Abstract
Objectives: The current study aimed to explore whether the CHADS2 score was predictive of lower extremity amputation (LEA) and death in people with peripheral arterial occlusive disease (PAOD).
Methods: This nationwide cohort came from Taiwan, with 16,888 PAOD patients, from 2000 through 2011, extracted from the Longitudinal Health Insurance Database 2000. Cox proportional hazard regression models were employed to identify the LEA and mortality risk according to CHADS2 score. The discriminatory properties of the score in predicting the outcomes were quantified by the area under the receiver operating characteristic curve (AUROC) and the Cox C-index.
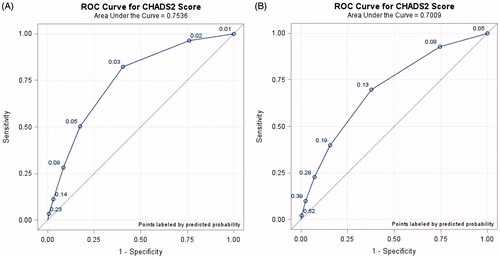
Results: The AUROC of the CHADS2 score in predicting LEA and death were 0.75 (95% CI = 0.73–0.77) and 0.70 (95% CI = 0.69–0.71), respectively. The CHADS2 score had an acceptable stratification capacity for LEA (C-index = 0.79) and death (C-index = 0.76) based on Cox-regression analysis.
Conclusions: This study correlates the CHADS2 score with risk of developing LEA and death in patients with PAOD. The acceptable discriminative power of the score diversifies its predictive role in this population.
Introduction
The burden of atherosclerosis-related diseases is huge worldwide; indeed, three common atherosclerosis diseases, including coronary artery disease (CAD), cerebral vascular disease (CVD), and peripheral arterial occlusive disease (PAOD) constitute the atherosclerotic cardiovascular disease (ASCAD) [Citation1].
Emerging role of PAOD has been noted recently; indeed, approximately two-thirds PAOD patients have some degree of CAD or CVD, highlighting the importance of PAOD surveillance [Citation2,Citation3]. Once PAOD was left undiagnosed and untreated, several sequelae might occur; among them, loss of lower limb gain more attention due to the deleterious biomedical and psychosocial effect [Citation2,Citation3]. Hence, to avoid the unexpected and unnecessary limb loss in PAOD patients, to construct a simply stratification tool for practical clinical use is urgently needed.
Expanded indications of CHADS2 score for predicting adverse outcomes in different groups have been reported although this particular score was originally designed for the evaluation of stroke risk among people with established AF [Citation4–8]. The current study was conducted to investigate whether the CHADS2 score, a real-made product, was predictive of incident lower limb amputation in people with PAOD. Additionally, the other outcome of all-cause mortality was also included for analysis.
Methods
Data source
Data were sourced from the Longitudinal Health Insurance Database (LHID) 2000. For research purpose, the National Health Research Institutes (NHRI) compiles all medical claims in the National Health Insurance (NHI) program and releases the database annually to the public [Citation9]. The details of the NHI program and LHID 2000 were reported elsewhere [Citation10,Citation11]. Diagnosis was made according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. This study was approved by the Institutional Review Board of China Medical University (CMUH-104-REC2-115).
Sampled participants
We selected patients aged ≥18 years with newly diagnosed PAOD (ICD-9-CM codes 440.2, 440.3, 440.8, 440.9, 443, 444.0, 444.22, 444.8, 447.8, 447.9), between 2000 and 2011, as the study cohort. PAOD patients with a previous diagnosis of lower extremity amputation (LEA) (ICD-9 procedure codes 84.1) were excluded. The PAOD diagnosis date was defined as the index date. The CHADS2 score was calculated for each patient by assigning 1 point each for age ≧75 years, a history of heart failure, hypertension, and diabetes mellitus; 2 points each for a history of an ischemic stroke/transient ischemic attack (TIA) [Citation12–15]. Other baseline comorbidities, such as atrial fibrillation (AF) (ICD-9-CM code 427.31), hyperlipidemia (ICD-9-CM code 272), chronic obstructive pulmonary disease (COPD) (ICD-9-CM codes 491, 492, 496), chronic kidney disease (CKD) (ICD-9-CM codes 580-589), and gout (ICD-9-CM code 274) were also included in the current study.
Outcomes
All study patients were followed from the index date to the occurrence of LEA, death, withdrawal from the NHI program, or the end of 2011 (whichever came first).
Statistical analysis
To characterize the PAOD cohort, we presented number and percentage for category variables, and mean and corresponding standard deviation (SD) for continuous variables. We calculated the incidence density rate of LEA and mortality according to CHADS2 score. Univariable and multivariable Cox proportional hazard regression models were employed to explore the risk of LEA and death according to CHADS2 score, shown as hazard ratios (HRs) with 95% confidence intervals (CIs). Cumulative incidence curves of LEA and mortality stratified by CHADS2 score were measured by Kaplan–Meier method. We applied log-rank test to assess the difference between curves. The predictive ability of CHADS2 score for LEA and mortality in the study cohort was assessed using area under the receiver operating characteristic (AUROC) curve. The C-index was also estimated based on Cox-regression analysis (Harrell C) to quantify the discriminatory properties of the CHADS2 score [Citation16]. All data analyzes were performed using SAS statistical software (Version 9.4, SAS Institute, Cary, NC). The two-sided significance level was set at p < .05.
Results
A total of 16,888 PAOD patients was included; among them, 76.8% patients were aged ≦74 years, and 52.9% were men (). Mean age of the study patients was 63.4 (±14.5) years. The four major comorbidities of the study patients were hypertension (68.1%), hyperlipidemia (43.0%), diabetes mellitus (25.7%), and COPD (22.7%). Most PAOD patients had a CHADS2 score of 1 (35.0%). Mean CHADS2 score was 1.49 (±1.30). Mean follow-up period was 5.35 (±3.46) years for LEA and 5.42 (±3.43) years for mortality.
Table 1. Baseline characteristics of PAOD patients.
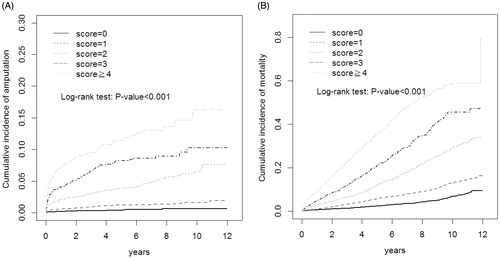
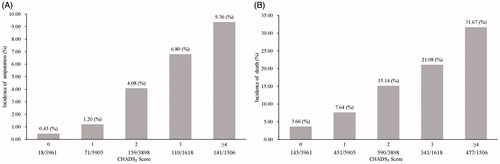
The incidence of LEA increased from 0.45% to 9.36% while the CHADS2 score increased from 0 to ≧4 (). The incidence of death increased from 3.66% in PAOD patients with CHADS2 score 0 to 31.67% in those with CHADS2 score ≧4 ().
Figure 1. The incidence of lower extremity amputation (A) and death (B) according to CHADS2 score in patients with peripheral arterial occlusive disease.
After adjusting for AF, hyperlipidemia, COPD, CKD, and gout, as compared with PAOD patients with a CHADS2 score of 0, the corresponding adjusted HR (aHR) for incident LEA were 2.37 (95% CI = 1.40–4.01), 7.78 (95% CI = 4.64–13.0), 14.2 (95% CI = 8.24–24.3), and 20.8 (95% CI = 12.1, 35.8) for those with a CHADS2 score of 1, 2, 3, and ≧4, respectively (trend test, p < .001) (). As compared with PAOD patients with a CHADS2 score of 0, the corresponding aHR for death for CHADS2 score 1, 2, 3, and ≧4, were 2.07 (95% CI = 1.72–2.50), 4.62 (95% CI = 3.84–5.57), 7.58 (95% CI = 6.21–9.27), and 13.2 (95% CI = 10.9–16.1), respectively (trend test, p < .001).
Table 2. Incidence and HR of lower extremity amputation and death in PAOD patients stratified by CHADS2 score.
Cumulative incidence curves of LEA and death stratified by CHADS2 score in PAOD patients are clearly demonstrated by Kaplan–Meier analyzes in . The AUROC of CHADS2 score in predicting LEA and death was 0.75 (95% CI = 0.73–0.77) and 0.70 (95% CI = 0.69–0.71), respectively (). The CHADS2 score had an acceptable discrimination power for LEA (C-index = 0.79) and death (C-index = 0.76) based on Cox-regression analysis (Harrell C) [Citation16].
Discussion
The predictive role of CHADS2 in incident LEA and all-cause mortality in people with PAOD has been shown for the first time in the present study.
Several predictors of lower limb amputation and mortality among PAOD patients have been defined [Citation17–19]. However, limited scoring systems were proposed for predicting extremity amputation and mortality in this specific patient population [Citation20–25]. Moreover, the proposed scoring systems are relative impractical for clinical use due to their complicatedness [Citation20–25]. Hence, the current study aimed to clarify whether the CHADS2 score, a ready-made product capturing several well recognized atherothrombotic risk factors [Citation4–8], served as an optimized risk scoring scheme for limb loss and mortality among people with PAOD. The presented results were comparable with prior studies [Citation20–25]; suggesting that CHADS2 score might be considered as a viable alternative of risk stratification tool in this population.
Early study has shown that an elevated CHADS2 score correlates with the end point of critical limb ischemia in people with PAOD [Citation26]. However, it should be noted that no attempt was made to assess the discriminative ability in that study since the odds ratio but not the AUROC or Cox C-index analysis was implemented. Moreover, the study conducted by Gary et al. was limited by the single-center design with relative small sample size. Furthermore, the hard outcome, such as mortality, was not included for analysis. In contrast, the main strength of our study is its large-scale, 16,888 study patients with an extended follow-up period. Our findings further diversified the predictive role of the CHADS2 score in risk stratification for LEA and mortality among PAOD patients. Further prospective investigations might be needed to verify the presented findings.
In this study, we found that people with PAOD were at an increased risk of lower limbs amputation and death while their CHADS2 scores were 1 or above, as compared with those with a score of 0. In addition, the CHADS2 score was reported to confer an acceptable power to predict the outcomes in PAOD patients. Based upon its inherent nature of convenience and simplicity, CHADS2 score might be helpful for the physicians for risk discrimination of LEA and mortality in this population.
Limitations
First, personal health behaviors were not available in this dataset. Furthermore, the information on the severity of PAOD, such as ankle-brachial index, Fontaine classification and Rutherford classification, and on therapies for PAOD, such as medical treatment, endovascular stenting and surgical intervention were not included in this study. Second, the diagnoses were made by ICD coding system. Finally, comparison between using the CHADS2 scoring system as a predictor of the outcomes and other outcomes-prediction tools in this patient population cannot be performed due to the limitations of this database.
Conclusions
This study reported for the first time that CHADS2 score was predictive of the outcomes of LEA and all-cause mortality in PAOD patients. Acceptable predictive ability was noted; hence, the CHADS2 score might be useful for the physicians while caring for these patients for risk stratification.
Disclosure statement
No potential conflict of interest was reported by the authors..
Additional information
Funding
References
- Stone NJ, Robinson JG, Lichtenstein AH, et al.; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–S45.
- Achterberg S, Cramer MJ, Kappelle LJ, et al.; SMART study Group. Patients with coronary, cerebrovascular or peripheral arterial obstructive disease differ in risk for new vascular events and mortality: the SMART study. Eur J Cardiovasc Prev Rehabil. 2010;17:424–430.
- Shammas NW. Epidemiology, classification, and modifiable risk factors of peripheral arterial disease. Vasc Health Risk Manag. 2007;3:229–234.
- Ogawa S, Aonuma K, Tse HF, et al. TheAPHRS’s 2013 statement on antithrombotic therapy of patients with nonvalvular atrial fibrillation. J Arrhythm. 2013;29:190–200.
- Fuster V, Rydén LE, Cannom DS, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011;57:e101–e198.
- Sun GZ, Ye N, Zhang NJ, et al. Association between CHADS2 score, depressive symptoms, and quality of life in a general population. BMC Psychiatry. 2017;17:80.
- Hsu CY, Chen TH, Su YW, et al. Usefulness of the CHADS2 score for determining risk of seizure in patients with atrial fibrillation. Am J Cardiol. 2016;118:1340–1344.
- Huang SS, Chan WL, Leu HB, et al. Association between CHADS2 score and the preventive effect of statin therapy on new-onset atrial fibrillation in patients with acute myocardial infarction. PLoS One. 2013;8:e74709.
- National Health Research Institutes. National Health Insurance Research Database. [cited 2015 Apr 14]. Available from: http://nhird.nhri.org.tw/en/index.html
- Hu WS, Lin CL. Association between cataract and risk of incident atrial fibrillation: a nationwide population-based retrospective cohort study. Mayo Clin Proc. 2017;92:370–375.
- Lin CJ, Liao WC, Chen YA, et al. Statin therapy is associated with reduced risk of peptic ulcer disease in the Taiwanese population. Front Pharmacol. 2017;8:210.
- Yang YW, Chen YH, Hsu CC, et al. CHADS2 scores as a predictor of ischemic stroke in patients with peripheral artery disease. Mayo Clin Proc. 2016;91:45–50.
- Chao TF, Liu CJ, Tuan TC, et al. Comparisons of CHADS2 and CHA2DS2-VASc scores for stroke risk stratification in atrial fibrillation: which scoring system should be used for Asians. Heart Rhythm. 2016;13:46–53.
- Chao TF, Liu CJ, Wang KL, et al. Incidence and prediction of ischemic stroke among atrial fibrillation patients with end-stage renal disease requiring dialysis. Heart Rhythm. 2014;11:1752–1759.
- Chao TF, Liu CJ, Chen SJ, et al. CHADS2 score and risk of new-onset atrial fibrillation: a nationwide cohort study in Taiwan. Int J Cardiol. 2013;168:1360–1363.
- Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387.
- Swaminathan A, Vemulapalli S, Patel MR, et al. Lower extremity amputation in peripheral artery disease: improving patient outcomes. Vasc Health Risk Manag. 2014;10:417–424.
- Jones WS, Patel MR, Dai D, et al. Temporal trends and geographic variation of lower-extremity amputation in patients with peripheral artery disease: results from US Medicare 2000–2008. J Am Coll Cardiol. 2012;60:2230–2236.
- Amrock SM, Weitzman M. Multiple biomarkers for mortality prediction in peripheral arterial disease. Vasc Med. 2016;21:105–112.
- Hackl G, Belaj K, Gary T, et al. COPART risk score predicts long-term mortality in peripheral arterial occlusive disease. Eur J Vasc Endovasc Surg. 2015;50:94–100.
- Moxey PW, Brownrigg J, Kumar SS, et al. The BASIL survival prediction model in patients with peripheral arterial disease undergoing revascularization in a university hospital setting and comparison with the FINNVASC and modified PREVENT scores. J Vasc Surg. 2013;57:1–7.
- Feringa HH, Bax JJ, Hoeks S, et al. A prognostic risk index for long-term mortality in patients with peripheral arterial disease. Arch Intern Med. 2007;167:2482–2489.
- Sprengers RW, Janssen KJ, Moll FL, SMART Study Group, et al. Prediction rule for cardiovascular events and mortality in peripheral arterial disease patients: data from the prospective Second Manifestations of ARTerial disease (SMART) cohort study. J Vasc Surg. 2009;50:1369–1376.
- Schanzer A, Mega J, Meadows J, et al. Risk stratification in critical limb ischemia: derivation and validation of a model to predict amputation-free survival using multicenter surgical outcomes data. J Vasc Surg. 2008;48:1464–1471.
- Gary T, Belaj K, Hafner F, et al. Graz critical limb ischemia score: a risk score for critical limb ischemia in peripheral arterial occlusive disease. Medicine. 2015;94:e1054.
- Gary T, Belaj K, Hafner F, et al. A high CHA(2)DS(2)-VASc score is associated with a high risk for critical limb ischemia in peripheral arterial occlusive disease patients. Atherosclerosis. 2012;225:517–520.