Abstract
In India, traditional social practices around marriage, such as non-involvement of prospective brides in choice of partner and timing of marriage, child/early marriage, dowry and purdah, compromise women’s agency at the time of marriage and may also affect contraceptive practices in marriage. This paper examines the associations between traditional marital practices and contraceptive behaviours, including women’s control over contraceptive decision-making, couples’ communication about contraception, and ever use of contraceptives, among married women aged 18–29 years (N = 1,200) and their husbands in rural Maharashtra, India. Multivariable logistic regression was used to examine the association between these marginalising social practices and family planning behavioural outcomes, adjusting for demographic and parity confounders. Wives who were the primary decision-makers on who to marry had higher odds of ever having communicated with their husband on pregnancy prevention (AOR 1.76, 95% CI 1.16-2.68), and ever using modern contraceptives (AOR 2.19, 95% CI 1.52-3.16). Wives who were the primary decision-makers on when to marry also had higher odds of ever having used modern contraceptives (AOR 1.86, 95% CI 1.21-2.93). Women’s involvement in marital choice may facilitate couples’ engagement related to family planning, possibly via the establishment of better communication between partners.
Introduction
Gender-based social practices that marginalise women and girls continue to be prevalent across the world. It is estimated that 38% of girls in Sub-Saharan Africa and 30% of girls in South Asia marry before the age of 18 (UNICEF Citation2019). The estimated rate of child marriage in India is 27% (as reported by respondents aged 20-24 years at the time of the survey) (IIPS and ICF Citation2017), and women often have limited marital decision-making control (on deciding who and at what age to marry). Early and child marriage leads to poor reproductive health, education and economic outcomes (Raj et al. Citation2009; Raj, Saggurti, Winter, et al. Citation2010; Raj, McDougal, et al. Citation2014; Yount, Crandall, and Cheong Citation2018). In these contexts, dowry (a method of payment through money, property, or gifts made by the bride’s family to the groom and his family) is longitudinally associated with women’s poor self-rated general health (Stroope, Kroeger, and Fan Citation2021).
Similarly, gender as a performance indicator in the form of veiling (purdah among Muslims or ghunghat among Hindus) also may marginalise women and act as a barrier to healthcare utilisation (Vissandjee, Barlow, and Fraser Citation1997; Desai and Andrist Citation2010). These marginalising social practices are rooted in gender-based power structures of patrilineal (male-line descent) and patrilocal (couple residing with the husband’s parents) norms, whereby in-laws have a strong influence over the couple’s health and fertility behaviour (Silverman et al. Citation2019; Anukriti et al. Citation2020; Kumar, Bordone, and Muttarak Citation2016; Char, Saavala, and Kulmala Citation2010). There is widespread and inter-generational transfer of social norms with respect to whom and when to marry, as well as contraception use, fertility desires and the acceptability of domestic violence (Raj, Ghule, et al. Citation2014; Barber Citation2001).
This ongoing pervasiveness of traditional marital practices can reinforce traditional expectations of early fertility in marriage due to pro-natal social norms, and the non-use of contraception until the desired number and sex of children are achieved. These practices are tied to marriage mainly driven by parents, in-laws and the extended family. These can create an environment where women have lower status or agency at marriage, leading to lower decision-making control (Raj, Ghule, et al. Citation2014; Jeyaseelan et al. Citation2015; Desai and Andrist Citation2010; Crandall et al. Citation2016). Evidence from interventions on couple communication and joint decision-making have shown improved contraceptive outcomes in India but have not documented the role of agency in this process (Raj et al. Citation2016; Pathfinder Citation2013; Subramanian, Simon, and Daniel Citation2018).
Although we know how lack of agency as sustained within marriage affects contraceptive use (Prata et al. Citation2017; Raj, Saggurti, Lawrence, et al. Citation2010; Santhya et al. Citation2010), there is still a lack of understanding of how agency at the time of marriage affects contraceptive use. Qualitative data reveals that women in India have low decision-making autonomy, especially over marital choice (McDougal et al. Citation2018), and that lack of agency in marriage (e.g. decision-making control) can act as a barrier to women’s use of family planning (Ghule et al. Citation2015). However, a further quantitative assessment is needed to explore how socially marginalising practices measuring agency in relation to marriage (marital choice, dowry and purdah) affect women’s involvement in contraceptive decision-making, contraceptive communication with their husbands, and contraceptive use. In this study, we set out to examine the influence of women’s agency at the time of marriage on family planning behaviour later in their marriage in an overall gender-unfriendly environment.
This paper aimed to study marital agency as measured by marginalising gender-based social practices around marriage, including women’s involvement with marital choice, early marriage, purdah and dowry, and whether these were associated with women’s involvement in contraceptive decision-making, communication about contraception in marriage, and whether they have ever used modern contraceptive methods. We hypothesised that traditional marital practices would be associated with lower odds of female decision-making control in marriage, lower odds of marital contraceptive communication, and lower odds of ever using contraception. The findings have implications for research to consider traditional marital practices as risk factors and for programmes to create awareness of the harmful health effects related to them for effective family planning behaviours that avert unwanted and unintended pregnancy.
Methods
Sample and data collection
We used a cross-sectional baseline sample from 1,201 couples enrolled in the CHARM2 [Counseling Husbands and wives to Achieve Reproductive Health and Marital Equity] study, a two-arm cluster randomised controlled trial (RCT) evaluating a gender-synchronised, gender-transformative family planning intervention in rural Maharashtra, India. The study was conducted in Junnar Taluka in the Pune District of Maharashtra, which is comprised of 183 villages (pop. 399,000) and 12 primary health centres (PHCs).
CHARM2 was implemented in 5 PHCs from which we selected 20 sub-centres (SCs) that functioned as the geographic clusters (areas served by the SC) randomised to the CHARM2 intervention or control condition. The CHARM2 intervention was a programme aiming to increase knowledge about and uptake of contraceptives, prevent unintended pregnancy, and decrease intimate partner violence among young married couples. Study staff recruited couples from 60 randomly selected households in each of the 20 geographic clusters. We identified all clusters and randomised them prior to study recruitment. We designed the sampling to yield a sample size of 1200 participants, based on a power calculation designed to evaluate CHARM2 impacts. Couples who were not currently married or cohabiting, or who reported sterilisation or infertility, were not eligible to participate in the study.
Trained gender-matched interviewers collected self-report data using electronic tablets between September 2018 and June 2019. The study included wives aged 18 to 29 years and their husbands. Ethical guidelines for domestic violence research from the World Health Organization were followed during data collection given the high rates of spousal violence in India (WHO Citation2001). Other protections included survey implementation in a private and secure area, only asking women about violence experiences, and the provision of information on domestic violence services regardless of participants’ responses to violence questions. We also provided all participants with information about free family planning services in the local public health system.
A detailed protocol for CHARM2 is published elsewhere (Dixit et al. Citation2019). The current analytic sample of 1,200 couples further excluded one couple with missing information on the intimate partner violence independent variable detailed below. The Institutional Review Boards of the University of California San Diego, the ICMR-National Institute for Research in Reproductive Health in India, and the Population Council approved the protocol, and all participants gave written informed consent before they participated in the study.
Measures
The dependent variables in this study were: a) women’s involvement in contraceptive decision-making developed from the survey item, “Would you say that using or not using contraception is mainly your decision, your husband’s decision, joint decision by both, your mother, mother in law, elderly head of household, your sibling, your husband’s sibling or someone else?”, categorised with responses of Yes (woman’s or joint decision with husband) or No (husband’s or other’s decision); and b) marital contraceptive communication, derived from the survey item, “Have you and your husband ever discussed what to use or do to prevent or stop a pregnancy?”, with responses of Yes or No; and c) contraceptive use ever, with responses of Yes or No. Modern contraceptive use ever was established from the survey items, “Have you ever used any methods to delay or avoid pregnancy?”, with response options Yes or No, and “Which methods have you ever used?”. Methods including pills, IUD or Copper-T, PPIUD, injectables, male condoms, female condoms, the emergency contraceptive pill and Lactational Amenorrhoea Method (LAM) were considered to be modern methods of contraception (World Health Organization Reproductive Health Citation2007). We focused on women’s perspectives in the selection of outcome variables, since we aimed to understand her agency based on the way her marriage started.
Independent variables were the traditional marginalising marital practices, used as a proxy for measuring agency at marriage. These included: women’s involvement in marital choice of mate, developed using the survey item, “Who was the primary person to decide whom you married?” with response options “Self, Mother, Father, Brother, Sister, Aunt, Uncle, Grandmother, Grandfather, Community leader, Religious leader, Other (specify)”; and women’s involvement in marital choice on marital timing, developed using the survey item, “Who was the primary person to decide when you should get married?” with response options “Self, Mother, Father, Brother, Sister, Aunt, Uncle, Grandmother, Grandfather, Community leader, Religious leader, Other (specify)”. Both variables were categorised into dichotomous variables of Self and Other as the primary decision-maker. Child marriage (wife <18 years) was ascertained from the survey item, “How old were you when you (first) got married?” categorised as Yes if married before age 18, and No if married at 18 or later. The practice of purdah variable used the survey item “Do you practice purdah?” with response options Yes, No. The practice of dowry variables used the survey item “When you got married, did your family give any nuptial gifts or money (dowry) to the boy's family?” with response options Yes, No.
There is a lack of studies using validated measures to assess the association between indicators of traditional marital practices and contraceptive use. The survey items we used were developed by the US and India-based CHARM2 investigator teams with guidance from their prior qualitative research in the region. They were tested in pilot interviews for the survey with 20 couples from within the target population.
Additional variables selected a priori as potential confounders, based on previous literature and the authors’ expertise, were wife’s age (continuous variable), wife’s education (None or Primary, Secondary or Higher), husband’s education (None or Primary, Secondary or Higher), caste (General, Scheduled Caste/Scheduled Tribe/Other Backward Castes), parity (0, 1, 2-5), any living son (Yes, No), below poverty line status (Yes, No), wife’s knowledge of contraceptive methods (Number of methods, Continuous). We also adjusted for the experience of intimate partner violence (physical and/or sexual) categorised as Yes, No. Considering dowry-related outcomes of domestic violence and dowry deaths (Kaur and Byard Citation2020; Babu and Babu Citation2011; Banerjee Citation2014), intimate partner violence may play a large role in contraceptive use.
Analysis
Descriptive frequencies and proportions were calculated for the marital practice variables with outcomes of women’s involvement in contraceptive decision-making, couples having ever discussed preventing pregnancy, and having ever used modern contraceptive methods. Multivariable logistic regression was used to assess whether traditional marital practices were associated with women’s involvement in contraceptive decision-making, having ever discussed preventing pregnancy, and having ever used modern contraception. Models were adjusted for potential confounders listed in the measures section. We did not find collinearity between confounders, with a Variance Inflation Factor (VIF) cut-off of 4 (Menard Citation2002).
We also considered exploratory analysis to construct a marital agency scale using the marginalising social practices items but found that although there are significant descriptive associations (See online Appendix Table A1) and correlations (See online Appendix Table A2) between these variables, a scale could not be constructed because they do not hang together when tested for internal consistency (Cronbach’s α = 0.39).
A sensitivity analysis was also conducted to assess the association of dowry and purdah with women’s involvement in contraceptive decision-making, ever discussing pregnancy prevention with their husband, and ever using contraceptives, first adjusting only for religion, since it was expected that these practices may differ by religion, and second adjusting for all main model potential confounders but using religion instead of caste, due to the expected association of these practices with religion and collinearity between caste and religion variables (See online Appendix Table A3).
Finally, we carried out a Poisson regression with robust variance estimation for the outcome of ever using modern contraception. This limits any inflation of effect sizes which may be seen in logistic regression since lifetime history of use of modern contraceptives is not rare in this sample (Zou Citation2004; Zou and Donner Citation2013) (See online Appendix Table A4). All analyses were performed using STATA version 15.0 (StataCorp 2017).
Results
Among wives, 15.6% reported being the primary decision-maker on who to marry, and 9.4% reported that they had been the primary decision-maker on when to marry. When asked about their age at marriage, 17.8% of wives reported that they were married before the age of 18. Purdah was practised by 9.7% of wives, and dowry was reported by 12.3% of wives (See ).
Modern contraception was used at some time by 58.1% of the couples, as reported by wives, while current (past 3 months) use of contraception was reported by 37.9% of wives. Contraceptive communication with husbands was reported by 72.9% of wives. The majority of wives (82.2%) reported that they were involved in contraceptive decision-making, jointly with husbands or alone (; see for prevalence of traditional marital practices by outcomes).
Figure 1. Prevalence of traditional marital practices and women’s involvement in contraceptive decision-making among married couples enrolled in CHARM2 in rural Maharashtra, India (N = 1,200).
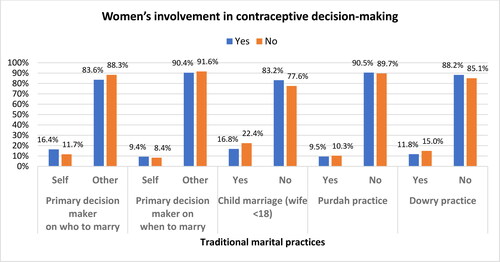
Figure 2. Prevalence of traditional marital practices and having ever discussed pregnancy prevention with husband among married couples enrolled in CHARM2 in rural Maharashtra, India (N = 1,200).
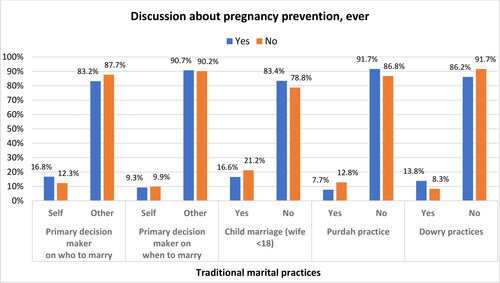
Figure 3. Prevalence of traditional marital practices and having ever used modern contraception among married couples enrolled in CHARM2 in rural Maharashtra, India (N = 1,200).
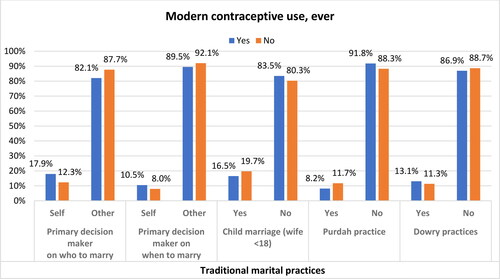
Table 1. Traditional marital practices and sociodemographic characteristics by women’s involvement in contraceptive decision-making, ever discussing pregnancy prevention, and ever using modern contraceptive methods, among married couples enrolled in CHARM2 in rural Maharashtra, India (N = 1,200).
In multivariable analysis, traditional marital practices did not show any significant association with women’s involvement in contraceptive decision-making (). After adjusting for potential confounders, wives who were primary decision-makers about who to marry had higher odds of ever discussing pregnancy prevention with their husbands (AOR 1.76, 95% CI 1.16-2.68). Dowry practices were associated with having ever discussed pregnancy prevention with their husbands in the unadjusted model (OR 1.77, 95% CI 1.14-2.74), but significance was not sustained in the adjusted model (AOR 1.57, 95% CI 0.97-2.53). Purdah was also associated with having ever discussed pregnancy prevention with their husbands in the unadjusted model; this association was maintained as a trend in multivariable analysis, but significance was not sustained (OR 0.60, 95% CI 0.40-0.89, AOR 0.65, 95% CI 0.41-1.02) ().
Table 2. Unadjusted and adjusted logistic regression between traditional marital practices with women’s report of women’s involvement in contraceptive decision-making, among married couples enrolled in CHARM2 in rural Maharashtra, India (N = 1,200).
Table 3. Unadjusted and adjusted logistic regression between traditional marital practices and having ever discussed preventing pregnancy with husband among married couples enrolled in CHARM2 in rural Maharashtra, India (N = 1,200).
The association between traditional marital practices with ever using modern contraception showed that wives who were the primary decision-makers on who to marry had higher odds of ever using modern contraception in the unadjusted analysis (OR 1.55, 95% CI 1.12-2.16), and this association was sustained when adjusted for other potential confounders (AOR 2.19, 95% CI 1.52-3.16). Wives who were the primary decision-makers about when to marry also had higher odds of ever using modern contraception when adjusted for confounders (AOR 1.86 95% CI 1.21-2.93) (). Purdah practice showed an association in the unadjusted analysis (OR 0.67 95% CI 0.46-0.98), but this association remained as a trend that did not meet statistical significance in the adjusted analysis. None of the other socially marginalising practices, including primary decision-making about when to marry, child marriage and dowry, showed a significant association with ever using modern contraceptives.
Table 4. Unadjusted and adjusted logistic regression between traditional marital practices and having ever used modern contraceptive methods, among married couples enrolled in CHARM2 in rural Maharashtra, India (N = 1,200).
Since the purdah practice was expected to be more commonly followed among those who follow the Muslim religion, and dowry among those who follow the Hindu religion, we conducted a sensitivity analysis to assess the association of these marginalising social practices with women’s involvement in contraceptive decision-making, ever discussing pregnancy prevention with the husband, and ever using modern contraceptives. The first regression adjusted for religion only, and the second included religion instead of caste, along with other primary analysis confounders. The Poisson regression analysis for the outcome ‘ever modern contraceptive use’ showed an estimate similar to the main analysis (see online Appendix Tables A3 and A4).
Discussion
Our findings show that only about one in six women reported being the primary decision-maker on who to marry. Even fewer, about one in thirteen, were the primary decision-makers on when to marry, and when asked about their actual age at marriage, over one in six women were married as children, before the age of 18. Other marginalised practices included purdah, practised by one in twelve women and dowry, practiced by one in thirteen women.
Wives who were the primary decision-maker on who to marry had higher odds of ever discussing pregnancy prevention with their husband and higher odds of ever using modern contraception. These findings indicate that when women are the primary decision-makers on who to marry, this facilitates discussion between the couple on their fertility desires, such as the prevention of any unwanted pregnancy and using a modern method of contraception. Wives who were the primary decision-makers on when to marry also had higher odds of ever using modern contraception. Thus, this lack of marital choice on who and when to marry may be harmful to women’s fertility-related agency in the long term and may need to be considered for the prevention of unintended pregnancy among couples in rural India.
The value of focusing on social norms concerning marital choice has been demonstrated in previous literature (Shakya et al. Citation2020; Raj, Ghule, et al. Citation2014), and there have been effective interventions that aim to delay marriage and increase contraceptive access in India (Pathfinder Citation2013). Building on this, our findings suggest that these interventions need to be expanded to consider women’s agency at the time of marriage and, beyond timing, to include choice of partner to influence couples’ communication around contraception. Qualitative work has also emphasised the need to understand the nuanced marital decision-making process to better equip programmes supporting women’s health (McDougal et al. Citation2018).
Although the choice of who to marry was associated with ever discussing pregnancy prevention with the husband, we do not know the nature of this discussion, so further research is needed to clarify the content of couple communication. This is to avoid any assumptions about such communications being a respectful and joint discussion for shared decision-making, specifically about the actual use of contraception. This may be evident in the lack of association of marital choice with women’s involvement in contraceptive decision-making. None of the traditional marital practices assessed here were associated with women’s involvement in contraceptive decision-making.
These findings should be viewed in the light of the rural Maharashtra context with respect to marriage formation, where marriage is usually arranged between two families by the elders of the family and community. The involvement or explicit approval of the bride and groom in that decision may vary. Families may take pride in forming marriages in a traditional manner as a way to preserving their culture and resisting modernisation or Westernisation. The local context further highlights the importance of understanding and working with local communities when undertaking this type of research to ensure an understanding of local social norms.
Our study shed light on the impact of marital agency, but it did not show some of the associations we expected. For example, child marriage has previously been established as an important predictor of contraceptive non-use and other poor reproductive health outcomes (Raj et al. Citation2009; Raj and Boehmer Citation2013). The association estimates for dowry and purdah in analyses with couple communication had confidence intervals close to 1, implying that there may not be a meaningful difference between those who report them and those who do not. These practices are a form of performance of gender and may not be directly influential on family planning behaviours. Another reason for this lack of some associations may be small sample size, affecting the power of the analysis. For example, in our sample, only 22 women reported purdah and 32 reported dowry among those who reported not being involved in contraceptive decision-making.
Limitations
The cross-sectional nature of the data precludes the assumption of causality, so findings must be interpreted with caution. Our findings are also specific to this sample and not nationally representative or readily generalisable. Study variables were self-reported, so are subject to recall and social desirability bias; for example, there may be underreporting of dowry incidents and child marriage because these practices are illegal in India. Overreporting of contraception use may also have occurred because participants interested in contraception may be self-selecting. For this reason, we also conducted a Poisson regression analysis to inspect any inflation of reported estimates.
Ethical challenges to research have been recognised in similar study contexts (Stenson et al. Citation2010), where consent can be viewed as a community decision (Bhutta Citation2004; Geller et al. Citation2004). There can be a lack of privacy in a multi-generation joint-family home. There can also be a power imbalance during consent due to participants’ socio-demographic background differing from that of interviewers (Andanda Citation2009; Mystakidou et al. Citation2009). Thus, innovative efforts to improve quality in such research contexts continue to be required.
Furthermore, there may be a selection bias for outcomes such as contraceptive use because sterilised couples are excluded from the CHARM2 intervention. Women in India tend not to use contraceptives until the desired parity and sex composition of children has been achieved, after which a majority opt for permanent contraceptives like female sterilisation (IIPS and Macro International Citation2007; IIPS and ICF 2017). Because sterilised women were not included in this study, we were not able to assess our research questions among those women who may be susceptible to fertility pressures and thus did not use contraceptives until they reached desired family size and opted for sterilisation. Evidence also shows that fertility pressures may influence contraceptive use differently based on type of contraceptive, such as higher use of covert and discreet or female-controlled methods like IUD when women face reproductive coercion (Silverman et al. Citation2020).
Future research
Future research specifically designed to assess marginalising practices is needed to better understand the effect of these practices on reproductive health outcomes such as contraceptive use. The prevalence of the marginalising social practices may also be lower in this sample compared to other samples from India, affecting the power of the analysis. For instance, dowry practice is more prevalent in northern states of India like Bihar and Uttar Pradesh, compared to the state of Maharashtra, where our sample came from (Desai and Andrist Citation2010; National Crime Recoards Bureau Citation2019). There may be other dimensions of gender such as economic factors affecting the availability of wage employment and wedding expenses, as well as gender performance beyond purdah of male-female in the household may help understand the context further. Furthermore, given the complexity of women’s agency as a construct, there may be other mechanisms, such as access to resources, individual attitudes, and social norms, that can have a higher influence on traditional marital practices and their impact. Evidence directly measuring social norms around girls’ age at marriage has highlighted their influence on outcomes of education (Jafarey, Mainali and Montes‐Rojas Citation2020).
Conclusion
We examined an understudied area of structural factors that affect women’s agency in public health. Our findings suggest that women’s active involvement in choice of marriage partner may facilitate discussions with husbands about pregnancy prevention. Additionally, women’s partner choice and choice in the timing of their marriage facilitates modern contraceptive use. Thus, future programmes in India need to target marital choice beyond just delay in marriage, to improve women’s agency, thereby fostering enhanced couple communication and contraceptive use.
Supplemental Material
Download MS Word (57.7 KB)Acknowledgements
We are grateful to the CHARM2 field research staff, the public and private healthcare providers and participants who enrolled in our study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Andanda, P. 2009. “Vulnerability: Sex Workers in Nairobi's Majengo Slum.” Cambridge Quarterly of Healthcare Ethics 18 (2):138–146. doi:10.1017/s0963180109090239
- Anukriti, S., C. Herrera‐Almanza, P. K. Pathak, and M. Karra, 2020. “Curse of the Mummy-ji: The Influence of Mothers-in-Law on Women in India.” American Journal of Agricultural Economics 102 (5):1328–1351. Catalina Herrera-Almanza, Praveen Pathak, and Mahesh Karra. 1351. doi:10.1111/ajae.12114
- Babu, G. R., and B. V. Babu. 2011. “Dowry Deaths: A Neglected Public Health Issue in India.” International Health 3 (1):35–43. doi:10.1016/j.inhe.2010.12.002
- Banerjee, P. R. 2014. “Dowry in 21st-Century India: The Sociocultural Face of Exploitation.” Trauma, Violence & Abuse 15 (1):34–40. doi:10.1177/1524838013496334
- Barber, J. S. 2001. “The Intergenerational Transmission of Age at First Birth Among Married and Unmarried Men and Women.” Social Science Research 30 (2):219–247.
- Bhutta, Z. A. 2004. “Beyond Informed Consent.” Bulletin of the World Health Orgaization 82 (10):771–777.
- Char, A., M. Saavala, and T. Kulmala. 2010. “Influence of Mothers-In-Law on Young Couples' Family Planning Decisions in rural India.” Reproductive Health Matters 18 (35):154–162.
- Crandall, A., K. VanderEnde, Y. F. Cheong, S. Dodell, and K. M. Yount. 2016. “Women's Age at First Marriage and Postmarital Agency in Egypt.” Social Science Research 57:148–160. doi:10.1016/j.ssresearch.2016.01.005
- Desai, S., and L. Andrist. 2010. “Gender Scripts and Age at Marriage in India.” Demography 47 (3):667–687. doi:10.1353/dem.0.0118
- Dixit, A., S. Averbach, J. Yore, G. Kully, M. Ghule, M. Battala, S. Begum, N. E. Johns, F. Vaida, P. Bharadwaj, et al. 2019. “A Gender Synchronized Family Planning Intervention for Married Couples in Rural India: Study Protocol for the CHARM2 Cluster Randomized Controlled Trial Evaluation.” Reproductive Health 16 (1):88. doi:10.1186/s12978-019-0744-3
- Geller, S. E., A. Patel, V. A. Niak, S. S. Goudar, S. A. Edlavitch, B. S. Kodkany, and R. J. Derman. 2004. “Conducting International Collaborative Research in Developing Nations.” International Journal of Gynaecology and Obstetrics 87 (3):267–271. doi:10.1016/j.ijgo.2004.08.019
- Ghule, M., A. Raj, P. Palaye, A. Dasgupta, S. Nair, N. Saggurti, M. Battala, and D. Balaiah. 2015. “Barriers to Use Contraceptive Methods Among Rural Young Married Couples in Maharashtra, India: Qualitative Findings.” Asian Journal of Research in Social Sciences and Humanities 5 (6):18–33. doi:10.5958/2249-7315.2015.00132.X
- IIPS and ICF. 2017. National Family Health Survey (NFHS-4) 2015-16. Mumbai, India.
- IIPS and Macro International. 2007. National Family Health Survey (NFHS-3) 2005-06. Mumbai, India.
- Jafarey, S., R. Mainali, and G. Montes, Rojas. 2020. “Age at Marriage, Social Norms, and Female Education in Nepal.” Review of Development Economics 24 (3):878–909.
- Jeyaseelan, V., S. Kumar, L. Jeyaseelan, V. Shankar, B. K. Yadav, and S. I. Bangdiwala. 2015. “Dowry Demand and Harassment: Prevalance and Risk Factors in India.” Journal of Biosocial Science 47 (06):727–745.
- Kaur, N., and R. W. Byard. 2020. “Bride Burning: A Unique and Ongoing Form of Gender-Based Violence.” Journal of Forensic and Legal Medicine 75:102035. doi:10.1016/j.jflm.2020.102035
- Kumar, A., V. Bordone, and R. Muttarak. 2016. “Like Mother(-in-Law) Like Daughter? Influence of the Older Generation's Fertility Behaviours on Women's Desired Family Size in Bihar, India.” European Journal of Population = Revue Europeenne de Demographie 32 (5):629–660. doi:10.1007/s10680-016-9379-z
- McDougal, L., E. C. Jackson, K. A. McClendon, Y. Belayneh, A. Sinha, and A. Raj. 2018. “Beyond the Statistic: Exploring the Process of Early Marriage Decision-Making Using Qualitative Findings from Ethiopia and India.” BMC Womens Health 18 (1):144.
- Menard, S. 2002. Applied Logistic Regression Analysis. Thousand Oaks, CA: SAGE.
- Mystakidou, K., I. Panagiotou, S. Katsaragakis, E. Tsilika, and E. Parpa. 2009. “Ethical and Practical Challenges in Implementing Informed Consent in HIV/AIDS Clinical Trials in Developing or Resource-Limited Countries.” SAHARA: Journal of Social Aspects of HIV/AIDS Research Alliance 6 (2):46–57. doi:10.1080/17290376.2009.9724930
- National Crime Recoards Bureau, Ministry of Home Affairs. 2019. Crime in India 2019: Statistics. Vol. 1. New Delhi: National Crime Records Bureau.
- Pathfinder. 2013. PRACHAR: Advancing Young People’s Sexual and Reproductive Health and Rights in India. New Delhi: Pathfinder International. https://www.pathfinder.org/publications/prachar-advancing-young-peoples-sexual-reproductive-health-rights-india/.
- Prata, N., A. Fraser, M. J. Huchko, J. D. Gipson, M. Withers, S. Lewis, E. J. Ciaraldi, and U. D. Upadhyay. 2017. “Women's Empowerment and Family Planning: A Review of the Literature.” Journal of Biosocial Science 49 (6):713–743. doi:10.1017/S0021932016000663
- Raj, A., and U. Boehmer. 2013. “Girl Child Marriage and Its Association With National Rates of HIV, Maternal Health, and Infant Mortality Across 97 Countries.” Violence against Women 19 (4):536–551. doi:10.1177/1077801213487747
- Raj, A., M. Ghule, M. Battala, A. Dasgupta, J. Ritter, S. Nair, N. Saggurti, J. G. Silverman, and D. Balaiah. 2014. “Brief report: Parent-Adolescent Child Concordance in Social Norms Related to Gender Equity in Marriage - Findings from Rural India.” Journal of Adolescence 37 (7):1181–1184. doi:10.1016/j.adolescence.2014.08.006
- Raj, A., M. Ghule, J. Ritter, M. Battala, V. Gajanan, S. Nair, A. Dasgupta, J. G. Silverman, D. Balaiah, and N. Saggurti. 2016. “Cluster Randomized Controlled Trial Evaluation of a Gender Equity and Family Planning Intervention for Married Men and Couples in Rural India.” PloS One 11 (5):e0153190. doi:10.1371/journal.pone.0153190
- Raj, A., L. McDougal, J. G. Silverman, and M. L. Rusch. 2014. “Cross-Sectional Time Series Analysis of Associations Between Education and Girl Child Marriage in Bangladesh, India, Nepal and Pakistan, 1991-2011.” PLoS One.9 (9):ve106210.
- Raj, A., N. Saggurti, D. Balaiah, and J. G. Silverman. 2009. “Prevalence of Child Marriage and its Effect on Fertility and Fertility-Control Outcomes of Young Women in India: A Cross-Sectional, Observational Study.” The Lancet 373 (9678):1883–1889.
- Raj, A., N. Saggurti, D. Lawrence, D. Balaiah, and J. G. Silverman. 2010. “Association Between Adolescent Marriage and Marital Violence Among Young Adult Women in India.” International Journal of Gynecology & Obstetrics 110 (1):35–39.
- Raj, A., N. Saggurti, M. Winter, A. Labonte, M. R. Decker, D. Balaiah, and J. G. Silverman. 2010. “The Effect of Maternal Child Marriage on Morbidity and Mortality of Children Under 5 in India: Cross Sectional Study of a Nationally Representative Sample.” BMJ 340 (1):b4258.
- Santhya, K. G., U. Ram, R. Acharya, S. J. Jejeebhoy, F. Ram, and A. Singh. 2010. “Associations Between Early Marriage and Young Women's Marital and Reproductive Health Outcomes: Evidence from India.” International Perspectives on Sexual and Reproductive Health 36 (3):132–139. doi:10.1363/ipsrh.36.132.10
- Shakya, H. B., J. Silverman, K. M. Barker, C. Lapsansky, J. Yore, S. Aliou, M. I. Brooks, and A. Raj. 2020. “Associations Between Village-Level Norms on Marital Age and Marital Choice Outcomes Among Adolescent Wives in Rural Niger.” SSM - Population Health 11:100621–100621. doi:10.1016/j.ssmph.2020.100621
- Silverman, J. G., S. C. Boyce, N. Dehingia, N. Rao, D. Chandurkar, P. Nanda, K. Hay, Y. Atmavilas, N. Saggurti, and A. Raj. 2019. “Reproductive Coercion in Uttar Pradesh, India: Prevalence and Associations with Partner Violence and Reproductive Health.” SSM - Population Health 9:100484. doi:10.1016/j.ssmph.2019.100484
- Silverman, J. G., S. Challa, S. C. Boyce, S. Averbach, and A. Raj. 2020. “Associations of Reproductive Coercion and Intimate Partner Violence with Overt and Covert Family Planning Use Among Married Adolescent Girls in Niger.” EClinicalMedicine 22:100359. doi:10.1016/j.eclinm.2020.100359
- StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.
- Stenson, A. L., C. T. Kapungu, S. E. Geller, and S. Miller. 2010. “Navigating the Challenges of Global Reproductive Health Research.” Journal of Women's Health (2002) 19 (11):2101–2107. doi:10.1089/jwh.2010.2065
- Stroope, S., R. A. Kroeger, and J. Fan. 2021. “Gender Contexts, Dowry and Women's Health in India: A National Multilevel Longitudinal Analysis.” Journal of Biosocial Science 53 (4):508–521. doi:10.1017/s0021932020000334
- Subramanian, L., C. Simon, and E. E. Daniel. 2018. “Increasing Contraceptive Use Among Young Married Couples in Bihar, India: Evidence From a Decade of Implementation of the PRACHAR Project.” Global Health, Science and Practice 6 (2):330–344. doi:10.9745/ghsp-d-17-00440
- UNICEF. 2019. Child Marriage. New York: UNICEF Data. https://data.unicef.org/topic/child-protection/child-marriage/
- Vissandjee, B., R. Barlow, and D. W. Fraser. 1997. “Utilization of Health Services Among Rural Women in Gujarat, India.” Public Health 111 (3):135–148.
- WHO. 2001. Putting Women First: Ethical and Safety Recommendations for Research on Domestic Violence Against Women. Geneva: World Health Organization.
- World Health Organization Reproductive Health. 2007. Family Planning: A Global Handbook for Providers: Evidence-Based Guidance Developed Through Worldwide Collaboration. Baltimore and Geneva: Johns Hopkins Ccp-Info.
- Yount, K. M., A. Crandall, and Y. F. Cheong. 2018. “Women's Age at First Marriage and Long-Term Economic Empowerment in Egypt.” World Development 102:124–134. doi:10.1016/j.worlddev.2017.09.013
- Zou, G. 2004. “A Modified Poisson Regression Approach to Prospective Studies with Binary Data.” American Journal of Epidemiology 159 (7):702–706.
- Zou, G. Y., and A. Donner. 2013. “Extension of the Modified Poisson Regression Model to Prospective Studies with Correlated Binary Data.” Statistical Methods in Medical Research 22 (6):661–670. doi:10.1177/0962280211427759
