Abstract
Objectives: To evaluate the economic burden of herpes zoster (HZ) on the US healthcare system among an immunocompetent population.
Methods: Claims data from the MarketScan Research databases for 2008–2011 were extracted to determine the incremental healthcare resource utilization (RU) and direct medical costs associated with HZ. Immunocompetent HZ-patients were identified and directly matched 1:1 with immunocompetent non-HZ controls using demographic and clinical variables. Analysis was limited to claims 21 days prior to through the first year following HZ diagnosis. Cases with post-herpetic neuralgia (PHN) were analyzed separately.
Results: A total of 98,916 HZ-patients were matched to controls. HZ-patients had a mean age of 50.4 (SD = 18.8) years and 56.6% were females. HZ-cases had significantly higher RU (0.016 inpatient visits, 0.153 ER visits, 2.116 outpatient office visits, and 3.730 other outpatient services) compared to controls (p < 0.001). Differences increased substantially in the presence of PHN. Total mean incremental healthcare costs for HZ-cases were $1308 and quadrupled to $5463 in those with PHN (both p < 0.001). Overall, primary cost drivers were outpatient prescriptions and other outpatient services. For those with PHN, inpatient services also played a significant role.
Limitations: This study was limited to only those individuals with US commercial health coverage or private Medicare supplemental coverage; therefore, results of this analysis may not be generalizable to HZ patients outside of the US, with other health insurance or without coverage.
Conclusions: HZ presents a significant economic and resource burden on the US healthcare system among immunocompetent patients of nearly all ages, particularly when complicated by PHN.
Introduction
Despite the availability of an efficacious and safe vaccine, herpes zoster (HZ), or shingles, continues to have a significant financial impact on the US healthcare system. HZ, characterized by unilateral radicular pain and a skin rash with blisters, is a reactivated varicella zoster virus (VZV) infection that affects the central nervous systemCitation1–3. An estimated one million new cases of HZ are reported each year in the US, with the risk increasing sharply after 50 years of ageCitation4–6. Post-herpetic neuralgia (PHN) constitutes the most common debilitating sequelae and cause of HZ-associated morbidity. Studies report 10–25% of patients develop PHN following the onset of HZ, with frequency increasing with ageCitation6–9. Several studies have demonstrated that HZ, and more particularly PHN, have a significant impact on quality-of-lifeCitation10–13.
Substantial costs are tied to the treatment for HZ in the US. The average cost for HZ treatment has been estimated to be between $431Citation14 and $1112Citation5 over the initial 90 days and ranged from $1052Citation15 to $1300Citation11 over the first year following diagnosis. Estimates suggest that the direct annual medical cost burden of HZ is over $1 billion in the USCitation5,Citation11. Several studies have examined the burden of HZ on the US population, both with and without the presence of PHN; however, these studies involved the use of data from 2003 and earlier, lacked control groups to estimate excess cost burden of illness, or examined the general population which included both immunocompromised and immunocompetent populationsCitation5,Citation11,Citation14,Citation15. The use of earlier data in these studies was prior to the availability of Zostavax (zoster vaccine live)Footnote†, a live-attenuated vaccine approved by the US Food and Drug Administration (FDA) for the prevention of HZ in immunocompetent adults 50 years of age and olderCitation4,Citation16. To date, recommendation by the Advisory Committee on Immunization Practices (ACIP) is limited to adults 60 years of age and olderCitation17,Citation18. The objective of this study was to evaluate incremental healthcare resource utilization and direct medical costs associated with herpes zoster among an immunocompetent population in the US using nationally-representative administrative databases from years 2008–2011, providing an update on the financial impact of HZ on the US healthcare system.
Patients and methods
Study design
This was a retrospective case-control analysis of immunocompetent patients with (cases) and without (controls) a diagnosis of herpes zoster. Total costs were assessed to describe the incremental financial burden of HZ patients within the 21-day pre-diagnosis phase to capture the prodromal symptoms of herpes zoster through the year following diagnosis. Differences in healthcare resource utilization events between those with and without diagnosed HZ were described and compared. To account for differences in costs and utilization due to disease severity, patients with PHN were identified and analyzed separately.
Data source
Administrative claims from the Truven Health Analytics MarketScanFootnote‡ Commercial Claims and Encounters (Commercial) and Medicare Supplemental and Coordination of Benefits (Medicare) databases for the period January 1, 2007 through December 31, 2011 were utilized for this study. Both the Commercial and Medicare databases contain integrated patient-level pharmacy and medical (inpatient and outpatient) claims for over 40 million individuals annually, encompassing employees, their spouses, and dependents covered under a variety of employer-sponsored fee-for-service and managed care health schemes. The MarketScan Research Databases include persons from all US states, are de-identified, and are fully compliant with the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Since this study did not involve the collection, use, or transmittal of individually identifiable data, Institutional Review Board review or approval was not required.
Study population
The target population was immunocompetent patients who did not have a zoster vaccine live claim. A series of selected ICD-9-CM diagnoses, procedures, and treatment criteria, informed by the Centers for Disease Control and Prevention, were used to determine the immunocompetent status of each patientCitation4. Specifically, these included malignancy, HIV, chronic renal disease, transplantation, diseases of white blood cells, aplastic anemia, other disease conditions indicating a compromised immune system, and treatment with selected chemotherapy/radiotherapy, corticosteroids, TNF inhibitors, protease inhibitors, and reverse transcriptase inhibitors, as well as azathioprine, cyclosporine, and tacrolimus. The full list of criteria and the codes used for identification will be furnished upon request. Patients with a diagnosis of HZ (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] diagnosis code 053.xx) between January 1, 2008 and January 1, 2011, enrolled continuously 12 months before and following the diagnosis, and having no claims for HZ or evidence of receiving zoster vaccine live in the 12 months prior to HZ diagnosis were eligible for inclusion. The study period spanned 24 months: 12 months before (pre-period) and after (observation period) the index date.
A sub-set of patients diagnosed with HZ and evidence of PHN was selected from the database. PHN was defined as pain that persisted for more than 90 days after the rash onset, and identification was made using the same method employed by Langan et al.Citation19, which is the modified algorithm proposed by Klompas et al.Citation20. The PHN cohort comprised HZ cases with:
at least one claim for HZ with other nervous system complications (ICD-9-CM 053.1x) between 3 months and 1 year after the initial HZ diagnosis OR
At least one claim for neuralgia, neuritis, and radiculitis (ICD-9-CM 729.2) between 3 months and 1 year after the initial HZ diagnosis OR
A second HZ diagnosis between 3 months and 1 year after the initial HZ diagnosis AND at least one pharmacy claim for an antidepressant, analgesic, or anticonvulsant within 1 month of the second diagnosis.
Matching
An immunocompetent control group without HZ (drawn from a 10% sample of the database) was selected and directly matched 1:1 to those with HZ using demographic and clinical variables, including age group in years (< 18, 18–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–79, 80+), gender (male or female), health plan type (comprehensive/indemnity, exclusive provider/preferred provider organization [EPO/PPO], point of service [POS], health maintenance organization [HMO], consumer directed/high deductible health plan [CDHP/HDHP], Other/Unknown), US Census geographical region (Northeast, North Central, South, West, Unknown), Charlson Comorbidity Index (CCI) (0, 1, 2, 3+), payer type (commercial or Medicare), pre-period expenditures (calculated from 365 days to 22 days prior to the index date and banded as follows: $0, $1–$251, $251–$500, $501+), and index year (2008, 2009, 2010, 2011). For patients with HZ, the index date was the date of the first claim with an incident HZ diagnosis, and index dates from potential cases were then randomly assigned over the pool of potential controls before matching.
Outcome measures
Healthcare resource utilization for cases (HZ diagnosis) and matched controls (without HZ diagnosis) was measured during the 21 days prior to index through the 12-month observation period (i.e. from index date −21 to index date +364). Specific utilization measures included inpatient admissions, emergency room (ER) admissions, outpatient office visits, and other outpatient services and were presented by age group in years (<50, 50–59, 60–64, 65–69, 70–79, 80+). The sub-set of cases with PHN was examined separately but over the same utilization categories.
Total healthcare costs, regardless of the reason for the hospitalization or visit, were measured during the 21 days prior to the index date through the 12-month observation period. Costs were segmented by inpatient admissions, ER visits, outpatient office visits, other outpatient services (e.g. lab and radiological services), and outpatient pharmacy and were presented by age group (< 50, 50–59, 60–64, 65–69, 70–79, 80+). The sub-set of cases with PHN was examined separately but over the same category of costs. Cost estimates were based on paid amounts of adjudicated claims, including insurer and health plan payments, co-payments, and deductibles. All costs were inflated to 2013 dollars based on the Medical Care Services component of the Consumer Price IndexCitation21.
Analysis
Standardized differences, which are used to quantify the statistical significance of differences independent of sample size, were calculated to examine the quality of the match between HZ cases and controls. Based on a prior work, it is considered a good match when the absolute value of standardized difference is less than 10% for the majority of matching factorsCitation22. All study variables, including demographic characteristics, clinical factors, healthcare utilization, and costs for each study cohort (HZ without PHN, HZ with PHN, all HZ, Matched Controls) were analyzed descriptively. For each category of included costs, means and standard deviations (SD) were presented for HZ patients and matched controls along with the difference in average costs, which represents incremental cost. Similarly, counts of resource utilization events were categorized and populated in the same manner as costs; t-tests were used to test for significant differences between the case and control groups. A p-value of <0.05 was considered statistically significant.
Results
Patient population
A total of 98 916 immunocompetent HZ patients were matched (1:1) to an identical number of immunocompetent control patients without HZ. HZ patients had a mean age (standard deviation) of 50.4 (18.8) years, 56.6% were female, and the majority (81%) were commercially insured. The cohorts were well balanced with regard to age, gender, payer, health plan type, population density, employee relationship, CCI, and pre-period expenditures after matching (standardized difference <10%; ).
Table 1. Demographics and baseline clinical characteristics of all study cohorts.
Within the main study population, a sub-set of 2405 subjects with PHN was directly matched to immunocompetent controls. Among all cases with HZ, those with PHN were older, composed of more females, and had a higher percentage covered by Medicare than those without PHN. Additionally, a higher percentage of PHN patients had a noticeably higher CCI and pre-period expenditures than their counterparts without PHN ().
Healthcare resource utilization and costs
Compared to matched controls, immunocompetent patients with HZ had significantly higher healthcare resource utilization during the 1-year observation period in all resource categories (inpatient admissions, ER visits, outpatient office visits, and other outpatient services). Measured among all patients, incremental healthcare resource utilization for HZ was 0.016 inpatient visits (95% CI = 0.013–0.018), 0.153 ER visits (95% CI = 0.146–0.159), 2.116 outpatient office visits (95% CI = 2.077–2.155), and 3.730 other outpatient services (95% CI = 3.525–3.935), all p < 0.01. With few exceptions, the incremental impact of HZ in all utilization categories increased with advancing age throughout the 1-year observation period across all HZ patients ().
Table 2. Annual incremental healthcare utilization associated with herpes zoster stratified by PHN status and age category.
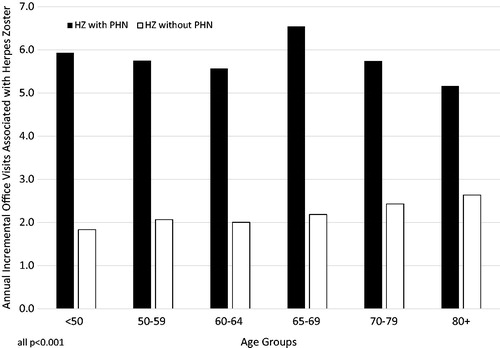
The incremental healthcare resource utilization attributable to HZ in each category increased substantially for patients with PHN (). The rate of other outpatient services was significantly higher in the PHN cohort, regardless of age, averaging over 10 claims for services throughout the year following diagnosis. Moreover, the average incremental count of outpatient office visits for PHN patients were at least double the values for those patients without PHN in nearly all age-groups ().
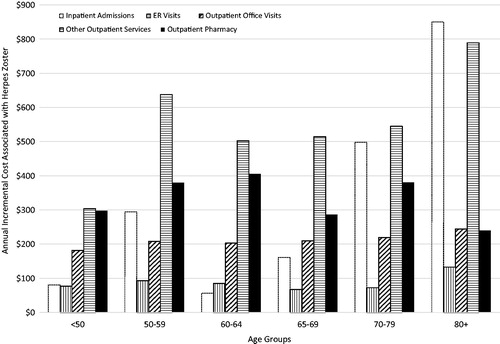
Figure 1. Annual incremental cost associated with herpes zoster by healthcare resource utilization category.
Across all HZ subjects, the mean incremental healthcare cost for immunocompetent individuals with HZ was $1308 (95% CI = $1184–$1433) and $5463 (95% CI = $4505–$6420) when PHN was present (both p < 0.001; ). Across categories of healthcare utilization, the incremental cost associated with HZ varied considerably. Among all patients with HZ, other outpatient services ($474, 95% CI = $422–$525) and pharmacy costs ($335, 95% CI = $311–$360) were the primary cost drivers, making up 62% of the total incremental cost. Incremental costs of care for HZ patients were observed to be similar among inpatient admissions ($216, 95% CI = $124–$307) and office visits ($199, 95% CI = $195–$204) and were $84 (95% CI = $77–$92) for ER visits ().
Figure 2. Annual incremental office visits associated with herpes zoster by PHN status and age group.
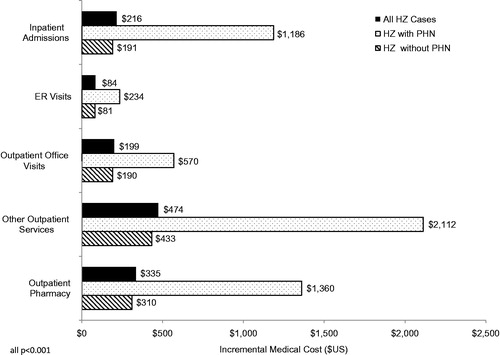
Table 3. Annual incremental healthcare cost associated with herpes zoster stratified by PHN status and age category.
For HZ patients with PHN, the incremental cost for inpatient admissions were over 6-times that of patients without PHN. Incremental outpatient pharmacy costs quadrupled, other outpatient services nearly quintupled, and ER and office visits nearly tripled in the presence of PHN (); all categorical comparisons to matched controls, regardless of timeframe, were statistically significant (p < 0.0001).
Significant incremental costs were observed between patients with HZ compared to matched controls in all age groups. Differences in average total costs across all HZ patients, as well as in those with PHN, increased with age but noticeably dipped in subjects aged 60–64 and 65–69 and then increased at age 70, with peak costs observed in HZ patients aged ≥80 years (). Similarly, healthcare costs steadily increased with age in HZ patients with PHN, with only a singular dip in those aged 65–69 years (not shown). When stratified by age and utilization category, the average incremental costs attributable to HZ for all medical services increased with age. However, incremental outpatient pharmacy costs showed a monotonically increasing trend with age until subjects reached age 65. By and large, significantly higher incremental costs were observed in immunocompetent HZ patients across age groups and all categories of costs; however, inpatient admissions costs were fairly inconsistent, reaching significance for all but those aged <50 and 60–69 ().
Discussion
This study provides an update on direct medical costs associated with HZ from a nationally-representative administrative US database from 2008–2011, after the availability of zoster vaccine live. We found that during the 1-year +21-day observation period, the incremental healthcare cost was $1308 in patients with HZ, which more than quadrupled in HZ patients with PHN ($5463).
Our results are consistent with previous published studies (all dollars converted to 2013 $US). In their population-based study, Yawn et al.Citation5 estimated 1-year costs to be $910 for those without PHN to $5548 for those with PHN. Similarly, in their studies of administrative claims, Dworkin et al.Citation11 and White et al.Citation15 and their respective colleagues reported average 1-year incremental costs of $1793 and $1152 in HZ patients without PHN and $5826 and $4455 for those with PHN, respectively. Total healthcare costs incurred by patients with HZ and the sub-set of patients with PHN increased in patients of nearly all age groups. Comparably, the average healthcare cost for HZ treatment was estimated to range from $567Citation14 to $1406Citation5 over the initial 90 days and from $1129 to $1782 over the first year following diagnosisCitation5,Citation11,Citation15. Among a sub-set of patients with PHN, the average per patient healthcare expenditure ranged from $3016 to $5548 in the year after diagnosisCitation5,Citation11,Citation15. Our results for resource utilization were also similar to what was previously observed. In this study, incremental healthcare utilizations associated with HZ were 2.12 outpatient office visits, 0.15 ER visits, and 0.016 inpatient admissions. Previously, White et al.Citation15 reported 2.14 outpatient visits, 0.137 ER visits, and 0.028 inpatient admissions over a 1-year follow-up period.
When stratified by utilization categories, the costs of care at the 1-year observation period were significantly higher in HZ patients presenting with PHN compared to HZ patients without PHN. While other outpatient services and pharmacy costs accounted for the major proportion of incremental costs in both the cohorts, inpatient hospitalization costs contributed significantly to the incremental costs of HZ patients with PHN. These results are consistent with a previous study in which it was noted that outpatient visits and prescription drugs were the major cost drivers in patients with HZ and hospitalization costs had a substantial share in the overall cost of HZ patients with PHNCitation5. In the present study, incremental costs of outpatient pharmacy and visits increased substantially with age among patients with HZ. Among HZ patients with PHN, incremental outpatient pharmacy costs increased markedly with age. A similar but less obvious trend was observed in the cost of care of all other healthcare resource utilization.
Data from the current study suggest that, while ACIP does not currently recommend the vaccination of adults 50–59 years of age, HZ patients in this age range have a substantial stake in the overall economic burden of HZ. In the current analysis, we found that ∼25% of HZ cases occurred in adults aged 50–59 and these patients were found to incur higher incremental costs (US$1614) than those in older reported age groups (other than those aged greater than 70 years). While the current study found significant economic burden associated with herpes zoster in patients aged 50 years and greater, estimates from a cost-effectiveness analysis by Rothberg et al.Citation23 demonstrated significant variability by age.
The findings in this study are subject to potential limitations. First, this study was limited to only those individuals in the US with commercial health coverage or private Medicare supplemental coverage; therefore, results of this analysis may not be generalizable to HZ patients outside of the US, with other health insurance or without coverage. Second, because paid claims were analyzed, the impact of the incremental cost attributable to HZ in those aged 65 years and older with Medicare supplemental insurance may be artificially diminished when compared to the incremental cost attributable to HZ in those aged <65 with commercial insurance. Third, there was potential for misclassification of HZ, covariates, or study outcomes as patients were identified through administrative claims data as opposed to medical records. PHN was identified using a previously published algorithm used in administrative claims rather than medical records, and, therefore, patients with PHN may have been misclassified as HZ without PHN and vice versa. Also, in some cases PHN can last for more than 1 year and other complications due to HZ are possible; therefore, our results may under-estimate the true costs related to HZ in an immunocompetent population. In addition, the look back for evidence of zoster vaccine live in the study population was 1 year; therefore, it is possible that some of the patients analyzed in this study were vaccinated prior to the 1 year look-back period. As with any claims databases, the MarketScan Research Databases rely on administrative claims data for clinical detail, and these data are subject to coding limitations and entry error. However, previous studies found that the positive predictive value of ICD-9-CM codes for HZ in administrative claims data was relatively high, ranging from 84–94%Citation24–26.
Conclusions
The findings of the current study demonstrate that HZ is a significant economic and resource burden on the US healthcare system among immunocompetent patients of nearly all ages and increases greatly when complicated by PHN. Further emphasis on vaccination against HZ should be considered to help alleviate this medical burden.
Transparency
Declaration of funding
This manuscript and the work described herein was funded by Merck & Co., Inc.
Declaration of financial/other relationships
Truven Health Analytics provides study design, programming, analysis, and manuscript development for major pharmaceutical and biotech firms. BHJ, LP, and GL are employees of Truven Health Analytics. JG was an employee of Truven Health Analytics at the time of the study and manuscript preparation. KK was a consultant working for Merck & Co., Inc. at the time of the study and manuscript preparation; and CJA is an employee of Merck & Co. Inc. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgment
The authors wish to acknowledge Santosh Tiwari for his editorial contribution to this study.
Notes
†ZOSTAVAX is a registered trademark of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Whitehouse Station, NJ.
‡MarketScan is a registered trademark of Truven Health Analytics.
References
- Thomas SL, Hall AJ. What does epidemiology tell us about risk factors for herpes zoster? Lancet Infect Dis 2004;4:26-33
- Brisson M, Edmunds WJ, Law B, et al. Epidemiology of varicella zoster virus infection in Canada and the United Kingdom. Epidemiol Infect 2001;127:305-14
- Schmader K. Herpes zoster in older adults. Clin Infect Dis 2001;32:1481-6
- Department of Health and Human Service. Centers for Disease Control and Prevention. Shingles (Herpes Zoster). Atlanta, GA, 2014 http://www.cdc.gov/shingles/about/overview.html. Accessed April 10, 2013
- Yawn BP, Itzler RF, Wollan PC, et al. Healthcare utilization and cost burden of herpes zoster in a community population. Mayo Clin Proc 2009;84:787-94
- Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 2005;352:2271-84
- Jung BF, Johnson RW, Griffin DR, et al. Risk factors for postherpetic neuralgia in patients with herpes zoster. Neurol 2004;62:1545-51
- Scott FT, Johnson RW, Leedham-Green M, et al. The burden of herpes zoster: a prospective population based study. Vaccine 2006;24:1308-14
- Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 2007;82:1341-9
- Katz J, Cooper EM, Walther RR, et al. Acute pain in herpes zoster and its impact on health-related quality of life. Clin Infect Dis 2004;39:342-8
- Dworkin RH, White, R, O’Connor AB, et al. Healthcare costs of acute and chronic pain associated with a diagnosis of herpes zoster. JAGS 2007;55:1168-75
- Drolet M, Brisson M, Schmader KE, et al. The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. Can Med Assoc J 2010;182:1731-6
- Johnson RW, Bouhassira D, Kassianos G, et al. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med 2010;8:37
- Insinga RP, Itzler RF, Pellissier JM. Acute/subacute herpes zoster: healthcare resource utilisation and costs in a group of US health plans. Pharmacoeconomics 2007;25:155-69
- White RR, Lenhart G, Singhal PK, et al. Incremental 1-year medical resource utilization and costs for patients with herpes zoster from a set of US health plans. Pharmacoeconomics 2009;27:781-92
- Schmader KE, Levin MJ, Gnann JW, JR., et al. Efficacy, safety, and tolerability of herpes zoster vaccine in persons aged 50-59 years. Clin Infect Dis 2012;54:922-8
- Harpaz R, Ortega-Sanchez IR, Seward JF; Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC). Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2008;57:1-30
- Hales CM, Harpaz R, Ortega-Sanchez I, et al. Update on recommendations for use of herpes zoster vaccine. MMWR 2014;63:729-31
- Langan SM, Smeeth L, Margolis JM, et al. Herpes zoster vaccine effectiveness against incident herpes zoster and post-herpetic neuralgia in an older US Population: a cohort study. PLoS 2013;10:1-11
- Klompas M, Kulldorff M, Vilk Y, et al. Herpes zoster and postherpetic neuralgia surveillance using structured electronic data. Mayo Clin Proc 2011;86:1146-53
- Bureau of Labor Statistics (BLS). United States Department of Labor, US Bureau of Labor Statistics, Division of Consumer Prices and Indexes Washington DC, 2014 http://www.bls.gov/cpi/. Accessed July 2014
- Ho DE, Imai K, King G, et al. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis 2007;15:199-236
- Rothberg MB, Virapongse A, Smith KJ. Cost-effectiveness of a vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. Clin Infect Dis 2007;44:1280-8
- Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc 2009;84:274-80
- Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613-9
- Yawn BP, Wollan P, St. Sauver J. Comparing shingles incidence and complication rates from medical record review and administrative database estimates: How close are they? Am J Epidemiol 2011;174:1054-61