Abstract
Introduction
Erectile dysfunction is an established, well known risk of any operative management of benign prostatic hyperplasia (BPH). However, there are some cases reported in which surgical treatment has paradoxically improved erectile function. Here, we present a systematic review of the literature pertaining to the effect of surgery on sexual function, focusing on reports of improvement in erectile function following surgery.
Materials and methods
We searched PUBMED, EMBASE, Web of Knowledge, and SCOPUS databases for the following keywords: ((“sexual function” OR “erectile function”) AND “improvement” AND “benign prostatic hyperplasia” AND “surgery”).
Results
Sixteen studies (total n = 2087) were reviewed which reported a significant improvement in any aspect of erectile function. Ten of these studies had a follow-up period of 12 months or more while five had a follow up less than 12 months. Various surgical methods were included in the 16 studies; however, five reported TURP outcomes specifically. Eleven studies reported outcomes using the International Index of Erectile Function (IIEF). Overall, a further 87 studies showed no significant change and 8 studies showed a significant reduction.
Conclusions
The majority of studies report no change in erectile function following surgical intervention for BPH. There seems to be no obvious correlating factor between the studies reporting an improvement in erectile function. Further research is needed to guide us in how to consent our patients for erectile function outcomes for BPH surgery.
Introduction
Patients with benign prostatic hyperplasia (BPH) often present with varying severity of lower urinary tract symptoms (LUTS), due to the anatomical obstruction of the urethra and/or bladder neck by the prostate. These features include frequency, urgency, nocturia, hesitancy, reduced urinary flow rate, incomplete emptying and the need to double void. Prevalence of BPH is estimated as 50% of men in their 50s, and reaches 80% for men over 80 years [Citation1]. However, not all men who have radiological BPH show clinical signs of LUTS. It is estimated that 18% of men aged 40–49 years old, and 56% of men aged 70–79 years old are symptomatic of BPH, as shown by the validated International Prostate Symptom Score (IPSS) being >8 [Citation2]. The primary aim of operative management of BPH is to reduce LUTS, which ultimately improves quality of life (QoL).
It is widely accepted that surgical procedures for bladder outflow obstruction pose a significant risk of erectile dysfunction. However, a less well-researched area is the potential improvement that surgical procedures can have on sexual function. While, LUTS have a significant negative impact on QoL for patients, sexual function can also have an important role to play in a patient’s well-being and sexual dysfunction is associated with poor mood and a negative impact on relationship quality [Citation3,Citation4].
There are many surgical options and various techniques now available to treat BPH including, transurethral resection of the prostate (TURP), photoevaporisation (PVP) prostatic urethral lift (PUL). The operative method and modality of energy used may be a factor in determining whether erectile function is affected. While surgical factors must be considered, patient factors should also be considered. Initial severity of LUTS is regarded as an independent risk factor that correlates with erectile dysfunction [Citation5]. A study conducted by Ozayar et al. [Citation6] reported that in men scheduled for BPH surgery, 36% of those with moderate LUTS and 94% with severe LUTS were found to have coexisting erectile dysfunction [Citation5], with other studies quoting similar finding [Citation7]. Age has also been shown to be a significant factor in predicting erectile dysfunction, with prevalence of erectile dysfunction gradually increasing from 6.5% in men aged 20–39 years old, to 77.5% in those aged 75 years and above [Citation8]. While these factors are risks for developing erectile dysfunction, they may also be predictors of those patients likely to improve sexual function following surgical treatment of BPH.
This review evaluates the reported potential improvements in erectile function after operative management of BPH. We hope to assess whether there are any factors, which may determine these improvements.
Materials and methods
This review was conducted in accordance to PRISMA guidelines using the MEDLINE, EMBASE and Web of Science database from January 1 1900 to November 9 2017.
The keywords used in the selection were (“sexual function” [All Fields] OR “erectile function” [All Fields]) AND (“improvement” [All Fields]) AND (“benign prostatic hyperplasia” [All Fields]) AND (“surgery” [All Fields]). For the purposes of this review, although sexual function is searched as a keyword, erectile function is classified as a separate attribute to sexual function as ejaculatory function.
All duplicates and non-English studies were excluded during this review. Only original studies that had evidence of a statistically significant improvement in any aspect of erectile function after surgical intervention were included. Non-relevant studies and studies with insufficient reporting of erectile function symptoms were excluded. Studies which showed no significant change in sexual function and those that showed, at least in some aspect, a significant reduction in sexual function were included. The included studies presented validated scoring systems for erectile function such as the IIEF or a suitable equivalent system devised by the authors ().
Table 1. Studies that showed significant improvement in sexual function after intervention.
Results
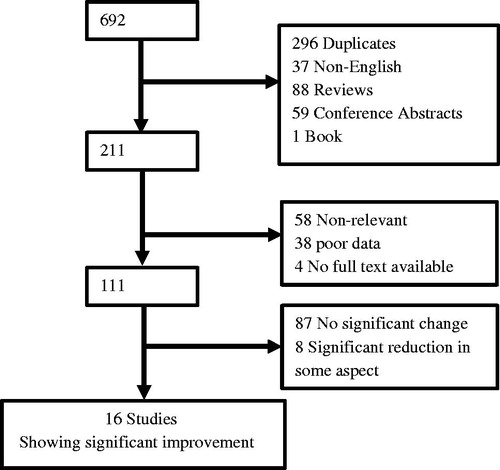
Six hundred and ninety-two studies were found from the initial search of PUBMED, EMBASE, WEB of SCIENCE, and SCOPUS databases. Two hundred and ninety-six duplicate studies were found. Thirty-seven non-English studies were excluded consisting of 11 French, 10 Chinese, five German, four Russian, three Japanese, three Italian, and one Spanish study. Eighty-eight review articles were then removed, but relevant reviews were searched for original studies and were discussed. Fifty-nine conference abstracts and one book were also removed. Fifty-eight studies which were non-relevant and 38 studies that had poor data on sexual function were then removed. Of these non-relevant studies to this review, the majority were assessing pharmacological treatment of BPH. We were unable to access the full text of four studies.
Studies were then divided into those that showed; statistically significant improvement in at least some aspect of sexual function (16 studies), no significant change in sexual function (87 studies) and those that showed a significant reduction in at least some aspect of sexual function (eight studies). The 16 studies that showed a significant improvement in at least some aspect of sexual function were mainly focused on in the discussion.
Discussion
Of the 111 original English articles which were relevant and had reliable data; 87 showed no significant change in any aspect of sexual function; eight showed a significant reduction and 16 studies showed significant improvement in some aspect of sexual function. This is interesting in light of the consensus being that surgical treatment of LUTS/BPH poses a significant risk of erectile dysfunction, hence this often features as a risk which is addressed as part of the consent process. Bearing this in mind, still the majority of these studies (87) showed no statistically significant change in erectile function following treatment, which would suggest while there is a risk of erectile dysfunction, this is relatively low and actually patients have more chance of having improvement in erectile function than reduction. Interestingly, a study conducted by Bardoli et al., focused on specific surgical technique used to treat symptomatic BPH and concluded that patients that underwent the Prostatic Urolift procedure did not suffer any sexual dysfunction side effects [Citation23].
Of the 16 studies, the techniques which showed improvement in sexual function (see ) were: Aquablation, Transurethral Enucleation of the Prostate, Prostatic Urethral Lift, Monopolar/Bipolar/Unspecified TURP, Plasmakinetic Resection of the Prostate, Prostatic Arterial Embolisation (PAE), Photovaporisation of Prostate (Greenlight PVP), Holmium Laser Enucleation of the Prostate (HoLEP), KTP photoselective vaporisation, open prostatectomy. Interestingly, although TURP is the technique mostly associated with sexual dysfunction, in this review it was the technique with the most studies showing improvement in sexual function with seven out of the 16 studies quoting this in their series.
Throughout the studies reviewed, the International Index of Erectile Function (IIEF) was the most popular method of assessing erectile function in participants, whether that be the short version (IIEF-5) or the non-altered version (IIEF-15). Eleven out of the 16 studies used IIEF-15, which in general is good as there is consistency within the community so research is more standardised making it easy to compare. Interestingly, McVary et al. [Citation11] found that participants entering with severe erectile dysfunction had significantly improved IIEF-5 scores following transurethral prostate convective water vapor thermal energy (Rezum). Henceforth, it is reasonable to deduce there could exist an indirect predictive variable between severe erectile dysfunction prior to surgery, that is the worse the erectile function prior to surgical treatment, the more the patient has to gain in erectile function due to treatment. A study conducted by Pavone et al. [Citation24] had reported a similar finding, this time using TURP. In their study, they found that no patients who had good erectile function before TURP improved their erectile function. On the other hand, 16.2% (22 out of 136 participants) of the cohort who had mild or moderate erectile dysfunction before TURP improved their erectile function; although, these results were not statistically significant.
Furthermore, it is important to note and counsel patients accordingly, that patients with normal or good erectile function initially are at more risk of having a reduction in erectile function following treatment. Bruyère et al. [Citation25] examined the effect of photoselective vaporization (PVP) of the prostate on sexual function and found that one subgroup, patients with normal preoperative erectile function, showed a significant decrease after treatment. Overall, it is safe to argue that patients with normal/good preoperative erectile function have more to lose and those with severe erectile dysfunction preoperatively have more to gain with regards to postoperative erectile function, and this is essentially could be a factor to consider when counselling patients prior to surgery.
Furthermore, although the articles which showed no statistically significant improvement in erectile function of their candidates did note that individuals or groups within their cohort in-fact improved their erectile function post-intervention. Choi et al. [Citation26] found that although overall their cohort of patients had a reduced IIEF score 3 months after TURP, which did improve to no significant change at 6 months. In addition, it was found that patients who had better voiding symptoms after TURP had improved erectile function the reasons for which remain unknown. Kim et al. [Citation27] also found a correlation where sexual satisfaction scores improved significantly with the improvements in LUTS and QoL following HoLEP. In addition to this, more novel laser techniques have been utilised in the treatment of symptomatic BPH such as Thulium Laser Enucleation of Prostate (ThuLEP); however, the long-term effects of this technique have not been fully investigated such as its effect on sexual function, rather more emphasis has been placed on the short-term outcomes such as post-operative bleeding and failed trial without a catheter (TWOC) [Citation28]. One study compared TURP, transurethral microwave thermotherapy (TUMT), interstitial laser coagulation of the prostate (ILC), and transurethral needle ablation TUNA and did report a 20.4%, 15.2%, 7.9%, and 17.1% increase in erectile function scores following the respective treatments; although, these were not statistically significant [Citation29].
Some of the excluded studies which showed no change or a reduction in erectile function could have had subgroups or a number of participants who did have an improvement in erectile function like the studies discussed above; however, they did not state this. Data on individual patient improvements would be beneficial to see any factors which would give patients a better chance of improving erectile function following treatment.
Although the 111 studies focus on assessing erectile function and of these 111, 16 showed improvement following surgical treatment, the other benefits and risks still need to be assessed for each treatment to weigh up whether overall it is suitable for the individual patient. The majority of studies did assess other outcomes such as peak urinary flow, post voidal residual volume, LUTS and QoL and in general these all did significantly improve after treatment. However, only a few studies reported on adverse effects such as retrograde ejaculation [Citation9,Citation11,Citation17] and incidence reported is between 0 and 70%. This can have impacts on patients’ fertility and is a factor of sexual function, hence again must be addressed appropriately during the consent process.
More recently, a number of studies evaluating the effectiveness of the PUL method to treat BPH showed significant improvements in ejaculatory function [Citation30–35], although they did not show any significant changes in erectile function. Importance must also be given to ejaculatory function as this may be an important factor for the patient’s psychological well-being and could be potentially considered for individual patients.
Limitations of the review
We acknowledge limitations of this review, for instance there is no single uniform definition of “sexual dysfunction”, which is used as a point of reference in the papers. In addition, throughout the review there is a variation in the use of the IIEF score. Although IIEF was the most popular method of assessing erectile function in participants, both the short version (IIEF-5) and the non-altered longer version (IIEF-15) were employed by some authors in this series. In this respect, both are validated scoring systems; however, it may affect the direct comparability of the cohorts.
Thirty-seven articles were excluded, as they were not in English with no translation available. Although unlikely, it is possible that there could have been some important data in these articles that may have changed the overall conclusion of this review.
Finally, the studies in general had good data on their participants’ baselines which included age, prostate volume, urinary flow and baseline erectile function. However, upon closer inspection other patient factors such as ethnicity, patient co-morbidities and concomitant medications were not mentioned. It would have been interesting to see if there was any correlation as to whether any patient factors had an impact on improving erectile function.
Conclusions
Although surgical intervention for BPH is assumed to have a negative impact on erectile function, this may appear to be an exaggeration of the true extent of harm and deterioration, as the majority of studies show no significant change in erectile function, with the converse of more of studies reporting an improvement. Overall, it is imperative that surgeons counsel their patients appropriately with regards to a potential risk of decline in erectile function and gain fully informed consent.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Vuichoud C, Loughlin KR. Benign prostatic hyperplasia: epidemiology, economics and evaluation. Can J Urol. 2015;22:1–6.
- Yassin A, Saad F, Hoesl CE, et al. Alpha-adrenoceptors are a common denominator in the pathophysiology of erectile function and BPH/LUTS—implications for clinical practice. Andrologia. 2006;38:1–12.
- Rosen RC, Seidman SN, Menza MA, et al. Quality of life, mood, and sexual function: a path analytic model of treatment effects in men with erectile dysfunction and depressive symptoms. Int J Impot Res. 2004;16:334–340.
- Arai Y, Aoki Y, Okubo K, et al. Impact of interventional therapy for benign prostatic hyperplasia on quality of life and sexual function: a prospective study. J Urol. 2000;164:1206–1211.
- Erkoc M, Besiroglu H, Otunctemur A. Metabolic syndrome is associated worsened erectile function in patients undergoing TURP due to benign prostatic hyperplasia. Age Male. 2016;19:111–116.
- Ozayar A, Zumrutbas AE, Yaman O. The relationship between lower urinary tract symptoms (LUTS), diagnostic indicators of benign prostatic hyperplasia (BPH), and erectile dysfunction in patients with moderate to severely symptomatic BPH. Int Urol Nephrol. 2008;40:933–939.
- Braun M, Wassmer G, Klotz T, et al. Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey’. Int J Impot Res. 2000;12:305–311.
- Saigal CS, Wessells H, Pace J, et al. Predictors and prevalence of erectile dysfunction in a racially diverse population. Arch Intern Med. 2006;166:207–212.
- Gilling P, Anderson P, Tan A, et al. Aquablation of the prostate for symptomatic benign prostatic hyperplasia: 1-year results. J Urol. 2017;197:1565–1572.
- Giulianelli R, Gentile B, Albanesi L, et al. Bipolar button transurethral enucleation of prostate in benign prostate hypertrophy treatment. A new surgical technique. Urology. 2015;86:407–413.
- McVary KT, Gange SN, Shore ND, et al. Treatment of LUTS secondary to BPH while preserving sexual function: randomized controlled study of prostatic urethral lift. J Sex Med. 2014;11:279–287.
- Zhang H-M, Zheng J-H, Xu Y-F, et al. Improvement of erectile function in patients with benign prostatic hyperplasia undergoing transurethral plasmakinetic resection of the prostate. Int J Urol. 2013;20:724–728.
- Pisco J, Campos Pinheiro L, Bilhim T, et al. Prostatic arterial emobolization for benign prostatic hyperplasia: short- and intermediate-term results. Radiology. 2013;266:668–677.
- Terrasa J‐B, Cornu J‐N, Haab F, et al. Prospective, multidimensional evaluation of sexual disorders in men after laser photovaporization of the prostate. J Sex Med. 2013;10:1363–1371.
- Elshal AM, Elmansy HM, Elkoushy MA, et al. Male sexual function outcome after three laser prostate surgical techniques: a single center perspective. Urology. 2012;80:1098–1104.
- Woo HH, Bolton DM, Laborde E, et al. Preservation of sexual function with the prostatic urethral lift: a novel treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Sex Med. 2012;9:558–575.
- Jaidane M, Arfa NB, Hmida W, et al. Effect of transurethral resection of the prostate on erectile function: a prospective comparative study. Int J Impot Res. 2010;22:146–151.
- Paick J-S, Um JM, Kim SW, et al. Influence of high-power potassium-titanyl-phosphate photoselective vaporization of the prostate on erectile function: a short-term follow-up. J Sex Med. 2007;4:1701–1707.
- Meng F, Gao B, Fu Q, et al. Change of sexual function in patients before and after Ho:YAG laser enucleation of the prostate. J Androl. 2006;28:259–261.
- Brookes ST, Donovan JL, Peters TJ, et al. Sexual dysfunction in men after treatment for lower urinary tract symptoms: evidence from randomised controlled trial. BMJ. 2002;324:1059–1061.
- Francisca EAE, d’Ancona FCH, Meuleman EJH, et al. Sexual function following high energy microwave thermotherapy: results of a randomized controlled study comparing transurethral microwave thermotherapy to transurethral prostatic resection. J Urol. 1999;161:486–490.
- Kunelius P, Häkkinen J, Lukkarinen O, et al. Sexual functions in patients with benign prostatic hyperplasia before and after transurethral resection of the prostate. Urol Res. 1998;26:7–9.
- Bardoli AD, Taylor WSJ, Mahmalji W, et al. Can the UroLift prostatic implant device treat the symptoms of benign prostatic hypertrophy, avoid sexual dysfunction and reduce hospital TURP waiting times? A single centre, single surgeon experience and review of the literature. Aging Male. 2017;20:192–197.
- Pavone C, Abbadessa D, Scaduto G, et al. Sexual dysfunctions after transurethral resection of the prostate (TURP): evidence from a retrospective study on 264 patients. Arch Ital Urol Androl. 2015;87:8–13.
- Bruyère F, Puichaud A, Pereira H, et al. Influence of photoselective vaporization of the prostate on sexual function: results of a prospective analysis of 149 patients with long-term follow-up. Eur Urol. 2010;58:207–211.
- Choi SB, Zhao C, Park JK, et al. The effect of transurethral resection of the prostate on erectile function in patients with benign prostatic hyperplasia. Korean J Urol. 2010;51: 557–560.
- Kim SH, Yang HK, Lee HE, et al. HoLEP does not affect the overall sexual function of BPH patients: a prospective study. Asian J Androl. 2014;16:873–877.
- Vazirian-Zadeh M, Anderson J, Gill R, et al. Thulium Laser Enucleation of the Prostate (ThuLEP) as a technique for treatment of BPH: evaluation of a six-year experience at a single institution. J Endolumin Endourol. 2018;1:e10–e14.
- Arai Y, Aoki Y, Okubo K, et al. Five year results of the prospective randomized controlled prostatic urethral LIFT study. Can J Urol. 2017;24:8802–8813.
- Roehrborn CG, Rukstalis DB, Barkin J, et al. Prospective, randomized, multinational study of prostatic urethral lift versus transurethral resection of the prostate: 12-month results from the BPH6 study. Can J Urol. 2015;22:7772–7782.
- Rukstalis D, Rashid P, Bogache WK, et al. Three year results of the prostatic urethral L.I.F.T study. Br J Urol. 2016;3:14–22.
- Sønksen J, Barber NJ, Speakman MJ, et al. Prospective multi-center study elucidating patient experience after prostatic urethral lift. Eur J Urol. 2015;68:643–652.
- Shore N, Freedman S, Gange S, et al. Prostatic urethral lift: two-year results after treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Can J Urol. 2014;21(1):7094–7101.
- Chin PT, Bolton DM, Jack G, et al. Prostatic urethral lift: two-year results after treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Urology. 2012;79:5–11.
- Jones A, Phan YC, Mahmalji W. UroLift for the treatment of lower urinary tract symptoms in a patient with AMS 700 MS implanted penile prosthesis. The first reported case in the literature. J Endolumin Endourol. 2019;2:e5–e12.
- Giulianelli R, Albanesi L, Attisani F, et al. Comparative randomized study on the efficaciousness of endoscopic bipolar prostate resection versus monopolar resection technique: 3 year follow-up. Andrologia. 2013;85:86–91.
- Gacci M, Bartoletti R, Figlioli S, et al. Urinary symptoms, quality of life and sexual function in patients with benign prostatic hypertrophy before and after prostatectomy: a prospective study. BJU Int. 2003;91:196–200.