Abstract
Urogenital cancers are frequently encountered in daily practice. Prostate cancer is the second most common type in adult males, and 2–3% of all adult cancers are renal cell carcinoma. Kaposi’s sarcoma originates from vascular endothelial cells and is the most common type of sarcoma observed in HIV-positive patients. However, the development of all these types of cancer in a patient without immunodeficiency is very rare. Incidence of urological malignancies increase with aging. In contrast to normal population, patient who have one urological malignancy have increased risk of getting another urological malignancy in a follow-up. So follow-up of this kind of patients is crucial and needs to be done carefully. In this case report, we aimed to discuss a 68-year-old patient who was diagnosed with concurrent prostate and kidney cancer and developed penile Kaposi’s sarcoma in follow-up.
Introduction
With the new methods and applications developed in diagnosis and treatment, it is possible to increase early diagnosis and survey of a cancer. The formation of a different type of cancer from a different focus after the diagnosis of the first cancer is defined as multiple primary cancers [Citation1]. Although it is common in the community, the development of several types of urogenital cancers in a patient is quite rare. In this case report, we present the first case of prostate cancer (PCa), renal cell carcinoma (RCC), RCC-induced tumor implantation, and finally penile Kaposi's sarcoma in the follow-up of an HIV-negative case.
Case report
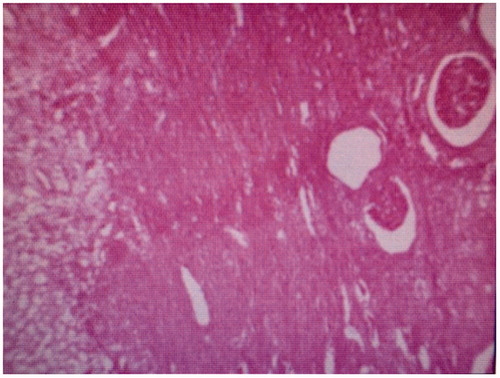
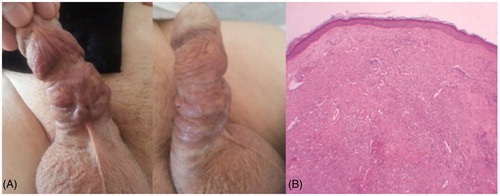
A 68-year-old male patient admitted to our hospital in December 2012 due to lower urinary tract symptoms and erectile dysfunction (ED), had a prostate specific antigen (PSA) of 10.5 ng/ml and transrectal ultrasound-guided prostate needle biopsy was performed. Gleason score 3 + 3 prostatic adenocarcinoma (PCa) was seen in 6 of 12 core. Abdominal magnetic resonance imaging (MRI), which was done for staging revealed a mass lesion of 45 mm in size, located in the middle part of the left kidney. The patient did not have any extra pathology and the left laparoscopic radical nephrectomy was performed in December 2012. Pathology revealed Furhman grade 1, T2N0M0 stage, and clear cell renal cell carcinoma (RCC) (). Then in March 2013, laparoscopic radical prostatectomy was performed for PCa and penile prosthesis implantation was performed afterwards. In the follow-up of the patient in January 2014, a 20 × 18 × 12 mm mass lesion on the right lobe of the liver adjacent to the anterior abdominal wall was detected in abdominal MRI. Radiological interpretation was a tumor cultivation that mimicked liver metastasis. In February 2014, the patient was operated by general surgery and the lesion was excised. RCC implantation of the lesion was reported as a result of histopathology (). The patient was started on sorafenib treatment, a tyrosine kinase inhibitor by medical oncology. There was no recurrence or metastasis in terms of PCa and RCC and the patient was followed-up until December 2017 and this time nodular skin lesions were detected on the penis. Kaposi sarcoma was seen in histopathological evaluation of cold punch biopsy taken from lesion (). The patient who had no known immunodeficiency or HIV infection was consulted with medical oncology and radiation oncology and informed about penectomy, radiotherapy, and chemotherapy options. As of now the patient is in the decision phase, no additional treatment has been implemented yet.
Discussion
Multiple primary cancers are mostly seen in the gastrointestinal system, respiratory system, head and neck region, and urogenital system, which constitute 13.5% of the total [Citation2]. Subhankar et al. reported that 23.6% of patients with RCC may have a distinct primary cancer focus, particularly in the male genital tract; several similar studies also suggest that renal carcinomas may be associated with prostate and bladder cancer [Citation3,Citation4]. In our case, PCa and RCC lesions detected at the time of admission were also compatible with the literature. However, peritoneal implantation on the contralateral side after radical nephrectomy is unusual case and needs to be discussed in literature [Citation5]. ED, which develops after radical prostatectomy and pelvic lymph node dissection, is a medical condition that is difficult to deal with and significantly impair the quality of life of the patient [Citation6,Citation7]. In one study, 81% of ED cases were found to prevent vaginal penetration within 2 years after radical prostatectomy [Citation8]. Protection of patients' sexual lives with penile prosthesis provides satisfactory results especially in sexually active patients. Therefore, we applied penile prosthesis to our patient in the postoperative period. But Kaposi's sarcoma, which was characterized by nodular skin lesions developing on the penis, was also surprising for us. Sorafenib is a tyrosine kinase inhibitor that can be used in standard medical treatment in metastatic RCC and may have side effects such as rash, mucositis, nausea, vomiting, and diarrhea [Citation9]. It is also known that sorafenib may have complications such as migration and erosion following the application of penile prosthesis in addition to skin findings [Citation10]. However, in our patient who did not have a known immunodeficiency and HIV infection, penile Kaposi's sarcoma following prosthesis application was the first mentioned in the literature considering the additional pathologies.
Conclusion
Incidence of urological malignancies increase with aging. In contrast to normal population patient who have one urological malignancy have increased risk of getting another urological malignancy in follow-up. So follow-up of this kind of patients is crucial and needs to be done carefully.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Wood ME, Vogel V, Ng A, et al. Second malignant neoplasms: assessment and strategies for risk reduction. J Clin Oncol. 2012;30:3734–3745.
- Chun TY. Coincidence of bladder and prostate cancer. J Urol. 1997;157:65–67.
- Subhankar C, Stefano T, Surinder B. Incidence and prognostic significance of secondary primary cancers in renal cell carcinoma. Am J Clin Oncol. 2013;36:132–142.
- Beisland C, Talleraas O, Bakke A, et al. Multiple primary malignancies in patients with renal cell carcinoma: a national population-based cohort study. BJU Int. 2006;97:698–702.
- Ozgur HY, Yildirim C, Urkmez A, et al. Contralateral tumor seeding of renal cell carcinoma mimicking late metastasis of liver after laparoscopic nephrectomy: a case report with review of the literature. Arch Ital Urol Androl. 2015;87:256–257.
- Naccarato A, Consuelo Souto S, Matheus WE, et al. Quality of life and sexual health in men with prostate cancer undergoing radical prostatectomy. Aging Male. 2018;1–8.
- Richards AB, Davis K, Gooden RO. Assessing the impact of sexual function on perceptions of masculinity among prostate cancer survivors in the United States: findings from the prostate cancer registry. Aging Male. 2018;1–5. DOI:10.1080/13685538.2018.1535582
- Wilt TJ, Brawer MK, Jones KM, et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med. 2012;367:203–213.
- Escudier B, Eisen T, Stadler WM, et al. target study group sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;365:125–134.
- Wilson SK, Delk JR, Salem EA, et al. Long-term survival of inflatable penile prostheses: single surgical group experience with 2,384 first-time implants spanning two decades. J Sex Med. 2007;4:1074–1079.