Abstract
Objective: The objective of this study was to compare the cost of radiofrequency (RF) ablation vs cryoablation (Cryo) for atrial fibrillation (AF).
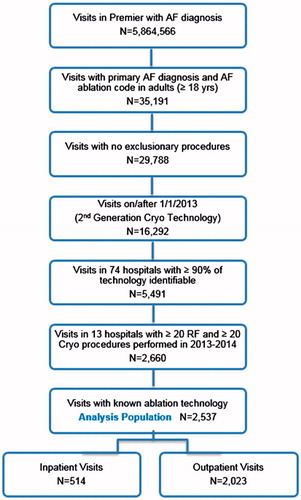
Methods: This retrospective cohort study used 2013–2014 records from the Premier Healthcare Database for adults with AF catheter ablation. Exclusions included non-AF ablation, surgical ablation, valve replacement or repair, or cardiac implant. Hospitals were required to perform ≥20 procedures using each technology, with the technology identifiable in at least 90% of cases. The primary endpoint was total variable visit cost, modeled separately for inpatient and outpatient visits, and adjusted for patient and hospital characteristics. Technology was categorized as RF or Cryo, with dual-technology procedures classified as Cryo. The Cryo cohort was further divided into Cryo only and Cryo with RF for sensitivity analyses. A composite adverse event endpoint was also compared.
Results: A total of 1261 RF procedures and 1276 Cryo procedures, of which 500 also used RF, met study criteria. RF patients were slightly older and sicker, and had more cardiovascular disease and additional arrhythmias. Adjusted inpatient costs were $2803 (30.0%) higher for Cryo, and adjusted outpatient costs were $2215 (19.5%) higher. Sensitivity models showed higher costs in both Cryo sub-groups compared with RF. Procedural complication rates were not significantly different between cohorts (p-values: 0.4888 inpatient, 0.5072 outpatient).
Conclusion: AF ablation using RF results in significantly lower costs compared with Cryo, despite an RF population with more cardiovascular disease. This saving cannot be attributed to a difference in complication rates.
Introduction
Atrial fibrillation (AF) affects 3–5 million Americans, and the incidence and prevalence are increasingCitation1,Citation2. While the overall prevalence has been reported at ∼1%, the rate is significantly higher in elderly patients, ranging from 0.1% in patients <55 years of age to 9% in patients 80 years of age or olderCitation2,Citation3. Many patients who develop AF also have co-morbid conditions, such as diabetes, hypertension, and structural heart diseaseCitation4,Citation5.
Since its initial description in the late 1990s, catheter ablation for AF has grown into an effective and important treatment option for many patients. Current consensus guidelines support the use of catheter ablation as second-line therapy in patients who do not respond to or cannot tolerate anti-arrhythmic drugs, and recent studies have also demonstrated the efficacyCitation6–8 and cost-effectivenessCitation9 of catheter ablation as a first-line intervention for AF. These data, and the results of other randomized controlled trials, support the efficacy and overall safety of catheter ablation for AF.
Radiofrequency (RF) ablation was the first FDA-approved procedure for the treatment of paroxysmal atrial fibrillation (PAF) in February 2009. Cryoablation (Cryo) was then granted FDA approval in December 2010 for the treatment of PAF. Several studies have shown shorter procedural times in Cryo vs RF, but it is unknown whether this has any effect on procedural costCitation10–12. Little real-world evidence has been published on the comparative costs and complication rates of the two technologies.
The objective of this study was to use real-world evidence to quantify and compare variable costs, and to identify any difference in adverse event rates that could affect these costs, for atrial fibrillation (AF) ablation with RF or Cryo technology.
Methods
Data source
The Premier Healthcare Database was used as the data source for this study. This database contains complete utilization, cost of care, diagnosis, and procedure coding from more than 700 hospitals throughout the US. The data from which this study was derived includes over 6 million inpatient discharges and 50 million outpatient visits per year, representing 20% of all inpatient discharges in the US.
All data used to perform this analysis were de-identified and accessed in compliance with the Health Insurance Portability and Accountability Act. As a retrospective analysis of a de-identified database, the research was exempt from IRB review under 45 CFR 46.101(b)(4).
Inclusion and exclusion criteria
Any inpatient or outpatient hospital visits in the Premier database from January 1, 2013 through December 31, 2014 were eligible for inclusion. Only those visits beginning with 2013 were utilized in this study in order to capture the use of second generation cryoablation technology. Visits were required to include both a primary diagnosis of AF (International Classification of Diseases, Ninth Revision [ICD-9] code 427.31) and either a CPT procedure code for AF catheter ablation (93651, 93656, and/or 93657) or an ICD-9 code 37.34 for catheter ablation without a non-AF CPT ablation code (93652–93655). The patient was required to be 18 years of age or older at the time of the visit. Visits were excluded if procedure codes were also present for AV node ablation, valve replacement or repair, cardiac implant (new or replacement), surgical ablation, or surgical left atrial appendage exclusion. See the Appendix for a complete list of these procedure codes.
From the group of all ablation visits that met the above inclusion and exclusion criteria, associated hospitals were required to meet additional inclusion criteria in order for the visits to be included in the analysis population. The first criterion was a minimum of a 90% identification rate for the type of ablation technology used in the procedures. The purpose of this criterion was to provide confidence in the cohort classifications. A minimum of 20 procedures using each technology was also required. This purpose of this criterion was to ensure the inclusion of centers experienced in both technologies.
Cohort definitions
All patient visits meeting the inclusion criteria were stratified into two primary cohorts based on the technology used for their AF ablation (RF or Cryo), as identified through charge descriptions in the Premier database. Visits with dual technology utilization were categorized as Cryo, since the cryoballoon is designed only for pulmonary vein isolation (PVI), suggesting that Cryo was the primary modality. Visits using only RF technology included PVI ablation with and without additional ablations.
Sensitivity analyses utilized a 3-category classification (RF, Cryo only, Cryo with RF) to distinguish Cryo patients having only PVI without the need of RF touch-up or additional lesion sets, as evidenced by the lack of RF usage, and patients with additional RF touch-ups or lesion sets, as evidenced by the utilization of dual technology. The RF cohort could not be similarly sub-divided since additional ablations would not necessitate a change in technology.
It should be noted that, due to the timeframe of the data used in this study, patients with AF were identified via a single ICD-9 code that did not allow differentiation of sub-groups with paroxysmal vs persistent AF. Only after a sufficient sample of data becomes available for the time period following the late 2015 ICD-10 coding adoption will it be possible to make this distinction in a hospital database.
Statistical analyses
The primary outcomes of interest for this study included variable hospital costs for the ablation visit (medication, supplies, and procedure costs) and a composite adverse event. Fixed costs, i.e. overhead, were summarized but not included in statistical models, as they would only be minimally impacted by differences in treatments. The composite adverse event was defined as the occurrence of any one or more diagnosis from a comprehensive list of potentially serious procedure-related events including cerebrovascular events, acute myocardial infarction, pericardial events, vascular access events, respiratory complications, phrenic nerve damage, bleeding, post-operative fistula, infection, and sedation complications. The appendix gives a complete listing of these events, with the corresponding diagnosis codes used for identification.
Patient characteristics and unadjusted costs associated with the ablation visit were stratified and summarized by each technology cohort and sub-cohort (RF, all Cryo, Cryo only, Cryo with RF) as well as inpatient vs outpatient status. Patient characteristics were summarized with percentages, while costs were summarized with medians, means, and standard deviations.
Statistical models
Generalized linear regression models with log links and gamma distributions were used to assess the impact of technology cohort on the variable hospital costs, while adjusting for statistically significant patient and hospital characteristics. Separate models were constructed for inpatient and outpatient visits. Logistic regression models were similarly developed for inpatient and outpatient visits to model the risk of incurring a composite adverse event, with the primary independent variable of interest being the technology cohort. All primary analysis models utilized the full RF vs Cryo cohorts, where both cohorts included patients with and without additional RF lesions for AF ablation touch-up or for additional arrhythmias. Sensitivity models were constructed similarly, but with the Cryo cohort divided into sub-groups of patients who received either Cryo only or Cryo with RF.
Results
A total of 2537 procedures (514 inpatient and 2023 outpatient) were identified in 13 hospitals that met the study criteria for the analysis population (). The allocation of procedures by cohort was 1261 RF and 1276 Cryo, with the Cryo cohort comprised of 60.8% (776 patients) having Cryo ablation only and 39.2% (500 patients) requiring additional RF ablations. The number of Cryo procedures was higher in 2014 than 2013 for both the inpatient and outpatient settings, whereas the number of procedures using RF increased in the outpatient setting while decreasing in the inpatient setting. RF patients were slightly older and had more coronary artery disease and chronic ischemic heart disease, across both inpatient and outpatient settings, than the Cryo patients, while the Cryo patients had more hypertension and obesity. Within the inpatient visits, the RF patients had higher severity disease status, more heart failure, and more diabetes than the Cryo cohort. RF patients were more likely to have additional arrhythmias, regardless of the setting, as would be expected since these arrhythmias could necessitate RF ablation ().
Table 1. Patient characteristics (n = 2537 visits).
Unadjusted variable costs for the analysis population of ablation visits are higher for the Cryo cohort and both Cryo sub-groups than for the RF cohort across both inpatient and outpatient settings. The primary comparator cohorts show median cost savings of $4830 inpatient and $1714 outpatient, and mean cost savings of $4342 inpatient and $1692 outpatient, for RF vs Cryo. Within the Cryo cohort, the sub-group of patients who also require RF have increased inpatient costs compared with patients who do not (median increase = $1929, mean increase = $3327), but outpatient differences are smaller and are bidirectional (median increase = $684, mean decrease = $706). Fixed costs follow similar patterns in the inpatient setting, but with lower cost differentials, and are similar across cohorts in the outpatient setting. Total costs, being the sum of fixed and variable costs, follow the same patterns as variable costs, with larger cost differentials ().
Table 2. Hospital costs, unadjusted (n = 2537 visits).
Adjusted variable cost estimates from the multivariable regression models are displayed in . Adjusted mean costs were higher in the Cryo cohort than in the RF cohort by 30.0% ($2803) in the inpatient setting and 19.5% ($2215) in the outpatient setting. In both hospital settings, having additional arrhythmia(s) was the most significant patient characteristic contributing to the cost adjustments (p-values =0.0003 inpatient, 0.0017 outpatient). In addition, hospital characteristics strongly influenced costs, with p-values ranging from <0.0001 to 0.0047 for the various hospital metrics in the two primary models ().
Table 3. Variable cost models with adjusted costs (n = 2537 visits).
The cost estimates from the sensitivity models, which sub-divided the Cryo cohort into Cryo only and Cryo with RF, are also shown in . These models indicate that, even in the absence of additional RF lesions, ablation with Cryo only (i.e. with PVI ablation only) is costlier than in the RF population, which includes patients with and without additional lesion sets. The adjusted mean cost increase for the Cryo only sub-group over the RF cohort is 16.9% ($1544) for inpatients and 14.9% ($1693) for outpatients. The sub-group having Cryo with RF is the costliest, with adjusted mean cost increases of 50.7% ($4647) for inpatients and 28.5% ($3227) for outpatients compared to RF ().
Composite adverse event rates, adjusted for significant patient and hospital characteristics, were similar among cohorts in both the inpatient and outpatient settings (p-values =0.4888 inpatient, 0.5072 outpatient). Although not the primary focus of this study, adverse events can have a substantial impact on the cost of a procedure, thus it was important to understand whether there was a differential event rate that could have contributed significantly to the differences in costs between cohorts.
Discussion
RF ablation has long been a second-line treatment for AF, with more recent studies focused on evaluating the benefits of its use as a first-line optionCitation13,Citation14. Cryoablation is a newer alternative that has been gaining in popularity. Both RF and Cryo ablations have been shown to be safe and effective treatments for paroxysmal AF, compared with drug therapyCitation15,Citation16.
Although Markov models have been utilized to demonstrate the cost-effectiveness of each technology in the treatment of paroxysmal atrial fibrillationCitation9,Citation17, direct comparisons of the procedural costs for AF ablation with RF vs Cryo are lacking. One early study showed a $7000 increase in procedural cost to the hospital for Cryo over RF, but this represented the experience of only a single site that was new to CryoCitation18.
Our study represents a first attempt to understand the real-world cost differential of Cryo vs RF by comparing hospital costs of ablation visits in 13 hospitals that routinely perform both procedures. We found that adjusted inpatient costs were 30.0% ($2803) higher for Cryo and adjusted outpatient costs were 19.5% ($2215) higher. A large proportion of the Cryo patients (39.2%) also required additional RF ablation. The real-world mix of patients with PVI only and patients with additional ablation is reflected in both the Cryo cohort and the RF cohort, although it is unknown whether the RF cohort had proportions similar to the Cryo cohort. ICD-9 coding did not allow us to distinguish paroxysmal vs persistent AF, but we did see that the RF cohort had more additional arrhythmias than the Cryo cohort (51% vs 40% inpatient, 42% vs 32% outpatient). They were also sicker on the whole, with 23% vs 13% of the inpatients at an APR-DRG severity level of 3 or 4, and had more cardiovascular disease, including heart failure, valvular disease, coronary artery disease, and chronic ischemic heart disease.
The large sample size of 2537 procedures allowed for separate analysis of inpatient and outpatient visits, which may represent fundamentally different patient populations. In addition, the size allowed us to analyze sub-groups within the Cryo cohort to estimate cost differences between patients requiring additional RF ablation and those not requiring RF. Unfortunately, it was not possible to similarly sub-divide the RF cohort into those patients with PVI only and those with additional ablations. The primary cost comparison representing the overall technology-related difference is that between the RF cohort and the entire Cryo cohort, since both of these populations are comprised of patients receiving PVI for PAF alone and patients receiving additional lesions for AF or for additional arrhythmias.
Due to the dependence on hospital administrative data, this study had some noteworthy limitations. In particular, many hospitals reported only non-specific wording for ablation catheters such that the type of technology was indeterminate. Similarly, it was not possible to determine the exact device(s) used for a particular procedure. Although each site was required to perform at least 20 procedures with each technology over the study period, the experience of individual operators was not known. As stated previously, the ICD-9 diagnosis coding available in this dataset did not allow for differentiation of paroxysmal vs persistent AF. Finally, there were several limitations related to the acute nature of the data, including the inability to distinguish index ablation procedures from repeat ablations and the inability to compare long-term treatment costs, including costs associated with repeat ablations.
Despite these limitations, this study had some important strengths, including the prospectively-developed protocol that directed the analysis, the large sample size, and utilization of multiple sites that routinely use both technologies. The results are a real-world representation of the patient population receiving AF ablation, the experience level of the operators performing the ablations, and the mix of devices used within the study period. The data source also allowed us to compare costs that encompassed all associated differences between treatments, including any differential costs associated with procedural complications. Ultimately, it is unlikely that there was any significant cost difference attributable to complications, since the overall rates were not significantly different among cohorts. This finding is consistent with prior studies that also found equal overall complication rates in RF and Cryo procedures, with higher rates of phrenic nerve palsy in Cryo and higher rates of some other complications in RFCitation19–21.
Conclusion
AF ablation with RF results in significantly lower hospital costs compared with second generation Cryo. These cost differences are sustained when Cryo is used without further need of RF, are increased with the use of dual technologies, and do not appear to be influenced by differential adverse event rates.
Transparency
Declaration of funding
This study was funded by Biosense Webster, Inc. The publication of study results was not contingent on the sponsor’s approval or censorship of the manuscript.
Declaration of financial/other relationships
TDH and SRP are employees of, and JAR is a consultant to, CTI Clinical Trial and Consulting Services, Inc., which is a paid consultant to Biosense Webster, Inc. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Appendix.docx
Download MS Word (14.3 KB)Acknowledgement
An abstract was presented at the The Heart Rhythm Society's Annual Scientific Sessions, May 4–7, 2016. No assistance in the preparation of this article is to be declared.
References
- Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370-5
- Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 2006;114:119-25
- Naccarelli GV, Varker H, Lin J, et al. Increasing prevalence of atrial fibrillation and flutter in the United States. Am J Cardiol 2009;104:1534-9
- Benjamin EJ, Levy D, Vaziri SM, et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994;271:840-4
- Levy S, Maarek M, Coumel P, et al. Characterization of different subsets of atrial fibrillation in general practice in France: the ALFA study. The College of French Cardiologists. Circulation 1999;99:3028-35
- Camm AJ, Lip GY, De Caterina R, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation–developed with the special contribution of the European Heart Rhythm Association. Europace 2012;14:1385-13
- Khan AR, Khan S, Sheikh MA, et al. Catheter ablation and antiarrhythmic drug therapy as first- or second-line therapy in the management of atrial fibrillation: systematic review and meta-analysis. Circ Arrhythmia electrophysiol 2014;7:853-60
- Wazni OM, Marrouche NF, Martin DO, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA 2005;293:2634-40
- Aronsson M, Walfridsson H, Janzon M, et al. The cost-effectiveness of radiofrequency catheter ablation as first-line treatment for paroxysmal atrial fibrillation: results from a MANTRA-PAF substudy. Europace 2015;17:48-55
- Ciconte G, Baltogiannis G, de Asmundis C, et al. Circumferential pulmonary vein isolation as index procedure for persistent atrial fibrillation: a comparison between radiofrequency catheter ablation and second-generation cryoballoon ablation. Europace 2015;17:559-65
- Hunter RJ, Baker V, Finlay MC, et al. Point-by-Point radiofrequency ablation versus the cryoballoon or a novel combined approach: a randomized trial comparing 3 methods of pulmonary vein isolation for paroxysmal atrial fibrillation (The Cryo Versus RF Trial). J Cardiovasc Electrophysiol 2015;26:1307-14
- Straube F, Dorwarth U, Ammar-Busch S, et al. First-line catheter ablation of paroxysmal atrial fibrillation: outcome of radiofrequency vs. cryoballoon pulmonary vein isolation. Europace 2016;18;368-75
- Cosedis Nielsen J, Johannessen A, Raatikainen P, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med 2012;367:1587-95
- Morillo CA, Verma A, Connolly SJ, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): a randomized trial. JAMA 2014;311:692-700
- Packer DL, Kowal RC, Wheelan KR, et al. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STOP AF) pivotal trial. J Am Coll Cardiol 2013;61:1713-23
- Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA 2010;303:333-40
- Reynolds MR, Lamotte M, Todd D, et al. Cost-effectiveness of cryoballoon ablation for the management of paroxysmal atrial fibrillation. Europace 2014;16:652-9
- Mandell J, Amico F, Parekh S, et al. Early experience with the cryoablation balloon procedure for the treatment of atrial fibrillation by an experienced radiofrequency catheter ablation center. J Invasive Cardiol 2013;25:288-92
- Jourda F, Providencia R, Marijon E, et al. Contact-force guided radiofrequency vs. second-generation balloon cryotherapy for pulmonary vein isolation in patients with paroxysmal atrial fibrillation-a prospective evaluation. Europace 2015;17:225-31
- Schmidt M, Dorwarth U, Andresen D, et al. Cryoballoon versus RF ablation in paroxysmal atrial fibrillation: results from the German Ablation Registry. J Cardiovasc Electrophysiol 2014;25:1-7
- Squara F, Zhao A, Marijon E, et al. Comparison between radiofrequency with contact force-sensing and second-generation cryoballoon for paroxysmal atrial fibrillation catheter ablation: a multicentre European evaluation. Europace 2015;17:718-24