Abstract
Aim
This study explores the risk of diabetes-associated lower and upper urinary tract diseases among male older adults aged 45 and above in India.
Methods
Longitudinal Ageing Study in India (LASI), 2017–2018 data was used in this study. The prevalence of various urinary tract problems and diabetes among male older adults was estimated by background characteristics using bivariate cross-tabulation. In addition, multivariate logistic regression was applied to examine the likelihood of urological disorders associated with diabetes.
Result
The prevalence of incontinence was highest among male older adults with diabetes, followed by kidney stones, benign prostatic hyperplasia, and chronic renal failure. Multivariate logistic regression estimation showed that men diagnosed with diabetes were 80% more likely to experience chronic renal failure, 78% more likely to suffer from incontinence, and 37% more likely to suffer from kidney stones than those without diabetes when controlling for various socio-demographic, behavioral, and co-morbidity status of the older adults.
Conclusions
The study findings suggest that diabetes is associated with multiple urinary complications among male older adults in India and needs more careful investigation of the phenomenon. Independent risk factors such as changes in lifestyle with regular monitoring and diagnosis may help to prevent the progression of diabetes and reduce the risk of diabetes-associated lower and upper urinary tract diseases among male older adults.
1. Introduction
Diabetes and its complications can have a severe impact on the urinary system. The kidneys are affected by diabetes, which increases the risk of kidney damage and failure [Citation1]. In addition, diabetes is associated with poor kidney function, which can lead to kidney stones [Citation2]. High blood pressure is another complication of diabetes that can lead to kidney disease [Citation3]. Some studies have shown that men who develop diabetes may also develop lower urinary tract symptoms (LUTS) or incontinence. The risk for developing LUTS or incontinence increases with age, particularly in men older than 80 years of age [Citation4]. Diabetes and urinary tract problems are common among older adults [Citation5].
The National Institute on Aging (NIA) estimates that approximately one in four older adults have diabetes, and this number is expected to increase to more than one in three by 2030. Older adults with type 2 diabetes may have more difficulty controlling their blood sugar levels and can experience excessive thirst, frequent urination, and weight loss because of the disease [Citation6]. Urinary tract problems are also common among older adults. This can affect their ability to live independently and may lead to hospitalization or death if left untreated. Diabetes, which affects more than 30 million people in the United States, is a serious chronic disease that can lead to kidney disease, heart disease, and other complications [Citation7].
The number of older adults with diabetes has grown steadily over the last decade, according to the Centers for Disease Control and Prevention (CDC). The CDC estimates that about 27 percent of people age 65 and older have diabetes [Citation7]. But this figure underestimates the problem because many people with diabetes do not know it or do not visit their doctor for help. Older men are at an especially high risk for developing some forms of diabetes – especially if they also have family history of the condition or other risk factors such as obesity, high blood pressure, and high cholesterol levels [Citation7,Citation8].
Diabetes is a serious health condition that affects millions of people worldwide. It can be treated and manageable, but it is important to identify and manage the risk factors for diabetes. Urinary tract problems are common among older men [Citation9]. The most common types of urinary tract problems include: urinary tract infections (UTIs). UTIs are caused by bacteria that get into the urinary tract, usually through contact with another person’s urine [Citation9]. Symptoms include burning with urination, frequent urination, a strong or foul odor while urinating and pain or pressure in the bladder or lower pelvis [Citation9].
The most common problems for men with diabetes are kidney disease and UTIs, which can lead to dangerous blood clots [Citation10,Citation11]. UTIs can be caused by bacteria, viruses, or other organisms [Citation12]. If left untreated, they can spread from the kidneys to the blood stream and cause an infection that is difficult to treat [Citation13]. Kidney disease progresses over time, but it can also be reversed with treatment. Patients should have regular kidney tests to determine if their kidneys are working properly and if they are at risk for developing kidney disease [Citation14]. UTIs can be prevented by taking medication regularly, drinking plenty of fluids, and using a clean catheter when going to the bathroom [Citation15,Citation16].
In India, older adults constitute a significant portion of the total population and carry comparatively higher prevalence of type-2 diabetes. Parallel to the diabetes burden, older adults in India are also exposed to multiple urinary complications along with other co-morbidities due to diabetes. In the above context, this study exclusively examined the diabetes associated differential in the prevalence and risk of chronic renal failure (CRF), urinary incontinence (UI), kidney stone, and benign prostatic hyperplasia (BPH) among male older adults aged 45 and above within a cross-sectional framework using the population-based survey, Longitudinal Ageing Study in India (LASI), Wave 1.
2. Data
Longitudinal Ageing Study in India (LASI) is a prospective cohort study of Indian older adults and this study utilized the baseline (wave 1) data from the survey. The survey was conducted during April 2017 to December 2018 across 35 states and union territories of India. The dataset is accessible subjected to a data request through https://www.iipsindia.ac.in/content/LASI-data. This survey is a part of the Global Health and Retirement Study (HRS). LASI wave 1 is the latest nationally representative dataset on older adults in India and provides the crucial information on demographic, socio-economic, familial, and health of the individuals. The target population of this survey was the older adults aged 45 and above and their spouses irrespective of their age and every individual was administered with three survey schedules – household, individual, and community schedule in the face-to-face interview. The survey instrument and the questionnaire were tested prior to the survey. The survey adopted a multistage area probability cluster sampling design to collect the samples. Within every state, a three-stage sampling was employed in the rural areas while a four-stage sampling design was employed in the urban areas. The details of the sampling design, survey instruments, and estimates are available elsewhere [Citation17]. The ethical clearance for this survey was received from the Indian Council of Medical Research (ICMR) and International Institute for Population Sciences, Mumbai and thus, this study required no further ethical approval. A total of 72,250 older adults and their spouses were interviewed in this survey from 42,949 LASI age-eligible (households with at least one member aged 45 and above) households. Of the total sampled individuals, 27,661 male older adults aged 45 and above constitute the analytical sample of this study.
2.1. Outcome variable
The present study identified four different lower and upper urinary tract diseases among male older adults. The selected diseases are chronic renal failure (CRF), urinary incontinence (UI), kidney stone, and benign prostatic hyperplasia (BPH) in this study. During the survey, individuals were asked to respond to the following question: “Have you ever been diagnosed with any of the following urogenital conditions or diseases? (a) Chronic Renal Failure, (b) Incontinence, (c) Kidney Stones, (d) BPH (Benign Prostatic Hyperplasia), and (e) None.” The responses were then coded as Yes “1” and No “0” to mark the occurrence of any above mentioned urinary tract diseases among older adult men in India.
2.2. Independent variable (predictor)
To assess the state of diabetes among individuals, self-reported diabetes information has been used from the survey. The respondents were asked, “Has any health professional ever diagnosed you with diabetes?” The responses were then coded as Yes “1” and No “0” to mark the association between diabetes as the main predictor with four selected lower and upper urinary tract diseases among male older adults in India.
2.3. Control variables (confounders)
We have adjusted the association of diabetes with urinary tract diseases for 11 socio-economic, bio-demographic, and behavioral variables. Age of the respondent was a continuous variable consisting of adults aged 45 or more years, which we have categorized into 45–59 and 60+ year male individuals [Citation17]. The individual’s residence was dichotomous, coded as “rural” and “urban.” Educational qualification was coded as “No schooling,” “Completed primary,” “Completed secondary,” and “Completed diploma/college.” Marital status was coded as: “Currently married,” “Widowed,” “Divorced/separated,” and “Not married.” The economic wellbeing of the individual was identified through the summary measure of monthly per capita consumption expenditure (MPCE), which was based on the food and nonfood expenses. The variable consists of five different economic quintiles: poorest, poor, middle, rich, and richest [Citation17]. To control the behavioral factors such as engagement in moderate energetic activities (EMEA) variable was coded as 0 “never,”1 “non-daily,” and 2 “Daily.” Both tobacco smoking and alcohol consumption status were coded as 0 “No” and 1 “Yes” for all the older adult men aged 45 and above. Furthermore, individuals with hypertension and depression were coded as 0 “No” and 1 “Yes.” As a measure of nutritional health status of the males, body mass index (BMI) of the individuals were categorized into four groups and coded as 1“underweight” (BMI <18.5), 2 “Normal” (BMI ≥18.5 to <25), 3 “Overweight” (BMI ≥25 to <30), and 4 “Obese” (BMI ≥30).
2.4. Statistical analysis
Univariate descriptive statistics (frequency and percentage for the categorical variables) was used to describe the characteristics of the study population of older adults in India. Bivariate cross-tabulation analysis was performed to estimate the prevalence of CRF, incontinence, kidney stone, and BPH by the background characteristics of the individuals. The chi-square test was also done to examine the differential in the prevalence of the target variables across the categories of the predictor variables. Multivariate logistic regression estimation was executed to check the statistical associations between the dependent and the independent variables under this study through estimated adjusted odds ratios (AORs). In addition, the interaction effects were also estimated using the multivariate logistic regression models, and the marginal probabilities were reported. We performed all statistical analyses using Stata (Version 14.1; StataCorp, College Station, TX, USA). Statistical significance was accepted at p < .05.
3. Results
3.1. Characteristics of the study population
provides a detailed understanding of the study population though descriptive statistics. A total of 27,661 male older adults aged 45 and above constitute the analytical sample of the study. Half of the older adults are in the age group of 60 and above. Two-third of the older adults reside in the rural areas. Almost one-third of the older adults do not have any formal education. Around 88% of them are currently married and 9% are widowed. Two-fifth of the older adults belong to the lowest two MPCE quintiles. Around 38% of them never engage in any kind of physical activity. More than half of the older adults (56%) do smoke and more than one-third (34%) of them consume alcohol. Almost one-fourth of them (24%) suffer from hypertension, 6% of them suffer from depression. Around one-fifth of them are underweight and more than one-tenth (13%) of the older adults are suffering from type-2 diabetes.
Table 1. Descriptive statistics of the study variables for the study population, India, LASI Wave 1, 2017–2018.
3.2. Prevalence of CRF
The prevalence of CRF is 8/1000 among older adults in India (). Age, economic status, physical activity pattern, diabetes, hypertension, and depression are the factors demonstrating a statistically significant differential in the prevalence of CRF (). The prevalence of CRF is higher (11/1000) among 60+ male older adults compared to 5/1000 among those in the age group of 45–59. Those who are never engaged in energetic activities demonstrate higher prevalence (10/1000 older adults) and the prevalence is found lowest (7/1000 older adults) among those who are engaged daily. Among the different population subgroups, male older adults with diabetes carry the highest prevalence of CRF and the observed prevalence is 15/1000 diabetic older adults compared to 7/1000 nondiabetic older adults. Whereas, older adults with hypertension show a prevalence of 14/1000 and the prevalence is 13/1000 among those older adults who have depression.
Table 2. Prevalence of CRF, incontinence, kidney stone, and BPH among per 1000 older adult men in India by their socio-economic and bio-demographic characteristics, India, LASI Wave 1, 2017–2018.
3.3. Prevalence of incontinence
The national prevalence of incontinence among older adults in India is observed highest among other three different types of urinary problems. And, the prevalence is as high as 30 per 1000 older adults in India (). The observed prevalence of incontinence shows statistically significant differential in terms of all the factors considered in this study except residence and economic status. The prevalence of incontinence is 43/1000 in the 60+ age group of male older adults and older adults with no schooling carry a prevalence of 30/1000. By marital status, widowed older adults show the highest prevalence (47/1000) followed by divorced/separated (33/1000). By physical activity pattern, who are nondaily in engaging themselves in the energetic activities or never engage themselves in energetic activities demonstrate comparatively higher prevalence of incontinence. The prevalence (35/1000) is quite high among smokers (compared to nonsmokers). On the contrary, the prevalence is observed to be higher among those who never consumed alcohol compared to those who consume. Diabetic older adults carry the highest prevalence of incontinence among all other population subgroups and the prevalence is as high as 53/1000 older adults. Older adults with hypertension and depression also carry substantially higher burden of incontinence. And in terms of BMI, older adults who are underweight carry comparatively higher prevalence (38/1000) of incontinence and the prevalence shows a gradual decrease with higher BMI.
3.4. Prevalence of kidney stone
Nationally, the average prevalence of kidney stone is 30/1000 older adult males which shows a variation across different population subgroups of different population characteristics (). Except age and smoking habit, all the variables show a statistically significant differential in the observed prevalence of kidney stone. Noticeably, the burden of kidney stone prevalence is higher in urban areas than in the rural areas of India. Among the educated, who completed primary schooling, carry an average prevalence of 35/1000 older adults which is also highest compared to the other education groups. The burden of kidney stone is found highest (32/1000 older adults) among those who are currently married and it is lowest among the never married older adults. According to economic status, it is the richer quintiles demonstrate higher prevalence of kidney stone than the poor MPCE quintiles. Those who are never engaged in energetic activities again show a higher prevalence of kidney stone among them. Among the alcohol consumers the prevalence is little higher than those who do not consume. Older adults with diabetes, hypertension, and depression reflect a very high prevalence of kidney stone and the prevalence is as high as 44/1000 among those who have depression followed by 42/1000 among those with diabetes and 41/1000 among those with hypertension. The BMI pattern of the prevalence shows that those who are overweight and obese are the one who carry higher average prevalence of kidney stone among them.
3.5. Prevalence of BPH
The average prevalence of BPH is 17/1000 male older adults in India (). Comparatively the burden of BPH is higher among 60+ males (21/1000) compared to the older adults in the age group of 45–59. There is no statistically significant difference is observed in the prevalence across rural and urban areas. The higher educated group of males carry higher prevalence of BPH. Overall, the middle and richer class reflect higher burden of BPH than those from the poorer MPCE class. The diabetic, nondiabetic differential in the prevalence is observed highly statistically significant and male older adults who suffer from diabetes carry higher burden of BPH (27/1000) compared to 16/1000 among nondiabetic male older adults. Similarly, hypertension, depression, and BMI also show statistically significant differential in the prevalence of BPH among Indian male older adults.
3.6. Prevalence of urinary problems among classified subgroups of male older adults
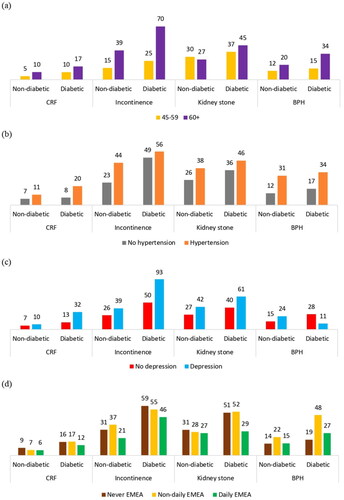
As describes different factor level differential in different urinary problems along with diabetes, this section provides the burden of different urinary diseases across classified subgroups of the male population in India considering diabetes as the key predictor and age, hypertension, depression, and physical activity as the correlates. is the graphical representation of the prevalence by the cross-classified subgroups of older adults with diabetes and age group. The figure indicates that the prevalence of incontinence is very high among the 60+ older adults with diabetes and the prevalence of CRF, kidney-stone, and BPH is always higher among this particular subgroup. presents the prevalence pattern by cross-classified categories of diabetes and hypertension, and those older adults who have diabetes and hypertension carry substantially higher burden of CRF, incontinence, kidney stone, and BPH. While estimating the prevalence pattern of all four types of urinary problems among older adults considering diabetes and depression, it is found that the prevalence of incontinence is as high as 93/1000 older adults who have diabetes and depression both followed by the prevalence of kidney stone and CRF (). Considering diabetes and physical activity, it is found that those older adults who never engage in energetic activities and have diabetes are the subgroup with highest prevalence of incontinence.
3.7. Diabetes-associated risk of different urinary problems among male older adults
The multivariate logistic regression estimation for each of the outcome variables provides the outcome-specific estimates of AORs of diabetes and other correlates considered in this specific study (). From the estimation, it is found that type-2 diabetes is a highly statistically significant predictor of CRF, incontinence, kidney stone, and BPH at p value less than 5%. The estimates of AORs suggest that older adults with diabetes are 80% (AOR: 1.80; p value < 0.01) more likely to experience CRF, 78% more likely to suffer from incontinence (AOR: 1.78; p value < 0.01), 37% more likely to suffer from kidney stone (AOR: 1.37; p value < 0.01), and 29% more likely to suffer from BPH (AOR: 1.29; p value < 0.05) than those older adults without diabetes.
Table 3. Estimated adjusted odds ratio from the multivariate logistic regression estimation for each of the outcome variables, India, LASI Wave 1, 2017–2018.
Age is found to be a significant predictor of different urinary problems except kidney stone and older adults in the 60+ age group are 2.4 times more likely to suffer from incontinence, 1.7 times more likely to suffer from CRF, and 1.9 times more likely to suffer from BPH than the older adults in the age group of 45–59. Physical activity pattern does not show any consistent association across the selected urinary problems. However, hypertension and depression are emerged to be the statistically significant predictors of different urinary problems. Older adults with hypertension are 55% more likely to experience CRF, 75% more likely to suffer from incontinence, 30% more likely to suffer from kidney stone, and 44% more likely to suffer from BPH compared to the older adults with no hypertension. In case of depression, older adults with depression are 2.1 times more likely to experience CRF, 1.5 times more likely to suffer from incontinence, 1.4 times more likely to suffer from kidney stone, and 1.5 times more likely to suffer from BPH compared to the older adults not having depression.
3.8. Interaction effects of diabetes and selected variables on different urinary problems
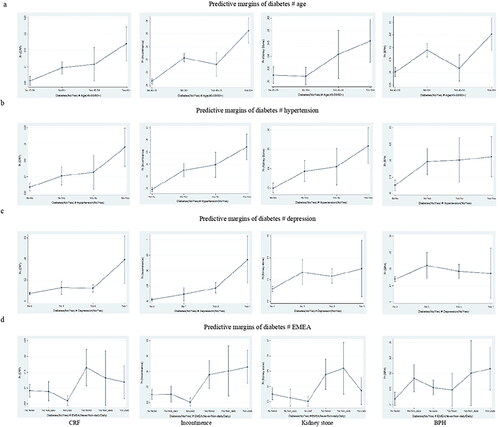
This section provides a detailed understanding of the interaction effects of the variables selected for each of the outcome variables in terms of the marginal probabilities from the logistic regression estimation (). If the interaction between diabetes and age is considered, then it is found that the chance of experiencing CRF is highest among the 60+ individuals with diabetes and the chances are quite higher to suffer from incontinence and kidney stone among the same group of individuals. Similar to kidney stone and incontinence, 60+ population with diabetes also demonstrate a significant chance to suffer from BPH. When the interactions between diabetes and depression are considered, it is found that the chances are quite high to suffer from different urinal problems such as CRD, incontinence, kidney stone, and BPH when the individual suffer from both diabetes and depression. Likewise, co-occurrence of diabetes along with hypertension among older adults increases the risk of suffering from different urinal diseases. The details of the estimated probabilities are also shown for the interactions between diabetes and the different categories of physical activity pattern. We also examined the main effects through the marginal probabilities for diabetes, age, depression, hypertension, and physical activity pattern as independent predictors of CRD, incontinence, kidney stone, and BPH. And it is found that diabetes as an independent predictor that demonstrates the highest marginal effects among all other predictors.
4. Discussion
Research on diabetes-associated urinary complications among older adults is scarce in India and so far, there is no population-based study available to highlight the public health burden of urinary complications among male older adults in India. Within a random sample of 27,661 male older adults with an average 12% prevalence of diabetes, the prevalence of CRF, incontinence, kidney stone, and BPH is estimated to be 8/1000, 30/1000, 30/1000, and 17/1000 population, respectively. It is also estimated that the average prevalence of CRF, incontinence, kidney-stone, and BPH are quite high among male older adults with diabetes compared to the national average across India.
Diabetes mellitus is associated with urological complications, which involve the endothelial and neural damage including the complications of genitourinary tract. The DM-associated urological complications are classified into three categories: lower urinary tract dysfunction, sexual dysfunction, and the UTIs [Citation18]. Persons with diabetes carry higher risk of developing bladder cystopathy as well as bladder dysfunction which involve diminished bladder filling sensation, poor contractility, infections, lithiasis, and renal damage [Citation18–20]. And LUTS are more prevalent among men with diabetes [Citation4,Citation21]. Pyelonephritis is another critical urinary complication prevalent among diabetic patients with a susceptibility to renal abscess, emphysematous cystitis, bacteremia, and sometimes with severe complications may lead to organ failure and even death [Citation18,Citation22]. The prevalence of CRF among Indian male older adults shows a distinct differential by diabetes mellitus whereby the prevalence is double among males with diabetes compared to the nondiabetic older adults. The multivariate regression estimation also confirms that diabetic older adults are 1.8 times more likely to suffer from CRF than those without diabetes. This clearly indicates that male older adults in India with diabetes are at higher risk of developing CRF and requires careful clinical interventions across India.
There are different types of UI and an understanding of the etiological risk factors through previous studies suggest that diabetes mellitus leads to the development of urge UI instead of stress UI. Macrovascular damage due to diabetes mellitus alters the detrusor muscle function and the functionality of neuronal component [Citation21,Citation23,Citation24]. According to previous studies, the condition of glycosuria due to DM causes detrusor overactivity, recurrent UTIs, and diabetic cystopathy which leads to the development of urge UI among patients [Citation5,Citation21,Citation23,Citation25]. In this study, we also investigated the diabetes-associated differential in the incontinence prevalence and the associated risk of suffering from incontinence among Indian male older adults. Diabetes mellitus is a chronic condition and nephropathy is one of the prevalent and important complications observed among other complications. The prevalence of urinary incontinence among male older adults varies across countries and with age. In India, the burden of UI among male older adults is maximum among all other types of urinary tract problems including kidney stone. In this specific study, we hypothesized that male older adults with diabetes mellitus carry higher risk of suffering from UI and the findings of the study clearly confirms that male older adults with diabetes are at more risk to suffer from UI. This study demonstrates a strong association between diabetes and UI in the study population after adjustments for confounding factors.
The burden of urinary stone disease has shown a gradual increase in the developed countries along with the incidences of metabolic syndrome and type-2 diabetes globally [Citation1,Citation26–28]. It has also been found that patients with diabetes carry higher prevalence of nephrolithiasis compared to those without diabetes [Citation29,Citation30]. Although the type of stone by its chemical composition is unknown, type-2 diabetes-associated change in the urinary pH alters the urine biochemistry which may lead to the formation of uric acid as well as calcium stones [Citation2,Citation30–32]. It is a growing concern that the prevalence of urinary stone disease has shown an increasing prevalence among older adults, and nephrolithiasis has been found to be associated with diabetes mellitus, metabolic syndrome, obesity, and hypertension [Citation33–37]. The kidney stone-associated morbidity rates are estimated to be higher among older adults [Citation38], and diabetic older adults are more susceptible to urinary complications and stone formation [Citation2]. As we explore the diabetes-associated differential in kidney stone and the associated risk, this study brings forth the evidence that male older adults with diabetes carry substantially higher burden of kidney stone than those older adults without diabetes. When adjusted for all other factors, male older adults demonstrate 1.4 times higher risk of developing kidney stone disease than those without diabetes. This clearly indicates that male older adults in India with diabetes are also at higher risk of suffering from kidney stone among other urinary complications.
Benign prostatic hyperplasia (BPH) is the enlargement of the prostrate due to proliferation of stromal and glandular elements; a commonly prevalent benign disease among male adults above age 40 and the prevalence of BPH increases rapidly with the increase of age among older adults [Citation39–41]. According to previous studies, prostate gland volume is related to the components of metabolic syndrome and noninsulin-dependent diabetes mellitus, hypertension, obesity, dyslipidemia, and hyperinsulinemia are predominant risk factors of developing BPH [Citation42,Citation43]. At the same time, clinical observations also confirm that men with diabetes and obesity show symptom of larger prostate gland compared to those without these metabolic conditions [Citation42,Citation43]. In this population-based study, we hypothesized that male older adults are at higher risk of developing BPH and the analysis of the data confirms that the prevalence of BPH is higher among male older adults with diabetes compared to those without diabetes. And, the multivariate regression analysis confirms that older adults with diabetes are 1.3 times more likely to suffer from BPH than their counterpart males without diabetes.
In this study, it has been found that diabetes is an independent and strong predictor of multiple urinary problems among male older adults in India. On the other hand, factors like age, depression, hypertension, physical activity, and BMI also significantly determine the risk in the development of different urinary complications including kidney stone.
Erectile dysfunction (ED) is common among males with diabetes and a low-dose tadalafil administration safely improves erectile dysfunction and peripheral blood flow among patients with type-2 diabetes [Citation44]. A previous cohort-based study examined the risk of developing prostate cancer among type-2 diabetes mellitus patients and found lower risk of prostate cancer among males with diabetes and metformin-users [Citation45]. The association between ED, hypogonadism, cardiovascular disease, and type 2 diabetes has been much documented, yet the evidence from long-term data are scarce and in this context a study investigated the effects of long-term testosterone therapy (TTh) with testosterone undecanoate in men with hypogonadism and ED [Citation46]. The study found that long-term TTh with testosterone undecanoate alleviates ED, improves cardiometabolic risk factors, and reduces prostate cancer [Citation46]. A different study conducted in China, compared the clinical and physiological parameters among three groups, impaired fasting glucose (IFG), high-risk type-2 diabetes mellitus (HR-T2DM), and normal fasting blood glucose (FBG) groups of BPH patients, and the study suggested that abnormal FBG plays an important role in BPH [Citation47]. BPH is prevalent among ageing men causing LUTS [Citation48] and other than ageing, modifiable factors such as metabolic syndrome contributes to the development of BPH and/or LUTS [Citation49]. A systematic review study also brings the epidemiological evidences on the linkages between metabolic syndrome and LUTS secondary to BPH [Citation50]. Another study reports a positive correlation between visceral adiposity index (VAI) and prostate volume among nondiabetic patients [Citation51].
In India, the prevalence of diabetes has grown steadily during the last decades and India is home to the second largest number of diabetes people in the world [Citation52]. As per the estimates by International Diabetes Federation (IDF)-2017, there are 72.9 million people with diabetes, which is estimated to rise up to 134.3 million by 2045 with a sharp increase in the prevalence in the urban areas, especially in the metropolitan cities [Citation52]. Parallel to the significant epidemiological burden of type-2 diabetes that India carries, diabetes control in India has also failed to maintain the global standards of mean HbA1c ≤ 7% and almost half of the people with diabetes remain undiagnosed across India [Citation53,Citation54]. The high prevalence of diabetes and diabetes-associated complications among patients in India possesses a public health burden and a threat in terms of the disease management due to vast geography, population count, and scarcity of diabetologists [Citation55,Citation56]. According to American College of Endocrinology (ACE) and American Association of Clinical Endocrinologists (AACE), life style intervention is the recommended and preferred treatment regimen for prediabetes and newly diagnosed subjects up to three months [Citation57,Citation58]; whereby, a study conducted in India found that 75% of the study participants were not briefed about lifestyle modification by their treating doctors and 55% of them were prescribed to start antidiabetic medicines on the same day of the diagnosis [Citation56]. The study also reports that 39% of the diabetic patients were treated by a doctor, not professionally expert to treat diabetes [Citation56]. Diabetes is a chronic disease, involves associated complications and thus diabetes management becomes costly among patients [Citation56]. On the other hand, the disease management after the onset of the disease requires regular check-ups and blood glucose monitoring, however, according to a previous study it has been found that the purchasing of glucometer among diabetic patients in India is almost negligible mainly due to two basic reasons – either the patients find it expensive or difficult to use a glucometer to self-monitor blood glucose level [Citation56,Citation59].
Type-2 diabetes is associated with a range of lower urinary tract complications to upper urinary tract complications. Also, nephropathy, neuropathy, and retinopathy are the different clinical challenges of diabetic complications and irregular bladder functions are also common among patients with diabetes; thus, prevention and treatment of UTIs is one of the primary goals to manage diabetic urinary complications among patients [Citation60]. Holistically, the management strategies are classified into three broad categories – behavioral, pharmacological, and surgical [Citation60]. The behavioral modalities primarily focus on prediabetic and diabetic subjects as the first-stage treatment with lifestyle modification, weight reduction, diet change, amount and timing of fluid intake, and pelvic and bladder muscle training [Citation61–63]. And, weight reduction has been found to be substantially associated with lowering the symptoms of UI among diabetic subjects [Citation63]. Also, cessation of alcohol consumption and smoking, increased fiber intake and regular bowel habits, maintaining blood pressure, and blood glucose are important components to prevent bladder dysfunctions and UTIs among the diabetic subjects [Citation60,Citation64]. As diabetes is associated with the development of multiple urinary problems among males in the older ages there is a public health need of reducing the burden of diabetes associated risk of urinary complications among older adults. In this regard, glycemic control plays a crucial role in reducing the risk of diabetes-associated urinary complications among older adults.
To understand the actual prevalence of diabetes-associated prevalence of urinary complications, there is no source of data available for India except the Chennai Urban Rural Epidemiology Study (CURES 45) that provided the prevalence estimate and the risk factors of diabetic nephropathy among South Indian Population. Onset of the disease, duration of the disease and medication history play a crucial role to identify the linkages between diabetes and the associated complications. In this regard, LASI is the first ever survey to collect the essential information on urinary problems, diabetes along with the socio-economic and demographic information of the older adults aged 45 and above. And this study is the first ever population-based study to shed light on the incidences of multiple lower and upper urinary tract problems among older adults in India and the risk of developing different urinary tract problems among individuals with type-2 diabetes. In India, the prevalence of diabetes in the general population is showing a steady increase over time while management of this disease and the associated urinary and other complications is a public health concern. In terms of providing appropriate health care services, there is a dearth of trained medical professionals, endocrine specialists to treat diabetes and diabetes-associated microvascular and macrovascular complications. If we consider the epidemiological burden of diabetes and its management across India, there are very few diabetes specialists and the doctor–patient ratio is not adequate to cope up with the situation [Citation55,Citation56]. Although diabetes care is complex and glycemic control is very important, yet monitoring of serum urea, urine microalbumin, checking glomerular filtration rate, examination of the prostrate, and bladder functions by experts will help to identify the potential diabetic urinary problems including kidney disease in time. In India, the high prevalence of diabetic complications is attributable to delay in diagnosis, cost of medicines – the cost of insulin in particular – other illnesses, inadequate health care facility [Citation65] which is likely to pose an additional threat and public health burden managing the diabetes-associated complications, especially urinary complications and kidney disease.
5. Conclusions
This study clearly brings up the evidence that the prevalence of chronic renal failure, UI, BPH and kidney stone are significantly higher among older adults with diabetes compared to those without diabetes. Multivariate analysis within a cross-sectional framework also confirms that diabetes mellitus is a predominantly significant and an independent predictor of each of the urinary complications, which raises the public health concern in terms of the management of the urinary complications among older adults in India. Given the existing burden of diabetic urinary complications among male older adults, health policy makers must focus on this potential public health issue and help build a robust health care system prioritizing diabetes management and facilitation of the diagnostic measures and treatment against urinary complications. Diabetes mellitus is preventable and requires life style modification in terms of physical activity, cessation from alcohol consumption and smoking, appropriate diet, and body weight management which can play a major role in diabetes management and help to reduce the risk of developing diabetic urinary complications. Although previous studies provide the estimate and risk factors of urinary complications; yet family medicine should prioritize the research on the epidemiology, etiology and the risk factors of renal failure, incontinence [Citation24], BPH, and kidney stone among diabetic subjects and among subjects with hypertension and other comorbidities. On the other hand, individuals having both diabetes and urinary complications require careful medical attention to achieve optimum glycemic control and monitoring against diabetic complications among them [Citation66]. Regular monitoring of microalbuminuria and GFR are also critical to avoid urinary complications among diabetic subjects. And a health care system involving diabetologists, nephrologists, dietician, diabetes educator, and experts experienced in diabetes complications can ensure appropriate treatment and care to the patients reducing the progression of diabetes and the associated urinary complications among patients [Citation66].
Ethical approval
This study is based on a de-identified secondarily available data and requires no further ethical approval from any institutional review board (IRB) to conduct the study. Informed consent is not applicable.
Acknowledgments
Authors cordially acknowledge the International Institute for Population Sciences (IIPS), Mumbai for providing the LASI Wave 1 dataset to conduct the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data is available subject to a data request. To access the data, request can be put through the link- https://www.iipsindia.ac.in/content/LASI-data.
Additional information
Funding
References
- Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003;63(5):1817–1823.
- Assimos DG. Diabetes mellitus and kidney stone formation. Rev Urol. 2006;8(1):44.
- Wang Z, do Carmo JM, Aberdein N, et al. Synergistic interaction of hypertension and diabetes in promoting kidney injury and the role of endoplasmic reticulum stress. Hypertension. 2017;69(5):879–891.
- Van Den Eeden SK, Ferrara A, Shan J, et al. Impact of type 2 diabetes on lower urinary tract symptoms in men: a cohort study. BMC Urol. 2013;13(1):1–7.
- Smith DB. Urinary incontinence and diabetes: a review. J Wound Ostomy Continence Nurs. 2006;33(6):619–623.
- Gundamaraju R, Vemuri R. Pathophysiology of greedy colon and diabetes: role of atropine in worsening of diabetes. Euroasian J Hepatogastroenterol. 2014;4(1):51–54.
- Centers for Disease Control and Prevention. National Diabetes Statistics Report website. https://www.cdc.gov/diabetes/data/statistics-report/index.html.
- Scott RA, Langenberg C, Sharp SJ, InterAct Consortium, et al. The link between family history and risk of type 2 diabetes is not explained by anthropometric, lifestyle or genetic risk factors: the EPIC-InterAct study. Diabetologia. 2013;56:60–69.
- Rowe TA, Juthani-Mehta M. Urinary tract infection in older adults. Aging Health. 2013;9(5):519–528.
- Thomas MC, Brownlee M, Susztak K, et al. Diabetic kidney disease. Nat Rev Dis Primers. 2015;1(1):1–20.
- Fünfstück R, Nicolle LE, Hanefeld M, et al. Urinary tract infection in patients with diabetes mellitus. Clin Nephrol. 2012;77(1):40–48.
- Sewify M, Nair S, Warsame S, et al. Prevalence of urinary tract infection and antimicrobial susceptibility among diabetic patients with controlled and uncontrolled glycemia in Kuwait. J Diabet Res. 2016;2016:1–7.
- Zasloff M. Why are diabetics prone to kidney infections? J Clin Invest. 2018;128(12):5213–5215.
- Triozzi JL, Gregg LP, Virani SS, et al. Management of type 2 diabetes in chronic kidney disease. BMJ Open Diab Res Care. 2021;9(1):e002300.
- Urinary tract infections (UTIs). Available from: https://www.nhs.uk/conditions/urinary-tract-infections-utis/.
- Catheter-associated urinary tract infections (CAUTI). Available from: https://www.cdc.gov/hai/ca_uti/uti.html.
- Wang Y, Jing Z, Ding L, et al. Socioeconomic inequity in inpatient service utilization based on need among internal migrants: evidence from 2014 national cross-sectional survey in China. BMC Health Serv. Res. 2020;20(1):1–11.
- Arrellano-Valdez F, Urrutia-Osorio M, Arroyo C, et al. A comprehensive review of urologic complications in patients with diabetes. Springerplus. 2014;3(1):1–8.
- Deli G, Bosnyak E, Pusch G, et al. Diabetic neuropathies: diagnosis and management. Neuroendocrinology. 2013;98(4):267–280.
- Daneshgari F, Liu G, Birder L, et al. Diabetic bladder dysfunction: current translational knowledge. J Urol. 2009;182(6 Suppl):S18–S26.
- Kebapcı N, Yenilmez A, Efe B, et al. Bladder dysfunction in type 2 diabetic patients. Neurourol Urodyn. 2007;26(6):814–819.
- Stapleton A. Urinary tract infections in patients with diabetes. Am J Med. 2002;113(1):80–84.
- Hill SR, Fayyad AM, Jones GR. Diabetes mellitus and female lower urinary tract symptoms: a review. Neurourol Urodyn. 2008;27(5):362–367.
- Izci Y, Topsever P, Filiz TM, et al. The association between diabetes mellitus and urinary incontinence in adult women. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(8):947–952.
- Helen Ebbesen M, Hannestad YS, Midthjell K, et al. Diabetes and urinary incontinence–prevalence data from Norway. Acta Obstet Gynecol Scand. 2007;86(10):1256–1262.
- Trinchieri A, Coppi F, Montanari E, et al. Increase in the prevalence of symptomatic upper urinary tract stones during the last ten years. Eur Urol. 2000;37(1):23–25.
- Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third national health and nutrition examination survey. JAMA. 2002;287(3):356–359.
- Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053.
- Taylor EN, Stampfer MJ, Curhan GC. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int. 2005;68(3):1230–1235.
- Meydan N, Barutca S, Caliskan S, et al. Urinary stone disease in diabetes mellitus. Scand J Urol Nephrol. 2003;37(1):64–70.
- Daudon M, Traxer O, Conort P, et al. Type 2 diabetes increases the risk for uric acid stones. J Am Soc Nephrol. 2006;17(7):2026–2033.
- Nerli R, Jali M, Guntaka AK, et al. Type 2 diabetes mellitus and renal stones. Adv Biomed Res. 2015;4:180. doi: 10.4103/2277-9175.164012.
- Sakhaee K, Adams-Huet B, Moe OW, et al. Pathophysiologic basis for normouricosuric uric acid nephrolithiasis. Kidney Int. 2002;62(3):971–979.
- Daudon M, Jungers P. Diabetes and nephrolithiasis. Curr Diab Rep. 2007;7(6):443–448.
- Obligado SH, Goldfarb DS. The association of nephrolithiasis with hypertension and obesity: a review. Am J Hypertens. 2008;21(3):257–264.
- Cupisti A, D'Alessandro C, Samoni S, et al. Nephrolithiasis and hypertension: possible links and clinical implications. J Nephrol. 2014;27(5):477–482.
- Rendina D, De Filippo G, D’Elia L, et al. Metabolic syndrome and nephrolithiasis: a systematic review and meta-analysis of the scientific evidence. J Nephrol. 2014;27(4):371–376.
- Curhan GC. Epidemiology of stone disease. Urol Clin North Am. 2007;34(3):287–293.
- Barry MJ. Epidemiology and natural history of benign prostatic hyperplasia. Urol Clin North Am. 1990;17(3):495–507.
- Hammarsten J, Högstedt B. Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol. 2001;39(2):151–158.
- Berry SJ, Coffey DS, Walsh PC, et al. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132(3):474–479.
- Hammarsten J, Högstedt B, Holthuis N, et al. Components of the metabolic syndrome—risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 1998;1(3):157–162.
- Hammarsten J, Högstedt B. BENKT: clinical, anthropometric, metabolic and insulin profile of men with fast annual growth rates of benign prostatic hyperplasia. Blood Press. 1999;8(1):29–36.
- Lee JS, Hong SH, Sun HY, et al. (2023). The efficacy and safety of tadalafil in the management of erectile dysfunction with diabetes and blood circulation issues. Aging Male. 2023;26(1):2176484.
- Kincius M, Patasius A, Linkeviciute-Ulinskiene D, et al. Reduced risk of prostate cancer in a cohort of Lithuanian diabetes mellitus patients. Aging Male. 2020;23(5):1333–1338.
- Saad F, Caliber M, Doros G, et al. Long-term treatment with testosterone undecanoate injections in men with hypogonadism alleviates erectile dysfunction and reduces risk of major adverse cardiovascular events, prostate cancer, and mortality. Aging Male. 2020;23(1):81–92.
- Zhao MJ, Huang Q, Wang XH, et al. Comparing clinical parameters of abnormal and normal fasting blood glucose in benign prostatic hyperplasia patients. Aging Male. 2020;23(5):655–662.
- Rosen RC, Wei JT, Althof SE, et al. Urology PSSCJ: association of sexual dysfunction with lower urinary tract symptoms of BPH and BPH medical therapies: results from the BPH registry. Urology. 2009;73(3):562–566.
- Calogero AE, Burgio G, Condorelli RA, et al. Epidemiology and risk factors of lower urinary tract symptoms/benign prostatic hyperplasia and erectile dysfunction. Aging Male. 2019;22(1):12–19.
- Russo GI, Castelli T, Urzi D, et al. Connections between lower urinary tract symptoms related to benign prostatic enlargement and metabolic syndrome with its components: a systematic review and meta-analysis. Aging Male. 2015;18(4):207–216.
- Besiroglu H, Ozbek E, Dursun M, et al. Visceral adiposity index is associated with benign prostatic enlargement in non-diabetic patients: a cross-sectional study. Aging Male. 2018;21(1):40–47.
- International Diabetes Federation. IDF diabetes atlas. 8th ed. Brussels, Belgium: International Diabetes Federation; 2017. p. 905–911.
- Joshi SR. Diabetes care in India. Ann Glob Health. 2015;81(6):830–838.
- American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement_1):S73–S84.
- Anjana RM, Deepa M, Pradeepa R, et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR–INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5(8):585–596.
- Dixit JV, Kulkarni RS, Badgujar SY. Diabetes care in India: a descriptive study. Indian J Endocrinol Metab. 2021;25(4):342–347.
- Nathan DM, Davidson MB, DeFronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30(3):753–759.
- Garber AJ, Abrahamson MJ, Barzilay JI, et al. AACE comprehensive diabetes management algorithm 2013. Endocr Pract. 2013;19(2):1–48.
- Tenderich A. Use of blood glucose meters among people with type 2 diabetes: patient perspectives. I Am Diabetes Assoc. 2013;26(2):67–70.
- Golbidi S, Laher I. Bladder dysfunction in diabetes mellitus. Front Pharmacol. 2010;1:136.
- Knowler WC, Barrett-Connor E, Fowler SE, Group DPPR, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Eng J Med. 2002;346(6):393–403.
- Subak L, Johnson C, Whitcomb E, et al. Does weight loss improve incontinence in moderately obese women? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(1):40–43.
- Brown JS, Wing R, Barrett-Connor E, et al. Lifestyle intervention is associated with lower prevalence of urinary incontinence: the Diabetes Prevention Program. Diabetes Care. 2006;29(2):385–390.
- Ho MH, Yip S, Bhatia NN. Lower urinary tract dysfunctions in women with diabetes mellitus. Curr Opin Obstet Gynecol. 2007;19(5):469–473.
- Pradeepa R, Mohan V. Epidemiology of type 2 diabetes in India. Indian J Ophthalmol. 2021;69(11):2932–2938.
- Hahr AJ, Molitch ME. Management of diabetes mellitus in patients with chronic kidney disease. Clin Diabetes Endocrinol. 2015;1(1):2.