Abstract
Introduction
The role of transperineal template biopsy for prostate cancer diagnosis is well established. Pre-biopsy multiparametric magnetic resonance imaging (MRI) is used in most centers for planning of prostate biopsies and staging. Cognitive and software fusion techniques are increasingly getting popular.
Methods
We retrospectively reviewed patients who underwent transperineal template biopsies from January 2016 till December 2018. This included patients on active surveillance, previous negative transrectal ultrasonography biopsies with persistently raised prostate-specific antigen/abnormal prostate on digital rectal examination and de-novo template biopsies. Two specialist uro-radiologists reported all the scans and the biopsies were performed by one experienced urologist. The cognitive biopsies were performed for PIRADS 3–5 lesions on MRI. Total of 330 patients underwent transperineal template biopsies and cognitive target biopsies were carried out in 75 patients who were included in the study. We evaluated the results as positive/negative cognitive biopsies and also according to the PIRAD scoring. Only the patients with prostate cancer on template biopsy histology were included.
Results
Fifty-seven (76%) of the cognitive biopsies were positive out of total 75.
Conclusions
Combined cognitive and systematic biopsies have excellent diagnostic rate especially for PIRAD 4–5 MRI areas.
Introduction
The prostate cancer diagnostic tools continue to evolve as ever before. The improvements are intended to improvise on under-diagnosis of aggressive cancer as well as over-diagnosis of insignificant disease. The standard transrectal ultrasound guided prostatic biopsies poorly sample anterior, midline and apical areas of prostate and hence often misses prostate cancer in these locations [Citation1,Citation2]. Further ∼20% of cancers often are under-staged with transrectal ultrasound guided prostatic biopsies [Citation3]. With increasing prostate volume in the patients in the age group 61–75 years, increased number of prostate biopsies are advocated rather than the conventional 12 core biopsies [Citation4].
The role of transperineal template guided biopsies for prostate cancer diagnosis is very well established. Bott et al. [Citation5,Citation6] developed the brachytherapy template-guided prostatic transperineal technique for prostatic biopsies. Since then this technique has evolved as the favorite option in the setting of previously missed or under-staged prostate cancer disease [Citation7].
Pre-biopsy multiparametric magnetic resonance imaging (MRI) is another addition in the evolution of prostate biopsies and is now used in most centers for planning of biopsies and staging. MRI prostate is reported universally according to the PIRAD (Prostate Imaging – Reporting and Data System scoring) indicating the likelihood possibility of prostate cancer. It is feasible to avoid prostatic biopsies in PIRAD 1–2 scores as the chance of diagnosis of clinically significant prostate cancer in these situations is low [Citation8–12].
Cognitive and software fusion techniques are increasingly getting popular as adjuncts to the prostatic biopsies to target suspicious lesions on the multiparametric MRI. This may serve as a tool to avoid unnecessary repeated systematic random prostatic biopsies. [Citation9,Citation13,Citation14] Further the localization, extent, and Gleason score of cancer found in fusion biopsies correlates well with the final histology of radical prostatectomy specimens [Citation15,Citation16]. The fusion technique can be via the use of dedicated hardware and algorithm-based fusion software [Citation17–19], or visual fusion which is based on cognitive appraisal of the location of the suspicious PIRAD lesion on the ultrasound without any additional equipment [Citation20,Citation21]. However, there is no consensus and plenty of controversy as to whether targeted prostatic biopsies alone or a combination should be the standard, due to non-uniform evidence [Citation9,Citation10,Citation17,Citation22–25]. Peri-neural invasion on the prostate biopsy has been shown to be strong predictor of worst prognostic outcome as a strong correlation was found between such invasion on the biopsy specimen and the biochemical recurrence of cancer [Citation26]. Having higher quality tissue on cognitive and fusion biopsies increase the chances of knowing about peri-neural invasion.
With the established effectiveness of diverse treatments for localized prostate cancer the identification of the psychological and the physical consequences of the disease and its various treatments has become an important issue [Citation27]. It is also equally important to choose the most appropriate diagnostic method to get the histology for the best final outcome of the disease.
Methods
The study is registered as an audit in the Medway NHS Foundation trust. We retrospectively reviewed consecutive patients who underwent transperineal template prostatic biopsies from January 2016 till December 2018. This included patients on active surveillance, negative transrectal ultrasonography (TRUS) biopsies with persistently raised prostate-specific antigen (PSA)/abnormal digital rectal examination and biopsy in naïve patients. Systematic mapping biopsies were taken from both the lobes and cognitive target biopsies consisted of four additional target biopsies in addition to systematic prostatic sampling. Biopsies were performed in the operating theatre under general anesthesia with the patient in the dorsal lithotomy position. All men received perioperative antibiotics and the antibiotics were continued postoperatively for 3 days. Using transrectal ultrasound probe, the prostate gland examined and prostate volume was determined. The suspicious MRI lesions cognitively projected according to the MRI study for cognitive fusion biopsies.
All MRI scans were done using 3 Tesla scanner and two dedicated specialist uro-radiologists reported all the scans. Radiologists evaluated suspicious lesions using T2-weighted imaging, diffusion-weighted imaging and lately dynamic contrast-enhanced MRI. The MRI prostate scans were reported as Tx (i.e. PIRAD 1/2), PIRAD 3, 4, and 5. The template biopsies were performed by only one experienced urologist.
Results
A total of 330 patients were included and were divided into two cohorts – The diagnostic (188 patients) and the active surveillance cohort (142 Patients). The Diagnostic cohort included patients who previously had benign transrectal ultrasound guided prostatic biopsies (156 patients) and biopsy naïve patients (32 patients). The indications of de-novo template biopsies were mostly patient preference. The active surveillance group included 106 patients with Gleason 3 + 3 prostate cancer, 18 patients with low volume Gleason 3 + 4 prostate cancer and also 18 patients who were previously on active surveillance (mostly diagnosed on transurethral resection of prostate – TURP). 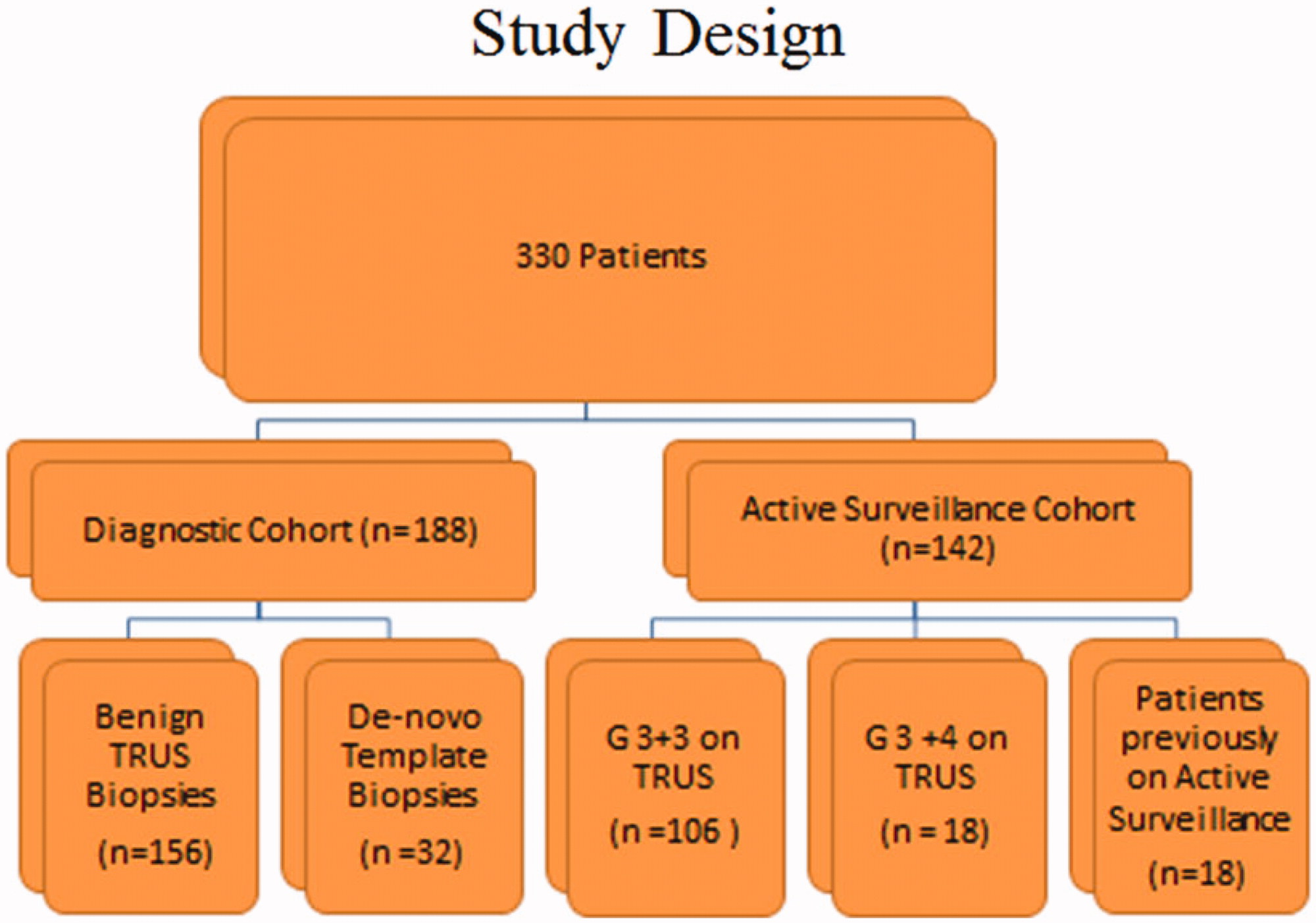
In the diagnostic group 147 (80.76%) of MRI scans were reported 3, 4, 5, and 35 (19.23%) as Tx (PIRAD1/2). For PIRAD 3–5 areas 51.70% revealed positive histology on template biopsies, PIRAD 1–2 the positive rate was 31.42%. Six patients did not have MRI for various reasons and two out of them were diagnosed with prostate cancer on template biopsies.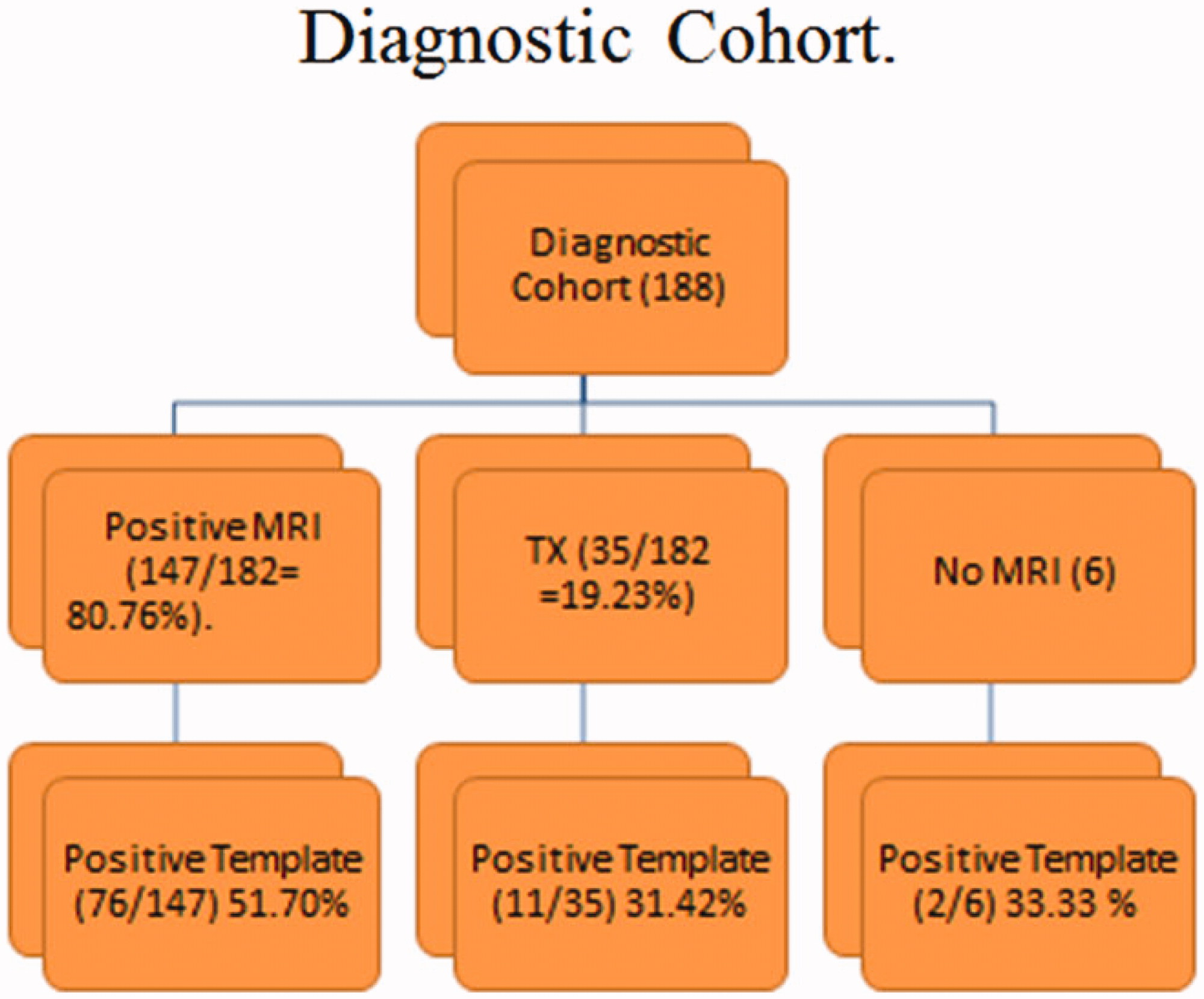
In the active surveillance cohort PIRAD 1/2 lesions were reported in 21(16.15%), PIRAD 3–5 in 109 (83.84%) whereas 12 patients did not have MRI. 74.31% of PIRAD 3–5 revealed prostate cancer whereas the cancer detection rate was only 42.85% for PIRAD 1–2 areas. 
Out of 330 patients, only 75 were included and had cognitive biopsies performed for PIRAD 3–5 lesions. We evaluated the results as positive/negative cognitive biopsies and also according to the PIRAD scoring. Only the patients with prostate cancer on histology were included.
Patient Characteristic
57 (76%) of the cognitive biopsies were positive out of total 75.
When the results were divided according to the PIRAD grades the positive rates were 53.33%, 83.72%, and 76.47% for PIRAD 3, PIRAD 4, and PIRAD 5 grades respectively. Patients with significant prostate cancer (>Gleason 3 + 4) have higher mean mean PSA and mean PSA densities. Mean PSA density of more than 0.107 ng/ml/cc was associated with significant prostate cancer (>Gleason 3 + 4) and similarly mean PSA density of less than 0.103 ng/ml/cc was associated less significant prostate cancer (<Gleason 3 + 4). In the target biopsies patients higher PIRAD scores were not particularly associated with significant prostate cancers and vice-versa.
Although about 75% of the cognitive biopsies are positive in our series, on further analysis we found that most of these cancers would have been diagnosed anyway on systematic biopsies. However there are still 16% of significant cancers which we diagnosed just on the basis of target biopsies. If only target biopsies are taken we would have missed 19/75 = 25.33% of cancers, out of these eight were clinically significant, that is, miss rate of 10.66% for clinically significant prostate cancers. Hence we suggest combined target and systematic transperineal template guided prostatic biopsies rather than target only or systematic only prostatic biopsies.
Discussion
Cognitive target biopsies enable improved detection rate of prostatic adenocarcinoma and importantly clinically significant cancers in the heterogeneous group of the patients. Combined cognitive and systematic biopsies have excellent diagnostic rate especially for PIRAD 4–5 MRI areas.
There are several studies in the literature which have evaluated the use of cognitive fusion transperineal prostatic biopsies and software based fusion biopsies. According to Hansen et al. [Citation28], in MRI equivocal lesions there is no additional benefit of targeted biopsies but for suspicious MRI areas combination of target and systematic biopsies is superior.
Targeted biopsies missed 10% of clinically significant cancers in our series, 13% in Kasivisvanathan et al. [Citation29] series. Kasivisvanathan et al. [Citation29] examined 182 men with a lesion suspicious for cancer on MRI and cognitive target biopsies yielded clinically significant cancer in 57%. Valerio et al. [Citation30] compared cognitive versus software based targeted transperineal prostate biopsies and found that both methods were comparable 64% versus 68% detection rate. Radtke et al. [Citation10] showed that while detecting similar amounts of Gleason score 7 or greater tumors, the use of multiparametric MRI/TRUS fusion mitigated the detection of lower grade disease. Miyagawa et al. [Citation31] noted that MRI-template biopsies detected 21% of cancers missed by systematic biopsy compared to the 4% by Kasivisvanathan et al. [Citation29].
As in our study, Hadashick [Citation32] and Miyagawa et al. [Citation31] found a higher proportion of cores positive for cancer using MRI-TB than systematic non-targeted biopsy. Prostate volume may have a role to play in the detection of prostate cancer by MRI fusion and targeted biopsies. Lower volume prostates have higher detection than the higher volume prostates (77% vs. 34%) [Citation33].
Conclusions
There is diagnostic advantage of the combination of targeted and systematic prostatic template guided biopsies for PIRAD 4 and 5 areas whereas for the PIRAD 3 areas the advantage seems to be less according to our study.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Nevoux P, Ouzzane A, Ahmed HU. Quantitative tissue analyses of prostate cancer foci in an unselected cystoprostatectomy series. BJU Int. 2012;110:517.
- Hu Y, Ahmed HU, Carter T, et al. A biopsy simulation study to assess the accuracy of several transrectal ultrasonography (TRUS)-biopsy strategies compared with template prostate mapping biopsies in patients who have undergone radical prostatectomy. BJU Int. 2012;110:812.
- Onik G, Miessau M, Bostwick DG. Three dimensional prostate mapping biopsy has a potentially significant impact on prostate cancer management. JCO. 2009;27:4321.
- Kocan H. Factors affecting the diagnosis of prostate cancer through 12 quadrant guided prostate biopsy. Aging Male. 2019. doi:10.1080/13685538.2019.1573219
- Bott SR, Henderson A, Halls JE, et al. Extensive transperineal template biopsies of prostate: modified technique and results. Urology. 2006;68:1037–1041.
- Bott SR, Henderson A, Parkinson MC, et al. Setting up a prostate cancer database: experiences on how to get out more than you put in. BJU Int. 2003;92:665–666.
- Vyas L, Acher P, Kinsella J, et al. Indications, results and safety profile of transperineal sector biopsies (TPSB) of the prostate: a single centre experience of 634 cases. BJU Int. 2014;114:32–37.
- Hansen N, Patruno G, Wadhwa K, et al. Magnetic resonance and ultrasound image fusion supported transperineal prostate biopsy using the Ginsburg protocol: technique, learning points, and biopsy results. Eur Urol. 2016;70:332–340.
- Siddiqui MM, Rais-Bahrami S, Turkbey B, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015;313:390–397.
- Radtke JP, Kuru TH, Boxler S, et al. Comparative analysis of transperineal template saturation prostate biopsy versus magnetic resonance imaging targeted biopsy with magnetic resonance imaging ultrasound fusion guidance. J Urol. 2015;193:87–94.
- Moore CM, Robertson NL, Arsanious N, et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol. 2013;63:125–140.
- Filson CP, Natarajan S, Margolis DJ, et al. Prostate cancer detection with magnetic resonance-ultrasound fusion biopsy: the role of systematic and targeted biopsies. Cancer. 2016;122:884–892.
- Gayet M, van der Aa A, Beerlage HP, et al. The value of magnetic resonance imaging and ultrasonography (MRI/US)-fusion biopsy platforms in prostate cancer detection: a systematic review. BJU Int. 2016;117:392–400.
- Schoots IG, Roobol MJ, Nieboer D, et al. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta analysis. Eur Urol. 2015;68:438–450.
- Baco E, Ukimura O, Rud E, et al. Magnetic resonance imaging-transectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol. 2015;67:787–794.
- Delongchamps NB, Lefèvre A, Bouazza N, et al. Detection of significant prostate cancer with magnetic resonance targeted biopsies—should transrectal ultrasound-magnetic resonance imaging fusion guided biopsies alone be a standard of care? J Urol. 2015;193:1198–1204.
- Radtke JP, Schwab C, Wolf MB, et al. Multiparametric magnetic resonance imaging (MRI) and MRI-transrectal ultrasound fusion biopsy for index tumor detection: correlation with radical prostatectomy specimen. Eur Urol. 2016;70:846–853.
- Sandler K, Patel M, Lynne C, et al. Multiparametric-MRI and targeted biopsies in the management of prostate cancer patients on active surveillance. Front Oncol. 2015;5:4.
- Yerram NK, Volkin D, Turkbey B, et al. Low suspicion lesions on multiparametric magnetic resonance imaging predict for the absence of high-risk prostate cancer. BJU Int. 2012;110:E783–8.
- Hutchinson RC, Costa DN, Lotan Y. The economic effect of using magnetic resonance imaging and magnetic resonance ultrasound fusion biopsy for prostate cancer diagnosis. Urol Oncol. 2016;34:296–302.
- Marks L, Young S, Natarajan S. MRI-ultrasound fusion for guidance of targeted prostate biopsy. Curr Opin Urol. 2013;23:43–50.
- Meng X, Rosenkrantz AB, Mendhiratta N, et al. Relationship between pre-biopsy multi-parametric magnetic resonance imaging (MRI), biopsy indication, and MRI-ultrasound fusion-targeted prostate biopsy outcomes. Eur Urol. 2016;69:512–517.
- Radtke JP, Teber D, Hohenfellner M, et al. The current and future role of magnetic resonance imaging in prostate cancer detection and management. Transl Androl Urol. 2015;4:326–341.
- Arsov C, Rabenalt R, Blondin D, et al. Prospective randomized trial comparing magnetic resonance imaging (MRI)-guided in-bore biopsy to MRI-ultrasound fusion and transrectal ultrasound-guided prostate biopsy in patients with prior negative biopsies. Eur Urol. 2015;68:713–720.
- Thompson JE, van Leeuwen PJ, Moses D, et al. The diagnostic performance of multiparametric magnetic resonance imaging to detect significant prostate cancer. J Urol. 2016;195:1428–1435.
- Vukocic M, Kavaric P, Magdelinic A, et al. Perineural invasion on biopsy specimen as predictor of tumor progression in aging male treated with radical prostatectomy. Could we use it for pre-surgical screening? Aging Male. 2019. doi:10.1080/13685538.2019.1581758
- Naccarato A, Consuelo Souto S, Matheus WE, et al. Quality of life and sexual health in men with prostate cancer undergoing radical prostatectomy. Aging Male. 2018. doi:10.1080/13685538.2018.1486397
- Hansen NL, Kesch C, Barrett T, et al. Multicentre evaluation of targeted and systematic biopsies using magnetic resonance and ultrasound image-fusion guided transperineal prostate biopsy in patients with a previous negative biopsy. BJU Int. 2017;120:631–638.
- Kasivisvanathan V, Dufour R, Moore CM, et al. Transperineal magnetic resonance image targeted prostate biopsy versus transperineal template prostate biopsy in the detection of clinically significant prostate cancer. J Urol. 2013;189:860–866.
- Valerio M, McCartan N, Freeman A, et al. Visually directed vs. software-based targeted biopsy compared to transperineal template mapping biopsy in the detection of clinically significant prostate cancer. Urol Oncol. 2015;33:e9–16.
- Miyagawa T, Ishikawa S, Kimura T, et al. Real time virtual sonography for navigation during targeted prostate biopsy using magnetic resonance imaging data. Int J Urol. 2010;17:855.
- Hadaschik BA, Kuru TH, Tulea C, et al. A novel stereotactic prostate biopsy system integrating pre-interventional magnetic resonance imaging and live ultrasound fusion. J Urol. 2011;186:2214.
- Erdogan A, Polat S, Keskin E, et al. Is prostate volume better than PSA density and free/total PSA ratio in predicting prostate cancer in patients with PSA 2.5–10 ng/mL and 10.1–30 ng/mL? Aging Male 2019. doi:10.1080/13685538.2019.1578741
