Abstract
Aims: Diets high in saturated fat are associated with elevated risk of heart disease. This study estimates the savings in direct (medical care) costs and indirect (job absenteeism) costs in the US from reductions in heart disease associated with substituting monounsaturated fats (MUFA) for saturated fats.
Materials and methods: A four-part model of the medical care cost savings from avoided heart disease was estimated using data on 247,700 adults from the 2000–2010 Medical Expenditure Panel Survey (MEPS). The savings from reduced job absenteeism due to avoided heart disease was estimated using a zero-inflated negative binomial model of the number of annual work loss days applied to data on 164,577 adults from the MEPS.
Results: Estimated annual savings in medical care expenditures resulting from a switch from a diet high in saturated fat to a high-MUFA diet totaled ∼ $25.7 billion (95% CI = $6.0–$45.4 billion) in 2010, with private insurance plans saving $7.9 billion (95% CI = $1.8–$14.0 billion), Medicare saving $9.4 billion (95% CI = $2.1–$16.7 billion), Medicaid saving $1.4 billion (95% CI = $0.2–$2.5 billion), and patients saving $2.2 billion (95% CI = $0.5–$3.8 billion). The annual savings in terms of reduced job absenteeism ranges from a lower bound of $600 million (95% CI = $100 million to $1.0 billion) to an upper bound of $1.2 billion (95% CI = $0.2–$2.1 billion) for 2010.
Limitations: The data cover only the non-institutionalized population. Decreased costs due to any decreases in the severity of heart disease are not included. Cost savings do not include any reduction in informal care at home.
Conclusions: Diets high in saturated fat impose substantial medical care costs and job absenteeism costs, and substantial savings could be achieved by substituting MUFA for saturated fat.
Introduction
Heart disease is the leading cause of death in the US, responsible for 611,105 (or 23.5% of all) deaths in the US in 2013Citation1. Besides smoking, the greatest risk factors for heart disease are high blood pressure and elevated low density lipoproteins (LDL) cholesterol, both of which are related to poor dietary practicesCitation2. The World Health Organization reports that behavioral risk factors such as diet are responsible for 80% of cases of heart diseaseCitation3. More generally, a comprehensive study of the global burden of disease concluded that dietary risks were the largest contributors to disease burden, premature death, disability, and numbers of healthy years of life lost in the USCitation4.
In recent decades, research has documented that the type of fat one consumes has important implications for healthCitation5–17. Saturated fatty acids (SFA) are mostly from animal products (meat and dairy) and tropical oils (e.g. coconut, palm, cocoa). Unsaturated fats are mostly from plant products and include: (1) monounsaturated fatty acids (MUFA), which are found in canola, olives, nuts, and peanuts; and (2) polyunsaturated fatty acids (PUFA), which are found in safflower, sunflower, corn, soybean, and sesame, as well as seafood and nuts.
Even though all fats have nine calories per gram, they differ in their consequences for morbidity and mortality. In particular, consumption of saturated fat and trans fats is associated with heart diseaseCitation7,Citation8,Citation10,Citation12,Citation18–20. In contrast, consumption of unsaturated fats is associated with reduced risk of heart diseaseCitation5–7,Citation12,Citation21. One important mechanism is that replacing saturated fats with unsaturated fats lowers LDL-cholesterolCitation22. Based on this evidence, the US Departments of Agriculture and Health and Human Services (in the 2015–2020 Dietary Guidelines for Americans), the World Health Organization (WHO) and the American Heart Association recommend replacing saturated fats with unsaturated fatsCitation3,Citation23–25.
The purpose of this analysis is to estimate the potential medical care cost savings in the US associated with a switch from a diet high in SFA to a diet high in MUFA. The savings associated with a high-MUFA diet, rather than a high-PUFA diet, are estimated because MUFAs are increasing in the food supply due to their functionality. Substituting MUFAs for saturated fat preserves flavor and shelf life, whereas PUFAs are unstable during storage and cooking, can alter flavors, and contribute to rancidity in packaged and fried foodsCitation7,Citation26,Citation27. The benefits of MUFA depend on their source; animal-based MUFA (which co-occur with SFA) tend to have no detectable health benefit, whereas plant-based MUFA are associated with benefits to cardiovascular healthCitation5,Citation6,Citation12,Citation28–31. This paper estimates the benefits of a switch from SFA to plant-based MUFA. As the relative health benefits of MUFA and PUFA continues to be debatedCitation7,Citation32–35, the purpose is to document the benefits of substituting MUFA for SFA, not MUFA relative to PUFA.
Methods
Data: Medical Expenditure Panel Survey (MEPS)
This study uses data from the 2000–2010 waves of the Medical Expenditure Panel Survey (MEPS), which is a comprehensive, nationally representative survey of the US civilian non-institutionalized population conducted annually since 1996 using an overlapping panel designCitation36. Respondents are surveyed about their medical care use and expenditures over the course of 2 years through five interview rounds. In addition, utilization and expenditure data are collected directly from participants’ medical service providers and pharmacies through the Medical Provider Component. Thus, the MEPS contains the richest and most complete data on the medical care utilization and expenditures for a nationally representative sample of Americans. The sample is limited to adults aged 18 years and older with non-zero survey weights, leaving 247,700 respondents for the analysis of medical expenditures. For our analysis of job absenteeism, we excluded those who did not have a job, or a job to return to, during any of the three MEPS survey rounds in the calendar year (78,750 respondents), and those who were employed but did not answer the question on work loss days (4,373 respondents). This left a sample of 164,577 for the analysis of job absenteeism.
The MEPS asks whether each respondent has ever been diagnosed with specific conditions, including several related to heart disease: coronary heart disease (CHD), angina pectoris, myocardial infarction, and any other kind of heart condition or heart attack. Individuals are classified as having heart disease if they have been diagnosed with any of these conditions.
Medical expenditures are aggregated over all types of care, including inpatient, outpatient, prescription drugs, and other care, which includes dental, vision, home healthcare services, and medical equipment, but excludes spending on over-the-counter medications. To ensure comparability over time, medical expenditures in each year were converted to year 2010 dollars using the Consumer Price Index of the US Bureau of Labor StatisticsCitation37.
Medical expenditures are categorized by payer: the patient (i.e. out-of-pocket expenditures), private health insurance companies, Medicare, Medicaid, all third-party payers combined, and the total from all sources. Estimates are also presented for sub-populations based on their primary insurance coverage: privately insured, Medicare beneficiaries, Medicaid beneficiaries, and the full year uninsured.
The MEPS also collects data from respondents about the number of work days lost to poor health; these are the number of days in which the respondent was unable to work for a half day or more due to illness or injury. We use information on the reference period associated with each interview to calculate the number of work loss days (WLD) in each year. In cases where WLD were missing for certain rounds, we scaled-up the WLD from the other survey rounds proportionally to generate an annual estimate. Using this method, we derived WLD for individuals of 18 and older who reported they had a job, or a job to return to, at any time during the calendar year.
MEPS data were collected through a stratified multi-stage probability design, which is accounted for in the calculation of the standard errors of the marginal effects. Specifically, the method of balanced repeated replications is used to estimate standard errors, accounting for clustering at the primary sampling unit level, stratification, and weightingCitation38.
Estimated impact of substituting MUFA for SFA
The calculation of the medical cost savings associated with switching to a high-MUFA diet (described later in this section) is based on the finding by Li et al.Citation5 that replacing 5% of energy intake from SFA with equivalent energy from plant-based MUFA was associated with a 15% lower risk of coronary heart disease (95% CI = 3–26%)Citation5. The universal adoption of a high-MUFA diet is simulated by calculating the medical cost savings of a 15% reduction in the prevalence of heart disease. As a robustness check, we also estimate the savings based on an earlier estimate; Estruch et al.Citation6 found in a randomized controlled trial that a Mediterranean diet (which is high in plant-based MUFA)Citation7 was associated with a 30% lower risk of major cardiovascular events (95% CI = 8–46%).
Methods for estimating direct (medical care) costs
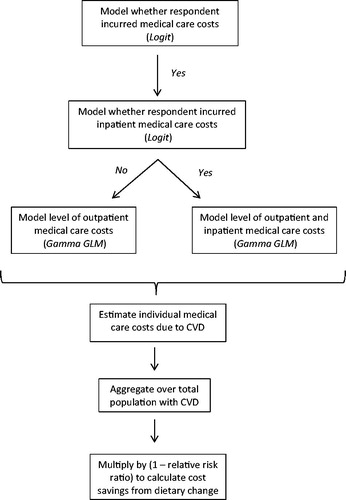
Estimating the medical care cost savings associated with cases of heart disease averted through dietary improvements involves several steps. An overview of these steps is provided in . First, the medical care costs associated with heart disease—both the average annual cost per case and the aggregate annual costs for the US—are calculated. These are estimated using a four-part model (4PM), which addresses both the non-normality of the cost data and the difference in expenditures between those with and without an inpatient stayCitation39,Citation40. The four parts of the 4PM are:
whether the respondent incurred any medical care costs that year, estimated using the entire sample;
whether the respondent incurred any inpatient costs that year, estimated using the sample of individuals who incurred medical care costs;
the amount of the respondent’s medical care costs that year, estimated using the sample of individuals who incurred medical care costs but did not have a hospital stay; and
the amount of the respondent’s medical care costs that year, estimated using the sample of individuals who incurred medical care costs and did have a hospital stay.
The first and second parts of the 4PM are estimated using logit models. Based on the results of Park and Hosmer-Lemenshow specification tests, the third and fourth parts of the 4PM are estimated using Gamma generalized linear models (GLM) with a log linkCitation41,Citation42. The Gamma GLM is commonly used to model medical expenditures for two reasons: (1) it specifies the variance to be proportional to the square of the conditional mean function, making it consistent with data distributions characterized by over-dispersion, such as medical expenditures; and (2) it allows one to directly model the raw-scale data, so regression coefficients do not have to be transformed in order to forecast expenditures.
All of the medical expenditure models controlled for the following individual characteristics: gender, race/ethnicity, respondent age, education level, Census region, whether the respondent lives in an urban area, whether the respondent was married, household composition, whether the survey information was self-reported as opposed to proxy-reported, source of health insurance, whether the respondent’s health insurance was administered by an HMO or managed care plan, and indicator variables for year.
The regression model also controls for whether the respondent had ever been diagnosed with each of the following common chronic conditions: diabetes, stroke, high blood pressure without heart disease, joint pain, emphysema, and asthma. These are MEPS “priority conditions”, for which data are collected from every respondent, irrespective of whether they used medical care during the year. By controlling for these co-morbid conditions that may also be caused by dietary fat intake, our model generates a conservative, lower-bound, estimate of the heart disease costs associated with a diet high in SFA.
Our regressor of interest is the indicator variable for whether the respondent had ever been diagnosed with heart disease. Using the 4PM, the average total and out-of-pocket medical expenditures per case of heart disease are estimated, as well as the aggregate medical expenditures associated with heart disease, by year, from 2000–2010 for the adult US population (i.e. those aged 18 and older).
The annual medical care costs of heart disease are calculated from several perspectives: total (from all sources), all third-party payments, Medicare payments, Medicaid payments, and out-of-pocket payments.
The estimate of savings has two sources of variability: (1) from the estimate of the relative risk of heart disease associated with a high-MUFA diet, that is, the uncertainty that is reflected in the 95% confidence interval (CI) reported in Li et al.Citation5; and (2) from the estimates of the medical care costs of heart disease, that is, the uncertainty that is reflected in the 95% CI around our estimates of the healthcare costs of heart disease. The first source of variation is accounted for using the delta methodCitation42, and the second is accounted for using the method of balanced repeated replications (BRR)Citation38. Specifically, we first estimate medical expenditures attributable to heart disease and calculate the standard error of this marginal effect using BRR to account for the complex survey design of the MEPS. Next, we multiply the marginal effect by one minus the relative risk estimate and calculate the standard error of this function using the delta method. As a result, the confidence intervals around the cost savings reflect both the uncertainty in the extent to which a high-MUFA diet reduces the risk of heart disease and the uncertainty in the costs of heart disease.
Methods for estimating indirect (job absenteeism) costs
We additionally estimate the indirect costs by estimating the annual work loss days (WLD) associated with heart disease. The WLD data are also non-normally distributed; specifically, many respondents report zero WLD, and a small percentage of the sample reports a large number of WLD.
We address both of these features of the data using a zero-inflated negative binomial model (ZINB)Citation43. This is an appropriate model when the outcome represents a count (i.e. takes only non-negative integer values) with many zero values. We include the same regressors from our medical expenditure models in our models of WLD, but make two minor modifications to reflect the difference between the employed sample at risk of WLD and the overall sample at risk of medical expenditures. First, our highest age category is age 65 and older (rather than 75 and older, which is a concession to the fact that there are fewer older subjects in the employed sample because of retirement). Second, we combine Medicare and Medicaid to create a single public insurance indicator (because fewer subjects in the employed sample are either old or poor). We also add regressors to the model that control for characteristics of the employer and occupation; specifically: employer size (number of employees is 1–24, 25–99, 100–499, 500 or more), whether employer size was not reported, industry (four categories grouped by similarity), professional occupation, union membership, whether the employer provides sick leave, and whether the employer provides paid time off to see the doctor.
We estimate the number of WLD attributable to heart disease at the individual level, which is used to calculate the value of lost productivity associated with heart disease for the average individual and for the full US adult working population from 2000–2010. In order to estimate productivity costs, we multiply each respondent’s predicted annual WLD by their reported work hours per day and hourly wage rate1,Citation39,Citation44. To ensure comparability over time, these productivity costs in each year are converted to year 2010 dollars using the Consumer Price Index of the US Bureau of Labor Statistics.
The MEPS asks respondents to report the number of days on which they missed at least half a day of work. This question is imprecise; one cannot infer whether the respondent lost half a workday, a full workday, or something in between on those days. To clearly convey this uncertainty, we calculate two productivity loss estimates: the lower bound assumes that respondents missed a half day of work per WLD, and the upper bound assumes the respondent missed a full day of work per WLD. By showing what the lost productivity is at its least and at its most, we clearly convey the uncertainty that is due to the wording of the question in MEPS.
As before, we estimate the savings associated with the adoption of a high-MUFA diet using the estimates of Li et al.Citation5 and apply the estimates of Estruch et al.Citation6 as a robustness check. In addition, our confidence intervals reflect uncertainty due to the estimate of the impact of a high-MUFA diet on heart disease and the estimate of the impact of heart disease on WLD.
Results
Summary statistics
reports descriptive statistics for the sample. Eighty-five per cent of the sample incurred some medical expenditures in the year they were observed in the MEPS; 9% incurred inpatient medical expenditures. On average, annual medical expenditures totaled $4,437 in 2010 dollars. Medical expenditures are highly skewed to the right, with a standard deviation of $12,378. In the employed sample, respondents averaged 4.32 WLD per year to illness or disability. In the overall sample, 11.2% of respondents were diagnosed with heart disease.
Table 1. Descriptive statistics: Medical Expenditure Panel Survey, 2000–2010.
Savings in direct medical care costs from replacing a high-SFA diet with a high-MUFA diet
The average increase in annual per capita medical expenditures associated with a diagnosis of heart disease is listed in the first row of . Among all adults, for the period 2000–2010, it averages $3,217 per year in 2010 dollars (95% CI = $2,970–$3,464), of which $406 were out-of-pocket payments (95% CI = $373–$439). Among all adults, heart disease raises medical expenditures by 28.1% (95% CI =26.3–29.9%). When examined by the source of one’s primary insurance, the average total annual medical expenditures associated with heart disease are: $3,309 (95% CI = $2,939–$3,679) for the privately insured, $5,232 (95% CI = $4,654–$5,810) for those on Medicare, $3,123 (95% CI = $2,165–$4,081) for those on Medicaid, and $1,562 (95% CI = $1,113–$2,010) for the uninsured. The costs of heart disease differ by primary payer for a variety of reasons, including differences in providers, severity of illness, quantity of care, and price.
Table 2. Per capita medical care expenditures associated with heart disease adults age ≥18.
lists the total US costs of heart disease in adults, both overall and separately, by payer: private insurance companies, Medicare, Medicaid, all third-party payers combined, and out-of-pocket by the patient. These costs are listed by year, as well as the annual average for the entire period (2000–2010) and the more recent period of 2008–2010, the latter of which may be more relevant given the increase in inflation-adjusted medical care costs. The data indicate that, in 2010, $171.3 billion was associated with heart disease (95% CI = $154.3–$188.4 billion). Overall predicted medical expenditures for this sample in 2010 were $1,164.1 billion; thus, heart disease was responsible for 14.7% (95% CI = 13.5–15.9%) of overall medical expenditures for this sample.
Table 3. Total medical care costs of heart disease (billions of 2010 USD).
Despite the fact that all expenditures are expressed in inflation-adjusted (year 2010) dollars, the medical care costs of heart disease more than doubled between 2000 ($81.1 billion) and 2010 ($171.3 billion). This is due to a variety of factors: the introduction of new and expensive treatments, changes in the utilization of existing treatments, changes in prices of existing treatments, and a rising number of cases of heart disease.
Of the $171.3 billion in medical care costs associated with heart disease, $14.5 billion (95% CI = $12.8–$16.2 billion) was paid out of pocket by patients, and third-party payers covered $155 billion (95% CI = $138.5–$171.5 billion). Within the category of third-party payers, private insurers paid $52.6 billion (95% CI = $44.8–$60.4 billion), Medicare paid $62.4 billion (95% CI = $52.0–$72.9 billion), and Medicaid paid $9.1 billion (95% CI = $5.8–$12.3 billion).
The costs of treating heart disease, listed in , are then used to estimate the savings in avoided medical care costs associated with the number of cases of heart disease averted because of dietary change. The nationwide savings in medical care expenditures associated with switching from a diet high in SFA to a high-MUFA diet, and thus reducing the risk of heart disease, are reported in . Savings are listed by year (2000–2010) as well as the average from 2000–2010 and during 2008–2010. Total savings are listed in the first column, with savings to specific payers listed in subsequent columns. Had the US consumed a high-MUFA rather than a high-SFA diet in 2010, it would have averted $25.7 billion (95% CI = $6.0–$45.4 billion) in medical expenditures, with private insurance companies saving $7.9 billion (95% CI = $1.8–$14.0 billion), Medicare saving $9.4 billion (95% CI = $2.1–$16.7 billion), Medicaid saving $1.4 billion (95% CI = $0.2–$2.5 billion), and patients saving $2.2 billion (95% CI = $0.5–$3.8 billion) in out-of-pocket payments.
Table 4. Total medical care cost savings from switching to a high-MUFA diet based on Li et al.Citation5 (billions of 2010 USD).
Those estimates are based on the estimated reduction in the risk of heart disease from replacing SFA with MUFA, as reported by Li et al.Citation5. As a robustness check, we estimated the savings using the 30% reduction in the risk of heart disease (95% CI =8–46%) found by Estruch et al.Citation6. indicates that, based on that estimate, if the US consumed a high-MUFA rather than a high-SFA diet in 2010, it would have averted $51.4 billion (95% CI = $19.0–$83.8 billion) in medical expenditures, with private insurance companies saving $15.8 billion (95% CI = $5.7–$25.9 billion), Medicare saving $18.7 billion (95% CI = $6.6–$30.8 billion), Medicaid saving $2.7 billion (95% CI = $0.8–$4.7 billion), and patients saving $4.3 billion (95% CI = $1.6–$7.1 billion) in out-of-pocket payments.
Table 5. Total medical care cost savings from switching to a high-MUFA diet based on Estruch et al.Citation6 (billions of 2010 USD).
Savings in indirect job absenteeism costs from replacing a high-SFA diet with a high-MUFA diet
The average increase in annual work loss days (WLD) per capita associated with a diagnosis of heart disease is listed in . Among all adults, it averages 3.5 per year (95% CI =2.7–4.3 days), which is the average amount by which the WLD of those with heart disease exceed those of individuals without heart disease. also shows the value of those lost work days; the lower bound (assuming each represented one-half of a lost work day) is $254 per person (95% CI = $197–$311) and the upper bound (assuming each represented a full lost work day) is $507 per person (95% CI = $394–$622).
Table 6. Per capita work loss days and work loss productivity cost associated with heart disease for working adults age ≥18.
The estimated indirect costs of heart disease and the savings in such indirect costs that would be associated with a nationwide switch from a high-SFA diet to a high-MUFA diet are listed in . We present both the lower bound (assuming only a half day was lost) and upper bound (assuming a full day was lost). In 2010, the total value of lost productivity from the increased job absenteeism due to all heart disease ranged from a lower bound of $3.9 billion (95% CI = $2.9–$4.8 billion) to an upper bound of $7.7 billion (95% C = $5.8–$9.6 billion).
Had the US consumed a high-MUFA rather than a high-SFA diet in 2010, it would have averted job absenteeism costs with a lower bound of $0.6 billion (95% CI = $0.1–$1.0 billion) and an upper bound of $1.2 billion (95% CI = $0.2–$2.1 billion). Those estimates are based on the estimated reduction in the risk of heart disease from a switch from SFA to MUFA reported by Li et al.Citation5. As a robustness check, we estimated the savings using the reduction in the risk of heart disease based on dietary change found by Estruch et al.Citation6. indicates that, based on that estimate, if the US consumed a high-MUFA rather than a high-SFA diet in 2010, it would have averted job absenteeism costs with a lower bound of $1.2 billion (95% CI = $0.4–$1.9 billion) and an upper bound of $2.3 billion (95% CI = $0.8–$3.9 billion).
Discussion and conclusions
At the national level for the US, the aggregate savings from avoided medical care expenditures on heart disease, due to a switch from a high-SFA diet to a high-MUFA diet, totals ∼$25.7 billion (95% CI = $6.0–$45.4 billion) in 2010. To put this in context, it is greater than the estimated medical care costs of alcohol abuse ($25.3 billion in year 2010 dollars)Citation45. It is also more than the 2011 budgets of the Centers for Disease Control and Prevention ($5.7 billion), Department of Commerce ($9.9 billion), and Department of the Interior ($13.7 billion). If the costs of treating heart disease continue to grow—they more than doubled between 2000 and 2010 (even controlling for inflation)—then the savings that could be achieved through dietary change will be even greater.
Notably, the savings from dietary change would accrue to the full range of payers in the healthcare sector. Had the US consumed a high-MUFA diet rather than a high-SFA diet in 2010, the savings to private insurance companies would have been $7.9 billion (95% CI = $1.8–$14.0 billion), Medicare $9.4 billion (95% CI = $2.1–$16.7 billion), Medicaid $1.4 billion (95% CI = $0.2–$2.5 billion), plus patients would have saved $2.2 billion (95% CI = $0.5–$3.8 billion) in out-of-pocket payments.
Avoided medical care costs are not the only benefits from dietary change. The estimates also imply that a switch from a high-SFA diet to a high-MUFA diet would involve a substantial reduction in job absenteeism costs, which range from a lower bound of $0.6 billion (95% CI = $0.1–$1.0 billion) to an upper bound of $1.2 billion (95% CI = $0.2–$2.1 billion) for 2010.
Our models estimate the savings associated with a switch from a diet high in SFA to a diet high in MUFA. This specific dietary change was the focus for reasons of feasibility and practicality. The switch is policy-relevant because the 2015–2020 US Dietary GuidelinesCitation24 recommend replacing SFA with MUFA or PUFA to lower the risk of heart disease. MUFA rather than PUFA was the focus because, although there are health benefits associated with a switch from SFA to a diet high in PUFACitation13–17,Citation32–35, a switch to MUFA is more realistic and practical than a switch to PUFA, because MUFA has advantages with respect to stability, shelf-life, and flavorCitation7,Citation26,Citation27. (However, the relative merits of both MUFA and PUFA continue to be studiedCitation33,Citation34.) The specific substitution of replacing 5% of energy intake from SFA with equivalent energy from plant-based MUFA was chosen as a realistic magnitude. Currently, SFA intakes in the US account for 11% of total energyCitation46; this exceeds the dietary recommendations that SFA constitute less than 10% of energy for the general adult populationCitation23,Citation34, and less than 7% of energy for individuals with heart diseaseCitation28. Currently, MUFA intakes in the US constitute only 12% of energyCitation46; in contrast, in the Mediterranean diet MUFA constitutes 16–29% of caloriesCitation25. Replacing SFA with MUFA may be a feasible option to meet current dietary recommendations as well as lower the risk of heart disease and its associated economic impact. The 5% substitution was also chosen for the practical reason that it has been sufficiently studied that there exists an estimate of its impact on the relative risk of heart diseaseCitation5.
Historically, there was ambiguity about whether replacing SFA with MUFA would reduce the risk of heart disease. Part of the uncertainty was rooted in the fact that some studies did not distinguish between MUFA of animal origin (which is less healthy) or of plant origin (which is more healthy)Citation5,Citation12,Citation17,Citation29–31. There is now evidence that replacing SFA with MUFA principally from plant sources reduces the risk of heart diseaseCitation6,Citation12,Citation31,Citation47,Citation48.
We emphasize that this paper’s estimates are based on a switch to MUFA from plant sources; MUFA from animal sources (which tends to co-occur with SFA) would likely not have the same benefits2,Citation24. However, end-point studies and epidemiological studies of the links between substituting MUFA for SFA, subsequent impacts on heart disease, and the ultimate impacts on costs are needed.
The savings in direct (medical care) costs and indirect (job absenteeism) costs estimated in this paper are associated with a switch by the entire US population to a high-MUFA diet. Such a complete switch is unlikely, but the total savings is a useful statistic because it indicates the economic impact of current dietary patterns.
Basing the calculation on the reduction in heart disease estimated by Estruch et al.Citation6 rather than that estimated by Li et al.Citation5 results in even greater estimated savings. However, we use the Li et al. estimates for our primary results because: (a) they are informative about the benefits of a high-MUFA diet generally (as determined using a food frequency questionnaire), whereas the Estruch et al. results concern a Mediterranean diet specifically; and (b) the Li et al. estimates are based on a substitution of 5% energy from SFA to MUFA, which may be more realistic than a change to the Mediterranean diet. Given that our estimates are based on the smaller reduction; they are to some extent conservative.
An important contribution of this analysis is that the confidence intervals around the estimated savings from dietary change take into account not only the standard errors in the estimate of the savings from averting heart disease, but also the standard errors in the estimate of the impact of dietary change on the risk of heart disease.
The data and methods used here have the following limitations. Although it is possible, given these data, to calculate the savings associated with a reduced prevalence of heart disease, it is not possible to estimate the savings associated with decreases in the severity of heart disease; i.e. it is possible to calculate savings from the extensive but not intensive margin. The calculation assumes that all Americans consume a high-SFA diet; to the extent that some Americans already consume a high-MUFA diet, the reduction in heart disease would be less.
Our regression model for direct costs assumes that, by avoiding heart disease, individuals would have incurred the same medical care costs as observationally identical respondents who did not develop heart disease. Thus, the model does not assume that individuals who avoid heart disease are perfectly healthy; it assumes that they experience the same illnesses as observationally identical individuals without heart disease. However, those without heart disease may be an imperfect counterfactual for those with heart disease, and thus the model may not perfectly capture the set of illnesses people would contract after avoiding heart disease and the medical care costs they would incur. Another limitation is that we do not adjust for additional healthcare costs that may occur during the additional years of life that result from avoiding heart disease.
The MEPS data of medical care expenditures do not include the costs of informal care at home by family and friends, which represents another potential source of savings from dietary change. The QALY or productivity gains associated with avoiding premature mortality are also not included in our estimate.
The estimate of the savings to Medicaid ($1.4 billion) is small relative to the estimated savings to Medicare ($9.4 billion) and private health insurance companies ($7.9 billion). This is partly because the MEPS does not include people in nursing homes, many of whom are eligible for Medicaid and incur substantial charges; for this reason, the MEPS, which only surveys the non-institutionalized population, understates the costs of heart disease among Medicaid beneficiaries. In addition, Medicaid pays less to healthcare providers than do private health insurance companies and the Medicare program. As a result, the costs of treating any given case are usually smaller when Medicaid is the payer.
Americans consume approximately a third of all of their calories away from home (which includes restaurants, i.e. both full-service and quick-serve, convenience stores, vending machines, school, work site and hospital cafeterias)Citation49. Thus, making a switch to a high-MUFA diet would require substitutions not only in home cooking but also in food and meals eaten away from home. Improvements in diet, thus, require changes in multiple sectors.
In summary, substantial savings could be achieved by switching from a high-SFA diet to a high-MUFA diet, in terms of reduced medical expenditures and job absenteeism associated with heart disease.
Transparency
Declaration of funding
This research was supported by Dow AgroSciences. The study design, conduct and analysis, and manuscript development were conducted by the authors independent of the funding source.
Declaration of financial/other interests
JC, CM, LGG, PKE, and PJHJ report no conflicts of interest. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
We thank Steve Walker, Kristie Sigler, Tiffany Howe, Andy Gard, and Lisa Brooks for editorial assistance.
Notes
Notes
1 Hourly wage information was not collected for self-employed respondents, so we imputed their wages as well as the wages of those with missing wage information using a standard two part model or 2PM44. The first part of the 2PM is a Probit model of employment (including having a job to return to) using the full sample of individuals aged 18–64. The second part of the 2PM is an OLS model of log wages for those with reported wages. We also used Duan et al.’sCitation39 non-parametric smearing factor estimate, adjusted for age-induced heteroscedasticity, to retransform the log wage estimates back to the raw scale of dollars. The regressors in both parts of the 2PM include age, age squared, gender, race, years of education, household composition, Census region, the log of family income per capita excluding the respondent’s wage income, and the spouse’s wage (if applicable). From the 2PM we calculate E(wage|X) and use this conditional mean function to impute wages for the self-employed and those employed by businesses, but with missing wage information.
2 For example, a pooled analysis of 11 cohort studiesCitation17 failed to detect any reduction in heart disease associated with a substitution of MUFA for SFA, but this is due, at least in part, to: the MUFA studied originated from animal sources rather than plant sources, and trans-fatty acids (TFA) were included with the MUFA. The editorial that accompanied the JakobsenCitation17 article stated that, as a result of incomplete controls for confounders in the Jakobsen study, “monounsaturated fatty acids may have acted as a surrogate for other risk factors” (p. 1283).
References
- Xu JQ, Murphy SL, Kochanek KD, et al. Deaths: final data for 2013. Natl Vital Stat Rep 2016;64:1-16
- Centers for Disease Control and Prevention. Heart Disease Fact Sheet. Atlanta, GA: Centers for Disease Control and Prevention, 2016. http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_heart_disease.htm
- Alwan A. Global status report on noncommunicable diseases 2010. Geneva, Switzerland: World Health Organization, 2011
- Institute for Health Metrics and Evaluation. The state of U.S. health: innovations, insights, and recommendations from the global burden of disease study. Seattle, WA: Institute for Health Metrics and Evaluation, 2013
- Li Y, Hruby A, Bernstein AM, et al. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease. J Am Coll Cardiol 2015;66:1538-48
- Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N England J Med 2013;368:1279-90
- Hammad S, Pu S, Jones PJ. Current evidence supporting the link between dietary fatty acids and cardiovascular disease. Lipid. 201; 51:507-17
- Bhupathiraju SN, Tucker KL. Coronary heart disease prevention: mutrients, foods, and dietary patterns. Clin Chim Acta 2011;412:1493-514
- Gillingham LG, Harris-Janz S, Jones PJH. Dietary monounsaturated fatty acids are protective against metabolic syndrome and cardiovascular disease risk factors. Lipids 2011;46:209-28
- ÓFlaherty M, Flores-Mateo G, Nnoaham K, et al. Potential cardiovascular mortality reductions with stricter food policies in the United Kingdom of Great Britain and Northern Ireland. Bull WHO 2012;90:522-31
- Lin L, Allemekinders H, Dansby A, et al. Evidence of health benefits of canola oil. Nutr Rev 2013;71:370-85
- Wang DD, Li Y, Chiuve SE, et al. Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med 2016; 176:1134-45; doi: 10.1001/jamainternmed.2016.2417. [Epub ahead of print]
- Becerra-Tomas N, Babio N, Martinez-Gonzalez MA, et al. Replacing red meat and processed red meat for white meat, fish, legumes or eggs is associated with lower risk of incidence of metabolic syndrome. Clin Nutr 2016;31:017
- Mensink, RP. Effects of saturated fatty acids on serum lipids and lipoproteins: a systematic review and regression analysis. Geneva: World Health Organization, 2016
- Brouwer IA. Effect of trans-fatty acid intake on blood lipids and lipoproteins: a systematic review and meta-regression analysis. Geneva: World Health Organization, 2016
- Hooper L, Martin N, Abdelhamid A, et al. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database System Rev 2015;6:CD011737
- Jakobsen MU, O’Reilly EJ, Heitmann BL, et al. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr 2009;89:1425-32
- Mozaffarian D, Katan MB, Ascherio A, et al. Trans fatty acids and cardiovascular disease. N Engl J Med 2006;354:1601-13
- Mente A, Koning LD, Shannon HS, et al. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 2009;169:659
- O’Sullivan TA, Hafekost K, Mitrou F, et al. Food sources of saturated fat and the association with mortality: a meta-analysis. Am J Public Health 2013;103:e31-e42
- Hu FB, Meir J, Stampfer MG, et al. Dietary fat intake and the risk of coronary heart disease in women. New Engl J Med 1997;337:1491-99
- Mozaffarian D, Clarke R. Quantitative effects on cardiovascular risk factors and coronary heart disease risk of replacing partially hydrogenated vegetable oils with other fats and oils. Eur J Clin Nutr 2009;63:S22-S33
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th edn. Washington, DC: U.S. Department of Agriculture, 2015. http://health.gov/dietaryguidelines/2015/guidelines/
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans 2015–2020. 8th edn [Internet]. Washington, DC: U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015. http://health.gov/dietaryguidelines/2015/guidelines
- Kris-Etherton PM. Monounsaturated fatty acids and risk of cardiovascular disease. Circulation 1999;100:1253-8
- Eckel RH, Borra S, Lichtenstein AH, et al. Understanding the complexity of trans fatty acid reduction in the American diet: American Heart Association Trans Fat Conference 2006: report of the Trans Fat Conference Planning Group. Circulation 2007;115:2231-46
- List GR, Orthoefer FT, editors. Trait-modified oils in foods. Chichester, West Sussex, UK: Wiley-Blackwell, 2015
- Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001;285:2486-97
- Hruby A, Hu FB. Saturated fat and heart disease: the latest evidence. Lipid Technology 2016;28:7-12
- USDA. Scientific Report of the 2015 Dietary Guidelines Advisory Committee: advisory report to the Secretary of Health and Human Services and the Secretary of Agriculture. Washington, DC: USDA, 2015
- Katan MB. 2009. Omega-6 polyunsaturated fatty acids and coronary heart disease. Am J Clin Nutr 2009;89:1283-4
- Grundy SM. What is the desirable ratio of saturated, polyunsaturated, and monounsaturated fatty acids in the diet? Am J of Clin Nutr 1997;66(Suppl):988S-90S
- Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 2006;114:82-96
- Kris-Etherton PM, Innis S, American Dietetic Association, Dietitians of Canada. Position of the American Dietetic Association and Dietitians of Canada: dietary fatty acids. J Am Diet Assoc 2007;107:1599-611
- Jakobsen MU, O'Reilly EJ, Heitmann BL, et al. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr 2009;89:1425-32
- Davis K. Sample design of the 2011 Medical Expenditure Panel Survey Insurance Component, Methodology Report #27. Rockville, MD: Agency for Healthcare Research and Quality, 2013
- Bureau of Labor Statistics. Handbook of Methods: U.S. Bureau of Labor Statistics, 2013. http://www.bls.gov/opub/hom/
- Krewski D, Rao JNK. Inference from stratified samples: properties of the linearization, jackknife and balanced repeated replication methods. Ann Stat 1981;9:1010-19
- Duan N, Manning WG, Morris CN, et al. A comparison of alternative models for the demand for medical care. J Bus Econ Stat 1983;1:115-26
- Newhouse JP. Free for all?: Lessons from the Rand Health Insurance Experiment. Cambridge, MA: Harvard University Press, 1996
- McCullagh P, Nelder JA. Generalized linear models. 2nd edn. London: Chapman and Hall; 1989
- Greene WH. Econometric analysis. 6th edn. Upper Saddle River, NJ: Pearson Prentice Hall, 2008
- Cameron AC, Trivedi PK. Regression analysis of count data. Econometric Society Monographs. Cambridge, UK: Cambridge University Press, 1998
- Jones A. Health econometrics. Chapter 6. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. 2000. New York, NY: Elsevier North-Holland, p 265-336
- Harwood H. Updating estimates of the economic costs of alcohol abuse in the United States: estimates, update methods, and data. Bethesda, MD: U.S. Dept. of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism, 2000
- U.S. Department of Agriculture, Agricultural Research Service Energy intakes: percentages of energy from protein, carbohydrate, fat, and alcohol, by gender and age. What we eat in America: NHANES 2009–2010. Washington, DC: USDA, 2012. www.ars.usda.gov/ba/bhnrc/fsrg
- Guasch-Ferré M, Babio N, Martínez-González MA, et al; PREDIMED Study Investigators. Dietary fat intake and risk of cardiovascular disease and all-cause mortality in a population at high risk of cardiovascular disease. Am J Clin Nutr 2015;102:1563-73
- Flock MR, Fleming JA, Kris-Etherton PM. Macronutrient replacement options for saturated fat: effects on cardiovascular health. Curr Opin Lipidol 2014;25:67-74
- Guthrie J, Lin B-H, Okrent A, et al. Americans’ food choices at home and away: how do they compare with recommendations? USDA, Economic Research Service, Washington, DC, 2013. http://www.ers.usda.gov/amber-waves/2013-february/americans-food-choices-at-home-and-away.aspx#.VyyyEE32aM8