Abstract
Introduction
Vasectomy is a popular choice of contraception worldwide. In the UK, vasectomy reversal is not usually licensed under the NHS with reports on outcomes being limited. Microsurgical reversal is a technique commonly performed under the operating microscope. Loupe magnification, however, is emerging as a safe and reliable technique to perform microsurgery.
Method
Loupe-assisted microsurgical vasovasotomies were performed on 14 men in a 3-year period. Indications for the procedure were for fertility only. Semen analysis variables were measured against European Association of Urologists (EAU) guidelines at six weeks. Patients were followed-up at clinic in three months. Data were collated using operation notes and cytology results, and analysed using descriptive statistics. Pearson’s correlation coefficient was used to compare years after vasectomy, and age to sperm count.
Results
The average sperm count in our group was 41.3 million per millilitre (median 29.95, range 2.7–107.8) at 6 weeks. Seventy-five per cent were found to have positive sperm motility, and all had acceptable sperm morphology at follow-up. A very low to weak correlation between time after vasectomy and age, with sperm count.
Conclusion
We have demonstrated that fertility and post-operative outcomes using a loupe-assisted microsurgical vasovasotomy approach are favourable as per EAU guidelines.
Introduction
Worldwide, approximately 6–8% of couples prefer vasectomy as a choice of contraception. This leaves approximately 42–60 million men who would undergo vasectomy as a permanent measure [Citation1]. Death of a child or remarriage may lead to many vasectomised men wanting to undergo reversal of the procedure to naturally conceive children [Citation1,Citation2]. Some of these men may consequently go on to conceiving future children via in vitro fertilisation or intracytoplasmic sperm injection [Citation1–3]. Furthermore, others may desire reversal due to non-fertility reasons such as debilitating symptoms from post-vasectomy pain syndrome, or vasitis [Citation1,Citation4].
In the UK, vasectomy reversal is not usually licensed under the NHS [Citation3]. Reports on outcomes and acceptable semen analysis following surgery are therefore limited in the country, generally following reference guidelines from the European Association of Urologists (EAU) on what an adequate sample should be [Citation5,Citation6]. This can leave clinicians struggling to effectively counsel men on post-operative fertility rates who are seeking this procedure.
Two techniques are widely used for vasectomy reversal: vasovasostomy or vasoepididymostomy [Citation7]. In 1902, the first human vasal repair was conducted by Martin, which was a milestone for mankind. Two decades later the first vasovasotomy was performed by Quinby and his associate, O’Connor [Citation1]. This has inspired future surgeons to strive for more experience and technical improvement, with the help of advancing innovations and technology to improve surgical outcomes [Citation7,Citation8].
Microsurgery is performed using either the operating microscope or loupe magnification [Citation9–11]. Use of the operating microscope is considered the “criterion standard;” however, loupes are emerging as a safe and reliable technique to perform microsurgery [Citation8,Citation10,Citation11]. More recently, robotic-assisted vasectomies are becoming more common, claiming excellent patency rates [Citation12–14].
In this study, we present our findings and outcomes in men undergoing vasectomy reversal via a loupe-assisted microsurgical vasovasostomy approach in the UK.
Method
In a rural town in the UK, a single surgeon performed microsurgical vasovasostomies on 14 men from 2016 to 2019. Indications for the procedure were for the desire to regain fertility for conception only.
Under a general anaesthetic, patients were positioned in the supine position. The operating field is prepared by using chlorhexidine wash, followed by sterile draping of the surrounding fields. A midline raphe incision is made, allowing access to both sides of the scrotum. The layers of the scrotum are subsequently dissected until the testis is delivered outside. The epididymis is examined and any sperm granuloma is dissected away. Loupes magnified by seven-fold were then used throughout the remaining procedure. The proximal and distal ends of the vas deferens are isolated and any scar tissue is resected away. Intravasal fluid from the vas is then expressed and the patency of the vas is checked with a 24G cannula catheterised into the lumen of the proximal and distal ends, with 3 ml of saline injected into each.
An end to end anastomosis is performed using a two layer closure technique. Using 8-0 polyglactin 910 (VICRYL®) an inner anastomosis is performed in the 12, 3, 6, and 9 o’clock positions, suturing the mucosa to mucosa of each end of the vas via an interrupted method. A second layer is then closed using an interrupted technique, suturing the muscularis layer to the serosa, at all four corners. The anastomosis is then made tension free by covering a layer of tunica over the vas. The tunica is everted and placed back into the scrotal sac. This process is repeated on the contralateral hemiscrotum before closing the dartos layer and skin using absorbable sutures. Bupivacaine 0.5% is injected into the operating site, and the wound is subsequently dressed.
Patients are discharged on the same day with a course of oral antibiotics and advised to wear scrotal support for 1 week. Furthermore, they are advised to abstain from sexual activity for 3–4 weeks and asked to provide a semen analysis performed in 6 weeks. Variables measured included sperm count, positive sperm motility (>32%), and positive sperm morphology (>4%) as per EAU guidelines. All patients are then followed-up at an outpatient clinic in three months.
Patient demographics and outcomes were collated using operation notes and cytology results, with analysis of the results using descriptive statistics. Pearson’s correlation coefficient was used to compare years after vasectomy, and age to sperm count.
Results
In a 3-year period, 14 men underwent a reversal of vasectomy under a single surgeon. The mean age in our group was 36.9 (range 27–49), with a median ASA grade of 1 (range 1–2). All men underwent a reversal of vasectomy for purposes of conception, and the whole group had this performed via a vasovasostomy approach. The average number of years from vasectomy to reversal in our group was 7.14 (median 5.5 years, range 2–17 years).
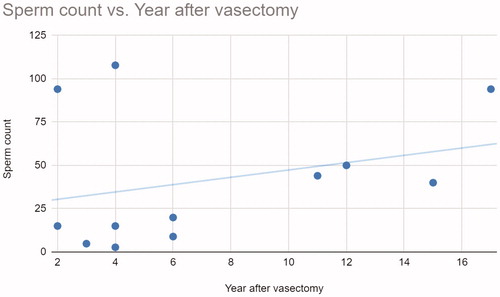
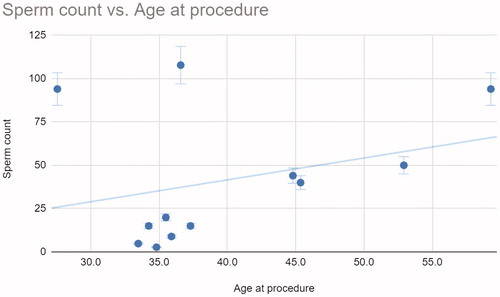
On follow-up at 3 months, one man had orchitis as a complication post procedure which was treated with oral antibiotics. There was no documented semen analysis for two patients who were lost to follow-up. The average sperm count in our group (n = 12) was 41.3 million per millilitre (median 29.95, range 2.7–107.8). Out of the 12 men, 75% (n = 9) were found to have positive sperm motility, and all had acceptable sperm morphology at follow-up. At 0.29 () and 0.3 (), respectively, there is a very low to weak correlation between time after vasectomy and age, with sperm count. There is no further follow-up and therefore subsequent documentation on whether these men went on to conceive children is unknown.
Conclusion
We have shown in our limited study that fertility and post-operative outcomes following vasectomy reversal using a loupe-assisted microsurgical vasovasostomy approach have been favourable. There were no serious post-operative complications at follow-up, with one complication being treated in the community. The age of men or length of duration from vasectomy to reversal are very weakly correlated with regard to sperm count. However, surprisingly, men who are older and who have had a longer duration between procedures seem to have slightly better outcomes, with contradicting outcomes from other studies [Citation8,Citation9]. We have also shown that the majority of men achieve a positive sperm motility rate at three months following reversal. It is unclear from our sample whether these men went on to successfully conceive children. Studies have shown that an increase in age can lead to a reduction in sperm DNA integrity, which could impact conception rates following reversal [Citation15,Citation16]. However, we would expect fertility rates to be favourable if they went under the in vitro fertilisation or an intracytoplasmic sperm injection ICSI route.
We would therefore advocate loupe-assisted microsurgical vasovasostomies in men wanting a reversal for fertility purposes. However, a higher powered sample and meta analyses studies would provide stronger data for clinicians to have more knowledge on accurately counselling patients. Younger men may have less favourable outcomes, and will need to be extensively counselled, however it remains to be clear how significant this may be.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Patel AP, Smith RP. Vasectomy reversal: a clinical update. Asian J Androl. 2016;18(3):365.
- Bernie AM, Osterberg EC, Stahl PJ, et al. Vasectomy reversal in humans. Spermatogenesis. 2012;2(4):273–278.
- Francisco L, Braga D, Figueira R, et al. Assisted reproductive technology outcomes in azoospermic men: 10 years of experience with surgical sperm retrieval. Aging Male. 2010;13(1):44–50.
- Jones A, Vazirian-Zadeh M, Phan Y, et al. Post vasectomy chronic pain: are we under diagnosing vasitis? A case report and review of the literature. Aging Male. [cited 2018 Sep 29]; [3 p.]. DOI:10.1080/13685538.2018.1513481
- NHS [Internet]. Can I get a vasectomy reversed? 2018. Available from https://www.nhs.uk/conditions/contraception/vasectomy-reversal-nhs/
- Ramasamy R, Schlegel PN. Vasectomy and vasectomy reversal: an update. Indian J Urol. 2011;27(1):92–97.
- Jungwirth A, Diemer T, Dohle GR, et al. EAU guidelines on male infertility. 2014. Paper presented at the EAU Annual Congress Barcelona, 2019. ISBN 978-94-92671-04-2.
- Namekawa T, Imamoto T, Kato M, et al. Vasovasostomy and vasoepididymostomy: review of the procedures, outcomes, and predictors of patency and pregnancy over the last decade. Reprod Med Biol. 2018;17(4):343–355.
- Potts JM, Pasqualotto FF, Nelson D, et al. Patient characteristics associated with vasectomy reversal. J Urol. 1999;161(6):1835–1839.
- Dickey RM, Pastuszak AW, Hakky TS, et al. The evolution of vasectomy reversal. Curr Urol Rep. 2015;16(6):40.
- Loughlin KR. Microsurgical vasectomy reversal and varicocele ligation. Urology. 1999;53(1):239–240.
- Hollingsworth MR, Sandlow JI, Schrepferman CG, et al. Repeat vasectomy reversal yields high success rates. Fertil Steril. 2007;88(1):217–219.
- Sigman M. The relationship between intravasal sperm quality and patency rates after vasovasostomy. J Urol. 2004;171(1):307–309.
- Kolettis PN, Burns JR, Nangia AK, et al. Outcomes for vasovasostomy performed when only sperm parts are present in the vasal fluid. J Androl. 2006;27(4):565–567.
- Deenadayal Mettler A, Govindarajan M, Srinivas S, et al. Male age is associated with sperm DNA/chromatin integrity. Aging Male. [cited 2019 Apr 9]. [8 p.]. DOI:10.1080/13685538.2019.1600496
- Duca Y, Calogero A, Condorelli R, et al. Early male aging or poor clinical consideration for males in IVF centers? An original study. Aging Male. [cited 2019 May 28]; [5 p.]. DOI:10.1080/13685538.2019.1618260