Abstract
This article explores the reception of the contraceptive implant, Implanon, by healthcare workers and patients in family planning units in South Africa’s public health sector. Based on observations conducted at public health facilities in the Eastern Cape Province, and on interviews with nurses and patients in the same province, the study explored real-world experiences of the implant. This article examines the strategies used by nurses to promote use of the device, and explores how patients themselves responded to a widescale, national rollout of the implant within government family planning services. The study examines the reception of Implanon in the context of the post-Apartheid era in South Africa, in which the vestiges of Apartheid-era healthcare provision, and lack thereof, continue to animate personal experiences of contraception.
Background
In 2014, the South African Department of Health began a national campaign to rollout the contraceptive implant, Implanon (Pillay et al. Citation2017). Implanon is a match-sized, flexible rod, made of silicone which is inserted into the upper-arm of the user, and which slowly releases the hormone etonogestrel into the blood stream. As a form of pregnancy prevention, Implanon is among the most effective contraceptives developed (Blumenthal, Gemzell-Danielsson, and Marintcheva-Petrova Citation2009). However, as this article shows, assumptions about its efficacy, including its affordability, are premised on ‘perfect-use’: namely, the idea that, once inserted, the implant will remain in situ, in the upper arm of its user, not requiring further medical attention such as treatment for side-effects, nor early removal. It was therefore hoped that Implanon would provide a rich new item on South Africa’s contraceptive menu, particularly for young women (Department of Health 2012).
The 2016 Demographic and Health Survey, the most recent for which data is available, found that 4% of women aged 15–49 were using Implanon. By the end of 2014, over 6,000 nurses had been trained on how to insert the device, and over 800,000 implants had been provided to women in South Africa (Lince-Deroche et al. Citation2016, 102). A lack of comprehensive data monitoring makes it difficult to estimate the rate of the implant’s removal. However, the small, extant literature in South Africa demonstrates high rates of premature discontinuation, with many women requesting early removal (Pillay et al. Citation2017; Chola et al. Citation2019; Krogstad et al. Citation2021). Research has also shown however that women on other forms of contraception anticipate using the implant in the future. A quantitative study of 481 women by Jonas et al. (Citation2021), for instance, found that 9.4% of women were currently using Implanon, while 20.2% intended to use it in the future.
This article examines the strategies used by healthcare workers to promote uptake of Implanon in their facilities, including the deliberate use of falsification to encourage patient acceptance of, and enthusiasm for, the device. It considers the dynamics of group counselling sessions at which family planning nurses promoted the implant, and in which patients voiced their concerns and posed revealing questions. It also foregrounds the experiences of patients, exploring the meaning of Implanon for them. It draws connections between contemporary meanings of Implanon and those surrounding the intrauterine device, another form of long-acting contraception, in South Africa’s Apartheid era.
Methods and study setting
This article examines Implanon’s reception among healthcare workers and their patients. It is based on 18 months of fieldwork, conducted over the course of 2014 and 2015. During this time, I conducted direct observation in the family planning wards of four healthcare facilities, including two large hospitals (Amathole Hospital and Buffalo City Hospital), and two clinics (Ubomi Day Hospital and Maitland City Clinic). These healthcare facilities were sampled because they provided public access to contraception. The study was a part of a wider project on the lives of HIV-positive adolescents, the Mzantsi Wakho study, which began in 2013 and ended in 2018 (Hodes et al. Citation2020). In the course of this wider study, over 1,000 hours were spent observing healthcare workers within family planning, HIV and trauma units, including during the years 2014–2015 which are the temporal focus here. This article focuses on data collected in the early years of the study, at a time when the national rollout of Implanon was a new and major priority for the Department of Health (Sehoai Citation2014, February 27). Contraceptive counselling sessions held in English were recorded and transcribed, and data were coded and analysed thematically and manually. All healthcare facilities and participants are anonymised and referred to by pseudonyms. This article focuses on observations in family planning units made between 2014, at the height of the Implanon public rollout, and 2015, in which resistance to Implanon had gathered pace. To supplement observations in healthcare facilities, a focus group (n = 16) was held with young women with experiences of contraceptive services in South Africa’s public health sector, and ongoing interviews were conducted with healthcare workers (n = 7) working within family planning wards and maternal and child healthcare within public health facilities. All interviews and focus groups were conducted in English. A qualitative dataset of interviews with adolescents living with HIV was coded manually for descriptions of Implanon over the course of a year from 2014 to 2015. Ethical permissions for the study were provided by the Universities of Cape Town and Oxford; the Eastern Cape Department of Health; and individual health facilities. Participants provided written informed consent for interviews and observations.
The study was located in the Eastern Cape to focus on the developmental challenges of healthcare in one of South Africa’s poorest provinces. Out of all of South Africa’s nine provinces, the Eastern Cape had the highest increase in maternal mortality between 2001 and 2007, and the highest levels of infant mortality (Human Rights Watch Citation2011, 4). Between 1997 and 2014, the Eastern Cape recorded a total of 4353 deaths among women during childbirth, pregnancy and puerperium (Saving Mothers 2018, 35). The Eastern Cape is among the poorest provinces in South Africa (Statistics South Africa Citation2018, 1). Conducting research in the Eastern Cape sheds light on the experiences of women, many of whom face employment insecurity and who carry a heavy burden in caring for their families.
The Implanon rollout
In 2014, the South African Department of Health launched a new campaign to rollout Implanon in public health facilities across South Africa. Thousands of nurses were trained in its insertion, using a ‘cascade’ method in which nurses who received direct training from the Department of Health trained their own colleagues on how to insert the device (Lince-Deroche et al. Citation2016). Nurses in family planning settings promoted the device with passion, recognising that it could reduce their workload by curtailing the need for repeat contraceptive appointments, pregnancy screening, antenatal and postnatal care, and termination of pregnancy. In 2014, on an average day in the family planning unit at Amathole Hospital, nurses inserted nine implants. In May 2014, nurses at Ubomi clinicFootnote1 inserted 184 implants.Footnote2 From 2014, the provision of Implanon for young women post-partum was so common as to be a form of routine care in certain healthcare facilities (Pillay, Manderson, and Mkhwanazi Citation2020).
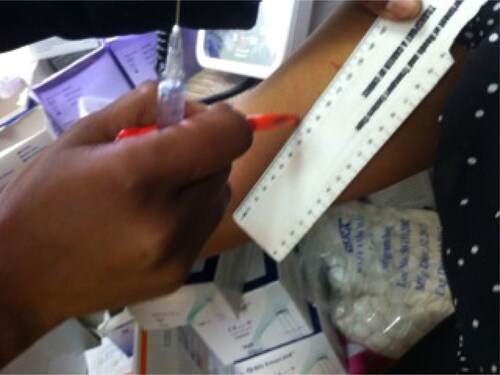
One of the key factors in the promotion of Implanon, by its manufacturers and by South African government health officials, was its supposed ease of insertion. The device came as a discrete package, including a trocar used to insert the device. The patient’s arm was measured, to determine the correct site of insertion just below the skin and to avoid embedding the device too deeply in surrounding tissue or muscle (). An anaesthetic was injected to numb the arm (). The trocar was then injected into the patient’s arm, and the cannula holding the implant itself was pushed for its release. The trocar was then retracted, with the device remaining in situ ().
Implanon’s insertion was not always as easy as appeared in Merck’s pamphlets, or in South Africa’s National Contraceptive Guidelines (Department of Health 2012, 32). The latter glosses over the intricacies of Implanon insertion, stating merely that the implant is ‘placed just under the skin of the upper arm’. Many healthcare workers in this study were understandably nervous about conducting Implanon insertions, fearing that they might insert the device too deeply, perforating muscle. The training that healthcare workers received helped to alleviate some of these anxieties, with a crucial caveat. Direct guidance was provided on Implanon’s insertion, but not its removal. Not anticipating that significant numbers of women would request removal, and not having any patients with which to experiment during the Implanon training, Dr Erasmus – a senior obstetrician gynaecologist – said that, during the course of the training the nurses had received, ‘there weren’t any cases to remove’ (personal correspondence, 27 October 2014). He explained: ‘They [nurses] practised a lot with insertion but, as there were no removal cases, they didn’t practice with this. It was not available in their training. So now the nurses lack confidence to remove them.’ Dr Erasmus explained that removing the implant was not as easy as inserting it. When this study was conducted, removals were only available at the two major hospitals in the city, and not in clinics or day hospitals.
Nurses working in clinics and day hospitals therefore had little or no experience removing the implant at the time their healthcare facilities began providing it. Moreover, nurses were under pressure to rollout Implanon as quickly as possible, in keeping with government fanfare that heralded the device as ushering in a new era in family planning (South African Government News Agency Citation2014). Healthcare workers therefore developed different tactics to promote Implanon. They presented the implant as a ‘techno-fix’, a technological device that would preclude the direct and opportunity costs of repeat contraceptive appointments required for other forms of birth control, principally injectables and the oral contraceptive pill. The literature on implanon highlights the convenience and efficacy of long-acting reversible contraception (Jonas et al. Citation2021; Chersich et al. Citation2017; Mullick et al. Citation2017). As explored below, in addition to touting its convenience, nurses sought more deeply to draw associations between Implanon and particular social values: of autonomy and independence, of responsibility for one’s health and fertility, and of upward mobility unfettered by the constraints of childrearing. Ironically, in later months of its national rollout in 2014, the discrete targeting of young women for Implanon sometimes had the opposite effect, evoking mistrust, suspicion and opposition. As Dr Erasmus explained: ‘Women are anxious about having a foreign body’.
Results
Promoting Implanon in South African healthcare facilities
In democratic South Africa, family planning units are intended to offer an array of services – including fertility support for those who are struggling to conceive. To a large extent, however, the bulk of family planning by nurses remains the provision of injectable contraceptives, principally depot-medroxyprogesterone acetate (‘Depo’) and Nuristerate (‘Nurrie’) (Chersich et al. Citation2017, 307). The rollout of Implanon was attractive to nurses in part because it promised to offset the amount of labour expended on repeat appointments for injectable and oral contraception. Yet some of the established practices of family planning nurses intended to reduce their workload, such as group contraceptive counselling for women receiving injectables, were carried over to the provision of the implant. In this study setting, women presenting in family planning facilities for contraception would be told to wait until a sufficient number had arrived and would then be given a group education session in which Implanon was promoted, with an emphasis on its benefits and little information about its prospective side-effects. As Sister Vukosi, a nurse conducting group contraceptive counselling, explained to patients seeking contraception at Ubomi Day Hospital:
‘There is this three-year implant that our government has given us for free. It’s very expensive, so expensive, and it is from private doctors, but [here] it is for free. It doesn’t have side-effects, it’s only a slight headache. It’s better than this one [gestures to boxes of contraceptive injections]. You can take it out when you want. It’s going to be finished, by next week. It will give you no problems with your womb. You don’t have to have the check-ups. Look, look [showing the register], how many people [have accepted Implanon]. There are no complaints. Look at all of these people [shows them the clinic register with patient information].
One of the patients in this group counselling session recounted: ‘There is a girl in my family who had the implant, and her arm became sore afterwards and she complained that she could not clean the house’. Sister Vukosi responded: ‘Even our aunty here [the clinic cleaner], she is cleaning with that arm, around our hospital, with that arm. They are lazy, others who say that they cannot clean. It [the implant] is not going to paralyse you. It’s not inside your veins, your arteries, it’s just outside the skin. It’s not moving all over your body, it’s just staying where it was. They are giving you the wrong information, your friends.’
Sister Vukosi sought to present Implanon as a luxury provided by the government, and an opportunity that should not be missed in case stocks were exhausted. But she also sought, most concertedly, to convince patients that there would be no negative side-effects.
One patient countered the nurse’s persuasive strategies with the authenticity of personal experience, of a family member who experienced pain and numbness, which had affected her mobility. The nurse responded with her own anecdote, a demonstration of direct experience, referring to the clinic’s cleaner who had accepted the implant without any impacts on her ability to clean the floors on which they were all standing. Despite the nurse’s techniques of persuasion, another criticism was levelled by patients: namely, that the implant would cause injury and bruising. Another young woman who was part of the group counselling session responded to the nurse’s promotion of Implanon by stating categorically: ‘I don’t want a wire, a blue rash, a bruise’. Revealing here is the description of Implanon as a ‘wire’. Healthcare workers were at pains to describe the device as a ‘plastic thing’, to highlight its inoffensiveness, and would often demonstrate the flexibility of the device by bending it with their fingers during patient education sessions, actively building associations with familiar domestic objects and describing Implanon as being like a ‘matchstick’. Some women had their own word for the device, which was decidedly less benign. They described Implanon as intsimbi – colloquially a piece of wire or metal picked up on the ground which, if lodged into the skin, could cause infection. The device was also described by one patient as a ‘steel knife’, a reference to the size and sharpness of the trocar used in its insertion.
In this study, healthcare workers reported that Implanon’s side-effects were widespread among their patients, including amenorrhoea and depression. Despite these side-effects, Dr. Erasmus, explained that women ‘love the implant because they’re not dependent on health services’. Implanon was seen as a potential solution to the costly and time-consuming repeat appointments required for other forms of contraception, including injectables and the oral contraceptive pill.
Sister Gerwel, a nurse in a family planning ward which had inserted 143 implants in a single month, described the enthusiasm with which older women received the implant:
‘The older women, when they come here, I tell them that if they don’t have the time to come to the clinic every two months for Nuristerate, [Implanon] will mean that they only have to come back in three years, and they said ‘I don’t have time to come every two months! Give this thing to me sister!’
‘The environment I am in, it’s very political. I’m saying the government brought us this thing (the implant) for R1,700 to get the votes. This thing is very expensive. I don’t know how long I’m going to have it. I use these strategies. I tell them, ‘This morning there were five white guys there. They came from […] those white areas. They came here to fetch your things [the implants]. The people with the money are coming here to fetch the things meant for us to benefit themselves… I tell them [patients], ‘Sister is trying to take you out of the bush. You must come out of the bush.’ I play on their education.’
Parallels between Implanon and the IUD
Interactions between nurses and patients revealed much about the strategies for promoting Implanon. They revealed the fears and suspicions that circulated about the implant, including that it would cause bruising, pain and numbness, and potentially have more harmful and serious effects. While concerns about migration and embedding may have been disproportionate to their real risks, both are empirical risks, although they are rare. These risks are apparent not just in the fine-print of obscure clinical reports, but also in Merck’s Implanon instruction manual. Merck’s information for healthcare workers inserting and removing Implanon states: ‘Complications related to insertion and removal procedures, such as pain, paraesthesia, bleeding, hematoma, scarring, or infection, may occur… Implant removal may be difficult or impossible if the implant is not inserted correctly, inserted too deeply, not palpable, encased in fibrous tissue, or has migrated’ (Merck Sharp & Dohme Citation2012).
The modern medical concept of a long-acting contraceptive device, that would remain in the body, is at least a century old. Early devices were mostly conceived as intrauterine in character, and it is only in recent decades that the technological potential of a sub-dermal contraceptive implant has emerged. Patients’ fears about migration and perforation were not only a response to a real medical risk, but to the experiential history of Impanon’s technological predecessors. In the history of intrauterine devices, migration, perforation and expulsion are some of the side-effects experienced by patients (Spilhaus Citation1974, Rowlands, Oloto, and Horwell Citation2016). These negative effects have driven medical experimentation and technological advancement in contraception, and they have also shaped popular understandings among healthcare workers and patients.
The IUD became available in South Africa for the first time in the late 1960s (Robertson Citation1971). The next decade saw both seismic changes in South Africa’s contraceptive policies, and a technological revolution in IUDs. In 1974, the Apartheid state launched its national family programme, the key aim of which was to reduce population growth among Black South Africans (Kaufman Citation2000; Brown Citation1987). The fear of oorstrooming (literally ‘streaming over’ or ‘swamping’) and that Black population growth would translate into political power unseating white minority rule, animated the state’s policies on population control. The inauguration of the state family planning programme in 1974 coincided with the modern technological revolution in contraception, beginning in the 1960s with the birth of the contraceptive pill. These two processes were mutually constitutive, with the state’s efforts to reduce Black population growth converging with medical advances in contraception. From the late 1960s, a variety of intrauterine devices were provided to patients in South Africa’s health sector (Robertson Citation1971; Spilhaus Citation1974; Spilhaus Citation1975). These included the Lippes Loop, the Margulis Spiral, the Copper T and the Dalkon Shield.
During the 1970s, several studies published in the South African Medical Journal provided insights into local contraceptive promotion by healthcare workers, and, more obliquely, their reception among patients (Robertson Citation1971; Spilhaus Citation1974). In 1974, the journal featured an article reporting the findings of a large study which compared the performance of IUDs among over 2,000 patients in a clinic in Soweto. It emphasises the benefits of the IUD precisely because these devices preclude patient agency. The article states:
‘The contraceptive pill and other conventional methods had been used previously, but it was obvious that these methods requiring patient-responsibility were of very limited use. The pill was simply not taken consistently and correctly, as sustained motivation was lacking due to lack of education, and our experience very soon led to the conviction that a good-performance IUD was infinitely preferable to the pill in our clinic society’ (Spilhaus Citation1974, 1302).
In a pathbreaking account of the history of contraception in South Africa, Barbara Brown (Citation1987) traces the exponential increase in contraceptive service provision and promotion starting with the establishment in 1974 of South Africa’s Family Planning Programme. Between 1974 and 1983, the number of clinics offering family planning increased twenty-fold, with over 36,000 contraceptive points in operation in 1983 (Brown Citation1987). By the mid-1990s, this number had doubled, and over 65,000 contraceptive points were available to the public, most of which were made up of stops on mobile contraceptive routes, often planned quarterly to coincide with the contraceptive renewals for clients using Depo (Cooper et al. Citation2004, 71). Local health authorities often provided only child health services, with family planning services provided by healthcare workers whose responsibility was only to provide contraception (Fonn et al. Citation1998, 23).
During the democratic transition, the transformation of the health system, and a concomitant focus on primary healthcare provision, led to a de-prioritisation of IUDs. This de-prioritisation was in part political, due to the association of IUDs with the imposition of oppressive medical controls which sought to limit births among Black women and to maintain the Apartheid political status quo (Chimere-Dan Citation1996). The post-Apartheid government sought to move away from population or birth control, with its associations of demographic discrimination. The effects of the AIDS epidemic, and its impacts on women’s reproductive health, absorbed the attention of gynaecologists and obstetricians, who faced catastrophic rates of HIV-related cancers and other pathologies. The IUD’s associations with Apartheid-era reproductive controls, and the resources and skills it required for insertion, resulted in its steep decline in provision. As Dr Mzamane, a senior gynaecologist in the Eastern Cape explained: ‘There’s resistance to IUDs, to pap smears. It comes back to a serious and dire shortage of equipment. You require a long lamp, a speculum, a long scissor. For the IUD, you need time, sterility, skill, a swab holder. The staff are worried that it will migrate, it will perforate, and so they are resistant to introducing it. There’s a lot of excitement about Implanon but they are going to have to remove it, to deal with the side-effects (18 January 2014).’
Part of the ‘excitement’ about Implanon, and a crucial component of its rapid rollout, was the growing fear in the late 2000s that particular forms of contraception, particularly depot-medroxyprogesterone acetate (Heffron et al. Citation2012), but also oral contraceptives and the T38-a copper intra-uterine device (Morrison, Turner, and Jones Citation2009), were associated with women acquiring sexually transmitted infections, including HIV. The possibility that hormonal contraception might increase HIV transmission risk had long been suggested in the clinical literature (Daly et al. Citation1994), but the fear that it could increase both HIV infection and transmission escalated dramatically with the publication of a large prospective cohort study in 2011 which found that the ‘[u]se of contraceptives was associated with a two-times increase in the risk of HIV-1 transmission from women to men’ (Heffron et al. Citation2012, 24). The findings of the study caused ructions within the scientific community, with some asserting that other studies had shown no association between hormonal contraception and HIV-infection (Myer Citation2012). However, the implications of the study were so severe that WHO (World Health Organisation) (Citation2012) convened a technical review in which it deliberated on the evidence base and decided ultimately that various study results were too mixed and their design too flawed to conclude that hormonal contraception increased the risk of HIV transmission or acquisition. Nonetheless, WHO added a cautious caveat in its report for inclusion in guidelines on the medical eligibility criteria for contraceptive use:
‘Some studies suggest that women using progestogen-only injectable contraception may be at increased risk of HIV acquisition, other studies do not show this association…[B]ecause of the inconclusive nature of the body of evidence on possible increased risk of HIV acquisition, women using progestogen-only injectable contraception should be strongly advised to also always use condoms…Expansion of contraceptive method mix and further research on the relationship between hormonal contraception and HIV infection is essential.’ (1)
An Implanon insertion gone awry
This study identified the case of a patient, Margaret, age 41, who had the implant inserted earlier that morning at a Maitland City Clinic (located in a densely populated urban area in the Eastern Cape). Margaret had reacted badly to the insertion, with significant swelling and bruising in her upper arm. As the morning wore on, she became increasingly worried about the implant, and decided to travel to Ubomi Day Hospital, known within the community for its superior medical care, to seek the attention of a nurse or doctor. At Ubomi, Margaret was examined by a doctor, who told her that she had not received training on Implanon and did not know how to treat her. The doctor advised Margaret to ‘go back to the clinic where she had it inserted to have it taken out’ (Sister Gerwel, personal correspondence, 21 November 2014). Instead, Margaret waited to consult the nurses at Ubomi’s family planning unit, who had received training on Implanon from the Department of Health. The nurses, including some of the most experienced providers of Implanon in the province, examined Margaret’s arm. The senior nurse, head of the family planning unit, commented that the implant was ‘very deep’, and that it had potentially penetrated the muscle. She advised Margaret to return to Maitland City Clinic. Back there, Margaret was examined by the same nurse who had inserted the implant and advised to ‘leave it to see what happens over the weekend’.
By 2015, this study found that requests for Implanon removal were so common in public health facilities around the Eastern Cape that the device was nicknamed ‘Outplanon’. In response, healthcare facilities developed their own informal protocols to stem the tide of Implanon removals. These included counselling procedures, in which nurses and doctors tried to persuade patients not to remove the devices; referral of patients to other facilities for the removal (in the knowledge that the burdens of transport and time might deter the patient from removing the device); mandatory requirements of a month-long waiting period after the request for removal; and outright refusals to remove the device. But even these strategies were of questionable effect. By 2014, healthcare workers in this study reported that women had started to remove the devices themselves.
While this was a grave disappointment to the healthcare workers and officials who had seen Implanon as a potential solution to South Africa’s reproductive woes, it was not in fact surprising. High rates of non-completion of Implanon, reflected in requests by patients for early removal of the device, are replete within the clinical literature, both globally and nationally. In a guide to contraceptive product selection published in the South African Journal of Family Practice in 2010 (Steyn and Kluge Citation2010), the authors refer to the international, specifically the US literature on Implanon’s side-effects. Citing research from the USA, they recognise that Implanon has an effect on bleeding patterns, with 20% of women experiencing amenorrhoea and 50% experiencing unpredictable or prolonged bleeding (Steyn and Kluge Citation2010, 502; NICE (National Institute for Health and Clinical Excellence) Citation2005). The article stated: ‘Up to 43% of women will discontinue Implanon prior to completion of the three years, most of whom do so because of irregular bleeding patterns’ (Faculty of Sexual and Reproductive Healthcare Clinical Effectiveness Unit 2008).
In conceiving of Implanon as a ‘techno-fix’, a technological device that would solve South Africa’s unmet demand for contraceptives, and which would reduce both the direct and the opportunity costs of repeat contraceptive appointments, South Africa’s Department of Health made a grave error. Following high rates of initial uptake in the aftermath of the state’s campaign to train nurses on providing Implanon, and on rolling out the device through public family planning services, the frequency of side-effects saw substantial numbers of requests for early removals of the implant (Adeagbo et al. Citation2017, 822; Beesham et al. Citation2019, 750). Patients reported a host of side-effects from Implanon, including irregular or prolonged menstrual bleeding, headache, weight-gain, and perpetual pain at the site of insertion. An interview with one young woman, Noluntu (aged eighteen), revealed some of the side-effects attributed to Implanon.
Interviewer: Have you heard about Implanon?
Noluntu: Oh yes I have heard about it, and also that it makes one bloated, as if they are blown air in them, even on their faces.
Interviewer: Oh, and what else do you know about it?
Noluntu: It stays in you for three years. I have this cousin who had it and before she had it she was tiny, now she’s big. Yoh! I heard when it treats you bad they don’t know how to take it out at the clinic. They just put the steel in your arm but they don’t know how to take it out.
Interviewer: Would you have it?
Noluntu: No. I’m scared.
Interviewer: Scared of what?
Noluntu: To gain weight. I saw my cousin and I don’t want to be like that… ugly. (personal correspondence, 9 July 2014).
Sister Mkhize (family planning nurse, personal communication, 20 June 2014) at Ubomi Day Hospital explained that initially patients were ‘excited’ about the implant and were ‘coming in numbers. ‘But then the education has been coming from the community’. Here, the community was seen as a source of misinformation and resistance to the implant.
In her patient counselling sessions, Sister Mkhize explained to patients that they should not consider the implant a temporary measure. ‘I don’t want people to insert it now, and then have it removed.’ In a study of the fiscal costs of contraceptive provision in South Africa, the authors estimated that the cost of early Implanon removals was ZAR 75 million, compared to an estimated ZAR 56 million if the normal removal rate (calculated according to three years of Implanon use by patients) was applied (Chola et al. Citation2019, 756). Nurses frequently emphasised the cost of Implanon in counselling sessions with patients, seeking to disincentivise early removals in spite of negative side-effects such as irregular bleeding.
In one of the small number of studies on user perspectives of Implanon in South Africa, researchers found that the vast majority of women who had asked for the implant to be removed had done so because of negative side-effects, especially ‘heavy or prolonged bleeding’ (Pillay et al. Citation2017, 819). The authors of the study noted that ‘Rumours, based on partially accurate information, appear to have accrued rapidly’, and noted that rumours and misinformation had also contributed to high rates of removal (Pillay et al. Citation2017, 815, 820).
Limitations
There are multiple limitations to this study. First, the article draws primarily on data gathered in 2014–2015, when Implanon was first widely introduced in the public healthcare sector. It is therefore limited in terms of the timespan. Second, the study focused on four healthcare facilities when the implant was rolled out across dozens or even hundreds of facilities from 2014 onwards. This work therefore represents the practices of only a small number of healthcare facilities. Third, the study draws on observational data and on qualitative interviews and focus groups. While the researcher made efforts to reduce the biases that accrue in observational and qualitative research, the researcher’s position as a young, White, English-speaking woman would have influenced her reception by study participants.
Conclusion
This chapter explores Implanon from the perspectives of healthcare workers and patients, delving into popular beliefs about the implant. It argues there are powerful continuities between the provision and experience of reproductive healthcare in Apartheid and post-Apartheid South Africa. The chapter examines how the social meanings of medical technologies are contested by patients, including through their interactions with healthcare workers. It is a study of the making of medical meaning in the present, but in relation to the ideas and experiences from the past.
South Africa’s family planning services were used historically to reduce population growth among the Black majority. During the transition to democracy, the government sought to expand the contraceptive method mix available in the public sector. In 2014, the Department of Health began a major campaign to rollout the Implanon in family planning units country wide. Despite being freely available, the uptake of implanon among women in South Africa has been relatively low (Chersich et al. Citation2017; Jonas et al. Citation2021; Beesham et al. Citation2022). After high initial uptake, the numbers of women presenting in the public sector for Implanon declined steeply, as popular accounts of Implanon’s negative side-effects gained traction. Myths about the implant’s migration hearkened back to popular accounts of the IUD, with many women voicing their suspicions that the implant might result in negative side-effects, including irregular or prolonged bleeding patterns. In group counselling sessions in healthcare facilities, women voiced both their enthusiasm and their trepidation towards Implanon, conveying both popular support for, and fears about, the new device.
This article reports on one of a limited number of studies to explore popular perceptions and practices regarding the implant, among both healthcare workers and women. Recent research has highlighted in particular what providers can do to ensure that women are prepared for the side-effects they may experience from Implanon (Mullick et al. Citation2017). More research is needed, in particular to understand the reasons for Implanon’s early removal, and to provide further, in-depth analysis about the discontinuation of the implant, together with women’s other contraceptive choices, in the post-Apartheid era.
Acknowledgements
I am grateful to peer reviewers for their valuable feedback on this work. Principal thanks go to the research participants and to the anonymised healthcare facilities in which this work was carried out. Thanks are also due to the co-principal Investigators of the Mzantsi Wakho study, Lucie Cluver and Elona Toska, and to Mildred Thabeng and Kanya Makabane for research assistance.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes
1 Clinics and healthcare workers in this study have been given pseudonyms to ensure confidentiality.
2 &
References
- Adeagbo, O., S. Mullick, D. Pillay, M. Chersich, C. Morroni, N. Naidoo, M. Pleaner, and H. Rees. 2017. “Uptake and Early Removals of Implanon NXT in South Africa: Perceptions and Attitudes of Healthcare Workers.” South African Medical Journal 107 (10):822–826.
- Beesham, I., A. Bosman, M. Beksinska, C. Scoville, J. Smit, and K. Nanda. 2022. “Contraceptive Method Preference and Reasons for Contraceptive Discontinuation among Women Randomised to Intramuscular Depot Medroxyprogesterone Acetate, A Copper Intrauterine Device or a Levonogestrel Implant: Findings from Durban, South Africa.” Contraception 108:37–43.
- Beesham, I., J. Smit, M. Beksinska, M. Panday, V. Makatini, and S. Evans. 2019. “Reasons for Requesting Removal of the Hormonal Implant, Implanon NXT, at an Urban Reproductive Health Clinic in KwaZulu-Natal, South Africa.” South African Medical Journal 109 (10):750–755.
- Blumenthal, P., K. Gemzell-Danielsson, and M. Marintcheva-Petrova. 2009. “Tolerability and Clinical Safety of Implanon.” The European Journal of Contraception and Reproductive Health Care 63 (1):29–36.
- Brown, B. 1987. “Facing the 'Black Peril’: The Politics of Population Control in South Africa.” Journal of Southern African Studies 13 (2):256–273.
- Chersich, M., N. Wabiri, K. Risher, O. Shisana, D. Celentano, T. Rehle, M. Evans, and H. Rees. 2017. “Contraception Coverage and Methods Used among Women in South Africa: A National Household Survey.” South African Medical Journal 107 (4):307–314.
- Chimere-Dan, O. 1996. “Contraceptive Prevalence in Rural South Africa.” International Family Planning Perspectives 22 (1):4–9.
- Chola, L., K. MacQuilkan, A. Winch, R. Rapiti, I. Edoka, C. Kohli-Lynch, and K. Hofman. 2019. “Projecting the Fiscal Impact of South Africa’s Contraceptive Needs: Scaling Up Family Planning Post 2020.” South African Medical Journal 109 (10):756–760.
- Cooper, D., C. Morroni, P. Orner, J. Moodley, J. Harries, L. Cullingworth, and M. Hoffman. 2004. “Ten Years of Democracy in South Africa: Documenting Transformation in Reproductive Health Policy and Status.” Reproductive Health Matters 12 (24):70–85.
- Daly, C., G. Helling-Giese, J. Mati, and D. J. Hunter. 1994. “Contraceptive Methods and the Transmission of HIV: Implications for Family Planning.” Genitourinary Medicine 70 (2):110–117.
- Department of Health, South Africa. 2012. “National Contraception Clinical Guidelines.” https://www.gov.za/sites/default/files/gcis_document/201409/contraceptionclinicalguidelines28jan2013-2.pdf
- Evidence for Contraceptive Options and HIV Outcomes (ECHO) Trial Consortium. 2019. “HIV Incidence among Women Using Intramuscular Depot Medroxyprogesterone Acetate, a Copper Intrauterine Device, or a Levonorgestrel Implant for Contraception: A Randomised, Multicentre, Open-Label Trial.” The Lancet 394 (10195):303–313.
- Fonn, S., M. Xaba, S. San Tint, D. Conco, and S. Varkey. 1998. “Reproductive Health Services in South Africa: From Rhetoric to Implementation.” Reproductive Health Matters 6 (11):22–32.
- Heffron, R., D. Donnell, H. Rees, C. Celum, N. Mugo, E. Were, G. de Bruyn, E. Nakku-Joloba, K. Ngure, J. Kiarie, et al. 2012. “Use of Hormonal Contraceptives and Risk of HIV-1 Transmission: A Prospective Cohort Study.” The Lancet Infectious Diseases 12 (1):19–26.
- Hodes, R. 2017. “Popular Perspectives on Teenage Pregnancy in South Africa.” In Young Families: Gender, Sexuality and Care, edited by N. Mkhwanazi and D. Bhana, 17–30. Cape Town: Human Sciences Research Council Press.
- Hodes, R., L. Cluver, E. Toska, and B. Vale. 2020. “Pesky Metrics: The Challenges of Measuring Antiretroviral Treatment Adherence among HIV-Positive Adolescents in South Africa.” Critical Public Health 30 (2):179–190.
- Hoggart, L., and V. L. Newton. 2013. “Young Women’s Experiences of Side-Effects from Contraceptive Implants: A Challenge to Bodily Control.” Reproductive Health Matters 21 (41):196–204.
- Human Rights Watch. 2011. “‘Stop Making Excuses’: Accountability for Maternal Health Care in South Africa.” https://www.hrw.org/report/2011/08/08/stop-making-excuses/accountability-maternal-health-care-south-africa
- Jonas, K., M. Mazinu, M. Kalichman, S. Kalichman, C. Lombard, C. Morroni, and C. Mathews. 2021. “Factors Associated with the Use of the Contraceptive Implant among Women Attending a Primary Heatlh Clinic in Cape Town, South Africa.” Frontiers in Global Women’s Health 2:672365.
- Kaufman, C. 2000. “Reproductive Control in Apartheid South Africa.” Population Studies 54 (1):105–114.
- Krogstad, E. A., M. Atujuna, E. T. Montgomery, A. M. Minnis, C. Morroni, and L.-G. Bekker. 2021. “Perceptions Matter: Narratives of Contraceptive Implant Robbery in Cape Town, South Africa.” Culture, Health & Sexuality 23 (3):383–396.
- Lince-Deroche, N., M. Pleaner, C. Morroni, S. Mullick, C. Firnhaber, J. Harries, E. Sinanovic, M. Mulongo, and P. Holel. 2016. “Achieving Universal Access to Sexual and Reproductive Health Services: The Potential and Pitfalls for Contraceptive Services in South Africa.” South African Health Review 1:95–108.
- Merck Sharp & Dohme. 2012. “Implanon: Insertion and Removal.” https://www.Implanon-usa.com/en/HCP/learn-about-it/insertion-and-removal/
- Morrison, C., A. Turner, and L. Jones. 2009. “Highly Effective Contraception and Acquisition of HIV and Other Sexually Transmitted Infections.” Best Practice & Research. Clinical Obstetrics & Gynaecology 23 (2):263–284.
- Mullick, S., M. Chersich, Y. Pillay, and H. Rees. 2017. “Introduction of the Contraceptive Implant in South Africa: Successes, Challenges and the Way Forward.” South African Medical Journal 107 (10):812–814.
- Myer, L. 2012. “The Limits of Observational Epidemiology: Hormonal Contraception and Women’s Risk of HIV Infection.” South African Journal of Science 108 (7/8):1–2.
- National Committee for the Confidential Enquiries into Maternal Deaths. 2018. “Saving Mothers. Seventh Triennial Report on Confidential Enquiries into Maternal Deaths in South Africa: Short Report.” https://www.westerncape.gov.za/assets/departments/health/saving_mothers_2014-16_-_short_report.pdf
- NICE (National Institute for Health and Clinical Excellence). 2005. Long-Acting Reversible Contraception. Clinical Guideline 30. London: NICE. https://www.nice.org.uk/guidance/cg30
- Pillay, D., M. Chersich, C. Morroni, M. Pleaner, O. Adeagbo, N. Naidoo, S. Mullick, and H. Rees. 2017. “User Perspectives on Implanon NXT in South Africa: A Survey of 12 Public-Sector Facilities.” South African Medical Journal 107 (10):815–821.
- Pillay, N., L. Manderson, and N. Mkhwanazi. 2020. “Conflict and Care in Sexual and Reproductive Health Services for Young Mothers in Urban South Africa.” Culture, Health & Sexuality 22 (4):459–473.
- Robertson, I. 1971. “Report on Family Planning Clinics Conducted in the Cape Town Municipal Area from 1960 to 1969.” South African Medical Journal 45:291–292.
- Rowlands, S., E. Oloto, and D. Horwell. 2016. “Intrauterine Devices and Risk of Uterine Perforation: Current Perspectives.” Open Access Journal of Contraception 7:19–32. doi:10.2147/OAJC.S85546
- Sehoai, R. 2014. “Motsoaledi Launches New Contraceptive Implant.” Bhekisisa Centre for Health Journalism, February 27. https://bhekisisa.org/article/2014-02-27-motsoaledi-launches-new-contraceptive-implant/
- South African Government News Agency. 2014. “Government Unveils Free Contraceptive Device for Women.” February 27. https://www.sanews.gov.za/south-africa/government-unveils-free-contraceptive-device-women
- Spilhaus, M. 1974. “The Intra-Uterine Devicei Soweto and Other Townships.” South African Medical Journal 48 (3):1302–1305.
- Spilhaus, M. 1975. “The Copper-T Intrauterine Device.” South African Medical Journal 49 (52):2153.
- Statistics South Africa and the South African Medical Research Council. 2018. “South Africa Demographic and Health Survey. Key Findings.” https://dhsprogram.com/pubs/pdf/SR248/SR248.pdf
- Statistics South Africa. 2018. “Community Survey. Provincial Profile Eastern Cape, 2016.” http://cs2016.statssa.gov.za/wp-content/uploads/2018/07/EasternCape.pdf
- Steyn, P., and J. Kluge. 2010. “Contraceptives: A Guide to Product Selection.” South African Family Practice 52 (6):499–504.
- WHO (World Health Organisation). 2012. Hormonal Contraception and HIV: Technical Statement. Geneva: World Health Organisation. https://www.ncbi.nlm.nih.gov/books/NBK131971/pdf/Bookshelf_NBK131971.pdf.