinetic resection, plasma kinetic vaporization and TUR in saline. B-TURP is one of the most recent advances in TUR surgery. With the bipolar device, there is no need to learn new skills to perform the operation when the operator is proficient in standard TURP [Citation30]. Like other bipolar systems, the TURis system allows coagulation of most small venous vessels during the resection. Due to the excellent visualization and a smaller resection loop, an experienced operator should have less capsular perforation. Therefore, irrigation fluid absorption can be greatly reduced, thus avoiding TURS. The most significant feature of the bipolar TURis system is its reduced effect on serum sodium levels due to less fluid absorption [Citation31]. These data suggest that the key advantage of the bipolar TURis system is less fluid absorption during surgery. The present study shows that the bipolar technique markedly reduced surgical hemorrhage, which might be just as important. B-TURP reduced the overall peri-operative and total surgical bleeding by 34% [Citation32]. Obturator nerve reflex (ONR) was less mentioned in bipolar system research. In the study by Miki et al. [Citation33] and Shiozawa et al. [Citation34], no ONR was observed in patients who had undergone TURis. It could also allow earlier removal of the catheter and earlier discharge from hospital [Citation35].
HoLEP is another promising technique. The holmium laser is a pulsed solid state laser, with a wave length of 2140 nm. This wavelength is strongly absorbed by water, making it ideal for safe use in an aqueous environment [Citation36]. It is reported [Citation37] that HoLEP is safe and effective in the surgical management of BPH, with the advantage of reduced intra-operative hemorrhage and peri-operative morbidity. Another Meta-analysis [Citation38] showed that HoLEP is as effective as TURP in improving subjective symptoms and urodynamic measurements at 6 and 12 months after treatment. Clinically, HoLEP seems superior to B-TURP in terms of blood loss, probably due to the hemostatic nature of the holmium wavelength. However, a report [Citation39] criticized HoLEP for its long operation duration, a steep learning curve and higher cost, ultimately reporting in favor of B-TURP. It is estimated that a trainee has to perform 20–30 cases on moderately sized glands (50 ml) before consistently reproducing good outcome [Citation40]. There may be two reasons to explain the mean longer duration of HoLEP. First, it requires additional time for fragmentation of the prostatic lobes into pieces small enough to be evacuated through the resectoscope sheath. However, a significant decrease in operation duration could be achieved by using a mechanical soft tissue morcellator. Second, more tissue are resected with HoLEP. In some recent series of studies that include large glands up to 100 g, the resected weight with HoLEP is much greater, and closer to that retrieved at open surgery.
Our Meta-analysis also shows that only two Chinese manuscripts [Citation20,Citation21] report that the irrigation time of HoLEP is significantly shorter than that of B-TURP, and the other two western manuscripts [Citation18,Citation19] do not mention the difference. It is perhaps for the excellent hemostatic characteristics of holmium, which is similar to the other report [Citation41]. Another reason may be that Caucasians have better coagulation function as compared with Asians. There are only three manuscripts [Citation19–21] reporting the catheterization time, showing that it varies greatly from about 24 to 120 h between different groups. The reason may be related to the habit of the operators. But there is no difference in blood transfusion, reoperation, catheterization of the postoperative complications between the two groups (p > 0.05). Nevertheless, there was severe heterogeneity for the analysis between studies. Consequently, we should interpret the pool result prudently.
Pooled analysis of the literature shows that the difference in operation duration between B-TURP and HoLEP is influenced mainly by the Mischel group [Citation19] who performed plasma kinetic enucleation of the prostate. With this study excluded, the operation time of B-TURP would be much shorter than that of HoLEP. Perhaps the morcellation in HoLEP is the main reason. It is generally thought that the resected tissue in HoLEP ought to be more than B-TURP. But in our Meta-analysis, we did not find significant difference between them (p > 0.05), regardless of different ages and prostate volumes among the four researches [Citation42]. The resection ratio is about 55% in both groups. Chen group [Citation20] reported that HoLEP could resect about 86% of the prostate volume; Amr group [Citation18] reported that B-TURP could resect about 81% of the prostate volume; Zhu [Citation21] and Mischel [Citation19] group reported that B-TURP or HoLEP could resect about 40% of the prostate volume. So the experience and habit of the operator are very important factors. Both B-TURP and HoLEP can get the similar resection ratio. The reoperation, re-catheterization, incontinence and UTI of the postoperative complications are similar between the two groups (p > 0.05). There is no difference in the efficacy in terms of IPSS, Qmax and PVR after 3–6 months follow-up (p > 0.05). But no data after more than 5–10 years follow-up are available in this Meta-analysis.
In conclusion, B-TURP and HoLEP are both safe and minimally invasive techniques that are similar in terms of symptomatic relief. Nevertheless, the conclusions from this study remain somewhat limited by the short follow-up periods, small sample sizes and lack of evaluation on complications such as erectile dysfunction [Citation5]. The findings reported in this Meta-analysis need further validation in larger RCTs involving larger numbers of patients and over a longer follow-up duration for B-TURP or HoLEP before a new gold standard procedure emerges for surgical treatment of BPH.
Declaration of interest
The authors have no conflicts of interest to declare in relation to this article.
Sponsored by Shanghai Municipal Planning Commission [No. 201540081], Shanghai Natural Science Foundation [No. 17ZR1417300], Shanghai Science and Technology Commission Fund [No. 14430720800] and NSFC Fund [No. 81570684].
References
- Wong SY, Woo J, Leung JC, et al. Depressive symptoms and lifestyle factors as risk factors of lower urinary tract symptoms in southern Chinese men: a prospective study. Aging Male 2010;13:113–9.
- Asiedu B, Anang Y, Nyarko A, et al. The role of sex steroid hormones in benign prostatic hyperplasia. Aging Male 2017;13:1–6; doi:10.1080/13685538.2016.1272101. [Epub ahead of print]
- Kaplan SA, O'Neill E, Lowe R, et al. Prevalence of low testosterone in aging men with benign prostatic hyperplasia: data from the Proscar Long-term Efficacy and Safety Study (PLESS). Aging Male 2013;16:48–51.
- Nakamura M, Fujimura T, Nagata M, et al. Association between lower urinary tract symptoms and sexual dysfunction assessed using the core lower urinary tract symptom score and International Index of Erectile Function-5 questionnaires. Aging Male 2012;15:111–4.
- Aktas BK, Gokkaya CS, Bulut S, et al. Impact of metabolic syndrome on erectile dysfunction and lower urinary tract symptoms in benign prostatic hyperplasia patients. Aging Male 2011;14:48–52.
- Wasson JH, Reda DJ, Bruskewitz RC, et al. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med 1995;332:75–9.
- Holtgrewe HL, Mebust WK, Dowd JB, et al. Transurethral prostatectomy: practice aspects of the dominant operation in American urology. J Urol 1989;141:248–53.
- Dunsmuir WD, Emberton M. National Prostatectomy Audit Steering Group. There is significant sexual dysfunction following TURP. Br J Urol 1996;77:39–40 (Abstract)
- Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. Cooperative study of 13 participating institutions evaluating 3885 patients. J Urol 1989;141:243–7.
- Wendt-Nordahl G, Häcker A, Reich O, et al. The vista system: a new bipolar resection device for endourological procedures: comparison with conventional resectoscope. Eur Urol 2004;46:586–90.
- Rassweiler J, Schulze M, Stock C, et al. Bipolar transurethral resection of the prostate technical modifications and early clinical experience. Minim Invasive Ther Allied Technol 2007;16:11–21
- Chun SS, Razvi HA, Denstedt JD. Laser prostatectomy with the holmium: YAG laser. Tech Urol 1995;1:217–21.
- Gilling GJ, Cass CB, Malcolm AR, Fraundorfer MR. Combination holmium and Nd:YAG laser ablation of the prostate: initial clinical experience. J Endourol 1995;9:151–3.
- Gilling PJ, Mackey M, Cresswell M, et al. Holmium laser versus transurethral resection of the prostate: a randomized prospective trial with 1-year follow-up. J Urol 1999;162:1640–4.
- Matsuoka K, Iida S, Tomiyasu K, et al. Transurethral holmium laser resection of the prostate. J Urol 2000;163:515–8.
- Chilton CP, Mundy IP, Wiseman O. Results of holmium laser resection of the prostate for benign prostatic hyperplasia. J Endourol 2000;14:533–4.
- Clarke M, Horton R. Bringing it all together: Lancet-Cochrane collaborate on systematic reviews. Lancet 2001;357:1728.
- Fayad AS, EI Sheikh MG, Zakaria T, et al. Holmium laser enucleation versus bipolar resection of the prostate: a prospective randomized study. Which to choose? J Endourol 2011;25:1347–52.
- Neill MG, Gilling PJ, Kennett KM, et al. Randomized trial comparing holmium laser enucleation of prostate with plasm-akinetic enucleation of prostate for treatment of benign prostatic hyperplasia. Urology 2006;5:1020–4.
- Chen Y, Chen Q, Wang Z, et al A prospective, randomized clinical trial comparing plasm-akinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year follow up. J Urol 2013;189:217–22.
- Zhu Q, Gu X, Yuan L, et al. TUBVP and HOLEP: desirable surgical options for large benign prostatic hyperplasia (>80 ml). Natl J Androl 2008;14:907–10.
- Pajovic B, Radojevic N, Dimitrovski A, et al. The therapeutic potential of royal jelly in benign prostatic hyperplasia. Comparison with contemporary literature. Aging Male 2016;19:192–6.
- Salah Azab S, Elsheikh MG. The impact of the bladder wall thickness on the outcome of the medical treatment using alpha-blocker of BPH patients with LUTS. Aging Male 2015;18:89–92.
- Rassweiler J, Teber D, Rainer Kuntz, Rainer Hofmann. Complications of transurethral resection of the prostate (TURP) – incidence, management, and prevention. Eur Urol 2006;50:969–80.
- ElMalik EM, Ibrahim AI, Gahli AM, et al. Risk factors in prostatectomy bleeding: preoperative urinary infection is the only reversible factor. Eur Urol 2000;37:199–204.
- Rieken M, Bachmann A, Shariat SF. Long-term follow-up data more than 5 years after surgical management of benign prostate obstruction: who stands the test of time? Curr Opin Urol 2016;26:22–7.
- Cornu JN. Bipolar, monopolar, photovaporization of the prostate, or holmium laser enucleation of the prostate: how to choose what's best? Urol Clin North Am 2016;43:377–84.
- Fayad AS, Elsheikh MG, Zakaria T, et al. Holmium laser enucleation of the prostate versus bipolar resection of the prostate: a prospective randomized study. “pros and cons”. Urology 2015;86:1037–41.
- Cornu JN, Ahyai S, Bachmann A, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 2015;67:1066–96.
- Chen Q, Zhang L, Fan QL, et al. Bipolar transurethral resection in saline vs traditional monopolar resection of the prostate: results of a randomized trial with a 2-year follow-up. BJU Int 2010;106:1339–43.
- Ho HS, Yip SK, Lim KB, et al. A prospective randomized study comparing monopolar and bipolar transurethral resection of prostate using transurethral resection in saline (TURIS) system. Eur Urol 2007;52:517–22.
- Fagerström T, Nyman CR, Hahn RG. Bipolar transurethral resection of the prostate causes less bleeding than the monopolar technique: a single center randomized trial of 202 patients. BJU Int 2009;105:1560–4.
- Miki M, Shiozawa H, Matsumoto T, Aizawa T. Transurethral resection in saline (TURis): a newly developed TUR system preventing obturator nerve reflex. Nippon Hinyokika Gakkai Zasshi 2003;94:671–7.
- Shiozawa H, Aizawa T, Ito T, et al. A new transurethral resection system: operating in saline environment precludes obturator nerve reflexes. J Urol 2002;168:2665–7.
- Chen Q, Zhang L, Liu YJ, et al. Bipolar transurethral resection in saline system versus traditional monopolar resection system in treating large-volume benign prostatic hyperplasia. Urol Int 2009;83:55–9.
- Cynk M. Holmium laser enucleation of the prostate: a review of the clinical trial evidence. Ther Adv Urol 2014;6:62–73.
- Mavuduru RM, Mandal AK, Singh SK, et al. Comparison of HoLEP and TURP in terms of efficacy in the early postoperative period and peri-operative morbidity. Urol Int 2009;82:130–5.
- Tan A, Liao C, Mo Z, Cao Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg 2007;94:1201–8.
- Gupta NP, Nayyar R. Management of large prostatic adenoma: lasers versus bipolar transurethral resection of prostate. Indian J Urol 2013;29:225–35.
- El-Hakim A, Elhilali MM. Holmium laser enucleation of the prostate can be taught: the first learning experience. BJU Int 2002;90:863–9.
- Ahyai SA, Lehrich K, Kuntz RM. Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur Urol 2007;52:1456–64.
- Coban S, Doluoglu OG, Keles I, et al. Age and total and free prostate-specific antigen levels for predicting prostate volume in patients with benign prostatic hyperplasia. Aging Male 2016;19:124–7.