Abstract
Objective
This study aims to evaluate the overall efficacy and safety between holmium laser enucleation of the prostate (HoLEP) and bipolar transurethral enucleation of the prostate (B-TUEP) for the treatment of benign prostatic hyperplasia (BPH).
Method
We systematically searched electronic databases (PubMed, Scopus, Web of Science, and Cochrane Library) to identify eligible comparative studies as of July 2021. The parameters including perioperative results, complications, and functional outcomes were evaluated. RevMan version 5.4 was used for the analysis.
Results
A total of 10 studies involving 1725 patients were included. HoLEP had lower operative time (p = .03), shorter catheterization time (p = .007), lower bladder irrigation time (p = .01), and higher enucleation weight (p = .01) compared with B-TUEP. However, there were no significant differences between the techniques regarding the length of stay (LOS), hemoglobin drop, transfusion rates, and complications. Furthermore, no significant differences were also observed in postoperative functional outcomes at 1, 3, 6, 12, or 24 months.
Conclusions
HoLEP has more advantages in perioperative parameters compared with B-TUEP, but no significant differences are found regarding functional outcomes and complications. Large-scale studies with long-term follow-up are required to compare the outcomes of these two techniques.
Introduction
Benign prostatic hyperplasia (BPH) is a progressive disease in middle-aged and elderly men, and its prevalence increases with age [Citation1]. The application of drugs such as α1-blockers and 5α-reductase inhibitors can alleviate lower urinary tract obstruction secondary to BPH, but there are still many patients who need surgical intervention. Traditional transurethral resection of the prostate (TURP) is the “gold standard” for the treatment of BPH [Citation2,Citation3]. Although technological improvements have made TURP performed by experienced surgeons generally safe, complications such as bleeding and transurethral resection syndrome are also frequently reported [Citation4].
In recent years, the surgical treatment of BPH has been continuously developed. The emerging minimally invasive techniques strive to be the same as standard resection, but with higher safety. Laser-based methods are combined with improved prostate enucleation techniques, such as the successful introduction of holmium laser enucleation of the prostate (HoLEP). This method is not only effective in hemostasis but also has advantages in improving the postoperative functional outcome of patients [Citation5,Citation6]. Some studies have reported that regardless of the size of the prostate, HoLEP may be more effective and safer than TURP [Citation7–9]. However, steep learning curves are the main obstacles to the widespread implementation of this procedure [Citation10]. Bipolar transurethral enucleation of the prostate (B-TUEP) as a combination equalizer of highly skilled TURP with a good result of laser enucleation has appeared [Citation11]. B-TUEP has been implemented as a safe, effective, and durable procedure for BPH in some medical centers, and it has superior outcomes at both short- and long-term follow-up compared with TURP [Citation12].
Some studies have compared HoLEP and B-TUEP, but the pros and cons of the two technologies remain controversial. Neill et al. [Citation13] reported that HoLEP had similar efficacy to B-TUEP, and it was associated with shorter operation time and fewer postoperative irrigation requirements. Another study conducted by Magistro et al. [Citation14] demonstrated no statistical difference regarding perioperative parameters, clinical outcomes, and the safety profile of both procedures. Thus, the purpose of this study was to use data from comparative studies to evaluate the safety and efficacy of HoLEP and B-TUEP, providing a high level of evidence for clinical practice.
Materials and methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria [Citation15] and was registered in the PROSPERO (ID: CRD42021271100).
Search strategy
Four electronic databases (PubMed, Scopus, Web of Science, and Cochrane Library) were searched to identify eligible studies up to July 2021, with no restrictions in terms of study or language. Search items included “holmium laser,” “bipolar,” “plasma,” “plasmakinetic,” “plasma-kinetic,” “enucleation,” “prostate,” “benign prostatic hyperplasia,” “BPH.” Reference lists of relevant studies and reviews were also manually searched. Two authors reviewed the literature independently, and any differences settled through discussion with a third author.
Inclusion and exclusion criteria
Studies that meet the following criteria were included: (1) randomized controlled trials (RCTs), cohort studies, or case-control studies; (2) patients with BPH requiring elective endoscopic enucleation of the prostate; (3) compared HoLEP with B-TUEP; and (4) studies that have evaluated at least one clinical efficacy or safety outcome. The exclusion criteria were as follows: (1) male with or previously suffering from prostate cancer; (2) reviews, comments, letters, case reports, meeting abstracts, and unpublished articles; (3) studies with unavailable data or insufficient data for analyses; and (4) duplicated studies based on the same patients.
Data extraction
Two independent reviewers extracted the required data from eligible studies, which were as follows: first author, publication date, study area, intervention method, sample size, age, perioperative and functional outcomes such as prostate volume, prostate-specific antigen (PSA), International Prostate Symptom Score (IPSS), quality of life (QoL), maximum urinary flow rate (Qmax), post-void residual volume (PVR), International Index of Erectile Function-5 (IIEF-5) score, operative time, enucleation weight, hemoglobin drop, catheterization time, bladder irrigation time, length of stay (LOS), blood transfusion rate, complications, and follow-up time. If available, complications graded according to the Clavien–Dindo classification (CDC) system were analyzed.
Quality assessment
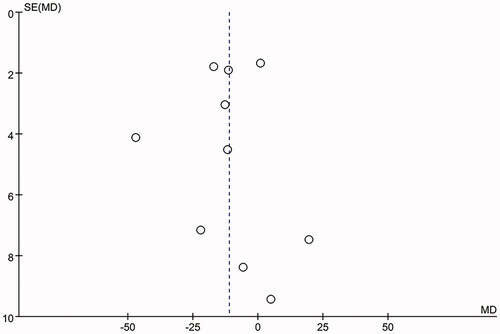
The level of evidence for each study was assessed according to the evidence assessment standards published by the Oxford Evidence-based Medicine Center [Citation16]. The quality of all included RCTs was estimated by the Jadad Scale [Citation17], whereas the quality of non-RCTs was established by using the Newcastle–Ottawa scale [Citation18]. In the current meta-analysis, a score of ≥ 3 was considered high-quality for the RCTs, and a score of ≥ 7 was considered high-quality for the non-RCTs. In addition, the funnel plot by Begg’s method was used to assess the publication bias.
Statistical analysis
The statistical analysis of this study was performed using Review Manager version 5.4. Continuous variables were pooled as mean difference (MD), whereas odds ratio (OR) was used for dichotomous variables. The random-effects model was used and heterogeneity between studies was estimated using Cochran’s Q and I2 tests. Low, moderate, and substantial heterogeneity was represented by the upper limit of the I2 value of 25%, 50%, and 75%, respectively. If the data in the article was expressed as the median (interquartile range), mean ± standard deviation (SD) was calculated according to the method described by Hozo et al. [Citation19]. In order to maintain the homogeneity of the data, the LOS is in “days,” and the catheterization time and bladder irrigation time are in “hours.” Moreover, sensitivity analysis was performed by excluding one or more studies suspected of causing heterogeneity. For all analyses, 95% confidence intervals (CIs) were reported. p<.05 was defined as statistically significant.
Result
Study characteristics
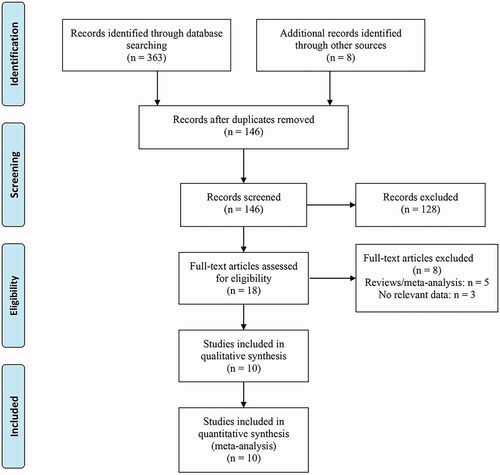
The search identified 371 studies. A total of 10 studies [Citation5,Citation13,Citation14,Citation20–26] involving 1725 patients (932 cases for HoLEP and 793 for B-TUEP) were included in the meta-analysis after removing duplicates and viewing the abstracts and full texts (). The key characteristics of these studies are recorded in . Four of these studies are RCTs and the other six are prospective or retrospective studies. These studies were conducted in many countries, including China, Egypt, Italy, Germany, France, and New Zealand. The follow-up period for the included studies ranged from 1 to 36 months. In most studies, functional outcomes were measured 1, 3, 6, 12, or 24 months after surgery. The quality assessment results of each study are contained in Supplementary material 1.
Table 1. Characteristics and designs of the included studies.
Table 2. Baseline characteristics of patients.
Baseline parameters
Compared with the B-TUEP group, the preoperative PV was larger in the HoLEP group (p = .02). However, there were no significant differences in preoperative PSA (p=.09), IPSS (p = .73), QoL (p = .31), Qmax (p = 0.87), and PVR (p = .42) between the two groups (Supplementary material 2).
Perioperative parameters
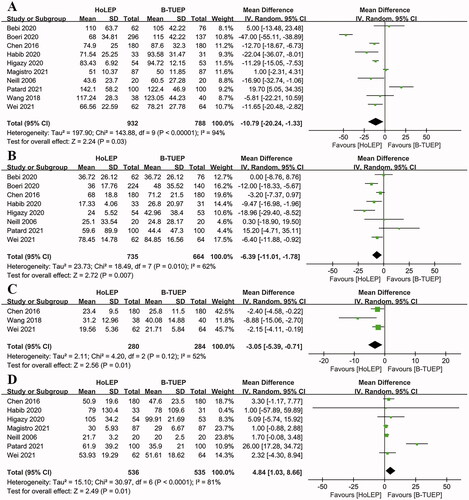
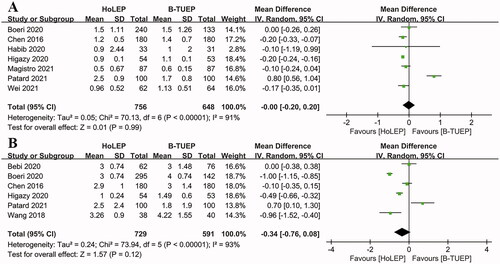
The operation time (MD −10.79 min; 95% CI −20.24, −1.33; p = 0.03), catheterization time (MD −6.39 h; 95% CI −11.01, −1.78; p = .007), and bladder irrigation time (MD −3.05 h; 95% CI −5.39, −0.71; p = .01) of HoLEP were significantly shorter than that of B-TUEP. Higher enucleation weight was also observed in the HoLEP group (MD 4.84 g; 95% CI 1.03, 8.66; p = 0.01) (). However, there were no significant differences between the procedures regarding hemoglobin drop (MD −0.00 g/dL; 95% CI −0.20, 0.20; p=.99) and LOS (MD −0.34 d; 95% CI −0.76, 0.08; p = .12) ().
Complications
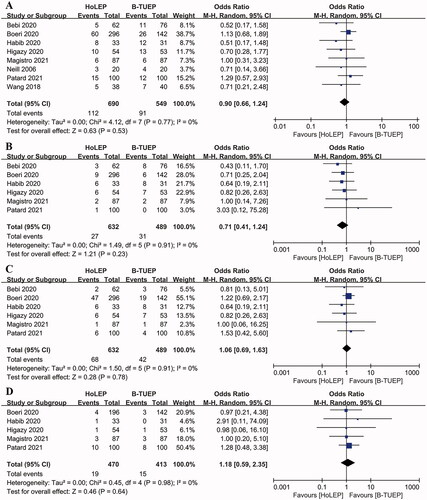
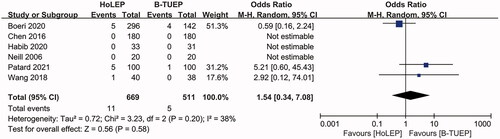
Fewer overall postoperative complications were found in the HoLEP group, but the difference did not reach the level of statistical significance (OR 0.90; 95% CI 0.66, 1.24; p = .53). There was no significant difference between HoLEP and B-TUEP regarding the odds of CDC grade I (OR 0.71; 95% CI 0.41, 1.24; p = .23), grade II (OR 1.06; 95% CI 0.69, 1.63; p = .78), and grade III (OR 1.18; 95% CI 0.59, 2.35; p = .64) (). In addition, transfusion rates were similar in the HoLEP and B-TUEP groups (OR 1.54; 95% CI 0.34, 7.08; p = .58; ).
Functional outcomes
The pooled results revealed that there was no difference in IPSS at 1 month (MD 0.40; 95% CI −0.18, 0.98; p = .18), 3 months (MD 0.61; 95% CI −1.40, 2.62; p = .55), 6 months (MD 0.86; 95% CI −0.74, 2.46; p = .29), 12 months (MD 0.11; 95% CI −0.26, 0.49; p=.55), and 24 months (MD −0.16; 95% CI −0.68, 0.37; p = .56) of follow-up between the two groups (Supplementary material 3).
There was no significant difference between the two groups in regard to QoL at 1 month (MD 0.25; 95% CI −0.27, 0.78; p=.34), 6 months (MD 0.10; 95% CI −0.27, 0.47; p = .59), 12 months (MD 0.18; 95% CI −0.09, 0.44; p = .19) and 24 months (MD −0.02; 95% CI −0.13, 0.09; p = .72; Supplementary material 3).
No significant differences were found in Qmax between groups at 1 month (MD 0.74; 95% CI −0.60, 2.08; p = .28), 3 months (MD −1.26; 95% CI −4.27, 1.74; p=.41), 6 months (MD −0.88; 95% CI −2.17, 0.41; p = .18), 12 months (MD −0.14; 95% CI −1.05, 0.77; p=.76), and 24 months (MD 0.16; 95% CI −0.52, 0.83; p = .65) after surgery (Supplementary material 3).
The combined analysis of PVR showed that there was no difference between HoLEP and B-TUEP at 1 month (MD −0.04; 95% CI −1.67, 1.60; p = .96), 3 months (MD −1.55; 95% CI −6.36, 3.26; p = .53), 6 months (MD −0.38; 95% CI −2.50, 1.74; p = .72), 12 months (MD −0.48; 95% CI −2.01, 1.04; p = .53), and 24 months (MD −0.48; 95% CI −2.43, 1.48; p = .63; Supplementary material 3).
IIEF-5 score was used for postoperative sexual function assessments. The Follow-up periods ranged from 6 to 36 months, and values from the last follow-up were included in the present meta-analysis. No significant difference was observed between groups regarding IIEF-5 (MD 0.20; 95% CI −1.70, 2.09; p = 0.84; Supplementary material 3).
Discussion
Although TURP is still the most commonly used procedure for BPH, recent advances in energy and technology have led to the emergence of various new transurethral surgical therapies, such as laser, bipolar enucleation, or vaporization, and Aquablation®, Making the treatment of BPH diversified [Citation27]. Since HoLEP was first described by Gilling in 1998 [Citation28], a large number of publications have published reports on the effectiveness, safety, and durability of the technology. HoLEP has been considered the new standard of surgical management for BPH in the twenty first century, but the implementation of this surgical method faces a steep learning curve and expensive costs [Citation10,Citation29]. Furthermore, as a combination of bipolar and enucleation technology, the B-TUEP is also regarded as a safe and effective alternative to TURP or open prostatectomy [Citation30,Citation31]. In B-TUEP, the adenoma was completely dissected along the surgical sac plane in a manner similar to the index finger of the surgeon during open prostatectomy, which is equivalent to HoLEP and is also considered an anatomic enucleation technique [Citation32]. Recent studies have shown that B-TUEP could be considered as a “size-independent procedure” because it provides a way to relieve symptoms for men with a prostate of all sizes, and has the same clinical efficacy and safety [Citation33].
Despite a growing amount of data reported in the literature, the comparison of HoLEP, and B-TUEP for the management of BPH is still unclear. And with that background, we performed a meta-analysis of the reported comparative studies to update the contemporary evidence base. In this study, we observed that HoLEP could have more advantages in perioperative parameters than B-TUEP. The significantly lower operation time, catheterization time, and bladder irrigation time in the HoLEP cohort. The biggest difference was found in the study of Patard et al. [Citation25], which used a bipolar device with an oval electrode button. This technology has been developed for vaporization and coagulation. Another possible explanation is the proficiency of the surgeon. Boeri et al., Habib et al., and Higazy et al. [Citation5,Citation23,Citation24] reported that the surgeons had rich experience in endoscopic enucleation (namely, >50 cases per technique). While, in the study of Patard et al. [Citation25], both two surgical methods were performed by inexperienced surgeons (>15 cases). In general, the key to shortening the operation time of endoscopic enucleation is to accurately identify the surgical capsule plane. Meanwhile, hemostasis is also very important to make the field of vision as clear as possible during the whole process [Citation34].
Our quantitative analysis revealed that hemoglobin drop and LOS did not differ between the two surgical techniques. Holmium laser is a pulsed laser with solidifying properties that penetrates tissue below the surface of the resection line and causes hemostasis. Hence, it has an excellent hemostatic effect when the prostate tissue is r enucleated [Citation13]. However, according to Enmar Habib [Citation23], since the process of enucleating tissue was accompanied by immediate bipolar electrical cauterization of any source of bleeding, so he observed a similar decrease in hemoglobin between the groups. Boeri et al. [Citation5] also demonstrated similar decreases in hemoglobin in patients receiving anticoagulant/antiplatelet therapy regardless of the type of surgery. Based on our results, this study supports the feasibility of using the HoLEP and B-TUEP procedures for daytime surgery. However, high-quality RCTs are needed to verify our findings.
The present study also suggested that the HoLEP group was associated with more enucleation weight (p = .01). Due to significant differences in the results of different studies, substantial heterogeneity exists (I2 =81%). This result, although important, should be interpreted with caution. Our analysis found that the prostate volume in the holmium laser group was higher than that in the bipolar group, which may be one of the reasons for the difference in enucleation weight. In the prospective cohort conducted by Patard et al. [Citation25], the weight of enucleation tissue was significantly higher for HoLEP (61.9 ± 39.2 versus 35.9 ± 21.0 g, p< .001), and differing from the other studies analyzed. They also claimed that part of the prostate tissue may be vaporized during the enucleation, resection, or morcellation process. Enucleation weight is a complex parameter and its measurement is affected by many factors. For example, weight varies according to measurement time and humidity [Citation35]. Moreover, Yosuke Hirasawa reported the effectiveness of enucleation not only increased with prostate size, and when the surgeon experience level more than 50 cases also improved significantly [Citation36]. This means that technical proficiency is essential for performing endoscopic enucleation. Of note, Yamamichi and colleagues confirmed that resection of the prostate weight was an important factor in improving voiding symptoms (Qmax) in post-HoLEP [Citation37]. Nevertheless, in the pooled analysis, no difference was observed in the Qmax between the groups.
Regarding postoperative functional outcomes, there were no significant differences in IPSS, QoL, Qmax, and PVR between HoLEP and B-TUEP during short- and long-term follow-up, which was highly consistent with the analysis of each included study. A growing body of clinical evidence indicates that surgical technique and experience seem to be more important than the energy source of endoscopic enucleation [Citation38]. Therefore, the proficiency of surgeons must be ensured to achieve the clinical benefits of HoLEP and B-TUEP technologies. Furthermore, no difference in the IIEF-5 score was observed in the pooled analysis, suggesting that neither technique influenced patients' erectile function.
The incidence of surgical complications has always been a concern by doctors. Our study demonstrated that HoLEP had a similar rate of overall complications as those of B-TUEP. According to the CDC system classification, we also found no difference in complications between the groups regardless of grade. In addition, no significant difference was observed in transfusion rates between the two energies. These findings are similar to those from previous studies [Citation5,Citation25]. Transfusion rates may differ greatly from institution to institution because of patient comorbidities and surgeon preferences [Citation39], larger study is needed to clarify the safety of these two enucleation techniques.
HoLEP is considered superior in terms of perioperative period, including shorter operation, catheterization, and bladder irrigation time. In contrast, B-TUEP has its own advantages in that the device is easily accessible and cost-effective [Citation25,Citation26]. B-TUEP is related to the operating equipment commonly used in urology. Therefore, it may be easier to get started [Citation25]. The surgeon can switch back directly to TURP if B-TUEP fails for any reason. Furthermore, B-TUEP seems to have a short learning curve compared with HoLEP. Feng et al. [Citation40] found a learning curve of about 40 cases for B-TUEP, while HoLEP requires roughly 40–60 cases to reach a proficient platform [Citation41]. However, the length of the learning curve may vary greatly depending on the difficulty of the enucleation method [Citation42]. From a technical point of view, B-TUEP has the same principle as HoLEP, providing surgeons with an alternative energy platform and allowing more informed choices based on patient and center conditions [Citation43]. In general, as a cost-effective device, the bipolar system could be used in many medical institutions (especially centers without holmium laser equipment).
This study has clinical value as the first meta-analysis to directly compare the safety and efficacy of HoLEP and B-TUEP in patients with BPH. However, some limitations in the analysis must also be emphasized. First, the inclusion criteria of various studies vary to a certain extent, so there is certain heterogeneity among studies. However, it included a relatively large number of patients (n = 1725) and, therefore, was representative of the available evidence. Second, only four studies were RCTs, providing high-level evidence for the outcomes of HoLEP and B-TUEP in the treatment of BPH. The six studies used a non-random design, so the risk of selection bias would inevitably increase. Third, high heterogeneity was observed in some outcome parameters. Differences in laser power, energy equipment, surgeon experience, and result evaluation may indicate high heterogeneity. Although we conducted a meta-analysis of these items using a random-effects model, these effects may still exist. Finally, for some outcomes, such as the IIEF-5 score, the pooled results contain only data from three studies; this could make the result less credible.
Conclusions
The current meta-analysis indicates that both HoLEP and B-TUEP are safe and effective surgical methods for treating BPH. HoLEP has more advantages in operation, catheterization, and bladder irrigation time compared with B-TUEP, but no significant differences are found regarding functional outcomes and complications. The degree of heterogeneity among studies limits the strength of our conclusions, and higher quality, large-scale RCTs with long-term follow-up are required to compare the outcomes of these two techniques.
Author contributions
The authors have no proprietary interest in any aspect of this study. Q. Wei and Y. X. Li are responsible for manuscript conceptualization. J. Z. Li, D. H. Cao, and Y. Huang are responsible for manuscript writing and data analysis. Z. Y. Xia, C. Y., Meng and L. Peng are responsible for data analysis. Q. Wei is responsible for manuscript editing.
Supplemental Material
Download MS Word (10.9 MB)Disclosure statement
All authors declare that they have no conflict of interest.
Additional information
Funding
References
- Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol. 2008;179(5):S75–S80.
- Gratzke C, Bachmann A, Descazeaud A, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015;67(6):1099–1109.
- Parsons JK, Dahm P, Köhler TS, et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2020. J Urol. 2020;204(4):799–804.
- Omar MI, Lam TB, Alexander CE, et al. Systematic review and Meta-analysis of the clinical effectiveness of bipolar compared with monopolar transurethral resection of the prostate (TURP). BJU Int. 2014;113(1):24–35.
- Boeri L, Capogrosso P, Ventimiglia E, et al. Clinical comparison of holmium laser enucleation of the prostate and bipolar transurethral enucleation of the prostate in patients under either anticoagulation or antiplatelet therapy. Eur Urol Focus. 2020;6(4):720–728.
- Enikeev D, Taratkin M, Morozov A, et al. Long-Term outcomes of holmium laser enucleation of the prostate: a 5-Year Single-Center experience. J Endourol. 2020;34(10):1055–1063.
- Park S, Kwon T, Park S, et al. Efficacy of holmium laser enucleation of the prostate in patients with a small prostate (≤30 mL). World J Mens Health. 2017;35(3):163–169.
- Gazel E, Kaya E, Yalcin S, et al. Comparison of the efficacy of holmium laser enucleation of the prostate in treating prostate volumes of ≤80 and > 80 mL. Urol Int. 2019;102(3):306–310.
- Yılmaz S, Yalçın S, Yılmaz M, et al. Comparison of outcomes of holmium enucleation of the prostate for small- and moderate-sized prostates. Andrologia. 2021;53(3):e13970.
- Robert G, Cornu JN, Fourmarier M, et al. Multicentre prospective evaluation of the learning curve of holmium laser enucleation of the prostate (HoLEP). BJU Int. 2016;117(3):495–499.
- Ryang SH, Ly TH, Tran AV, et al. Bipolar enucleation of the prostate-step by step. Andrologia. 2020;52(8):e13631.
- Arcaniolo D, Manfredi C, Veccia A, et al. Bipolar endoscopic enucleation versus bipolar transurethral resection of the prostate: an ESUT systematic review and cumulative analysis. World J Urol. 2020;38(5):1177–1186.
- Neill MG, Gilling PJ, Kennett KM, et al. Randomized trial comparing holmium laser enucleation of prostate with plasmakinetic enucleation of prostate for treatment of benign prostatic hyperplasia. Urology. 2006; 68(5):1020–1024.
- Magistro G, Schott M, Keller P, et al. Enucleation vs. Resection: a matched-pair analysis of TURP, HoLEP and bipolar TUEP in medium-sized prostates. Urology. 2021;154:221–226.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- Brozek JL, Akl EA, Alonso-Coello P, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64(5):669–677.
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in Meta-analyses. Eur J Epidemiol. 2010;25(9):603–605.
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13.
- Chen YB, Xu H, Xu H, et al. Comparison of plasmakinetic enucleation of the prostate with holmium laser enucleation of the prostate in the treatment of benign prostate hyperplasia. Int J Clin Exp Med. 2016;9(4):7328–7333.
- Wang JW, Zhang MD, Ping H, et al. [Plasmakinetic enucleation of the prostate versus holmium laser enucleation of the prostate for benign prostatic hyperplasia]. Zhonghua Nan Ke Xue. 2018;24(12):1084–1088.
- Bebi C, Turetti M, Lievore E, et al. Sexual and ejaculatory function after holmium laser enucleation of the prostate and bipolar transurethral enucleation of the prostate: a single-center experience. Int J Impot Res. 2020. [Online ahead of print]
- Habib E, Ayman LM, ElSheemy MS, et al. Holmium laser enucleation vs bipolar plasmakinetic enucleation of a large volume benign prostatic hyperplasia: a randomized controlled trial. J Endourol. 2020;34(3):330–338.
- Higazy A, Tawfeek AM, Abdalla HM, et al. Holmium laser enucleation of the prostate versus bipolar transurethral enucleation of the prostate in management of benign prostatic hyperplasia: a randomized controlled trial. Int J Urol. 2021;28(3):333–338.
- Patard PM, Roumiguie M, Sanson S, et al. Endoscopic enucleation for prostate larger than 60 mL: comparison between holmium laser enucleation and plasmakinetic enucleation. World J Urol. 2021;39(6):2011–2018.
- Wei Z, Tao Y, Gu M, et al. Plasma kinetic enucleation vs. holmium laser enucleation for treating benign prostatic hyperplasia: a randomized controlled trial with a 3-Year Follow-Up. J Endourol. 2021;35(10):1533-1540.
- Lee MS, Assmus M, Agarwal D, et al. Contemporary practice patterns of transurethral therapies for benign prostate hypertrophy: results of a worldwide survey. World J Urol. 2021;39(11):4207–4213.
- Fraundorfer MR, Gilling PJ. Holmium: YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results. Eur Urol. 1998;33(1):69–72.
- Lourenco T, Armstrong N, N’Dow J, et al. Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement. Health Technol Assess. 2008;12(35):iii, ix–ix-x. 1–146, 169–515.
- Cornu JN. Bipolar, monopolar, photovaporization of the prostate, or holmium laser enucleation of the prostate: how to choose what’s best? Urol Clin North Am. 2016;43(3):377–384.
- Geavlete B, Stanescu F, Iacoboaie C, et al. Bipolar plasma enucleation of the prostate vs. open prostatectomy in large benign prostatic hyperplasia cases - a medium term, prospective, randomized comparison. BJU Int. 2013;111(5):793–803.
- Liu C, Zheng S, Li H, et al. Transurethral enucleation and resection of prostate in patients with benign prostatic hyperplasia by plasma kinetics. J Urol. 2010;184(6):2440–2445.
- Bebi C, Turetti M, Lievore E, et al. Bipolar transurethral enucleation of the prostate: is it a size-independent endoscopic treatment option for symptomatic benign prostatic hyperplasia? PLoS One. 2021;16(6):e0253083.
- Abdulwahab Al-Radhi M, Lun LK, Safi M, et al. Can bipolar transurethral enucleation of the prostate be a better alternative to the bipolar transurethral resection of the prostate: a prospective comparative study. Medicine (Baltimore). 2021;100(20):e25745.
- Pallauf M, Kunit T, Ramesmayer C, et al. Endoscopic enucleation of the prostate (EEP). the same but different-a systematic review. World J Urol. 2021;39(7):2383–2396.
- Hirasawa Y, Kato Y, Fujita K. Transurethral enucleation with bipolar for benign prostatic hyperplasia: 2-Year outcomes and the learning curve of a single surgeon’s experience of 603 consecutive patients. J Endourol. 2017;31(7):679–685.
- Yamamichi F, Shigemura K, Kitagawa K, et al. Predictive factors of improvement for voiding symptoms after holmium laser enucleation of the prostate. Int J Urol. 2019;26(1):136–137.
- Herrmann TRW, Gravas S, de la Rosette JJ, et al. Lasers in transurethral enucleation of the Prostate-Do We really need them. J Clin Med. 2020;9(5):1412.
- Li J, Cao D, Meng C, et al. Comparison of the efficacy and safety of minimally invasive simple prostatectomy and endoscopic enucleation of prostate for large benign prostatic hyperplasia. Front Med. 2021;8:773257.
- Feng L, Song J, Zhang D, et al. Evaluation of the learning curve for transurethral plasmakinetic enucleation and resection of prostate using a mentor-based approach. Int Braz j Urol. 2017;43(2):245–255.
- Brunckhorst O, Ahmed K, Nehikhare O, et al. Evaluation of the learning curve for holmium laser enucleation of the prostate using multiple outcome measures. Urology. 2015;86(4):824–829.
- Enikeev D, Morozov A, Taratkin M, et al. Systematic review of the endoscopic enucleation of the prostate learning curve. World J Urol. 2021;39(7):2427–2438.
- Xu P, Xu A, Chen B, et al. Bipolar transurethral enucleation and resection of the prostate: whether it is ready to supersede TURP? Asian J Urol. 2018;5(1):48–54.