Abstract
Introduction
We aimed to evaluate plasma thiol and disulphide levels as an additional marker to prostate specific antigen (PSA) in the diagnosis of prostate cancer (PCa).
Methods
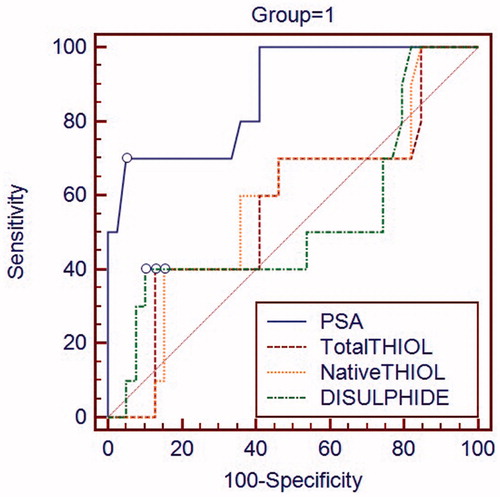
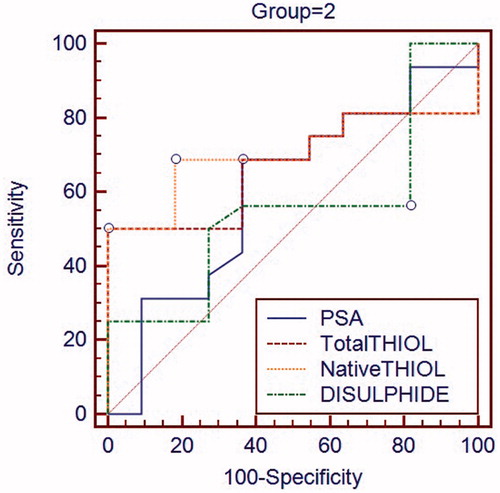
Between March 2017 and January 2018 prospective study was conducted among patients with PSA levels of 2.5–20 ng/mL without suspicion of malignancy in rectal examination and who underwent prostate needle biopsy. Patients were divided into two groups according to PSA level as 2.5–10 ng/mL (Group 1) and 10.01–20 ng/mL (Group 2). Diagnostic efficacy of thiol, disulphide and PSA levels were measured by ROC analysis.
Results
A total of 76 patients were included in the study. There were 49 patients in group 1 and 27 patients in group 2. There was no significant difference between two groups in terms of PSA density and prostate size. In Group 1, area under curve (AUC) was higher in PSA than other parameters with statistically significant difference (p<.05). In group 2, AUC of native and total thiol was higher than PSA but there was no statistically significant difference for AUC in parameters.
Conclusions
We think that plasma thiol test may be used in diagnosis of prostate cancer while PSA levels between 10 to 20 ng/mL. However, further studies are required.
Introduction
Prostate cancer (PCa) is the most common cancer in men after skin cancers and accounts for the second-highest morbidity rate in men [Citation1,Citation2]. Tumor markers have been more frequently used in the diagnosis of PCa than in the diagnosis of other urological malignancies. The use of prostate specific antigens (PSA) as tumor markers in PCa has led to a rise in the diagnosis of non-palpable T1c stage PCa that could not be previously diagnosed [Citation3]. Conversely, Stamey and colleagues demonstrated that elevated PSA levels were associated with advanced stage PCa, and further studies have supported this association [Citation4–6]. Unnecessary biopsies and post-biopsy complications due to elevated PSA levels may pose a significant problem. However, diagnosis and treatment of clinically insignificant cancer on the basis of PSA screening results also put the patients under the risk of unwanted complications as well as surgical risk of radical prostatectomy. Researchers have searched for a new marker because the specificity and sensitivity of the PSA test were not very high in the diagnosis of PCa. In addition to serum PSA level measurements, techniques such as free PSA/total PSA ratio, prostate cancer antigen-3, prostate health index, 4 K score, PSA velocity, and PSA doubling time have been developed to avoid unnecessary biopsies and detecting clinically significant PCa.
Oxidative stress due to excessive production of reactive oxygen species causes damages to DNA, protein, and lipids. Oxidative protein damage causes irreversible modifications in serum and tissue proteins. Thiols are essential and potent anti-oxidant molecules containing a functional sulfhydryl group protecting organism against the harmful effects of oxidative stress damage. In 2014, Erel et al. defined thiol/disulphide homeostasis for the first time and demonstrated its measurability in serum [Citation7]. These disulphide bonds can be reduced back to the thiols, resulting in the formation of a dynamic thiol/disulphide homeostasis, which plays a crucial role in antioxidation, and, therefore, it is believed that to play a role in the pathogenesis of numerous diseases such as diabetes, coronary artery disease, and cancer [Citation8–10]. We also investigated the clinical importance of thiol and disulphide in patients with 2.5 and 20 ng/mL PSA levels. According to the results of our literature search, this is the first known study on the comparison of thiol, disulphide and PSA in the diagnosis of PCa thus our study provides original data on this important issue. The present study, plasma native thiol, total thiol, and disulphide levels were investigated as an alternative marker to PSA in the diagnosis of PCa in our tertiary referral center.
Material and methods
The study was prospectively conducted in patients who applied to urology outpatient clinic between March 2017 and January 2018 and who were scheduled for prostate biopsy after receiving written informed consent from all patients because of elevated PSA levels. The study was conducted in accordance with the Declaration of Helsinki and approved by the local ethical committee. Blood samples were collected from all patients prior to biopsy for evaluation of serum all thiol types and disulphide levels. The patients who had a PSA level was between 2.5 and 20 ng/ml with normal rectal examination were included in the study. Patients were divided into two groups according to the PSA level as 2.5–10 ng/mL (Group 1) and 10.01–20 ng/mL (Group 2). Prostate density has calculated the division of PSA level to the prostate weight.
Patients with a history of long-term urethral catheterization, a recent anamnesis of urinary infection, a history of uncorrected coagulopathy, a myeloproliferative disease, high PSA level (>20 ng/ml), prostate malignancy suspicion after prostate examination and PCa with metastases detected in the imaging procedures were excluded from this study. Single-dose antibiotic prophylaxis (ciprofloxacin 1 g) and distal gastrointestinal system cleaning (rectal enema 135 cc) were applied to all the patients one hour before the biopsy. After transrectal ultrasound examination, prostate biopsy was performed on all 12 quadrants of prostate under intrarectal local anesthesia (lidocain 5–10 ml %10) with a 25 cm 18 Gauge Tru-Cut needle powered by an automatic spring-loaded disposable biopsy gun. All procedures were performed in outpatient settings and the antibiotic prophylaxis was continued for additional three days. Post biopsy, all specimens were evaluated by the same uropathologist.
Statistical analyses
The data were verified for normal distribution using Kolmogorov-Smirnov test and expressed as mean ± standard deviation (normal distribution), median values and p < .05 as considered with statistical significance. The independent sample t-test, Mann–Whitney U and Chi-squared test were used for comparison of the groups. The receiver operating characteristic (ROC) curves were analyzed to assess the diagnostic efficacy of total PSA, total thiol, native thiol and disulphide (MedCalc Statistical Software demo version 16.2.0, Ostend, Belgium; https://www.medcalc.org; 2016).
Results
There were 76 patients in this prospective study with a mean age of 62.88 ± 7.91 years. Of these patients, 49 were in Group 1 and 27 were in Group 2. Prostate volume ranged from 24 to 152 ml, with a mean of 66.97 ± 23.75 ml. Total thiol, native thiol, and disulphide levels were higher in Group 1 than Group 2; however, no significant difference was detected (). Prostate weights were bigger in the group 2 than group 1 but there was no statistically significant difference between two groups in terms of prostate size (). Detection of prostate cancer was higher in Group 2. The diagnostic efficacy of thiol, disulphide and PSA levels were measured by ROC analysis. ROC analyzes of both groups are shown in and . In Group 1, area under curve (AUC) was higher in PSA test than the other parameters (total thiol, native thiol, and disulphide) with statistically significant difference (p < .05). shows the AUC values and comparative results of all parameters. In group 2, AUC of native and total thiol was higher than PSA but there was no statistically significant difference for AUC in the parameters.
Table 1. Comparison of total thiol, native thiol and disulphide values between Group 1 and Group 2.
Table 2. Comparative results of groups after receiver operating characteristic (ROC) analysis.
Discussion
The diagnostics of prostate cancer is complicated because of cancer heterogeneity and differentiated progression in various subgroups of patients. The introduction of PSA in the diagnosis and screening of PCa has markedly increased the rate of PCa diagnosis. However, prospective studies comprising large series with long-term follow-up have demonstrated that quality of life decreased owing to over-diagnosis, over-treatment, and related complications because of the diagnosis of clinically insignificant PCa [Citation11–17]. Furthermore, unnecessary biopsies and treatment and related complications caused cost-effectiveness and reduce the quality of life. In a study, 76,693 men aged between 55 and 74 years were divided into two groups and annual serum PSA levels were measured in the screening group [Citation18]. In this study, prostate biopsy was performed on individuals with PSA levels of more than 4 ng/mL and/or positive findings in rectal examination. No significant difference was noted in PCa mortality rate between the screening and control groups in the 7-and 13-year follow-ups [Citation18]. In a study including 162,243 men from seven European countries aged between 55 and 69 years were followed up for 9 years [Citation15]. The authors reported a 20% decrease in PCa mortality rate using PSA-based screening. They also reported that 48 patients had to be treated and 1410 patients had to be screened for preventing a single mortality from PCa and that PSA screening was associated with a high risk of over-diagnosis [Citation11–19]. For the 11- and 13-year follow-ups, decrease in mortality rate was 21% and 29%, number of men to be screened was 1055 and 781, and number of patients to be treated were 37 and 27, respectively [Citation11–19].
Taking the above-mentioned information into consideration, urologists required alternative new biomarkers and techniques, such as free PSA/total PSA ratio, prostate cancer antigen-3, prostate health index, 4 K score, PSA velocity, and PSA doubling time, to complement PSA for detecting and treating patients with clinically significant PCa. In addition, multiparametric magnetic resonance imaging, an imaging technique that has been increasingly used in recent years and included in the urology guidelines, issued for performing biopsy on patients requiring the procedure and for effective active monitoring on patients during follow-ups. The use of the GRADE-GROUP classification in addition to the Gleason classification by pathologists in the diagnosis of PCa can facilitate the detection of clinically significant PCa. In our presented study, the role of thiol and disulphide levels were investigated for diagnosing PCa, which we consider may be as sensitive as, but more specific than, PSA. To our best knowledge, this is the first study that could be an alternative to PSA when PSA levels were between 10 and 20 ng/mL.
Dynamic thiol-disulphide homeostasis has a critical role within the organism and thiol/disulphide balance has been associated with several disorders such as diabetes mellitus, cancer, migraine, hyperemesis gravidarum, obstructive sleep apnea and chronic renal failure [Citation20,Citation21]. In a recent study, authors investigated the role of thiol/disulphide homeostasis in the differentiation of benign diseases and PCa and found that total thiol and native thiol levels were significantly higher in patients with PCa than in those with benign diseases [Citation22]. In our study, although not statistically significant we demonstrated that when PSA levels were between 10 and 20, total thiol and native thiol levels were found to be high. Based on this information, in these cases, we think that thiol and disulfide levels can be measured as a novel marker, and thus unnecessary biopsy can be prevented. In a study, the authors evaluated thiol/disulphide homeostasis prior to and 6 months following radical prostatectomy in patients with PCa and reported that decreased thiol and total antioxidant status levels weakened anti-oxidant defence mechanism in the patients with prostate cancer as indicated and increased oxidative stress in prostate cancer patients may cause metabolic disturbance and have a role in the aetiopathogenesis of prostate cancer [Citation23]. In a recent study investigated ischemia modified albumin (IMA) levels and inflammatory biomarkers in patients with prostate tumour [Citation24]. This study and control groups comprised of 25 patients with PCa and 30 healthy individuals, respectively. The results of this retrospective study revealed that the C-reactive protein, IMA, and PSA levels were higher and free PSA and frap levels were lower in the PCa group than in the control group. As a conclusion, the authors of this study demonstrated that both inflammatory and oxidative processes are increased during prostate tumour and there is a reduction of antioxidant defenses in prostate tumour pathology [Citation24]. Taken together, the author reported that elevated oxidative stress and inflammation were reportedly effective in the pathogenesis of PCa [Citation24].
The limitations of our study include the absence of a control group of healthy individuals and low number of study population especially in Group 2. Another limitation of our study is that chronic ischemic and systemic inflammatory diseases, smoking, alcohol and using antioxidant supplements were not excluded from the study because these conditions may have effects on plasma thiol and disulfide level.
Conclusions
In PSA based PCa screening, certain complications, such as unnecessary biopsy, over-diagnosis, over-treatment, and a subsequent decrease in quality of life, occur. The use of a marker with high specificity in conjunction with PSA may aid in reducing frequency of these complications. Although not statistically significant, we found that total and native thiol levels were higher than PSA in patients with PSA levels between 10 and 20 ng/mL. Based on this result we think that thiol may be used as an alternative marker while PSA level 10 to 20 ng/mL. Large-scale, prospective, and randomized studies are needed for obtaining more accurate results on this topic.
Ethical approval
Institutional review board (IRB) approval was acquired from our university’s ethics committee in Istanbul, Turkey. Also, informed consent was obtained from all individual participants included in the study. All procedures performed in studies were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA A Cancer J Clin. 2019;69:7–34.
- Yassin A, Nettleship JE, Talib RA, et al. Effects of testosterone replacement therapy withdrawal and re-treatment in hypogonadal elderly men upon obesity, voiding function and prostate safety parameters. Aging Male. 2016;19:64–69.
- Diamandis EP, Yousef GM, Luo LY, et al. The new human kallikrein gene family: implications in carcinogenesis. Trends Endocrinol Metab. 2000;11:54–60.
- Stamey TA, Yang N, Hay AR, et al. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N Engl J Med. 1987;317:909–916.
- Catalona WJ, Smith DS, Ratliff TL, et al. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med. 1991;324:1156–1161.
- Brawer MK, Chetner MP, Beatie J, et al. Screening for prostatic carcinoma with prostate specific antigen. J Urol. 1992;147:841–845.
- Erel O, Neselioglu S. A novel and automated assay for thiol/disulphide homeostasis. Clin Biochem. 2014;47:326–332.
- Altıparmak IH, Erkuş ME, Sezen H, et al. The relation of serum thiol levels and thiol/disulphide homeostasis with the severity of coronary artery disease. Kardiol Pol. 2016;74:1346–1353.
- Ergin M, Aydin C, Yurt EF, et al. The variation of disulfides in the progression of type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 2018. DOI:10.1055/s-0044-100376
- Karatas F, Acat M, Sahin S, et al. The prognostic and predictive significance of serum thiols and disulfide levels in advanced non-small cell lung cancer. Aging Male. 2019;1–10. DOI:10.1080/13685538.2018.1559805
- Andriole GL, Crawford ED, Grubb RL, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009;360:1310–1319.
- Andriole GL, Crawford ED, Grubb RL, et al. Prostate cancer screening in the randomized prostate, lung, colorectal, and ovarian cancer screening trial: mortality results after 13 years of follow-up. J Natl Cancer Inst. 2012;104:125–132.
- Schroder FH, Hugosson J, Roobol MJ, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360:1320–1328.
- Schroder FH, Hugosson J, Roobol MJ, et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med. 2012;366:981–990.
- Schroder FH, Hugosson J, Roobol MJ, et al. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet. 2014;384:2027–2035.
- Coban S, Doluoglu OG, Keles I, et al. Age and total and free prostate-specific antigen levels for predicting prostate volume in patients with benign prostatic hyperplasia. Aging Male. 2016;19:124–127.
- Erdogan A, Polat S, Keskin E, et al. Is prostate volume better than PSA density and free/total PSA ratio in predicting prostate cancer in patients with PSA 2.5–10 ng/mL and 10.1–30 ng/mL? Aging Male. 2019;12:1–7.
- Marcus PM, Ogden SL, Gren LH, et al. Non-compliance with the initial screening exam visit in the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial. Prev Med. 2014;67:82–88.
- Lilja H, Cronin AM, Dahlin A, et al. Prediction of significant prostate cancer diagnosed 20 to 30 years later with a single measure of prostate-specific antigen at or before age 50. Cancer. 2011;117:1210–1219.
- Eren Y, Dirik E, Neşelioğlu S, et al. Oxidative stress and decreased thiol level in patients with migraine: cross-sectional study. Acta Neurol Belg. 2015;115:643–649.
- Dikis OS, Acat M, Casim H, et al. The relationship of thiol/disulfide homeostasis in the etiology of patients with obstructive sleep apnea: a case-control study. Aging Male. 2019;1–8. DOI:10.1080/13685538.2019.1573890
- Sonmez MG, Kozanhan B, Deniz ÇD, et al. Is oxidative stress measured by thiol/disulphide homeostasis status associated with prostate adenocarcinoma? Cent Eur J Immunol. 2018;43:174–179.
- Hanikoglu F, Hanikoglu A, Kucuksayan E, et al. Dynamic thiol/disulphide homeostasis before and after radical prostatectomy in patients with prostate cancer. Free Radic Res. 2016;50:79–84.
- Da Silveira RA, Hermes CL, Almeida TC, et al. Ischemia-modified albumin and inflammatory biomarkers in patients with prostate cancer. Clin Lab. 2014;60:1703–1708.