Abstract
Acute vasitis is a rare infection of the vas deferens. Clinical presentation and disease rarity can cause difficulty in correctly diagnosing this condition. Adjuncts to aid diagnosis can be used that include ultrasound scan (USS) or computed tomography. We report a unique case of acute vasitis following vasectomy, reversal and subsequent re-do vasectomy diagnosed using USS.
Introduction
Vasitis is a rare condition characterized by inflammation of the vas deferens. It includes vasitis nodosa and acute vasitis [Citation1]. Vasitis nodosa is more common; it is a condition of chronic inflammation caused by obstruction of the vas deferens. Acute vasitis is acute infection caused by urinary pathogens [Citation1]. Patients present with pain and swelling in the groin, and have a broad differential diagnosis [Citation2]. This can cause diagnostic dilemma and potentially unnecessary surgery. We aim to present our unique experience of ultrasound proven acute vasitis following vasectomy.
Case report
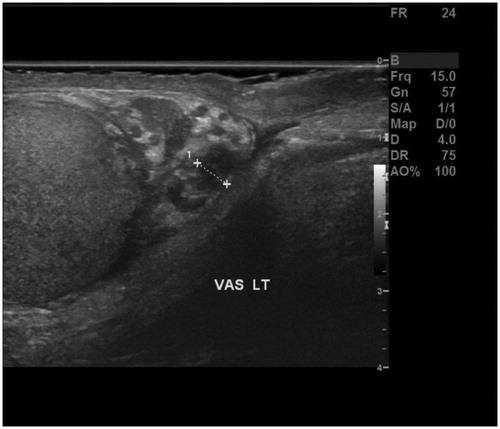
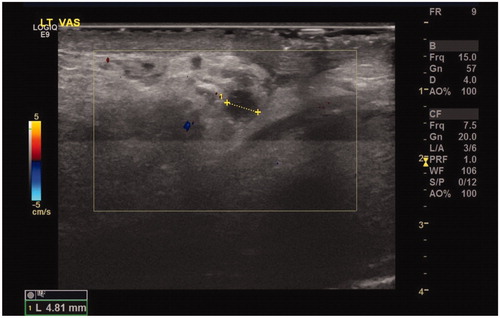
A 52-year-old man presented with acute-on-chronic left testicular pain. There was a past surgical history of vasectomy, followed by reversal of vasectomy, and subsequent re-do vasectomy. There was also history of complex regional pain syndrome affecting his left hand and right foot. Clinical examination of his scrotum revealed an exquisitely tender left vas deferens. Inflammatory markers were normal. An urgent scrotal ultrasound scan (USS) was performed that reported left vasitis ( and ). He was successfully treated conservatively with oral ciprofloxacin 500 mg twice daily for 10 days.
Discussion
The vas deferens connects the epididymis to the ejaculatory ducts and functions to move sperm through its 30 cm length. It is divided into three anatomical segments: scrotal, suprascrotal and prepubic. The scrotal segment is convoluted and tortuous, with the latter segments linear [Citation1]. Vasitis is a rare condition that results from inflammation of the vas deferens, which includes vasitis nodosa and acute vasitis [Citation1].
Vasitis nodosa is a chronic inflammatory disorder associated with obstruction of the vas deferens resulting in leakage of spermatozoa into the spermatic cord. This benign condition is commonly associated with vasectomy [Citation2]. Acute vasitis is a rare infection of the vas deferens. The pathogenesis of acute vasitis is similar to epididymitis, and is caused by retrograde spread of urinary tract pathogens from the prostatic urethra, prostate or seminal vesicles [Citation1]. Common pathogens include Escherichia coli and Haemophilus influenza [Citation3].
Acute vasitis presents with localized pain and swelling in the scrotal and groin regions. As a result, the diagnosis of acute vasitis can be difficult and cause uncertainty. The reason for this is the rarity of this disease but also the more common alternative pathology, which include inguinal hernia, epididymitis or testicular torsion [Citation4]. When acute vasitis involves the scrotal segment of the vas deferens, it is especially difficult to differentiate clinically from epididymitis [Citation1].
Historically, cases of acute vasitis have been reported as an intra-operative finding [Citation2]. This is likely because of less readily available diagnostic adjuncts [Citation4], such as USS, CT or magnetic resonance imaging (MRI) scan. More recently, Yang et al. [Citation1] reported 12 cases of acute vasitis diagnosed using USS as part of a retrospective analysis. However, two more recent case reports from both Patel et al. [Citation2] and Eddy et al. [Citation4] reported diagnostic uncertainty when using USS and need for more invasive and costly imaging. Treatment for vasitis is conservative with a course of antibiotics without the need for surgical intervention [Citation2].
What is unique to this case is that the patient had a reversal of vasectomy and subsequent re-do vasectomy. To our best knowledge, no previous case reports of acute vasitis have had a vasectomy. Vasectomy is one of the most common urological procedures performed, there are around 500,000 performed in the United States each year [Citation5], Trinick et al. [Citation6] reported rates of vasectomy at 34% in patients in their 60s. It is the most effective male contraceptive method and has a success rate of 98% [Citation7]. The procedure is typically performed under local anaesthesia and involves excision of at least 1 cm of the vas deferens. Electrocautery fulguration to the remaining ends of the vas deferens, or placement of sutures, is a technique used to prevent recanalization [Citation5]. Complications associated with vasectomy include infection, symptomatic hematoma, vasectomy failure and post-vasectomy pain syndrome (PVPS) [Citation8].
PVPS is defined as constant or intermittent testicular pain for 3 months or longer with a severity that interferes with daily activities prompting the patient to seek medical treatment [Citation9]. The incidence of PVPS is unknown and highly variable in the literature, Leslie et al. [Citation10] prospectively surveyed 593 men undergoing vasectomy and 14.7% of men reported chronic scrotal pain. The pathophysiology of this condition is unclear. Some of the mechanisms thought to cause PVPS include direct damage to spermatic cord, compression of nerves via inflammation, back pressure from epididymal congestion and perineural fibrosis [Citation7]. It is a diagnosis of exclusion following clinical examination, USS and routine urinalysis [Citation7]. Treatment is often conservative with non-steroidal anti-inflammatory drugs, tricyclic antidepressants, nerve blocks or gabapentin. If these fail, surgical intervention may be considered and include vasectomy, epididymectomy, microsurgical spermatic cord denervation and orchidectomy [Citation5,Citation8].
As of yet, there has been no link between acute vasitis and vasectomy. Therefore, we expect that patients could potentially be misdiagnosed with PVPS rather than acute vasitis without proper clinical evaluation. The importance of this is that treatment differs for these two conditions, with no reported indication for antibiotics for PVPS unless there is suspected concomitant infection [Citation11].
The pathophysiology of acute vasitis is thought to be as a result of retrograde spread of urinary tract pathogens and infections. There is a well-known link between diabetes and infection. It has been reported that there is a 10-fold increase in diabetes prevalence from men in their 40s to their 60s [Citation12]. There is also association between low androgen levels due to increased age and prevalence of urinary tract infections at 35% [Citation6]. It is pertinent to consider acute vasitis in the differential diagnosis when evaluating a patient with these co-morbidities presenting with inguino–scrotal pain and infection.
Conclusion
Acute vasitis can present diagnostic dilemma owing to disease rarity and more common alternative diagnosis. We present our unique case of ultrasound proven vasitis in a patient following vasectomy, reversal of vasectomy and subsequent re-do vasectomy. Treatment is conservative with a course of antibiotics. When clinical and USS features are inconclusive, CT scan or MRI can be considered to aid diagnosis and avoid surgical intervention.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Yang DM, Kim HC, Lee HL, et al. Sonographic findings of acute vasitis. J Ultrasound Med. 2010;29:1711–1715.
- Patel K, Lamb B, Pathak S, et al. Vasitis: the need for imaging and clinical acumen. BMJ Case Rep. 2014;2014:bcr2014206994.
- Chan PT, Schlegal PN. Inflammatory conditions of the male excurrent ductal system: part II. J Androl. 2002;23:461–469.
- Eddy K, Piercy B, Eddy R. Vasitis: clinical and ultrasound confusion with inguinal hernia clarified by computed tomography. Can Urol Assoc J. 2011;5:74–76.
- Tan WP, Levine LA. An overview of the management of post-vasectomy pain syndrome. Asian J Androl. 2016;18:323–337.
- Trinick T, Feneley M, Welford H, et al. International web survey shows high prevalence of symptomatic testosterone deficiency in men. Aging Male. 2011;14:10–15.
- Sinha V, Ramasamy R. Post-vasectomy pain syndrome: diagnosis, management and treatment options. Transl Androl Urol. 2017;6:S44–S47.
- Smith-Harrison LI, Smith RP. Vasectomy reversal for post-vasectomy pain syndrome. Transl Androl Urol. 2017;6:S10–S13.
- Valencic MR, Granitsiotis P, Kirk D. Chronic testicular pain: an overview. Eur J Urol. 2004;45:430–436. Re: Eur J Urol. 2005;47:720.
- Leslie TA, Illing RO, Cranston DW, et al. The incidence of chronic scrotal pain after vasectomy: a prospective audit. BJU Int. 2007;100:1330–1333.
- Tan WP, Levine LA. What can we do for chronic scrotal content pain? World J Mens Health. 2017;35:146–155.
- LeRoith D. Diabetes in the aging male. Aging Male. 2005;8:133–134.