Abstract
Objectives
We aimed to investigate the effect of kinesiotaping (KT) on the respiratory parameters as measured by spirometry and depression in the chronic obstructive pulmonary disease (COPD) patients.
Methods
In this prospective, randomized, controlled, single-blind study 42 male patients with COPD diagnosis were randomized into two groups. In Group1 (n = 21) routine COPD medical treatment plus kinesiotaping and in Group2 (n = 21) only routine COPD medical treatment was given. KT was changed on every fifth day (for a total of three times and 15 days). The patients were assessed using Visual Analog Scale (VAS) for difficulty experienced by the patients during respiration, respiratory function test (RFT), modified medical research council (mMRC) dyspnea scale and beck depression inventory (BDI). The data were obtained before treatment and posttreatment.
Results
In Group 1; statistically significant improvement was found in all parameters except for FVC and FVC % following treatment compared to pretreatment values. Comparison of the difference scores (the amount of recovery between posttreatment and pretreatment) of the two groups showed significantly superior improvement in Group1 for all parameters except for FVC, FVC % and FEV1% following the treatment (p < .05).
Conclusions
The results of this study showed that supplementary kinesiotaping improved respiratory function and depression significantly compared to only routine medical treatment in COPD patients who were in stable condition.
1. Introduction
Chronic obstructive pulmonary disease (COPD) is an inflammatory disease that arises from the abnormalities of the airway and the alveoli and is characterized by permanent respiratory symptoms and restriction of air flow [Citation1]. Disturbed ventilation and gas exchange, dysfunctional peripheral and respiratory muscles, reduction in the capacity of oxygen consumption, and shortness of breath and decrease in exercise capacity developing as a result of the combined effects of the above changes are observed in COPD [Citation2]. The most frequent clinical symptoms are shortness of breath, chronic cough, and sputum production. The gold standard for COPD diagnosis is the respiratory function tests (RFT) [Citation1], which allow objective assessment and follow-up of lung capacity and the functional status [Citation3]. Detection of localized air flow obstruction (postbronchodilator FEV1/FVC <%70) in the RFT of the patients of middle to advanced age and with the history of chronic symptoms and exposure to risk factors confirms the diagnosis of COPD [Citation1].
Detection and treatment of several co-morbidities including depression is crucial in the management of COPD [Citation1]. The purpose of medical treatment of COPD is to reduce the frequency and severity of the symptoms and to improve the functional capacity and the quality of life [Citation4]. Pulmonary rehabilitation (PR) is described in the update of ATS/ERS in 2013 as a comprehensive modality that aims to improve the physical and emotional status of COPD patients and involves individualized exercise training and behavioral modifications [Citation5].
Kinesiotherapy (KT) employs a cotton tape with a layer of hypoallergenic adhesive which can stretch upto 140% of its original length. It is known to have a mechanism of action exerted through a combination of its biomechanical, exteroceptive, circulatory, and analgesic effects [Citation6]. Kinesiologic taping is currently used in several musculoskeletal system problems as well as in the rehabilitation of the patients with central nervous system disorders such as hemiplegia, cerebral palsy, multiple sclerosis, and also in nerve entrapment and peripheral nerve injuries including the brachial plexus [Citation7–14]. It has also been employed in headache, constipation, torticollis, temporomandibular joint disorders, asthma, and for the purpose of increasing the respiratory capacity [Citation15]. However, we could not find any report showing the evidence for increased respiratory capacity with kinesiotaping in the literature. In order to better demonstrate that the respiratory capacity of the lung increased with kinesiotaping, we thought to do this study in COPD, one of the most common diseases that reduced lung respiratory capacity. In this study, our purpose was to investigate the effect of kinesiotaping on depression and the respiratory parameters as measured by spirometry in the male COPD patients who were in stable condition.
2. Materials and methods
This study was designed as prospective, randomized, controlled, and single-blind. After approval of the local ethics committee (Decision number was 2011- KAEK-25 2016/22–03) 50 patients with COPD were assessed for eligibility of the study.
2.1. Patients
Inclusion criteria were (1) male patients aged 40 to 75 years; (2) patients with stable moderate or severe COPD and under routine medical COPD therapy (beta 2 agonist and inhaled corticosteroid) for at least 1 year.
Exclusion criteria were (1) Acute COPD exacerbations, (2) Uncontrolled arterial hypertension and diabetes mellitus, (3) Peripheral and central nervous system diseases, (4) Coronary artery disease, (5) Polyneuropathy, (6) Mental retardation, (7) Antidepressant usage, (8) Metabolic disorders.
Forty-two patients, who were found to be eligible for the study, were given detailed information about the study and a written consent form was signed by them. Demographic characteristics of the patients and pretreatment evaluation parameters were recorded.
2.2. Randomization
Patients who were included in the study were randomized into two groups using a random number table.
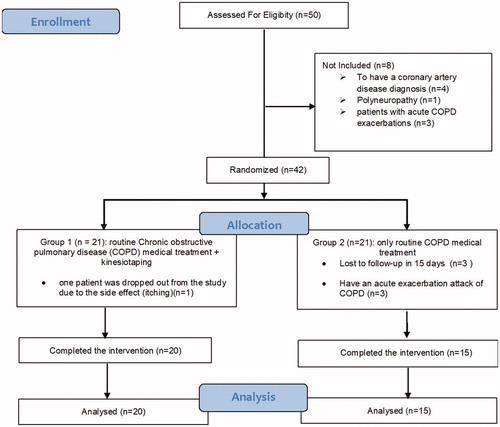
In Group1 (n = 21): routine COPD medical treatment plus kinesiotaping and in Group2 (n = 21): only routine COPD medical treatment was given ().
2.3. Interventions
2.3.1. Kinesiotaping (KT)
In Group 1, KinesioTex Gold (KinesioTex Gold, Kinesio®; Albuquerque, New Mexico) was used for KT application. Patients were seated on a chair. When the patients were at the end of the expiration, it was applied bilaterally on the fifth to sixth and ninth to tenth intercostal muscles transversally and on the anterior and posterior axillary line longitudinally with 50% tension (). In order to stimulate the muscle and support the function, the stimulation technique is usually applied from the origin to the insertion of the muscle with the recommended stretching of 25 to 50% [Citation16]. KT was changed on every fifth day (for a total of three times and 15 days) by the same certified physiatrist who had previously attended the KT training course. The patients were instructed not to take the tapes off at any time but they were allowed to take showers. The researcher, who was blind to the type of treatment, completed post-treatment (15th day) evaluations for each patient and recorded the data.
2.4. Evaluation parameters
2.4.1. Primary outcome measure
Visual Analog Scale (VAS) and Modified Medical Research Council (mMRC) Dyspnea Scale.
2.4.2. Visual Analog Scale (VAS)
Difficulty experienced by the patients during respiration was assesses by VAS. VAS was measured on a 0–10 cm scale.
2.4.3. Modified Medical Research Council (mMRC) Dyspnea Scale
It is a five-item measure based on a variety of physical activities that cause a feeling of dyspnea. The patients are asked to mark the level of activity that causes the feeling of dyspnea [Citation17,Citation18].
2.4.4. Secondary outcome measure
Respiratory function test (RFT) and Beck Depression Inventory (BDI).
2.4.5. Respiratory function test (RFT)
RFT was done using the spirometer “Spirolab II” MIR 010, a product of Medical International Research (MIR).For spirometric evaluation performed after bronchodilator, the forced vital capacity (FVC), forced expiratory volume at first second (FEV1) and FEV1/FVC were recorded. The measurements were made by a technician according to the American Thoracic Society (ATS)/European Respiratory Society (ERS) criteria [Citation17,Citation18].
2.4.6. Beck Depression Inventory (BDI)
The scale was designed to contain the indications found on the depression. Likert type scale consists of 21 symptom categories. Each symptom category is evaluated with scores ranging from 0 to 3. The highest score that can be taken from the scale is 63. The higher the total score, the higher the level of depression or the severity [Citation19]. Turkish validity and reliability study of BDI was previously done by Hisli et al. in 1988 [Citation20].
2.5. Statistical analysis
Analysis of the collected data was performed using IBM SPSS 22.0 statistical package program. The Pearson chi-square (χ2) or Yates χ2 tests were used in the comparison of the categorical variables. Normal distribution of the data was tested using Shapiro–Wilk test. When it was distributed normally, independent samples t-test was used for between-groups comparisons. When it was distributed abnormally, Mann–Whitney U test was used for between-groups comparisons and Wilcoxon’s test for intra-group comparisons. Values with a probability of (p) α < .05 was accepted as significant.
2.5.1. Power Analysis
In the results of a previous 10-patient pilot study, the kinesiotape patients’ mMRC Dyspnea Scale scores were found to be 2.35 ± 0.82 in the pretreatment, and the posttreatment mMRC Dyspnea Scale scores was 1.57 ± 0.80. To obtain a study power of 85% (α = 0.05), 21 patients from each group for the required sample size – a total of 42 patients –were assessed.
3. Results
One patient was left out of the study from Group 1 due to a side effect of the treatment (itching). In group 2, 3 patients were excluded because of acute exacerbation of COPD and 3 patients abandoned the study because of private reasons (). The present study was completed with a total of 35 patients (Group 1; n = 20 and Group 2; n = 15) ().
Distribution of age, body mass index (BMI), and complaint duration times of the patients are presented in . Pretreatment evaluation of the parameters in both groups is presented in . There was no statistically significant difference between the two groups for demographic characteristics and pretreatment evaluation parameters (p > .05).
Table 1. Comparison of demographic characteristics of patients.
Table 2. Comparison of the pretreatment and posttreatment values within the groups and between the groups.
In Group 1; a statistically significant improvement was found in all parameters except for FVC and FVC % following treatment compared to pretreatment values ().
In Group 2, a statistically significant improvement was found only in FEV1 compared to pretreatment values ().
The difference scores were calculated by subtracting the pretreatment values from the post-treatment values. Thus, it was tried to compare the degrees of post-treatment recovery. Comparison of the difference scores of the two groups showed significantly superior improvement in Group1 for all parameters except for FVC, FVC % and FEV1% following treatment (p < .05) ().
Table 3. Comparison of difference score between groups.
4. Discussion
The results of this study showed that kinesiotaping added to routine medical therapy was more effective in improving respiratory function and depression compared to only routine medical treatment in the patients who had moderate to severe COPD but were in stable condition.
Kinesiotaping (KT) is a therapeutic modality which was first developed by Kenso Kase [Citation16] and has been used in several musculoskeletal system disorders, sports injuries, and neurological and pediatric diseases [Citation7–14]. Kinesiotaping has been shown to increase the interstitial space in and beneath the skin and improve blood circulation and mobility by its lifting effect on the skin. Improvement of circulation and mobility is expected to reduce local inflammation, relieve pain, prevent tissue damage, support wound healing, increase the performance, and help neuromuscular reeducation [Citation21].
Kase et al. [Citation16] have suggested that kinesiotaping stimulated the mechanoreceptors in proportion with the amount of tension applied to the skin by the tape. This stimulus sends signals to the central nervous system which then elicits a positional stimulus in that skin area. That positional stimulus then leads to a sensory stimulus through enhancement or limitation of movement. Increased proprioception has also been suggested as another mechanism of action in kinesiotaping. The effect of kinesiotaping was assessed in a placebo-controlled study in 42 patients with either shoulder impingement syndrome or rotator cuff tendinitis according to the parameters of pain, disability, and joint range of motion (ROM). The authors concluded that the improvement in abduction may have been the result of an increase in stimulation of the proprioception and supraspinatus muscle strengthening, which then may have improved mobility [Citation8]. In the light of these literature we also believe that kinesiotaping may increase proprioception and may stimulate the patients in our study for deeper respiration.
Kase et al. [Citation16] outlined the positive effects of kinesiotaping as creation of more space over the inflamed area by lifting and straightening the fascia, soft tissue, and the skin and reduction of edema by diverting the exudative flow to the lymphatic channels. The improvement observed in the respiratory tests in our study may be attributed to the increase in the ventilation space and lymphatic circulation which may have contributed to the improvement of chest movements.
There are a limited number of studies in the literature investigating the efficacy of kinesio Taping method on the respiratory system. In two different studies researchers aimed to investigate the effects of kinesio taping method on muscle strength in healthy volunteers. In one study, they reported that the Kinesio taping method applied to the diaphragmatic and accessory muscles provided no effects on the muscle strength. They also reported that the lack of spirometric and volumetric test results in the study was a limitation [Citation22]. In the other study, where the effects of kinesio taping were investigated on the respiratory system in the athletic trainers during the periods of exercising, they found out an increase in expiratory tidal volume without a concurrent effect on the respiratory rate and heart rate [Citation23].
In a study on primary COPD patients with exacerbations, Kinesio Taping® applied to the respiratory muscles adjunctive to standard physiotherapy was found to be effective in improving the oxygen saturation in patients with a COPD exacerbation but without hypoxemia. However, in regards to the results of the spirometric tests, there was no statistically significant difference between the control group and the kinesio taping group in which the method was applied to the diaphragm and scalene muscles [Citation24]. Tomruk et al. reported that the levels of peak expiratory flow (PEF) and the walking distances in the six-minute walk test (6MWT) increased in patients with COPD who were applied Kinesio taping on the trapezius and diaphragmatic muscles [Citation25]. Another study showed that breathing exercises and Kinesio taping when applied in combination, enhanced the muscle tonus and tightness in stroke patients [Citation26].
A study on mechanically ventilated intensive care patients investigated the efficacy of kinesio taping when applied to the thoracic wall and attempted to demonstrate the effects of the method on the respiratory muscles by ultrasonographic muscle measurements. It was demonstrated in this study that the progression of the muscle atrophy due to the mechanical ventilation was attenuated on the side where kinesio taping was applied [Citation27].
The review of the literature informs that the kinesio taping method resulted in diverse results on the respiratory system. There are studies reporting that the method provided positive effects, however, there are also other studies reporting that no effects were observed. The results of this present study are similar to those of the studies reported in the literature, which reported positive results in favor of kinesio taping, however, the lack of detailed spirometric measurements and the application of the kinesio taping method to diverse locations in the chest wall in those studies limit the extent of a comparative discussion of the results. The results of this present study demonstrated that kinesio taping increased the levels of measured values of FEV1, and FEV1/FVC in spirometric measurements in patients with COPD.
The effects of kinesiotaping are known to vary with different amounts of stretching and different locations of application. Several taping techniques have been developed on the basis of these effects. The muscle technique employs the applications that create either stimulation or inhibition of the muscles. In this study, stimulation technique was used to support the function of respiratory muscles according to the method suggested by Kase et al. [Citation16]. The improvement in respiratory function tests may be attributed to the increase in the respiratory capacity provided by this kinesiotaping technique.
Another important point demonstrated in our study results is the lower scores in Beck depression scale in patients treated with kinesio taping. This shows that the mood of the patients with COPD can be impacted by the results of the respiratory function tests and that the decline in FEV1 may increase the tendency of the patients to develop a depressive condition [Citation28,Citation29]. Studies in patients with COPD have shown that adjuvant treatment modalities can ameliorate depression [Citation30]. In our study, the levels of FEV1 increased after the medical treatment only in the medical treatment group compared to the baseline, however, this increase was higher in the medical treatment group with adjunctive kinesio taping. This supports the reports in the literature that kinesio taping, as an adjunctive therapy, improves the mood of the patients by increasing the FEV1 levels [Citation28,Citation29]. We are of the opinion that the effect of kinesio taping on depression in COPD patients is worth investigating in more detail.
4.1. Limitations
The relatively small patient population and the lack of longer follow-up evaluations may be noted as the limitations of this study.
5. Conclusions
The results of this study showed that supplementary kinesiotaping improved respiratory function and depression significantly compared to only routine medical treatment in COPD patients who were in stable condition.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
The registration number (Local ethics committee): 2011- KAEK-25 2016/22-03.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of COPD; 2017. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/.
- MacIntyre NR. Mechanisms of functional loss in patients with chronic lung disease. Respir Care. 2008;53:1177–1184.
- American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am J Respir Crit Care Med. 1995;152:77–120.
- Restrepo R, Alvarez MT, Wittnebel LD, et al. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis. 2008;3:371–384.
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society Statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:13–64.
- Brateanu D. Kinesio taping technique and kinesio tex. Timisoara Phys Educat Rehabil J. 2009;2:36–40.
- Göksu H, Tuncay F, Borman P. The comparative efficacy of kinesio taping and local injection therapy in patients with subacromial impingement syndrome. Acta Orthop Traumatol Turc. 2016;50:483–488.
- Thelen MD, Dauber JA, Stoneman PD. The clinical efficacy of kinesio tape for shoulder pain: a randomized, double-blinded, clinical trial. J Orthop Sports Phys Ther. 2008;38:389–395.
- Öztürk G, Külcü DG, Mesci N, et al. Efficacy of kinesio tape application on pain and muscle strength in patients with myofascial pain syndrome: a placebo-controlled trial. J Phys Ther Sci. 2016;28:1074–1079.
- Jaraczewska E, Long C. Kinesio taping in stroke: improving functional use of the upper extremity in hemiplegia. Top Stroke Rehabil. 2006;13:31–42.
- Yasukawa A, Patel P, Sisung C. Pilot study: investigating the effects of Kinesio Taping in an acute pediatric rehabilitation setting. Am J Occup Ther. 2006;60:104–110.
- Karadag-Saygi E, Cubukcu-Aydoseli K, Kablan N, et al. The role of kinesiotaping combined with Botulinum toxin to reduce plantar flexors spasticity after stroke. Top Stroke Rehabil. 2010;17:318–322.
- Walsh SF. Treatment of a brachial plexus injury using kinesiotape and exercise. Physiother Theory Pract. 2010;26:490–496.
- Cortesi M, Cattaneo D, Jonsdottir J. Effect of kinesio taping on standing balance in subjects with multiple sclerosis: a pilot study. NeuroRehabilitation. 2011;28:365–372.
- Celiker R, Güven Z, Aydog T, et al. The kinesiologic taping technique and its applications. Turkish J Phys Med Rehabil. 2011;57:225–235.
- Kase K, Wallis J, Kase T. Clinical therapeutic application of the kinesio taping method. Tokyo, Japan: Ken Ikai Co Ltd; 2003.
- Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968.
- Bestall J, Paul E, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–586.
- Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatr. 1961;4:561–571.
- Hisli N. Beck Depresyon Envanteri’nin geçerliliği üzerine bir çalışma (A study on the validity of Beck Depression Inventory). Psikoloji Dergisi. 1988;6:118–122.
- Cools AM, Witvrouw EE, Danneels LA, et al. Does taping influence electromyographic muscle activity in the scapular rotators in healthy shoulders? Man Ther. 2002;7:154–162.
- Zübeyir S, Nilüfer K, Burcu C, et al. The effect of kinesiology taping on respiratory muscle strength. J Phys Ther Sci. 2012;24:241–244.
- Malehorn K, Hiniker J, Mackey T, et al. Kinesio tape® applied to the thorax augments ventilatory efficiency during heavy exercise. Int J Exer Sci. 2013;6:157–163.
- Daitx RB, Dos Santos K, Dohnert MB, et al. Limited utility of Kinesio Taping® in the physiotherapy treatment for patients with chronic obstructive pulmonary disease exacerbation. Physiother Theory Pract. 2018;34:741–746.
- Tomruk M, Keleş E, Özalevli S, et al. Effects of thoracic kinesio taping on pulmonary functions, respiratory muscle strength and functional capacity in COPD patients: a pilot randomized controlled study. European Resp J. 2017;50:PA1534.
- Wang JS, Cho KH, Park SJ. The immediate effect of diaphragm taping with breathing exercise on muscle tone and stiffness of respiratory muscles and SpO2 in stroke patient. J Phys Ther Sci. 2017;29:970–973.
- Ökmen BM, Ökmen K. Effectiveness of kinesiotaping on diaphragm thickness, diaphragmatic thickening fraction, and intercostal muscle thickness in patients undergoing mechanical ventilation: a pilot study. Europ Res J. 2019;5:68–76.
- Di Marco F, Verga M, Reggente M, et al. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir Med. 2006;100:1767–1774.
- Kömürcüoğlu B, Balioğlu M, Öztuna I, et al. KOAH’lı erkek olgularda depresyon. (Depression among male COPD patients). Toraks Dergisi. 2000;3:31–34.
- Ng TP, Niti M, Tan WC, et al. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167:60–67.