Abstract
Background and objective: Atrial fibrillation (AF) is a risk factor for acute ischemic stroke (AIS). In mainland China, little is known of the hospitalization expenses of AIS patients with AF compared to those with normal sinus rhythm (SR). This study compared the itemized expenses of AIS patients with or without AF in a hospital in Huizhou City.
Methods: Patients hospitalized for AIS from March 2014 to March 2015 were enrolled, including 73 with AF and 751 with normal SR. Stroke severity was scored using the National Institutes of Health Stroke Scale (NIHSS). Non-parametric statistical tests were used to determine differences in hospital expenses between the two groups, of which influencing factors were analyzed using single factor and multiple stepwise linear regression analyses.
Results: Medicine was the predominant expense during hospitalization of all AIS patients. Patients with AF incurred significantly higher expenses for medicine, bed, treatments, examinations, laboratory tests, and nursing than patients with normal SR (p < .05); however, the medicine and bed expenses of patients at the same stroke level in the two groups were similar. Independent factors influencing the higher costs of AF patients were hospital length of stay, pulmonary infection, urinary-tract infection, NIHSS scoring, gastrointestinal bleeding, and congestive heart failure (p < .05). Independent predictors of hospital length of stay were NIHSS scoring, pulmonary infection, and urinary-tract infection (p < .05).
Conclusion: AIS patients with AF incurred higher expenses during hospitalization compared with those with normal SR, due to greater stroke severity, higher rates of pulmonary infection and congestive heart failure, and longer hospital stays.
Introduction
Atrial fibrillation (AF) is a common sustained heart arrhythmia. The prevalence of AF in the general population significantly rises with ageCitation1, reportedly doubling with every decade after the age of 50 years, and up to 10% after 80 yearsCitation2. AF is also more prevalent in males than in femalesCitation3. The disease is not only a burden to the patients and their families, but also to the healthcare system; costs due to AF increased by almost 19% from 1990 to 2010Citation4.
AF is a proven independent risk factor for brain stroke, often leading to disability and deathCitation5. The percentage of AF patients suffering from related acute ischemic stroke (AIS) varies among countries, from 6–32%Citation1. Thus, AIS associated with AF is a public health problem worldwide. In Europe and America, the costs of stroke associated with AF include the direct costs of hospitalization, nursing fees after leaving the hospital, treatment fees after stroke recurrence, and costs of community medical care. These costs are higher for AIS patients with AF than without AFCitation6,Citation7.
There is little known of AF and stroke within the population of mainland China. Since the prevalence of AF varies among countries from 0.1–4%Citation1, an epidemiological survey of morbidity, treatment, and its consequent costs is urgently needed. The present study examined the effect of AF on expenses associated with AIS in mainland China, and investigated the application of oral anticoagulants as stroke prevention therapy.
Patients and methods
Ethics statement
The study was approved by the Ethics Committee of Huizhou City Central Municipal Hospital. Data were handled in a manner that did not reveal the identity of any patients or control subjects, so consent forms (written/oral) for individuals were not required.
Study design
Information was collected from the patients hospitalized for AIS from March 2014 to March 2015 in the Department of Neurology, Huizhou Municipal Central Hospital, Huizhou Hospital Affiliated to Guangdong Medical College. The selection of the samples mainly referred to related research articles and combined with the actual situation of our hospital. First, the expansion of the study span may introduce confounding factors, including monetary inflation, which may harm the representation of the study. Second, there is a unified clinical treatment standard of cerebral infarction in ChinaCitation8, by which the medicine cost of the patients are even. For analysis, these AIS patients were divided into two groups according to cardiac rhythm: those with AF (Group A) and those without AF but with normal sinus rhythm (SR; Group S). The itemized expenses for hospitalization of these two groups were compared.
Patients
Patients hospitalized with AIS and treated at the Departments of Neurology, Huizhou Municipal Central Hospital, Huizhou Hospital Affiliated to Guangdong Medical College between March 2014 and March 2015, were enrolled. This hospital is a third-class level-A hospital in Guangdong Province, serving nearly 4 million residents in its service area. According to hospital rank, third-class level-A is the top level in China.
All the patients met the definitive criteria for AIS in accordance with the neurology branch of the Chinese Medical Association (2010)Citation9, which are consistent with the criteria of the World Health Organization (1999)Citation10. The patients enrolled in this study had been admitted to the hospital within 1 week after the onset of the disease. In the AF patients, AF had been diagnosed by physician via electrocardiogram (ECG) and kept on record, or patients were found to have permanent, persistent, paroxysmal AF during hospitalization for AIS through ECG, ECG monitoring, or 24-h Holter monitor. The patients with normal SR were those with no record of AF 1 year before hospitalization for AIS and no appearance of AF during the hospitalization, but were determined to have normal SR on ECG examination, with the exclusion of any other sick sinus syndrome.
The data of Chinese patients with AIS should be reported monthly by third-class and second-class hospitals, according to the requirements of the Ministry of National Health and the China National Stroke Registry (2008)Citation8. Hence, to avoid the duplication of reports, the statistical results excluded patients transferred from second-class to third-class hospitals. In addition, patients who underwent stent implantation in the internal carotid artery, vertebral artery, or intracranial artery were excluded for several reasons. First, the stent implantation was not included in conventional emergency treatment of stroke, due to its belonging to the prevention treatment. Second, the implantation could not be carried out in most of the hospitals, making the exclusion of the operation expense representative in China. Third, the cost of stent implantation takes up most of the hospital expenses, which may result in great changes in the hospitalization costs.
Data collection
Information collected from the patients included gender, age, ethnicity, admission and discharge time, National Institutes of Health Stroke Scale (NIHSS) score, and past medical history. NIHSS scores were obtained in all the individuals by clinical physicians who admitted the patients. Past medical history of the patients included type 2 diabetes, hypertension, chronic kidney disease, hyperlipidemia, hyperuricemia, congestive heart failure and other complications, such as pulmonary infection, urinary tract infection, gastrointestinal (GI) bleeding, and others. A cranial computed tomography (CT) or magnetic resonance imaging (MRI) examination was performed for each patient.
In this study, the prices for chargeable services were in accordance with the standards for medical services in Huizhou (2014). Hospital expenses included the costs of bed, consultation, nursing, medicine, blood examination, CT, MRI, x-ray, ultrasound, ECG, oxygen, transfusion of blood or blood products, and decompressive craniotomy. The degree of stroke severity after admission were categorized according to NIHSS: mild, ≤8; moderate, 9–15; or severe, ≥16Citation11. The type and dosage of anticoagulants within 6 months prior to the stroke were recorded.
Statistical analyses
SPSS19 software was utilized for statistical processing. To study the difference in hospital expenses between patients with AF or normal SR, the characteristics of patients and the itemization of the costs were statistically described. The hospital expenses and stay duration are shown as the mean and standard deviation (mean ± SD). All cost data were originally calculated in Chinese Yuan (CNY) and presented in US dollars (exchange rate: 1 US$ = 6.2122 CNY; 30 March 2014). All continuous variables are not normally distributed (including age). So, non-parametric statistical tests were also used to compare the patient groups. Continuous variables were analyzed using a Mann-Whitney U-test, while binary variables were analyzed with a Chi-squared test. The factors influencing hospital costs and length of stay were analyzed by single factor analysis (rank correlation) and multivariate analysis (multiple stepwise linear regression). As the results of the analysis of hospital expenses and stay time were not normally distributed, they were, thus, transposed to natural logarithm values, to create normal distributions. The exclusion criteria for the variables in the linear model were p > .1. The inclusive standard was p < .05, as the statistical inspection level was p = .05.
Results
General situation
All patients including old stroke patients were admitted to our third-class hospital. The study enrolled 824 patients with AIS (average age = 64.7 ± 12.0 years), among which 73 (8.86%) patients had AF (Group A), and 751 (91.14%) had SR (Group S). The average age of patients with atrial fibrillation stroke is higher than that of the non-atrial fibrillation group (p < .001). Compared with Group S, patients in Group A had significantly longer hospitalizations (p = .006) (); Group A also had a significantly higher percentage of women (p = .01) and percentage of patients with moderate or severe stroke, pulmonary infection (p < .001), or congestive cardiac failure (p < .001).
Table 1. Demographic and clinical characteristics of the patients.
Hospital expenses
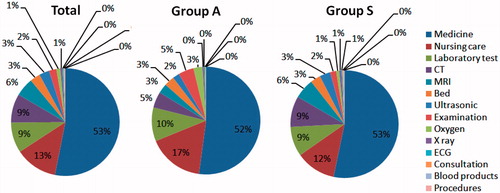
Overall, the medicine fees accounted for 52.9% of hospital expenses, and this was the highest single expense. For patients in Groups A and S, the percentages of total expense for drugs were 51.1% and 53.1%, respectively, and, thus, statistically comparable ().
Figure 1. Percentage of direct-cost components for patients with AF (Group A) or without AF (Group S). AF, atrial fibrillation; ECG, electrocardiogram; CT, computed tomography; MRI, magnetic resonance imaging.
When considering the entire study population, the average total hospital expense per patient was $2,393.66 ± 2,356.41; however, the average total expense for each patient in Group A ($4,054.11 ± 3,704.88) was significantly higher than that for patients in Group S ($2,341.98 ± 2,124.94; p < .001). Furthermore, the average costs for medicine (p = .001), bed (p = .001), consultation (p < .001), ECG (p < .001), oxygen (p < .001), examinations (p < .001), and nursing (p < .001) were all significantly higher in Group A than in Group S. However, after adjusting for NIHSS scoring, patients of both groups at similar stroke levels had similar total expenses for hospitalization, and for medicine and bed ().
Table 2. Hospitalization expenses of patients.Table Footnote*
Factors influencing hospital expenses
The single factor analysis showed that AF, hospitalization, pulmonary infection, congestive heart failure, chronic kidney disease, digestive tract bleeding, and NIHSS score were related to the cost of hospitalization (). Multiple stepwise linear regression analysis showed that hospital expenses were associated with the length of hospital stay (p < .001), pulmonary infection (p < .001), congestive heart failure (p = .016), urinary tract infection (p = .007), NIHSS score (p < .001), and GI bleeding (p = .014). These influential factors were associated with the natural logarithm value of hospital expenses in linear fitting (R2 = .645, ).
Table 3. Univariate analysis of hospital costs and hospital stay, correlation coefficients, r (p).
Table 4. Multivariate analysis of hospital costs and length of stay.
Factors influencing length of hospital stay
The average length of hospital stay for all patients was 11.5 ± 9.3 days, but significantly longer for Group A (14.9 ± 11.9 days) than Group S (11.2 ± 8.9 days, p = .006). Single factor analysis showed that age, pulmonary infection, AF, congestive heart failure, chronic kidney disease, GI bleeding, and NIHSS were associated with the length of hospital stay (). Multiple stepwise regression analysis showed that NIHSS score (p < .001), pulmonary infection (p < .001), and urinary tract infection (p = .036) influenced the length of hospital stay, although these factors were poorly associated with the natural logarithm value of hospitalization in linear fitting (R2 = .136; ).
Discussion
Prevalence of AIS with AF in China
AIS patients with AF usually experience long-term disability, with increased risk of death and medical expenses. A survey of the disease in mainland China is crucial for understanding its prevalence, to design treatment guidelines, and to perform stroke prevention for AF patients. In recent years, the prevalence of AF in AIS was reportedly 6.3–8.3%in ChinaCitation12. In the present study, it was 8.4%, which is significantly lower than the 24–37% in western countriesCitation13.
Medical records are important to support research on AIS patients with AF. For their research of AIS patients with AF, Ali et al.Citation14 considered patients’ histories of AF within 1 year before admission, prevalence described by community physicians, results of admitting ECGs, and AF newly diagnosed during the 3 months after admission. Reports from countries outside of China indicated that 8.3% of the patients with stroke were newly found to have AF during continuous ECG monitoring or on 24-h dynamic electrocardiogramCitation15. Eleven per cent of patients demonstrates AF within 1 month after admission via ECG monitoringCitation16. In the present study, 39 patients with a history of AF were found to have AF on admission, and AF was newly-diagnosed in 25 patients when admitted to the hospital. Four patients with a history of AF showed no AF on the ECG at admission, but were confirmed to have AF during continuous ECG monitoring or 24-h Holter ECG examination during hospitalization. The other five patients with a prior history of AF showed no AF on the admission ECG, but did so later on ECG monitoring or multiple ECG examinations.
Among the 73 patients with AF, 64 (87.7%) received diagnoses through routine ECG examination, revealing the lack of long-time monitoring in cardiac rhythm. Thus, there is a strong possibility of missed diagnosis.
Expenses associated with AIS in China
According to a survey carried out by the Chinese Ministry of National Health in 2003, the direct expenses of stroke patients were ¥19,595,000,000 ($3,154,277,067), with an additional ¥37,450,000,000 ($6,028,460,127) for outpatient and over-the-counter medical charges. These accounted for 6.52% of the medical expenses and 5.68% of the total health expenditures in China at that time. In addition, the direct medical costs of stroke patients increased by 18.04% from 1993 to 2003. This is greater than the increase in gross domestic product (8.95%) during the same periodCitation8.
Therefore, the Ministry of National Health in 2008 formulated a quality control standard for ischemic stroke/cerebral infarction, laying down a set of inspection items that includes blood tests, color Doppler ultrasound of the carotid artery, and neuroimaging. It stipulated that patients with indications of blood clots should be treated with alteplase or urokinase for thrombolysis, and they should be given antiplatelet and anticoagulant therapy when they have coagulation symptoms. The data of patients hospitalized with AIS, including total hospital expenses, should be reported monthly by all second- and third-class hospitals in China. Excluded from these reports are patients who undergo internal carotid artery, vertebral artery, or intracranial artery stent implantation and patients transferred from second-class to third-class hospitals. Hence, the diagnosis and treatment of AIS is strictly defined in second- and third-class hospitals throughout the country.
The costs of medicines in China are standardized nationally, and medical service charges are set by the provincial Department of Development and Reform, according to local economic levels. In particular, a national standard of medical service prices was developed by the National Development and Reform Commission, Ministry of National Health, and State Administration of Traditional Chinese Medicine in China. It was reported that the per capita hospital expense in one third-class hospital in Taiyuan City, Shanxi Province in 2011was ¥7,641.18 (∼$1,230.03)Citation17, and ¥18,242.65 (∼$2,936.58) in Peking University Third Hospital in Beijing in 2012Citation18. In our present study conducted in Huizhou City, the average per-patient cost was $2,493.66 ± 2,356.41. Thus, the hospital costs varied by location, indicating the regional differences in charges for bed, treatments, examinations, laboratory tests, and nursing.
In this study, the costs for medicine of the hospitalized AIS patients accounted for 53% of their total hospital expense. In particular, patients with AF spent a slightly higher percentage of their bills (53%) on medicine than did patients with normal SR (51%; p = .114). These percentages were consistent with the domestic reports of third-class hospitals in recent years (49.3–54.9%)Citation19, but much higher than the drug fees of AIS patients in western countries (3.1–7%)Citation6. The high percentage due to the costs of medicine in China could be one of the reasons. Besides, the hospitals must make a profit from the selling of drugs, due to inadequate subsidization from the government. The labor costs in China (doctor check-up, nursing, and rehabilitation) are lower than in developed countries, and therefore constitute a smaller portion of the total hospital expense. Moreover, Chinese patients favor using the maximum in dosages, because they believe that larger doses lead to quicker recovery. The application of traditional Chinese medicine is another reason for the higher total costs for medicine, which has been widely applied in the patients with AIS in mainland China. Of the Chinese patients who had stroke attack within 3 hours, 83.1% were given Intravenous injection of Chinese medicine, while 30.6% of the discharged patients were taking Chinese medicineCitation20,Citation21. Of note, the hospital expenses associated with AIS in western countries include charges for internal carotid artery stent implantation and internal carotid artery stenosis intimal dissection, which are extremely expensive. For example, in the UK per-patient charges for internal carotid artery stent implantation and internal carotid artery stenosis intimal dissection were £2,350 and £3,923, respectively (∼¥22,807 and ¥38,073) (∼$3,893.31 and $6,499.34, exchange rate: 1 US$ = €0.7275; March 31, 2014)Citation14. In our present survey, the average hospital expense of the patients with AIS increased to ¥80,680.85 ($12,987.48), due to the cost of the above interventional therapies (¥59,065.93; $9508.05). These two surgical procedures for AIS have become recommended in Europe and America in recent yearsCitation22,Citation23, and are now relatively common. However, in the latest version of AIS treatment guidelines in mainland China (2014) they were yet to be recommendedCitation24.
Comparison of expenses between AIS with AF and AIS with normal SR
The per capita hospital costs of AIS patients with AF have been reported to be higher than that of AIS patients with normal SR. For example, in the UK the total expenses of AIS associated with AF (£9,083 ± 7,381; ∼$15,048.05 ± 12,228.3) were 158.5% that of AIS with normal SR (£5,729 ± 6,071: p < .001; ∼$9,491.39 ± 10,057.99)Citation14. In Germany, the costs of AIS with AF were 133.8% that of AIS with normal SR (€11,799 ± €8,817; p < .001; ∼$16,218.56 ± $12,119.59, exchange rate: 1 US$ = €0.7275; March 31, 2014), and in the US they were 126.6% ($23,770 ± $18,779: p < .001)Citation7. Our present results revealed a similar pattern, namely that the total expenses of Group A (¥25,184.91 ± 23,015.44, $4,054.11 ± 3,704.88) were 173.1% that of Group S (¥14,548.85 ± 13,200.53; p < .001, $2,493.66 ± 2,356.41; p < .001). In particular, the patients with AF spent more in average expenses on medicines, bed, treatments, ECG examination, oxygen, laboratory tests, and nursing than did patients with normal SR (p < .001). However, after further stratifying the patients in two groups by stroke severity (NIHSS score), we found that the total hospital expenses of patients at the same stroke severity were not significantly different.
In the present study, the patients in Group A had higher NIHSS scores, longer average hospital stays, and a greater percentage with pulmonary infection or congestive heart failure than characterized by the AIS patients with normal SR. This indicates higher disease severity in the patients with AF. The poorer condition of these patients likely explains their higher hospital expenses compared with the patients with normal SR. Our results are in accord with the research conducted in most western countries that AF increases both the economicCitation25 and temporalCitation26 costs of AIS patients.
Furthermore, the multiple stepwise linear regression analysis of the present study showed that hospital stay, pulmonary infection, urinary tract infection, GI bleeding, NIHSS score, and congestive heart failure were independent predictors of hospital expenses of AIS patients; the latter two factors were also reported by Ali et al.Citation14. We found that AF was not an independent predictor of hospital expenses of AIS, which was not consistent with previous studiesCitation14,Citation27.
Various limitations characterize this study, including the lack of long-term monitoring of cardiac rhythm, and the small number of subjects in a single institution. The number of stroke patients with AF was relatively small in our hospital, owing to the ratio of these individuals in the patients with AIS. However, the amount of the stroke patients with AF was large in China, suggesting the importance of the survey. Although the samples being from a single hospital was one of the shortcomings in our studies, we consider it had a significance in this field. First, it was the first study for the treatment of acute ischemic stroke patients with atrial fibrillation and non-atrial fibrillation in Chinese mainland, which would provide reference data for domestic counterparts, in order to control medical costs, especially in medical burden. Second, the hospital was the first single disease quality control center in China, the treatment for stroke in which was in strict accordance with the country standard. Thus, the individual difference among the patients proved to be relatively small. Third, the data could provide a reference for the regional health insurance policy, which varied in different regions of China. Meanwhile, multiple factors may be introduced from the data during longer spans, including monetary inflation and other factors, resulting in poorly representative results. Thus, we choose a 1-year research period for this study, in order to be conducive to the decision-makers to make reasonable policy.
Conclusion
AIS patients with AF incurred significantly higher hospital expenses than did the AIS patients with normal SR, mainly because the former were more seriously ill, with a higher prevalence of pulmonary infection or congestive heart failure leading to longer average hospital stay. Medicine was the predominant cost of hospitalization to treat AIS in this study population. More research is needed to increase the understanding of the epidemiology of AIS with AF, and improve the management of future national healthcare in China.
Transparency
Declaration of funding
This study was not financially supported by any institution or sponsor.
Declaration of financial/other relationships
The authors report no conflicts of interst. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
This study was conducted according to the Ministry of Health “Involves people of biomedical research ethics review method (trial) (2007)”, and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. In this study the subjects’ rights and interests are fully protected.
References
- Rahman F, Kwan GF, Benjamin EJ. Global epidemiology of atrial fibrillation. Nat Rev Cardiol 2014;11:639-54
- Wolf PA. Awareness of the role of atrial fibrillation as a cause of ischemic stroke. Stroke 2014;45:e19-21
- Furberg CD, Psaty BM, Manolio TA, et al. Prevalence of atrial fibrillation in elderly subjects (the Cardiovascular Health Study). Am J Cardiol 1994;74:236-41
- Chugh SS, Roth GA, Gillum RF, et al. Global burden of atrial fibrillation in developed and developing nations. Glob Heart 2014;9:113-19
- Fuster V. Atrial fibrillation: an epidemiologic, scientific and clinical challenge. Nature Clin Prac Cardiovasc Med 2005;2:225
- Sussman M, Menzin J, Lin I, et al. Impact of atrial fibrillation on stroke-related healthcare costs. J Am Heart Assoc 2013;2:e000479
- Wang G, Joo H, Tong X, et al. Hospital costs associated with atrial fibrillation for patients with ischemic stroke aged 18-64 years in the United States. Stroke 2015;46:1314-20
- Department of Health Administration. Quality management manual of single disease. Scientific and Technical Documentation Press, China, 2008. p 122
- Writing group in cerebral vascular disease group of neurology branch of Chinese Medical Association. Treatment guidelines of acute ischemic stroke in China 2010. Chin J Neurol 2010;43:146-53
- MONICA Manual, Part IV:Event Registration. Section 2: Stroke event registration data component. Office of Cardiovascular Disease, World Health Organization; 1999[cite 16 Oct 2008]. Available from: http://www.ktl.fi/publications/monica/manual/part4/iv-2.htm.
- Muchada M, Rubiera M, Rodriguez-Luna D, et al. Baseline National Institutes of Health stroke scale-adjusted time window for intravenous tissue-type plasminogen activator in acute ischemic stroke. Stroke 2014;45:1059-63
- Feng HY, Wang XW. Risk and prognosis of cerebral infarction with atrial fibrillation. Chin J Prac Nerv Dis 2014;17:50-2
- Bang A, McGrath NM. The incidence of atrial fibrillation and the use of warfarin in Northland, New Zealand stroke patients. N Z Med J 2011;124:28-32
- Ali AN, Howe J, Abdel-Hafiz A. Cost of acute stroke care for patients with atrial fibrillation compared with those in sinus rhythm. Pharmacoeconomics 2015;33:511-20
- Rizos T, Güntner J, Jenetzky E, et al. Continuous stroke unit electrocardiographic monitoring versus 24-hour Holter electrocardiography for detection of paroxysmal atrial fibrillation after stroke. Stroke 2012;43:2689-94
- Flint AC, Banki NM, Ren X, et al. Detection of paroxysmal atrial fibrillation by 30-day event monitoring in cryptogenic ischemic stroke: the Stroke and Monitoring for PAF in Real Time (SMART) Registry. Stroke 2012;43:2788-90
- Liu L, Feng X. Analysis of hospitalization expenses among 7420 Cerebral infarction inpatints in general hospital. National Medical Frontiers of China; 2012;7:95-6
- Yu Wan JZ. Correlation factors of hospital stay and hospitalization costs among AIS patients. J Prac Med 2014;9:1420-3
- Wang D. Analysis on influential factors to the expenses of cerebral infarct patients. Hainan Med J 2012;24:118-20
- Yuan J, Zhu Y, Yao M, et al. Traditional Chinese medicine prescribed for acute stroke patients: a cross-sectional survey. Chin J Neurol 2015;48:284-7
- QUEST Group. Treatment of acute ischemic stroke in China. Chin J Neurol 2009;42:223-8
- European Stroke Organisation Executive Committee, ESOW. Guidelines for management of ischaemic stroke and transient ischaemic attack. Cerebrovasc Dis 2008;25:457-507
- Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:870-947
- Cerebral vascular disease group of neurology branch of Chinese Medical Association. Treatment guidelines of acute ischemic stroke in China 2014. Chin J Neurol 2015;48:246-57
- Casciano JP, Dotiwala ZJ, Martin BC, et al. The costs of warfarin underuse and nonadherence in patients with atrial fibrillation: a commercial insurer perspective. J Manag Care Pharm 2013;19:302-16
- Hannon N, Daly L, Murphy S, et al. Acute hospital, community, and indirect costs of stroke associated with atrial fibrillation: population-based study. Stroke 2014;45:3670-4
- Diringer MN, Edwards DF, Mattson DT, et al. Predictors of acute hospital costs for treatment of ischemic stroke in an academic center. Stroke J Cerebr Circ 1999;30:724-8
