Abstract
Aim
Although appendicitis is a disease of the young, it has been speculated that its incidence has increased among the elderly people. In this study, it was aimed to evaluate annual changes of appendicitis seen in older patients (≥60 years) throughout a 10-year period.
Methods
All adult patients who were surgically treated for acute appendicitis were retrospectively analyzed with respect to pathological analysis, gender, age and proportion of the patients aged 60 or over in an annual base. Variability in the mean age and proportion of the older patients aged 60 or over throughout the study years were regarded as the main outcomes.
Results
There were 3296 patients with a mean age of 30.42 ± 12 years. Distribution of gender was similar (p = 0.636). There was a significant positive correlation in the mean age of the patients throughout the study years (p = 0.043). Stratification by the age of 60 yielded a significant increase in percent of the older patients, from 0.93% at 2007 to 4.28% at 2016 (p = 0.019).
Conclusions
The mean age of the patients with acute appendicitis is going to increase. Therefore, it is expected that all surgeons are more likely to be confronted with elderly patients with appendicitis in the near-future.
Introduction
In studies dealing with epidemiology of acute appendicitis (AA) from several regions of the world, it has been stated that there were significant differences in incidences, sex, age, and seasonal variations [Citation1–6]. Age of the patients, as one of the main epidemiological factors of AA, may have an important impact on its incidence. In relation with age and incidence, there have been controversial issues with regard to the decreased appendicitis rates, especially from Western countries including Denmark and Spain, in association with the decreased number of their population, and in the United States [Citation1,Citation3]. It has also been reported that the frequency of AA is increasing in the developing countries and Canada [Citation3,Citation7]. Therefore, the changes in demographics of the countries, that is, sustained decreases or increases in fertility and dramatic increases in life expectancy resulting in an overall increased ratio of elderly people may have a role in changing the epidemiology of AA [Citation8].
Although appendicitis is often thought of as a disease of the young, it has been reported that there has been a higher proportion of the population aged 60 or over with AA in recent years in association with increasing life expectancy [Citation1,Citation8–11]. However, it has also been speculated that whether this change was a real event occurring on a national level for the United States [Citation1]. So, whether or not AA has been more commonly seen in older patients in different regions of the World remains to be an unresolved issue.
In this study, it was aimed to analyze annual changes of AA seen in older patients (≥60 years) throughout a 10-year period in a public/governmental hospital.
Materials and methods
The study was approved by the local ethical committee for clinical studies (17828-18.08.2017). Informed consent could not be taken from the patients due to the retrospective design of the study. The study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments. The study was registered to researchregistry.com via unique identifying number of researchregistry2588.
The medical records of all adult patients (≥16 years old) who were surgically treated with a presumptive diagnosis of AA were retrospectively analyzed from 1 January 2007 to December 31, 2016. The decision for the surgery was at the discretion of the attending surgeon based on the history, the physical examination and the results of laboratory and imaging modalities. Conservative approach for the treatment of AA has not been used in this hospital during the study period.
Age, sex, operation date and final pathology results were obtained from the hospital information system using the search terms “appendicitis” and “appendectomy”. This search yielded 3733 consecutive patients who underwent appendectomy between 1 January 2007 and December 31, 2016.
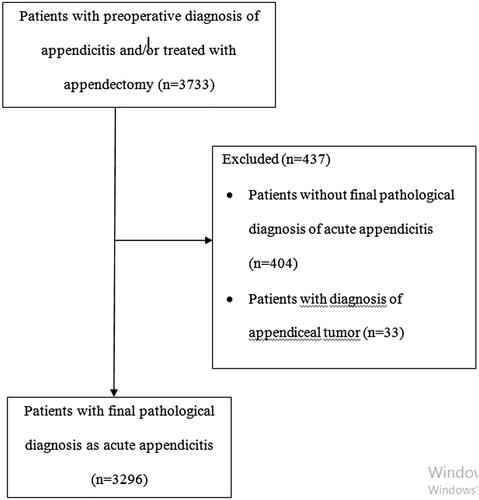
The patients with appendectomy either open or laparoscopic for AA and the patients with appendectomy plus drainage were all included. The patients in the absence of histopathological diagnosis of AA (n = 404) and the patients with tumoral lesions of the appendix vermiformis (n = 33) were excluded. Therefore, a total of 3296 patients were remained for the study group. Flow diagram of the study was given in . The histopathological diagnosis of AA was confirmed in the presence of peri-appendicular infiltration of the polymorphonuclear leukocytes.
The patients were grouped according to the operation date as annually and then were analyzed with respect to gender and age. For the analysis of gender distribution, the proportion of the male patients (%) as to all patients for each year was used. For the analysis of the proportion of AA seen in older patients, two different approaches were used: the changes in the mean age of the patients treated in each year and the proportion of the population aged 60 or over. For the definition of the aged population, the age of 60 was regarded as the lower limit based on the classification of the United Nations [Citation12].
Statistical analysis
The hypothesis of this study was that age of the patients with AA has increased leading to a higher proportion of AA seen in aged population. The variability in the mean age of the patients and the proportion of the population aged 60 or over throughout the study years were regarded as the main outcomes. Therefore, each parameter was reviewed by year to determine their variability for each year, that is, from 2007 to 2016. All statistical analyses were performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). All continuous values were presented as the mean ± standard deviation (SD). Categorical variables were expressed as frequencies and percentages. The percentages of the male patients and AA in aged population were calculated as the number of the cases in each category divided by the size of the population of the study group in each year.
Spearman’s rank correlation test (rs as the correlation coefficient) was used for the examination of the associations between the changes of AA cases with regard to the total number of the cases, the proportion of the male patients, the mean age and the proportion of the population aged 60 or over throughout the study years. For this purpose, the study years from 2007 to 2016 was shown as numbers from 1 to 10, respectively. The statistical results were presented at a 95% confidence interval. The differences were considered statistically significant if the p value was less than 0.05.
Results
The mean age of the patients (n = 3296) with AA was 30.42 ± 12 years with a range of 16-88 years. There were 2231 male patients (67.7%). The percent of the male patients was 0.68. Distribution of the patients according to the total number, the percent of the male patients, the age and the percent of older patients (≥60 years) is detailed in an annual base in . The changes of the mean age of the patients throughout the study years are given in .
Figure 2. Line graph showing mean age (year) with 95% confidence interval of the patients throughout the study years between 2007 and 2016, by year. The numbers 1 to 10 indicates the years 2007 to 2016, respectively.
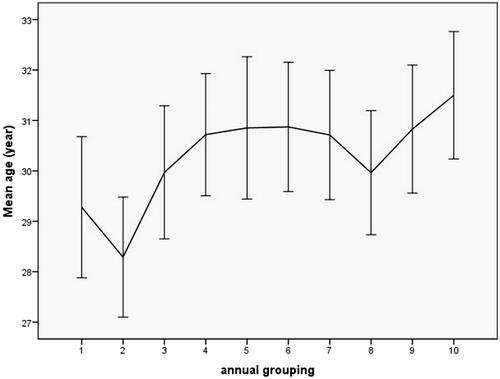
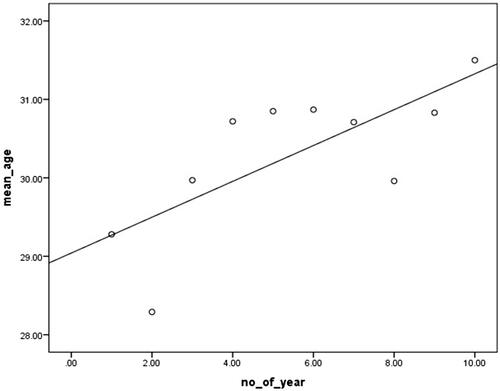
There was a significant increase in the number of AA cases (rs=0.818, p = 0.004). The number was almost doubled from 215 at 2007 to 397 at 2016. Distribution of the male and female patients was similar throughout this 10-year study period (rs=-0.171, p = 0.636). Correlation analysis showed that there was a significant increase in the mean age of the patients throughout the study years (rs=0.648, p = 0.043) ().
Figure 3. Correlation between mean age of the patients (line y:mean_age) and the study years (line x: no_of_years). The numbers 1 to 10 in line × indicates the years 2007 to 2016, respectively.
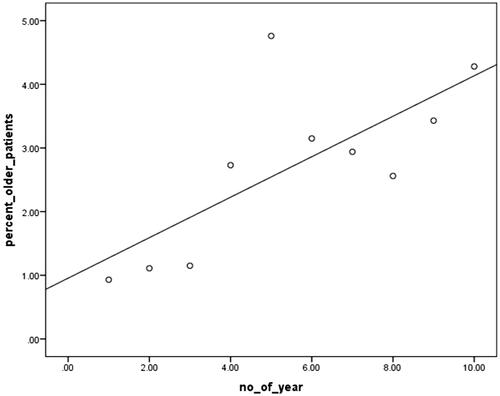
Stratification by the age of 60 yielded a significant increase in the percent value of the older patients, starting from two patients with a ratio of 0.93% at 2007 to 17 patients with a ratio of 4.28% at 2016 (rs=0.721, p = 0.019) ().
Discussion
The findings of this study showed that the proportion of older patients pathologically proven AA whose age 60 or over to all cases has increased significantly over the last 10 years in this public/governmental hospital.
In association with the activity of the mucosa-associated lymphoid tissues which make up most of the appendix vermiformis, it has been believed that the incidence of AA declines after the third decade [Citation2]. In a cadaveric study from Bangladesh, it has been shown that normal diameter of the lymphoid follicles of the appendix vermiformis reduces significantly with advancing age (over 50 years) [Citation13]. However, it has been reported that up to 15% of all AA cases are seen in elderly patients for the last several decades. Therefore, AA in the elderly is a controversial issue that necessitates further pathophysiological explanation. The lymphoid structure of the appendix vermiformis begins to decrease in the early adulthood, and atrophied and obliterated at the older ages [Citation14]. Additionally, the size of the appendix vermiformis begins to decrease from the early adulthood. The structural components including the number and diameter of the lymphoid follicles and glands, the luminal diameter and the wall thickness may be questioned from the clinical perspective of the appendix-related problems. The higher incidence of AA in the young adults may be closely associated with these structural components that changes with age. In Bakar’s study [Citation14], it has been reported that the diameter of the appendix vermiformis and the overall number of germinal centers show a negative correlation with the age of the subjects. Although the authors thought that higher frequency of AA is not related with the luminal diameter of the appendix vermiformis and the number of mucosal glands, they recommended further studies to find out the correlation between the number of germinal centers and the incidences of AA in association with the different age groups.
Although there have been several lower age limits such as 60, 65 or 68 years for the definition of elderly patients, 60 years or over was used in this study according to the definition of the United Nations and the studies published by Storm-Dickerson and Peltokallio [Citation8–10,Citation12].
It has been thought that the incidence of AA in elderly patients has increased in association with increasing life expectancy especially in developing and developed countries [Citation9]. Guller et al. [Citation15] reported that 6.5% of the cases with AA were equal to 65 years of age and older based on the Nationwide Inpatient Samples of the United States between 1998 and 2000. The United States data also showed that there was a significant increase in the percent out of number of hospitalizations for AA in patients whose age is 60 years and older between 1996 and 2008 [Citation1]. In this study, the proportion of older patients (≥60 years) increased from 8.5% to 10.6%. The authors concluded that the mean age at diagnosis has increased by 3.1 year over the time period between 1996 and 2008 in accordance with our results. Another study from Finland also reported a significant increase in the proportion of older people (≥60 years) with appendicitis from 4.6% to 8.8% between 1969 and 1974 [10]. In Ceresoli’s study from Italy, 3.32% of all patients treated for AA were detected as 65 years or older [Citation16]. In another study from South-Western Nigeria, older patients (>60 years) comprised only 1.3% of all appendicitis cases [Citation2]. In another study from Turkey, the proportion of older patients (>65 years) with AA was shown to be 2.37% [Citation17]. In the present study, the percent of the older patients (≥60 years) was calculated as 4.28%. Therefore, it is better to accept that variable incidence of AA due to the substantial differences in sex, age or development status of the countries in different regions of the World is a reality [Citation3,Citation18]. Instead of comparison of such factors gathered from several geographical regions of the World, epidemiological evaluation of AA should be performed according to data of each country or region.
It is also interesting to see this continuing upward age trend in the present study and the other studies exploring the cases starting from 1969 to 2016 [Citation1, Citation10]. It has been thought that increasing life span and better diagnostic testing might be responsible for this issue [Citation1]. Kang et al. [Citation19] from England conclude that although admission rates for AA significantly declined between 1989 and 2000, there was an increase in hospital admissions for AA only in patients between 35 to 64 years. Even in the countries in which a decrease in the incidence of AA has been detected, its proportion among the elderly is increasing. As a conclusion, these findings show that all surgeons are more likely to be confronted with elderly patients suffering from AA in near-future [Citation10].
Based on the findings of a recent guideline, the use of computed tomography has been recommended especially in older patients with inconclusive ultrasonographic findings. In addition, it has been reported that computed tomography should be used in older patients (>40 years) who were treated with conservative management [Citation20].
The management of AA in the elderly patients via minimally invasive techniques is another speculative issue. Laparoscopic appendectomy has been regarded as a feasible and safe approach even in complicated appendicitis cases for the older patients [Citation21–24]. It is generally recommended for obese, older adult patients with co-morbidities [Citation24]. Among the minimally invasive techniques, single incision laparoscopic appendectomy has been also offered as an innovative approach. Although similar postoperative results have been reported for both single incision and standard laparoscopic appendectomies, applicability of single incision laparoscopic appendectomy in the older patients has been still questioned [Citation22,Citation24].
In the absence of complicated AA such as perforation, non-operative management of AA with antibiotics have gained popularity during the last decades [Citation25]. In summary, it has been shown that there was a treatment failure rate of approximately 8% during the primary hospitalization and an additional 20% rate of recurrent appendicitis in patients with non-operative management for AA [Citation25]. Considering this real-world data, we conclude that AA without complications can be treated using antibiotics even in the older patients.
As a recent event, the COVID pandemic has changed the attitudes of the physicians dealing with AA [Citation26]. Conservative approach has been used more frequently for mild AA during the COVID pandemic. Almost one-third of the surgeons switched to open appendectomy without an evidence-based data. Therefore, current guidelines are needed to clarify these controversial issues for AA during the COVID pandemic.
Retrospective design and use of a cohort from a single institution might be regarded as the main limitations for this study. We regarded clinical presentation, different pathological conditions including perforation and peri-appendicular abscess, morbidity and mortality out of the main scope of the study, therefore, comparison of the patients with regard to these factors was not performed. In this study, the diagnosis of AA was based on the final histopathological examination. Exclusion of the cases with normal appendix vermiformis, lack of any case with conservative treatment for suspicious AA and large sample size were the strengths of this study. In this way, it was ensured that the results are directly related to the research question.
In conclusion, it has been shown that the mean age of the patients with AA is going to be increased. Also, it has been expected that AA is going to be detected in patients whose age is getting older in-near future compared with the previous findings. This issue necessitates an accurate pathophysiological explanation for the occurrence of AA in aged people in whom the appendix vermiformis is thought to be atrophied and obliterated.
Compliance with an ethical standard
Study follows the principles of the Declaration of Helsinki.
Disclosure statement
The authors have no financial relationships relevant to this article to disclose.
The authors declare that they have no conflict of interest.
Table 1. Demographic variables of the patients with final pathological diagnosis of acute appendicitis (n = 3296) based on an annual base.
Additional information
Funding
References
- Buckius MT, McGrath B, Monk J, et al. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res. 2012;175(2):185–190.
- Oguntola AS, Adeoti ML, Oyemolade TA. Appendicitis: trends in incidence, age, sex, and seasonal variations in South-Western Nigeria. Ann Afr Med. 2010;9(4):213–217.
- Al-Omran M, Mamdani M, McLeod RS. Epidemiologic features of acute appendicitis in Ontario. Canada. Can J Surg. 2003;46:263–268.
- Anderson JE, Bickler SW, Chang DC, et al. Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995-2009. World J Surg. 2012;36(12):2787–2794.
- Wei PL, Chen CS, Keller JJ, et al. Monthly variation in acute appendicitis incidence: a 10-year nationwide population-based study. J Surg Res. 2012;178(2):670–676.
- Stein GY, Rath-Wolfson L, Zeidman A, et al. Sex differences in the epidemiology, seasonal variation, and trends in the management of patients with acute appendicitis. Langenbecks Arch Surg. 2012;397(7):1087–1092.
- Coward S, Kareemi H, Clement F, et al. Incidence of appendicitis over time: a comparative analysis of an Administrative Healthcare Database and a Pathology-Proven Appendicitis Registry. PLoS One. 2016;11(11):e0165161.
- Segev L, Keidar A, Schrier I, et al. Acute appendicitis in the elderly in the twenty-first century. J Gastrointest Surg. 2015;19(4):730–735.
- Storm-Dickerson TL, Horattas MC. What have we learned over the past 20 years about appendicitis in the elderly? Am J Surg. 2003;185(3):198–201.
- Peltokallio P, Tykkä H. Evolution of the age distribution and mortality of acute appendicitis. Arch Surg. 1981;116(2):153–156.
- Cohen-Arazi O, Dabour K, Bala M, et al. Management, treatment and outcomes of acute appendicitis in an elderly population: a single-center experience. Eur J Trauma Emerg Surg. 2017;43(5):723–727.
- United Nations 2013. World Population Aging Report. Available online: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf.
- Rahman MA, Parash TH, Banu LA. Diameter of the lymphoid follicles in the vermiform appendix of Bangladeshi cadaver. Mymensingh Med J. 2014;23:315–320.
- Bakar SM, Shamim M, Salam A, et al. Microscopic studies on postmortem vermiform appendix of the adult males of Bangladesh. Ir J Med Sci. 2016;185(1):249–257.
- Guller U, Jain N, Peterson ED, et al. Laparoscopic appendectomy in the elderly. Surgery. 2004;135(5):479–488.
- Ceresoli M, Zucchi A, Allievi N, et al. Acute appendicitis: Epidemiology, treatment and outcomes- analysis of 16544 consecutive cases. WJGS. 2016;8(10):693–699.
- Konan A, Hayran M, Kılıç YA, et al. Scoring systems in the diagnosis of AA in the elderly. Ulus Travma Acil Cerrahi Derg. 2011;17(5):396–400.
- Noudeh YJ, Sadigh N, Ahmadnia AY. Epidemiologic features, seasonal variations and false positive rate of acute appendicitis in Shahr-e-Rey, Tehran. Int J Surg. 2007;5(2):95–98.
- Kang JY, Hoare J, Majeed A, et al. Decline in admission rates for acute appendicitis in England. Br J Surg. 2003;90(12):1586–1592.
- Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27.
- Di Saverio S, Mandrioli M, Sibilio A, et al. A cost-effective technique for laparoscopic appendectomy: outcomes and costs of a case-control prospective single-operator study of 112 unselected consecutive cases of complicated acute appendicitis. J Am Coll Surg. 2014;218(3):e51–e65.
- Mandrioli M, Inaba K, Piccinini A, et al. Advances in laparoscopy for acute care surgery and trauma. World J Gastroenterol. 2016;22(2):668–680.,
- Gavriilidis P, de’Angelis N, Katsanos K, et al. Acute Appendicectomy or Conservative Treatment for Complicated Appendicitis (Phlegmon or Abscess)? A Systematic Review by Updated Traditional and Cumulative Meta-Analysis. J Clin Med Res. 2019;11(1):56–64.
- Di Saverio S, Mandrioli M, Birindelli A, et al. Single-incision laparoscopic appendectomy with a low-cost technique and surgical-glove port: "How To Do It" with comparison of the outcomes and costs in a consecutive single-operator series of 45 cases. J Am Coll Surg. 2016;222(3):e15–e30.
- Podda M, Gerardi C, Cillara N, et al. Antibiotic Treatment and Appendectomy for Uncomplicated Acute Appendicitis in Adults and Children: A Systematic Review and Meta-analysis. Ann Surg. 2019;270(6):1028–1040.
- Ielpo B, Podda M, Pellino G, et al. Global attitudes in the management of acute appendicitis during COVID-19 pandemic: ACIE Appy Study. Br J Surg. 2020.DOI:https://doi.org/10.1002/bjs.11999