Abstract
Men ignore self-care, displaying low frequency in health services. Aging increases the prevalence of LUTS and BPE, impacting the quality of life. The objective is to understand how the advancement of age can be determinant for men's health in Natal, Brazil. Then, 503 men aged between 43 and 83 attended the Blue November Campaign of 2015. All subjects were submitted to anamnesis, clinical and laboratorial evaluation including measuring their blood pressure, waist circumference, glucose, total cholesterol, HDL-C, LDL-C, triglycerides and BMI was calculated. In addition, IPSS, PSA, IIEF-5 and DRE data were collected. The mean IPSS presented an increase with age, 43–59 years (6.28 ± 6.02) and 70–80 years or more (8.65 ± 5.80). PSA dosages increase with aging (adult group 1.63 ± 2.70), being more accentuated in the older group (4.66 ± 5.70), while the mean IIFE-5 showed a decrease with aging in 43–59 years (21.79 ± 4.67) and an important decrease at 70–80 years or more (16.24 ± 6.71). The number of DRE > 30 g showed significant growth in the older group. All presented statistical significance (p < .05) and were associated with aging. The Blue November Campaign creates an annual self-care opportunity for aging men as their health is gradually affected.
Introduction
Aging is defined as a dynamic and progressive process in which morphological, functional, biochemical and psychological changes occur which determine the progressive loss of the individual’s adaptive capacities to the environment, causing greater vulnerability and a greater incidence of pathological processes [Citation1].
Lower urinary tract symptoms (LUTS) are a common, age-related condition in men, characterized by urinary frequency, urgency, decreased force of stream, and nocturia. LUTS have a major impact on the quality of life and cause a substantial economic burden. They have traditionally been related to bladder outlet obstruction (BOO), which is often caused by benign prostatic enlargement (BPE) resulting from the histological condition of benign prostatic hyperplasia (BPH) [Citation2].
The prevalence of LUTS in community samples and in clinic attendees has been extensively evaluated worldwide [Citation3]. The increasing prevalence of LUTS with age represents a particularly concerning public health issue [Citation4]. LUTS and BPE have a major impact on public health and medical care expenditures [Citation5]. Men do not highly value illness and they have low self-care discipline, which distance them from access to health services. They tend to choose hospital services, private practices and emergency care or emergency services [Citation6]. In Brazil, the National Policy on the Health of Older Adults comprises a set of both individual and collective health actions covering health promotion and protection, disease prevention, diagnosis, treatment, rehabilitation and health maintenance [Citation7]. The Blue November Campaign is part of these actions and includes a set of awareness strategies on the importance of prevention and early diagnosis of diseases that affect the male population, especially the most prevalent [Citation8].
Much evidence suggests that other than aging, modifiable factors such as increasing prostate volume, obesity, diet, dyslipidemia, hormonal imbalance, hypertension, metabolic syndrome (MetS), alcohol and smoking also contribute to the development of LUTS and/or BPH. More recently, studies have suggested that these patients easily develop erectile dysfunction (ED) [Citation9].
Considering that LUTS have a negative impact on health-related quality of life and are associated with high personal and societal costs [Citation10] and also impacts a decline in sex life, mainly combined with the absence of self-care by the male public, low attendance to health service, and due to the scarcity of data in Brazil. This study has the objective to understand how the advancement of age can be determinant for men's health in Natal, an urban area in northeastern Brazil. The study assumes an important role by the Blue November Campaign in the male public’s adhesion, health diagnosis, self-care motivation and the establishment of an annual monitoring routine of male health for aging men.
Material and methods
Study population
The present is a descriptive cross-sectional study based on an urban community sample of men aged 40 years or older, invited between November 2015 and April 2016 through television advertisements seeking volunteers to take part in the Blue November Campaign of 2015 prevention of male diseases awareness program, promoted by the University Hospital Onofre Lopes. A total of 503 men who agreed to participate in the study signed the informed consent form. Next, these men who accepted the invite on the Blue November Campaign of 2015 were included in the study and all were submitted to anamnesis, clinical and laboratory evaluation and LUTS data were collected by the International Prostate Symptom Score (IPSS) of the American Urological Association (AUA), of BPE by digital rectal examination (DRE) of the prostate and prostate specific antigen (PSA), erectile function (EF) by an abridged 5-item version of the International Index of Erectile Function (IIEF-5).
The research was carried out according to the Norms and Ethical Guidelines of the National Health Council Resolution 510/2016 of the Brazilian Ministry of Health, and approved by the Research Ethics Committee of the University Hospital Onofre Lopes; Federal University of Rio Grande do Norte in 2014 with Certificate of Presentation for Ethical Appreciation (CAAE) 25997913.1.0000.5292.
Measurements
Blood pressure was measured in the clinical evaluation with a mercury sphygmomanometer applied to the left arm, with the subject in the sitting position. Waist circumference (WC) was measured using an inelastic measuring tape at the midpoint between the iliac crest and the lowest rib, with the patient standing. Body mass index (BMI) was calculated by dividing the subject’s weight in kilograms by the square of their height in meters (Kg/m2) using a Filizola automatic anthropometric scale (São Paulo, SP, Brazil) calibrated by INMETRO.
Blood samples were drawn after overnight-fasting and using automated methods and commercially available assays at the Laboratory of Clinical Analysis of the University Hospital Onofre Lopes. We measured FG using the enzymatic test kit AA, and lipid profile (including TG by the enzymatic test kit GOP/PAP AA, total cholesterol by the enzymatic test kit AA, HDL-C by colorimetric test kit monofase AA plus all by Wiener Lab, Rosario, Argentina in automated Wiener Lab CMD 800 iX1 equipment). LDL-C was calculated according to the Friedewald formula and PSA was assessed by a microparticle chemiluminescence immunoassay (Architect, Sligo, Ireland).
LUTS were classified into three symptom categories: mild (0–7 points), moderate (8–19 points) and severe (>19 points). DRE evaluated the size and texture of the prostate, being classified as normal ≤30 g (one digital pulp), or increased >30 g (two or more digital pulps) and with nodules, respectively. EF was classified into five categories: normal (25 to 22 points), mild to moderate (16 to 11 points) moderate (10 to 8 points) and severe (7 to 5 points).
Statistical analysis
Continuous variables were described using means ± standard deviation. Analysis of variance with the post hoc Tukey’s test was used to compare means across age groups, and the Fisher’s exact test to compare proportions. Statistical significance was assumed with p < .05. Data analysis was performed using Stata 13 (Stata Corp., Collegue Station, TX, USA).
Results
The Blue November Campaign is directed to the prevention of male diseases; therefore, the socio-demographic profile of the population was mostly male. The public of the present study consisted of men living in the metropolitan area of the city of Natal, Rio Grande do Norte, northeastern Brazil, and the age group comprised 43–83 years.
The study evaluated a sample of 503 men with a mean age of 57.35 ± 6.85 years, measuring systolic and diastolic blood pressure and WC, calculating BMI and also analyzed glucose, total cholesterol, HDL-C, LDL-C and triglycerides, with their means shown in . For systolic and diastolic blood pressure, the mean values were 136.75 ± 20.21 and 84.51 ± 13.83, respectively, while WC presented a mean of 100.38 ± 10.82 and BMI of 28.15 ± 4.09. The means for biochemical analyzes were glucose (123.21 ± 75.10), total cholesterol (217.81 ± 44.63), HDL-C (44.62 ± 11.89), LDL-C (136.68 ± 35.84) and triglycerides (189.57 ± 126.35).
Table 1. Baseline characteristics of study participants.
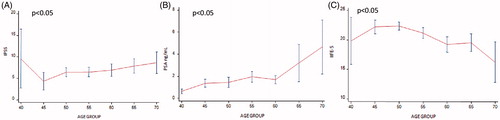
Mean IPSS, PSA and IIFE-5 results were related to age groups and are presented in . IPSS showed the following averages: 40 years (9.57 ± 7.68); 45 years (4.34 ± 6.06); 50 years (6.42 ± 6.34); 55 years (6.46 ± 6.68); 60 years (6.92 ± 6.97); 65 years (7.86 ± 6.41); and 70 years (8.65 ± 5.80). Statistical significance was found between IPSS and age (p < .05), indicating that increase in IPSS is associated with aging. We observed an initial decrease followed by an increase from 45 years, a little increase at 50 years, a higher increase at age 60, with an important increase at age 65, and the highest increase at 70 years. The mean of the PSA dosage values were: at 40 years (0.63 ± 0.23); 45 years (1.36 ± 1.01); 50 years (1.44 ± 2.82); 55 years (1.99 ± 2.88); 60 years (1.69 ± 1.86); 65 years (3.21 ± 6.53); and 70 years (4.66 ± 5.70). We found a statistically significant association between PSA dosage and age increase (p < .05). A little increase was observed from 40 years until 55 years, a decrease at 60 years, a relevant increase at 65 years, and the highest increase at 70 years. In addition, the means for IIFE-5 presented: at 40 years (19.86 ± 4.45); 45 years (22.23 ± 3.40); 50 years (22.35 ± 4.22); 55 years (21.16 ± 5.32); 60 years (19.25 ± 6.25); 65 years (19.53 ± 5.54); and 70 years (16.24 ± 6.71). Statistical significance was found between IIFE-5 and aging (p < .05), indicating that a decrease in IIFE-5 is associated with increasing age. We observed a decrease with the age groups, being unchanged between the 45 and 50-year-old group, with a short decrease at 55 years, again unchanged at 60 and 65 years, and an important decrease from 65 and 70 years.
Figure 1. Genitourinary signs and symptoms of men from Blue November Campaign 2015 by age group. (A) Mean of IPSS by age group. (B) Mean of PSA by age group. (C) Mean of IIEF-5 by age group.
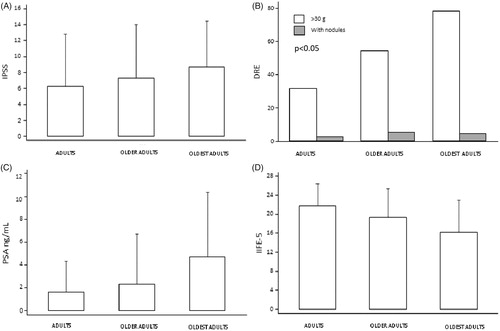
In order to enable observation of IPSS, DRE, PSA and IIFE-5 changes during aging, the sample of the present study was categorized into three age groups: adults (43 to 59 years), older adults (60 to 69 years) and oldest adults (70 to 80 years or more) (). The presented means of IPSS for the adults (6.28 ± 6.02), older adults (7.29 ± 6.75) and oldest adults (8.65 ± 5.80) age groups had no statistically significant values (p > .05), possibly due to the mean age being 58 years old. DRE > 30 g demonstrated statistically significant growth with aging (p < .05). DRE > 30 g had twice the frequency in the oldest adults group, while DRE with nodules remained almost unchanged between the aging groups. The PSA means were not statistically different (p > .05) between adults (1.63 ± 2.70) and older adults 2.29 ± 4.39, but were higher (<.05) in the oldest adults group (4.66 ± 5.70). The means of IIFE-5 presented for the adults (21.79 ± 4.67), older adults (19.36 ± 5.97) and oldest adults (16.24 ± 6.71) age groups showed a statistically significant decrease with aging (p ≤ .05).
Figure 2. Changes of genitourinary signs and symptoms of men from Blue November Campaign 2015 by aging group: adults (43 to 59 years), older adults (60 to 69 years) and oldest adults (70 to 80 years or more). (A) Mean of IPSS by aging group. (B) Number of DER > 30 g by aging group. (C) Mean of total PSA by aging group. (D) Mean of IIEF-5 by aging group.
Discussion
Aging in Brazil
The process of demographic change that occurred in Brazil since 1940 evidenced a decline in mortality and subsequent decline in fertility, increasing the presence of adults and older adults. The rapidly changing age structure determines the new profile of demand for social policies, since chronic degenerative noninfectious diseases characteristic of adults have increased. Observational studies have shown a narrow association between qualitative characteristics of the diet and the occurrence of chronic-degenerative diseases such as cardiovascular diseases, non-insulin dependent diabetes mellitus, different types of cancers and even obesity [Citation11].
The National Health Survey of 2013 evaluated the nutritional status of the Brazilian adult population by assessing BMI, which increased with age in both genders, and showed that the prevalence of overweight category for men was 57.3%, while it was 17.5% for obesity. Abdominal obesity was also evaluated, measuring WC and considered increased for males with WC ≥ 102 cm. The prevalence found increases with age, reaching 35.0% in the age group above 55 years old [Citation12]. The Blue November Campaign is a strategy used by the Brazilian Ministry of Health for the prevention of more prevalent male diseases which affect men after 45 years of age, being the onset of the aging process [Citation8].
Men seek less basic healthcare services and choose hospital services, private clinics and emergency care or services. A study performed in a basic health service in Niterói city showed that only 180 adult males, 56% registered, sought care [Citation6]. The Blue November Campaign contributed to greater adhesion by the urban male adult population living in Natal city to basic healthcare, totaling 503 men. Our study showed the mean age of the participants as 57 years old, with the majority being at the onset of aging.
Aging, lower urinary tract symptoms (LUTS), benign prostate enlargement/hyperplasia (BPE/BPH) and erectile function (EF)
Aging as a process has been discovered to be associated with the development of various symptoms of different organ systems in the body, including the genitourinary tract. Age was reported to be one of the most reliable risk factors for the progression of LUTS/BPH. Its influence is greater than those of other sociodemographic characteristics. The conditions leading to LUTS are among the most prevalent diseases in older adults, with serious impairment to quality of life [Citation13]. LUTS represent one of the most common and bothersome conditions seen in daily urologic practice, affecting at least one in every four men older than 40 years old [Citation10]. Studies conducted with cohorts of men have shown that the prevalence of LUTS increase with aging. In Germany it increased to 33.8% about 4 years later [Citation14], and in Austria, 50% of men have reported worsening of the symptoms within a 5-year period [Citation15].
A study conducted in five countries (Canada, Germany, Italy, Sweden, and the United Kingdom) reported the prevalence of LUTS in the survey population, with all symptoms among men increasing with advancing age, especially for those ≥60 years of age [Citation16]. Another study with men who live in Nigeria also showed that the severity of IPSS increases with age and was significantly worse among subjects of 65 years and above (p < .001), with serious impairment to quality of life [Citation13].
In the Boston Area Community Health (BACH) Survey, LUTS prevalence increased markedly with age from 8% in men 30 to 39 years, to 35% in men 60 to 69 years [Citation17]. Similarly, in the European and Korean UrEpik study, the prevalence of male LUTS increased 10% per decade from 40 to 79 years of age [Citation18].
Prostate growth and enlargement and clinically significant LUTS are extremely common in aging men, as prostatic hyperplasia is evident in 50% of men aged 51 to 60 years, while almost half of all men will develop clinically significant LUTS as they age. The prevalence of benign prostate enlargement BPE/BPH and LUTS rises markedly with aging. It is estimated that nearly 50% of all men at the age of 60 have histological BPH, and the prevalence approaches 90% by 80 years of age [Citation10].
More recently, ED has been linked to LUTS/BPH as a part of this syndrome, suggesting that patients with BPH or LUTS easily develop ED, and that LUTS/BPH symptoms often coexist with ED [Citation8]. Although LUTS and ED are common disorders in aging men, they are independently associated with each other [Citation19].
A large number of clinical population-based and longitudinal studies have shown a strong correlation between ED and LUTS. Researchers using collected data from the National Health and Nutrition Examination Survey (NHANES) showed that Hispanic men were more likely to report ED, with prevalence increasing steadily from 6.5% in men aged 20–39 years to 77.5% in those 75 years and older, while the presence of LUTS in 2858 Austrian men aged 20-80 years, in particular voiding symptoms, nocturia and quality of life impairment due to LUTS were independent risk factors for the presence of ED [Citation20].
One in five subjects suffered from ED in a Cologne Male Survey, a study including approximately 5000 German men aged 30-80 years. The prevalence of LUTS was 72% in men with ED versus 38% in those without ED [Citation21]. The Multinational Survey of the Aging Male (MSAM-7) conducted in the US and six European countries (the UK, France, Germany, the Netherlands, Italy, and Spain) indicated a link between ED and LUTS, with ED being more prevalent in patients with increasing LUTS complaints. Only a quarter of men who had no LUTS suffered from ED, while four in five men with severe LUTS had reduced or no erections [Citation22]. A clinical trial (MTOPS Study) reported a strong correlation between baseline American Urological Association symptom index and the various domains of sexual function. The association between LUTS and ED was examined prospectively in 17,086 men in a health professionals follow-up study. The risk of ED increased with rising LUTS severity, with stronger correlation in younger than in older men [Citation23]. The Asian Survey of Aging Males (ASAM) study was carried out in Asian men aged 50-80 years from five Asian countries (Hong Kong, Singapore, Malaysia and, Philippines and Thailand), with the results showing higher prevalence of ED and ejaculatory dysfunction in groups of diabetic and hypertensive patients [Citation24].
Our study showed a higher percentage with light LUTS (score 0–7) and BPE/BPH in the normal category (DRE 30 g and PSA value in all age groups within the values of reference). The IIFE-5 normal category (score 25–22) also presented a higher percentage in ED. The association observed between aging, LUTS, BPE/BPH does not match that described in the literature, while aging/ED association confirms the independence between them described in the studies.
Among the main potential risk factors for LUTS/BPH and ED beyond aging, such as hypertension and cardiovascular disease, hyperlipidemia, type-2 diabetes mellitus, obesity/waist circumference, we also have hypogonadism (aggravating factors) and genetic predisposition (conditioning factors) [Citation9]. Several studies demonstrated that androgen replacement therapy improves the LUTS/BPH parameters, obesity and metabolic syndrome [Citation25–29]. The prostate is also influenced by serum vitamin D levels [Citation30]. Scientific evidence that Serum vitamin D levels affect the prostate size and the relationship between LUTS/BPH have been shown in various cross-sectional [Citation30–32] and molecular studies [Citation33,Citation34]. Thus, we should also pay attention to sex hormones levels and vitamin D status as an integral part of the general health of the aging male.
Lower urinary tract symptoms (LUTS) benign prostate enlargement/hyperplasia (BPE/BPH) and metabolic syndrome (MetS)
Our study investigated a community-based sample of men ≥43 years old with no specific symptoms or previous diagnosis of LUTS. We found no evidence of an association between LUTS or signs of BPE/BHP and MetS. In the same way, studies conducted among non-institutionalized men in Guangxi, China [Citation3], Seoul, Korea [Citation35,Citation36], Japan [Citation37], Vienna [Citation38] also found no association between LUTS and MetS.
The investigation of a possible association between LUTS-BPE/BPH and MetS is complex because it is mainly based on patients with LUTS referred from urology clinics. However, additional epidemiological studies with long-term follow-up are necessary to determine the role of MetS and other individual components in the etiopathogenesis of LUTS-BPE/BPH to better understand their role as possible risk factors for the development and progression of these symptoms, and to identify new therapeutic targets and create novel strategies for managing LUTS and BPE/BPH.
The Blue November Campaign as a self-care strategy and annual men's health agenda
Male health-related behaviors can help to explain higher mortality, lower adherence to preventive actions, and lower frequency of health services in the male population [Citation39]. Care for oneself, appreciation of the body for the meaning of health, and care for others are not questions put forth in the socialization of men [Citation40]. The Blue November Campaign is a health strategy for the male population to promote elucidation of total healthcare of the general man and to establish an annual routine of medical consultations from age 45 [Citation41].
Although technology for health diagnoses have expanded, the male public still has a strong resistance to self-care. Therefore, adherence to the invitation to participate in the Blue November Campaign was successful and enabled evaluating a significant number of men for the presence of prevalent diseases and comorbidities that affect the aging process. Though trends of signs and symptoms behaved as expected in male aging, the importance of the campaign is reiterated as an opportunity to awaken annual self-care by men to prevent disease and ensure healthy aging.
Conclusions
One of the determining factors for male's disregard for self-care stems from a cultural portrayal of masculinity, clouding their self-perception and recognition of symptoms of illness, interpreted as fragility, and thereby fostering the male self-sufficiency paradigm.
The Blue November Campaign was affirmed as an opportunity to propose interventions for men’s health care, to promote clarification and comprehensive care of men’s overall health, and to establish an annual routine of medical consultations starting from 45 years of age. A multidisciplinary team with a humanized approach is required when addressing aging male health issues and establishing strategies to mitigate the impacts of the physiological changes from aging.
Limitations of this study can be partly explained by the sample selection criterion, which enabled an evaluation of a larger number of men belonging to the onset of aging group, including patients with low incidence of genitourinary signs and symptoms. Moreover the only available measure for prostatic volume was through DRE, while transabdominal ultrasound is a more precise measure for prostate weight estimate in scientific parameters. Also, different regions may require further studies due to distinct characteristics of its populations to better assess the signs and symptoms of aging in health.
Acknowledgements
We thank the nursing and medical staff at Urology Clinic, as well as the biochemists and laboratory technicians staff at the Laboratory of Clinical Analysis, both of the University Hospital Onofre Lopes for their help.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Netto FLM. Aspectos biológicos e fisiológicos do envelhecimento humano e suas implicações na saúde do idoso. Pensar a Prática. 2004;7:75–84.
- Gravas S, Bach T, Bachmann A, et al. Guidelines on the managements of non-neurogenic male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO). Netherlands: Eur Assoc Urol; 2015; p. 6–97.
- Gao Y, Wang M, Zhang H, et al. Are metabolic syndrome and its components associated with lower urinary tract symptoms? Results from a Chinese male population survey. Urology. 2012;79:194–201.
- Parsons JK, Bergstrom J, Silberstein J, et al. Prevalence and characteristics of lower urinary tract symptoms in men aged ≥80 years. Urology. 2008;72:318–321.
- St Sauver JL, Jacobsen SJ. Inflammatory mechanisms associated with prostatic inflammation and lower urinary tract symptoms. Curr Prostate Rep. 2008;6:67–73.
- De Oliveira MM, Daher DV, Da Silva JL, et al. Men’s health in question: seeking assistance in primary health care. Ciênc Saúde Coletiva. 2015;20:273–278.
- Brasil. Ministério da Saúde. Envelhecimento e saúde da pessoa idosa. Brasília: Ministério da Saúde; 2007.
- Instituto Nacional do Câncer. Posicionamento do Ministério da Saúde acerca da integralidade da saúde do homem no contexto do Novembro Azul. Rio de Janeiro: INCA; 2015;n.001. Available from: www1.inca.gov.br/inca/Arquivos/nota_tecnica_saude_do_homem_ms.pdf
- Calogero AE, Burgio G, Condorelli RA, et al. Epidemiology and risk factors of lower urinary tract symptoms/benign prostatic hyperplasia and erectile dysfunction. Aging Male. 2018;2:1–8.
- Lee CL, Kuo HC. Pathophysiology of benign prostate enlargement and lower urinary tract symptoms: Current concepts. Ci Ji Yi Xue Za Zhi. 2017;29:79–83.
- Monteiro CA. Velhos e novos males da saúde no Brasil: a evolução do país e suas doenças. São Paulo: Hucitec Nupens/USP; 2000; p. 61–89.
- Brasil. Ministério do Planejamento, Orçamento e Gestão. Pesquisa Nacional de Saúde 2013: Ciclos de vida Brasil e grandes regiões. Rio de Janeiro: IBGE; 2015.
- Adegun PT, Adebayo PB, Areo PO. Severity of lower urinary tract symptoms among middle aged and elderly nigerian men: impacto on quality of life. Adv Urol. 2016;2016:1.
- Rohrmann S, Katzke V, Kaaks R. Prevalence and progression of lower urinary tract symptoms in an aging population. Urology. 2016;95:158–163.
- Madersbacher S, Haidinger G, Temml C, et al. Prevalence of lower urinary tract symptoms in austria as assessed by an open survey of 2,096 men. Eur Urol. 1998;34:136–141.
- Irwin DE, Milsom I, Hunskaar S, et al. Population-based survey of urinary incontinence, overactive bladder and other lower urinary tracts symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–1314.
- Kupelian V, Wei JT, O’Leary MP, et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and etnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Intern Med. 2006;166:2381–2387.
- Boyle P, Robertson C, Mazzetta C, et al. The prevalence of lower urinary tract symptoms in men and women in four centres. The UrEpik study. BJU Int. 2003;92:409–414.
- Orabi H, Albersen M, Lue TF. Association of lower urinary tract symptoms and erectile dyzfunction: pathophysiological aspects and implications for clinical management. Int J Impot Res. 2011;23:99–108.
- Saigal CS, Wessells H, Pace J, et al. Predictors and prevalence of erectile dysfunction in a racially diverse population. Arch Intern Med. 2006;166:207–212.
- Braun M, Wassmer G, Klotz T, et al. Epidemiology of erectile dysfunction: results of the 'Cologne Male Survey'. Int J Impot Res. 2000;12:305–311.
- Rosen R, Altwein J, Boyle P, et al. Lower urinary tract symptoms and male sexual dysfunction the multinational survey of the aging male (MSAM-7). Eur Urol. 2003;44:637–649.
- Mc Vary KT, Foley J, Slawin KM, et al. The long term effect of doxazosin, finasteride, and the combination on sexual function in men participating in the MTOPS study. J Urol. 2004;171:315. Abstract 1194.
- Li MK, Garcia LA, Rosen R. Lower urinary tract symptoms and male sexual dysfunction in Asia: a survey of ageing men from five Asian countries. BJU Int. 2005;96:1339–1354.
- Canguven O, Talib RA, El Ansari W, et al. Testosterone therapy has positive effects on anthropometric measures, metabolic syndrome components (obesity, lipid profile, Diabetes Mellitus control), blood indices, liver enzymes and prostate health indicators in elderly hypogonadal men. Andrologia. 2017;49:e12768. doi:10.1111/and.12768
- Yassin A, Nettleship JE, Talib RA, et al. Effects of testosterone replacement therapy withdrawal and re-treatment in hypogonadal elderly men upon obesity, voidind function and prostate safety parameters. Aging Male. 2016;19:64–69.
- Meuleman EJ, Legros JJ, Bouloux PM, et al. Effects of long-term oral testosterone undecanoate therapy on urinary symptoms: data from a 1-year, placebo-controlled, dose-ranging trial in aging men with symptomatic hypogonadism. Aging Male. 2015;18:157–163.
- Yassin DJ, Doros G, Hammerer PG, et al. Long-termtestosterone treatment in elderly men with hypogonadism and erectile dysfunction reduces obesity parameters and improves metabolic syndrome and health-related quality of life. J Sex Med. 2014;11:1567–1576.
- Shigehara K, Sugimoto K, Konaka H, et al. Androgen replacement therapy contributes to improving lower urinary tract symptoms in patients with hypogonadism and benign prostate hypertrophy: a randomised controlled study. Aging Male. 2011;14:53–58.
- Park SG, Yeo JK, Cho DY, et al. Impact of metabolic status on the association of serum vitamin D with hypogonadism and lower urinary tract symptoms/benign prostatic hyperplasia. Aging Male. 2018;21:55–59.
- Canguven O, Talib RA, El Ansari W, et al. Vitamin D treatment improves levels of sexual hormones, metabolic parameters and erectile function in middle-aged vitamin D deficient men. Aging Male. 2017;20:9–16.
- Espinosa G, Esposito R, Kazzazi A, et al. Vitamin D and benign prostatic hyperplasia - a review. Can J Urol. 2013;20:6820–6825.
- Ruan L, Zhu JG, Pan C, et al. Association between single nucleotide polymorphism of vitamin D receptor gene FokI polymorphism and clinical progress of benign prostatic hyperplasia. Sci World J. 2015;2015:1.
- Yalcinkaya S, Eren E, Eroglu M, et al. Deficiency of vitamin D and elevated aldosterone in prostate hyperplasia. Adv Clin Exp Med. 2014;23:441–446.
- Hong GS, Shim BS, Chung WS, et al. Correlation between metabolic syndrome and lower urinary tract symptoms of males and females in the aspect of gender specific medicine: a single institutional study. Korean J Urol. 2010;51:631–635.
- Park HK, Lee HW, Lee KS, et al. Relationship between lower urinary tract symptoms and metabolic syndrome in a community based elderly population. Urology. 2008;72:556–560.
- Ohgaki K, Hikima N, Horiuchi K, et al. Association between metabolic syndrome and male lower urinary tract symptoms in Japanese subjects using three sets of criteria for metabolic syndrome and International Prostate Symptom Score. Urology. 2011;77:1432–1438.
- Temml C, Obermayr R, Marszalek M, et al. Are lower urinary tract symptoms influenced by metabolic syndrome? Urology. 2009;73:544–548.
- Courtenay WH. Constructions of masculinity and their influence on men's well-being: a theory of gender and health. Soc Sci Med. 2000;50:1385–1401.
- Schraiber LB, Gomes R, Couto MT. Homens e saúde na pauta da Saúde Coletiva. Ciênc Saúde Coletiva. 2005;10:7–17.
- Modesto AAD, Lima RLB, D’Angelis AC, et al. A not-so-blue November: debating screening of prostate cancer and men’s health. Interface (Botucatu). 2018;22:251–262.
