Abstract
Aims: To estimate the direct cost of hypoglycemia in insulin-treated adults with type 1 diabetes (T1DM) and type 2 diabetes (T2DM) in Denmark.
Materials and methods: The Local Impact of Hypoglycemia Tool (LIHT) was used to estimate the costs associated with insulin-related hypoglycemia. Average utilization of healthcare resources, including the costs of pre-hospitalization, hospital admission, healthcare professional contact and follow-up, glucose/glucagon, and extra SMBG tests to monitor blood glucose following an episode, was used to calculate an average cost per severe and per non-severe hypoglycemic episode. The cost per episode was then applied to the rates of severe and non-severe hypoglycemia in people with T1DM and T2DM in Denmark.
Results: The direct cost of insulin-related hypoglycemia in Denmark is DKK 96.2 million per year, which equates to EUR 12.9 million. For people with T1DM prone to severe hypoglycemia (defined as having ≥2 severe episodes in the past year), the cost per person per year increases by DKK 4,155 compared with the T1DM population average, and for people with T2DM prone to non-severe hypoglycemia (defined as having ≥1 non-severe episode in the last 4 weeks), the cost increases by DKK 647 per person per year compared with the T2DM population average.
Conclusions: The LIHT highlights the substantial economic burden of insulin-related hypoglycemia in Denmark, and provides a means to estimate the savings that could be made by lowering hypoglycemia rates. For example, the costs associated with using a new insulin or introducing a patient education program could be offset with the cost saving from reducing hypoglycemia.
Introduction
Diabetes is a chronic metabolic condition characterized by high blood glucose levels (hyperglycemia). Prolonged hyperglycemia increases the risk of microvascular and macrovascular complications, including heart disease, stroke, nephropathy, and retinopathyCitation1. Diabetes was estimated to affect 5.7% of the total population in Denmark in 2012Citation2,Citation3, and ∼10% of patients had type 1 diabetes (T1DM) and 90% had type 2 diabetes (T2DM)Citation2.
All people with T1DM and 14.5% of people with T2DM in Denmark require treatment with insulin to lower blood glucose levelsCitation4,Citation5. Danish guidelines for T1DM recommend the use of a basal-bolus insulin regimen, with insulin analogs recommended as the basal insulin to reduce the risk of hypoglycemia, and in particular nocturnal hypoglycemiaCitation5. For people with T2DM, Danish guidelines recommend metformin as first-line therapy; however, insulin is also recommended as a first choice for those with severe hyperglycemia, after which metformin can be added or switched to when blood glucose levels have stabilizedCitation6. In Denmark, people with T2DM initiate insulin therapy with either premixed insulin 1–2 times daily or basal insulin 1–2 times daily. Intensification to a basal-bolus regimen is required with disease progression and the deterioration of beta-cell function.
Hypoglycemia is a common side-effect of insulin therapy, occurring when blood glucose levels are low (defined as <3.9 mmol/L by the American Diabetes AssociationCitation1). Symptoms of hypoglycemia include anxiety, palpitations, weakness, and confusion, and severe cases can cause seizure, coma, and even deathCitation7. Non-severe episodes can be self-treated, whereas severe episodes require third-party assistanceCitation8, which can range from the administration of carbohydrates or glucagon by family, friends, or co-workers, to pre-hospitalization, emergency care visits, and, in some cases, hospitalization.
Hypoglycemia not only poses a burden to the patient, but also an economic burden to healthcare systems (direct costs) and society (indirect costs). Direct costs include medication (glucose/glucagon), ambulance services, and hospitalization for severe episodes, and general practitioner (GP) contact and extra blood glucose testing after severe and non-severe episodesCitation9–11. Indirect costs include working time lost due to a hypoglycemic episode from both absenteeism and presenteeismCitation12. There are also economic costs to the patient and their family/friends, including additional food required to treat the hypoglycemic episode and carer costs.
The economic consequences of hypoglycemia have become more relevant since the introduction of insulin analogs, which have lower rates of hypoglycemia than the traditional neutral protamine Hagedorn (NPH) insulinCitation13,Citation14, and in turn newer analogs that have lower hypoglycemia rates than older insulin analogsCitation15,Citation16. This has led to the consequent revision of many treatment guidelines to recommend insulin analogs over NPH for their more favorable hypoglycemia profile, despite their higher pack price and, in some cases, newer insulin analogs over their older counterparts. Therefore, in addition to the clinical benefit to the patient of switching insulin to one with lower hypoglycemia rates, it has become more important to understand the economic consequences of hypoglycemia in order to assess the overall cost of therapy rather than just the cost of insulin.
The aim of this study was to calculate the direct cost of insulin-related hypoglycemia in adults with diabetes in Denmark, both for the total population and a sample general population of 100,000, to enable easy adaptation to a specific region or hospital, for example.
Methods
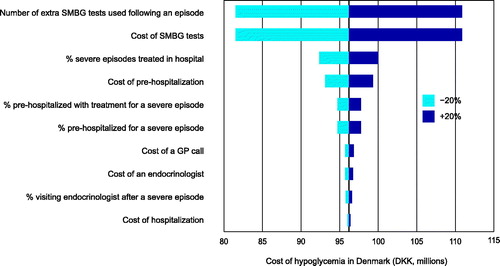
The Local Impact of Hypoglycemia Tool (LIHT) was developed to estimate the costs of severe and non-severe hypoglycemia in the UK, and has been adapted to provide costs of hypoglycemia specific to the Danish population. The methods have been described previouslyCitation17; in brief, the LIHT performs calculations based on epidemiological data, insulin usage, and healthcare unit costs and utilization values associated with hypoglycemic episodes, which can then be applied to the population of interest ().
Figure 1. Descriptive flow of calculations performed by the LIHT. HCP: healthcare professional; LIHT: Local Impact of Hypoglycemia Tool; T1DM: type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus.
Model inputs
A structured literature search was conducted to identify Danish-specific publications containing data on hypoglycemia and/or resource utilization associated with hypoglycemic episodes.
The Danish Diabetes Association reported that there were 320,545 people with diabetes in Denmark on December 31, 2012, of which 10% had T1DM and 90% T2DMCitation2. There were 3,789 children and adolescents with diabetes in Denmark in 2012Citation18, all of which were assumed to have T1DMCitation2. Therefore, after subtracting the number of children and adolescents with T1DM, the population of adults with T1DM and T2DM in Denmark was estimated to be 28,266 and 288,490, respectively. This analysis was only concerned with insulin-related hypoglycemia, therefore the number of insulin users (73,910) was extracted from MEDSTAT prescription data, 2013Citation4. All patients with T1DM require insulin (32,055); therefore, it was assumed that the remaining 41,855 people were adult patients with T2DMCitation2, corresponding to 14.5% of the total T2DM population. The total population of Denmark (5,599,665) was taken from Statistics Denmark for quarter 4 of 2012Citation3, to correspond with the number of people with diabetes, which was reported for December 2012.
The hypoglycemia rates used in the model were taken from the Danish results of a questionnaire-based survey conducted in seven European countries (n = 601 in Denmark)Citation11,Citation19. People with T1DM experienced 0.6 severe and 98.6 non-severe hypoglycemic episodes per year, and people with insulin-treated T2DM experienced 0.1 severe and 27.4 non-severe episodes per year.
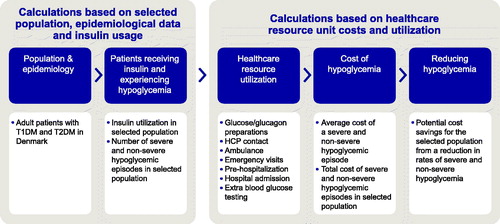
A recent randomized, open-label, blinded-endpoint crossover study (HypoAna) in Denmark captured resource utilization for patients with T1DM prone to recurrent severe hypoglycemia (defined as having ≥2 severe episodes in the past year)Citation20. It found that 20.3% of severe hypoglycemic episodes required assistance from medical personnel; the resource utilization for these episodes is shown in and is assumed for all patients with T1DM and T2DM who experience a severe hypoglycemic episode requiring medical assistance.
Figure 2. Treatment pathway and healthcare utilization values. GP: general practitioner; SMBG: self-monitored blood glucose; T1DM: type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus.
The HypoAna study also found that 9.4% of severe hypoglycemic episodes that were treated at home required emergency treatment (glucose/glucagon). A Danish study that investigated the method of treatment by a Mobile Emergency Care Unit for severe hypoglycemia treated at home found that oral glucose, intramuscular glucagon, and intravenous glucose were used in 27%, 33% and 71% of severe episodes, respectivelyCitation10.a
Values for additional blood glucose testing following a hypoglycemic episode were taken from a questionnaire-based study on non-severe hypoglycemia in DenmarkCitation11. This study found that, within 7 days of a non-severe hypoglycemic episode, people with T1DM used an average of 2.1 extra self-monitoring blood glucose (SMBG) tests and people with T2DM used an extra 2.8 tests on average. Due to a lack of corresponding data, these values were conservatively assumed to also apply to severe hypoglycemic episodes, although the actual number of extra tests used following severe hypoglycemia is likely to be higher than with a non-severe episode.
The same study also found that 1% of people with T1DM and 7% of people with T2DM contact their GP after a non-severe hypoglycemic episodeCitation11; in this analysis it was conservatively assumed that the contact was a telephone consultation.
The LIHT used the treatment pathway shown in and applied the costs shown in to calculate the cost of hypoglycemia in Denmark.
Table 1. Unit costs for healthcare resources.
Scenario analyses
Scenario analyses were performed to calculate the cost of hypoglycemia in the sub-population of people with diabetes who experience recurrent hypoglycemia. The HypoAna study assessed the rates of severe and non-severe hypoglycemia among people with T1DM who suffer from recurrent severe hypoglycemia (defined as having ≥2 severe episodes in the past year)Citation21. The mean number of severe episodes in the preceding year was reported as 5.8Citation22, and the non-severe episode rate was 56.5b episodes per person per year, 47.5 of which were in the daytime and 9.0 of which were nocturnalCitation23. The same study reported that 19% of people with T1DM suffered two or more episodes of severe hypoglycemia in the previous yearCitation22, equating to 5,371 patients who are prone to recurrent severe hypoglycemia in Denmark.
For T2DM, there were no equivalent data available for people that experience ≥2 severe episodes per year in Denmark, perhaps due to the fact that severe hypoglycemia is less common in people with T2DM. However, one retrospective study that investigated the frequency and risk of severe hypoglycemia in Danish patients with T2DM that were on intensive multifactorial treatmentCitation24 reported an overall incidence of 0.44 episodes per person in the preceding year, whilst no data were reported for non-severe episodes. Another recent questionnaire-based study in Denmark reported the rate of non-severe hypoglycemia in a sub-group of people that reported ≥1 non-severe episode in the study recall periodCitation11. A total of 51.31% of people with T2DM were included in this populationCitation11, equating to 21,476 people with T2DM prone to recurrent non-severe hypoglycemia in Denmark. The rate of non-severe hypoglycemia in this population was 49.9 episodes per year, 35.7 of which were in the daytime and 14.2 of which were nocturnalCitation11. The rate of severe hypoglycemia was 0.2 episodes per yearCitation25.
Results
Direct costs
The estimated direct cost per hypoglycemic episode ranges from DKK 17.01 to DKK 11,791.85, where the lower cost corresponds to a home-treated episode where the person only uses 2.1 extra SMBG tests following the episode and the higher cost represents a severe episode requiring pre-hospitalization, hospital admission with treatment, treatment by an endocrinologist, a follow-up endocrinologist visit, and 2.8 extra SMBG tests following the episode. The higher cost could be considerably greater if an extended stay in hospital is required.
The average direct cost for a severe hypoglycemic episode in Denmark is estimated as DKK 938.91 for people with T1DM and DKK 944.58 for people with T2DM. The average direct cost for a non-severe episode is DKK 17.28 and DKK 24.55 for people with T1DM and T2DM, respectively ().
Table 2. Cost breakdown per episode for severe and non-severe hypoglycemia.
The estimated total direct cost of insulin-related hypoglycemia in Denmark is DKK 96.2 million per year (), which equates to EUR 12.9 million (using an exchange rate of 0.1343444396 obtained from www.xe.com on April 29, 2016). This corresponds to DKK 1.7 million in a sample general Danish population of 100,000. The total direct cost of non-severe hypoglycemia is DKK 76.3 million, of which DKK 18.8 million is due to nocturnal episodes.
Table 3. Direct costs of insulin-related hypoglycemia per year in Denmark and in a sample population of 100,000.
Scenario analyses
In the sub-population of people with T1DM who are prone to recurrent severe hypoglycemia (5,371 people), the direct cost of hypoglycemia is DKK 34.5 million per year, DKK 29.2 million of which is for severe episodes and DKK 5.2 million for non-severe episodes. The total direct cost per person per year in this population is DKK 4,154.82 higher than the T1DM population average. This increase in cost is driven by a much higher cost for severe episodes due to the increase in rate and the high cost per episode. Of the DKK 5.2 million direct cost for non-severe hypoglycemia in this population, daytime episodes are responsible for DKK 4.1 million and nocturnal episodes for DKK 1.2 million.
For people with T2DM who are prone to recurrent non-severe hypoglycemia (21,476 people), direct costs are DKK 30.4 million per year, DKK 4.1 million of which are for severe episodes and DKK 26.3 million for non-severe episodes. The total direct cost per person per year in this population is DKK 646.90 higher than the T2DM population average, which is driven by the large increase in the rate of non-severe episodes. Of the DKK 26.3 million direct cost for non-severe hypoglycemia in this population, daytime episodes are responsible for DKK 18.8 million and nocturnal episodes for DKK 7.5 million.
Sensitivity analysis
In sensitivity analyses, hypoglycemia rates are varied by 10–50% for both severe and non-severe episodes separately as well as together, to show the cost savings or losses associated with reductions or increases in the rates of hypoglycemia ().
Table 4. Costs associated with rates of hypoglycemia in Denmark.
Reducing the rates of both severe and non-severe hypoglycemia by 20%, which may be possible by, for instance, changing insulin to one with a better hypoglycemia profile, results in a substantial cost saving of DKK 19.2 million per year in Denmark.
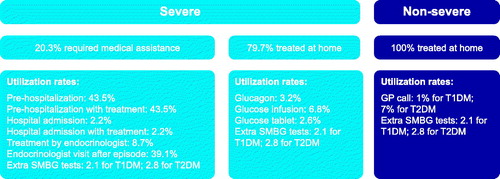
An additional sensitivity analysis varies all the unit costs and the utilization of resources by ±20%. The top two drivers of the model relate to the cost of SMBG tests and the number of extra SMBG tests used following a hypoglycemic episode. This is due to the much higher rate of non-severe episodes compared with severe episodes, and the fact that the cost of non-severe episodes is largely made up of the cost of extra SMBG tests. As stated earlier, the cost of an SMBG test used in this analysis is the cost of the least expensive test available in Denmark, and this analysis demonstrates that using a higher priced test would result in a substantial increase in costs.
The next four main drivers of the model are the percentage of severe episodes requiring medical treatment (rather than being treated at home), the cost of pre-hospitalization, the percentage pre-hospitalized with treatment for a severe episode, and the percentage pre-hospitalized for a severe episode. Varying all the other inputs by ±20% results in very little change (<1%) from the base case. The top 10 drivers of the model are shown in .
Discussion
The results of this study show that the cost of insulin-related hypoglycemia in Denmark is considerable, and highlights the savings that are possible if hypoglycemia is reduced. It is possible to reduce the rate of hypoglycemia by changing to a form of insulin with a better hypoglycemia profile, or by introducing patient education programs. The LIHT provides the opportunity for budget holders to compare the costs of changing insulin or introducing patient education programs with the savings that could be realized as a result of a reduced hypoglycemia rate. On the other hand, the International Diabetes Federation have predicted a 19% rise in the number of people with diabetes in Europe by 2040Citation26, which would result in a substantial increase in the cost burden of hypoglycemia.
This study highlights the substantial cost of non-severe hypoglycemia, which is often ignored or under-estimated. The cost of non-severe episodes in Denmark per year is over 3.5-fold higher than the cost of severe episodes (DKK 76.3 million vs 19.9 million per year), due to the much higher rate of non-severe episodes experienced by both T1DM and T2DM patients. This is despite the higher cost per episode for severe hypoglycemia compared with non-severe hypoglycemia (DKK 938.91 vs 17.28 in people with T1DM and DKK 944.58 vs 24.55 in people with T2DM, respectively).
Scenario analyses demonstrate that there is an increase in costs for people that are prone to recurrent hypoglycemia. The total cost per person per year is DKK 4,154.82 higher for people with T1DM that are prone to recurrent severe hypoglycemia than for the overall T1DM population reported in the base case, and people with T2DM who are prone to recurrent non-severe hypoglycemia cost DKK 646.90 more per person per year compared with the overall T2DM population, as reported in the base case.
Although the rate of severe episodes is higher for people with T1DM prone to recurrent severe hypoglycemia than the overall T1DM population (5.8 vs 0.6 episodes per year, respectively), the rate of non-severe episodes is actually lower (56.5 episodes per year compared with 98.6 in the base case). This could be explained by the fact that the rates used in the scenario analysis are taken from a clinical trialCitation23 in which non-severe hypoglycemic episodes had to be accompanied by a documented blood glucose level <3.9 mmol/L, whereas the base case uses rates from a real-world studyCitation12, where non-severe hypoglycemia was reported by people based on symptoms (regardless of blood glucose level) or low blood glucose (regardless of symptoms). Therefore, the more rigorous criteria employed for non-severe hypoglycemia in the clinical trial could explain the lower rate reported compared with the rate observed in the real-world study used in the base case. Furthermore, people who experience multiple severe episodes annually have been reported to be less aware of the symptoms of hypoglycemiaCitation7,Citation27, and this could also lead to non-severe episodes being unrecognized.
The study used to inform the scenario analysis for people with T1DM who are prone to recurrent severe hypoglycemiaCitation22,Citation23 also reports a relative rate reduction of 29% (95% CI =11–48; p = 0.010) for severe episodes with insulin analogs compared with human insulin, and a corresponding relative rate reduction of 6% (95% CI =2–9; p = 0.0077) for non-severe episodes. Combining both these reductions translates into a cost saving of DKK 8.8 million per year in Denmark (a 25% reduction) in this sub-population of people with T1DM experiencing two or more severe episodes per year (5,371 people) if using insulin analogs instead of human insulin.
The costs calculated for hypoglycemia in Denmark are unlikely to be over-estimated due to a number of conservative assumptions. The main assumption stems from the data used for resource utilization following a severe hypoglycemic episode that requires medical assistance. These data come from the HypoAna study in order that they be Denmark-specific; however, this study was in patients with T1DM who experience recurrent severe hypoglycemia. These resource utilization values are assumed to apply to all people with T1DM and T2DM in this analysis. This can be considered a conservative assumption, since people with T1DM who are prone to severe hypoglycemia may not require as extensive treatment as other people with diabetes, due to a familiarity with the symptoms and treatment of hypoglycemia. In addition, people with T2DM have previously been shown to have a higher resource utilization for hypoglycemia than people with T1DM. An analysis of 15 phase 3a clinical trials found that 47.4% of severe hypoglycemic episodes occurring in people with T2DM were treated at hospital, with 27.3% of episodes requiring hospitalization for more than 24 hoursCitation9. This compares with only 14.5% of severe hypoglycemic episodes occurring in people with T1DM requiring treatment at hospital with 5.0% of episodes requiring hospitalization for more than 24 hours. Another conservative assumption in the present analysis is that it does not consider an extended hospital stay, which could result in substantial additional costs. The rates of severe hypoglycemia are also unlikely to be over-estimated, since the rates used in this analysis, even in the sub-population of patients with recurrent hypoglycemia, are lower than many other published severe hypoglycemia ratesCitation24,Citation28,Citation29.
Additionally, the cost of SMBG tests used in this analysis was at the time of this study the least expensive that was publicly available, and people are assumed to use the same number of extra tests following a severe hypoglycemic episode as a non-severe episode due to a lack of data for severe episodes. In reality, people are likely to use a higher number of extra SMBG tests in the week following a severe episode to monitor and stabilize their blood glucose levels.
Another reason that the costs are unlikely to be lower in clinical practice than calculated is that children have not been considered in this analysis. While it is difficult to speculate as to the cost per patient compared with adults, there would at least be some extra costs involved for treating hypoglycemia in the 3,789 children in Denmark with diabetes that are not included hereCitation18.
Results using UK data, costs, and utilization values in the LIHT were published in 2015Citation17. The direct and indirect cost per episode and per general population of 100,000 have been converted into DKK to directly compare the results (). However, it is important to note that this comparison is for illustrative purposes only, and it is acknowledged that individual costs, healthcare budgets, pathways of care, and thus the overall burden of hypoglycemia may differ between the two countries. The estimated cost of hypoglycemia is substantially higher per episode in the UK than in Denmark, which further supports the conservative nature of the Denmark estimates. In particular, the average cost of a severe episode in people with T2DM is over 3.5-fold higher, which is due to a greater percentage of people treated by medical personnel and requiring hospitalization in the UK. The cost per 100,000 general population is considerably higher for severe episodes in the UK, with the estimate for people with T1DM being over 8-fold higher and for people with T2DM over 22-fold higher. This is due to the higher cost per episode, and the higher severe hypoglycemia rates used (3.2 vs 0.6 episodes per year for people with T1DM, and 0.7 vs 0.1 episodes per year for people with T2DM). This is in contrast to the non-severe hypoglycemia rate, which is higher in Denmark than in the UK (98.6 vs 29 episodes per year for people with T1DM, and 27.4 vs 10.2 episodes per year for people with T2DM). However, the cost per non-severe episode in the UK was estimated to be over 7-fold and 5-fold higher than the cost estimated for Denmark for people with T1DM and T2DM, respectively. This means that there is not such a large difference between the UK and Denmark for non-severe hypoglycemia in a 100,000 general population when compared with severe hypoglycemia, although the costs are still higher in the UK.
Table 5. Comparison of the results for Denmark with the results from the UK.
Indirect costs, for example lost working time due to hypoglycemic episodes, were not considered in this analysis, but can be substantial. A cross-sectional survey of Danish Diabetes Association members in 2012 found that 56.2% of adults with T1DM and 29.8% of adults with insulin-treated T2DM were employedCitation12. The estimated time lost for physical recovery per hypoglycemic episode was 166.7 minutes for a severe episode and 48.4 minutes for a non-severe episode for T1DM patients, and 169.6 and 58.0 minutes for a severe and non-severe episode, respectively, for insulin-treated T2DM patientsCitation12. A survey of 81 people with diabetes in Sweden found that non-severe hypoglycemic episodes incurred lost productivity costs of USD 248.1 per patient per yearCitation30, and the indirect cost of severe hypoglycemia is likely to be higher. Indirect costs are, therefore, also likely to play a significant part in the economic burden of hypoglycemia in Denmark. Other costs that are not considered in this analysis because they are difficult to quantify include additional contact with healthcare professionals (e.g. emails), extra foods required for the treatment of episodes, and carer costs. It is also important to note that this study is only concerned with insulin-related hypoglycemia; however, hypoglycemia can also be common with other anti-diabetic medicines, most notably sulfonylureas and glinidesCitation31, and, therefore, the total cost of hypoglycemia in Denmark will most likely be higher than that calculated in this study.
An important aspect of hypoglycemia other than the substantial economic burden on healthcare systems is the burden from a patient perspective. Concern about hypoglycemia is often a major barrier to the initiation or intensification of insulin therapy, and people may miss or reduce their insulin dose following hypoglycemiaCitation32–35. Both of these can lead to hyperglycemia and an increase in the risk of the associated comorbidities (e.g. cardiovascular disease, nerve damage, kidney disease)Citation26, which, in turn, would lead to further increases in healthcare costs. The previous under-estimation of non-severe hypoglycemic episodes on the economic burden has been discussed, and it is important to note that non-severe episodes can also have a profound impact on patients’ quality of life and adherence to therapy, and should not be overlooked. A reduction in both severe and non-severe hypoglycemia would, thus, not only reduce healthcare costs, but would also reduce and mitigate some of the other grave implications of hypoglycemia, including non-adherence to therapy, glycemic control, and lack of initiation or intensification of insulin therapy. Hypoglycemia also has a substantial impact on patients’ functioning and well-being, and reducing hypoglycemia would result in improved quality of life for patients with diabetes.
Conclusion
The results of this study highlight the substantial economic burden of insulin-related hypoglycemia in Denmark, and allows the evaluation of how hypoglycemia rates affect the healthcare budget and how the choice of insulin could lead to substantial budget savings. The results may aid clinicians and budget holders in their choice of insulin treatment by taking into account the hypoglycemia profile of the insulin and the likely offset of costs achieved by reducing hypoglycemia rates.
Transparency
Declaration of funding
This study was funded by Novo Nordisk.
Declarations of financial/other relationships
The authors have no other relevant affiliations or financial involvements with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript, apart from those disclosed. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Notes
Notes
a Percentages do not add up to 100% because some people were given more than one treatment for the same hypoglycemic episode (combination therapy).
b This was a weighted average between 52% of patients in the human insulin arm experiencing 1.12 episodes per patient-week and 48% of patients in the insulin analog arm experiencing 1.05 episodes per patient-week.
References
- American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care 2014;37(Suppl 1):S14-S80
- Danish Diabetes Association. Diabetes in Denmark. http://www.diabetes.dk/presse/diabetes-i-tal/diabetes-i-danmark.aspx. Accessed February 2016
- Statistics Denmark. StatBank Denmark. Population of all Denmark, quarter 4 2012. http://www.statbank.dk. Accessed June 2016
- Statens Serum Institute. Dataleverancer og Lægemiddelstatistik [Data Supplies and Medicines Statistics]. Copenhagen, Denmark; 2013. http://medstat.dk. Accessed June 2016
- Dansk Endokrinologisk Selskab. Kliniske retningslinier for behandling af voksne med Type 1 diabetes. http://www.endocrinology.dk/Kliniske%20retningslinier%20-%20DM%20type%201.pdf. Accessed December 2016.
- Dansk Endokrinologisk Selskab. Insulinbehandling af patienter med type 2-diabetes, 2014 revision. http://www.endocrinology.dk/PDF/InsulinbehandlingDM2rev2014.pdf. Accessed December 2016.
- Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003;26:1902-12
- Brod M, Christensen T, Thomsen TL, et al. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health 2011;14:665-71
- Heller SR SR, Frier BM, Herslov ML, et al. Severe hypoglycaemia in adults with insulin-treated diabetes: impact on healthcare resources. Diabet Med 2016;33:471-7
- Hatting NP, Mikkelsen S. Treatment of hypoglycaemic diabetics in a prehospital setting is safe. Dan Med J 2015;62:A5044
- Jensen MM, Pedersen-Bjergaard U. Self-reported frequency and impact of non-severe hypoglycemic events in insulin-treated diabetic patients in Denmark. Diab Manage 2015;5:67-78
- Domgaard M, Bagger M, Rhee NA, et al. Individual and societal consequences of hypoglycemia: A cross-sectional survey. Postgrad Med 2015;127:438-45
- Horvath K, Jeitler K, Berghold A, et al. Long-acting insulin analogues versus NPH insulin (human isophane insulin) for type 2 diabetes mellitus. Cochrane Database Syst Rev 2007:CD005613
- Monami M, Marchionni N, Mannucci E. Long-acting insulin analogues vs. NPH human insulin in type 1 diabetes. A meta-analysis. Diabetes Obesity Metab 2009;11:372-8
- Lane W, Bailey T, Gerety G, et al. SWITCH 1: Reduced hypoglycemia with insulin degludec (IDeg) versus insulin glargine (IGlar), both U100, in patients with T1D at high risk of hypoglycemia: A randomized, double-blind, crossover trial. Poster presented at the American Diabetes Association, 76th Annual Scientific Sessions, June 10–14, 2016, New Orleans, LA
- Wysham C, Bhargava A, Chaykin L, et al. SWITCH 2: Reduced hypoglycemia with insulin degludec (IDeg) versus insulin glargine (IGlar), both U100, in patients with T2D at high risk of hypoglycemia: A randomized, double-blind, crossover trial. Poster presented at the American Diabetes Association, 76th Annual Scientific Sessions, June 10–14, 2016, New Orleans, LA
- Parekh WA, Ashley D, Chubb B, et al. Approach to assessing the economic impact of insulin-related hypoglycaemia using the novel Local Impact of Hypoglycaemia Tool. Diabetic Med J Br Diabetic Assoc 2015;32:1156-66
- Sundhed.dk. Diabetes mellitus in children. https://www.sundhed.dk/sundhedsfaglig/laegehaandbogen/paediatri/tilstande-og-sygdomme/endokrinologi/diabetes-mellitus-hos-boern/. Accessed June 2016
- Ostenson CG, Geelhoed-Duijvestijn P, Lahtela J, et al. Self-reported non-severe hypoglycaemic events in Europe. Diabetic Med J Br Diabetic Assoc 2014;31:92-101
- Pedersen-Bjergaard U, Kristensen PL, Norgaard K, et al. Short-term cost-effectiveness of insulin detemir and insulin aspart in people with type 1 diabetes who are prone to recurrent severe hypoglycemia. Curr Med Res Opin 2016;20:1-7
- Kristensen PL, Pedersen-Bjergaard U, Beck-Nielsen H, et al. A prospective randomised cross-over study of the effect of insulin analogues and human insulin on the frequency of severe hypoglycaemia in patients with type 1 diabetes and recurrent hypoglycaemia (the HypoAna trial): study rationale and design. BMC Endocr Disord 2012;12:10
- Pedersen-Bjergaard U, Kristensen PL, Beck-Nielsen H, et al. Effect of insulin analogues on risk of severe hypoglycaemia in patients with type 1 diabetes prone to recurrent severe hypoglycaemia (HypoAna trial): a prospective, randomised, open-label, blinded-endpoint crossover trial. Lancet Diabetes Endocrinol 2014;2:553-61
- Agesen RM, Kristensen PL, Beck-Nielsen H, et al. Effect of insulin analogues on frequency of non-severe hypoglycaemia in patients with type 1 diabetes prone to severe hypoglycaemia: The HypoAna trial. Diabetes Metab 2016;42:249-55
- Akram K, Pedersen-Bjergaard U, Borch-Johnsen K, et al. Frequency and risk factors of severe hypoglycemia in insulin-treated type 2 diabetes: a literature survey. J Diabetes Complic 2006;20:402-8
- Novo Nordisk. Data on file, Available on request.
- International Diabetes Federation (IDF). Diabetes Atlas, Seventh Edition, 2015. http://www.diabetesatlas.org/. Accessed December 2016. Diabetes Atlas, Seventh Edition; 2015
- Geddes J, Schopman JE, Zammitt NN, et al. Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. Diabetic Med J Br Diabetic Assoc 2008;25:501-4
- Edridge CL, Dunkley AJ, Bodicoat DH, et al. Prevalence and incidence of hypoglycaemia in 532,542 people with Type 2 diabetes on oral therapies and insulin: a systematic review and meta-analysis of population based studies. PLoS One 2015;10:e0126427
- Khunti K, Alsifri S, Aronson R, et al. Rates and predictors of hypoglycaemia in 27 585 people from 24 countries with insulin-treated type 1 and type 2 diabetes: the global HAT study. Diabetes Obesity Metab 2016;18:907-15
- Brod M, Wolden M, Christensen T, et al. Understanding the economic burden of nonsevere nocturnal hypoglycemic events: impact on work productivity, disease management, and resource utilization. Value Health 2013;16:1140-9
- Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015;38:140-9
- Brod M, Rana A, Barnett AH. Impact of self-treated hypoglycaemia in type 2 diabetes: a multinational survey in patients and physicians. Curr Med Res Opin 2012;28:1947-58
- Peyrot M, Barnett AH, Meneghini LF, et al. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabetic Med J Br Diabetic Assoc 2012;29:682-9
- Leiter LA, Yale J-F, Chiasson J-L, et al. Assessment of the impact of fear of hypoglycemic episodes on glycemic and hypogycemia management. Can J Diabetes 2005;29
- Willis WD, Diago-Cabezudo JI, Madec-Hily A, et al. Medical resource use, disturbance of daily life and burden of hypoglycemia in insulin-treated patients with diabetes: results from a European online survey. Expert Rev Pharmacoecon Outcomes Res 2013;13:123-30
- Bilde L. International sammenligning af akut ambulancetjeneste. En foranalyse vedrørende finansieringsmæssige og økonomiske aspekter. December 2003. http://www.kora.dk/media/529721/dsi-1422.pdf. Accessed February 2016
- Danmarks Statistik. Forbrugerprisindeks. http://dst.dk/da/Statistik/emner/forbrugerpriser/forbrugerprisindeks. Accessed February 2016
- The Danish Health Data Authority. DRG-takster 2015. http://sundhedsdatastyrelsen.dk/da/afregning-og-finansiering/takster-drg/takster-2015. Accessed February 2016
- Lyngsie PJ, Lopes S, Olsen J. Incidence and cost of hypoglycemic events requiring medical assistance in a hospital setting in Denmark. J Comp Eff Res 2016;5:239-47
- Laegeforeningen. Honorartabel Dagtid 01-04-2016. http://www.laeger.dk/portal/pls/portal/!PORTAL.wwpob_page.show?_docname=11179448.PDF. Accessed April 2016
- Danish Medicines Agency. Prices & Reimbursement. Price of GlucaGen. http://www.medicinpriser.dk/?lng=1. Accessed February 2016
- Danish Medicines Agency. Prices & Reimbursement. Price of glucose-Na-K. http://www.medicinpriser.dk/?lng=1. Accessed February 2016
- Matas. Matas Sports Care Druesukker Pebermynte 100 tabl. https://www.matas.dk/matas-sports-care-druesukker-pebermynte-100-tabl. Accessed February 2016
- Nomeco. MaerkevareSortiment. http://service.nomeco.dk/webdoc/mrkkat.pdf. Accessed February 2016