Abstract
Background: While the impact of COPD in Western-Europe is known, data from Eastern-Europe is scarce. This study aimed to evaluate clinical characteristics, treatment patterns, and the socio-economic burden of COPD in Eastern-Europe, taking Bulgaria as a reference case.
Methods: A representative sample of Bulgarian patients with COPD was randomly chosen by pulmonologists, based on the following inclusion criteria: COPD diagnosis with at least 1 year of living with COPD, ≥40 years of age, and use of COPD medication. Patient characteristics, treatment, quality-of-life, healthcare resource use, and costs were systematically assessed.
Results: A total of 426 COPD patients were enrolled. Approximately 69% were male, 40% had occupational risk factors, 45% had severe and 11% had very severe COPD. Mean CAT scores were 13.80 (GOLD A), 21.80 (GOLD B), 17.35 (GOLD C), and 26.70 (GOLD D). Annual per-patient costs of healthcare utilization were €579. Yearly pharmacotherapy costs were €693. Indirect costs (reduced and lost work productivity) outnumbered direct costs three times.
Conclusions: Bulgaria has relatively high percentages of (very) severe COPD patients, resulting in considerable socio-economic burden. High smoking rates, occupational risk factors, air pollution, and a differential health system may be related to this finding. Eastern-European COPD strategies should focus on prevention, risk-factor awareness, and early detection.
Keywords:
Introduction
Worldwide, the prevalence of chronic obstructive pulmonary disease (COPD) is high, with an estimated prevalence of 11.7% (8.4–15.0%) in 2010Citation1–3. In Europe, COPD prevalence ranges between 2.1–26.1%Citation4, with hardly any information being available for Eastern Europe, while the available data are highly uncertainCitation5. Information is available for Greece, where the prevalence rate of COPD was defined as between 3–18.4%Citation6. Notably, Eastern European countries are countries with rapidly growing economies and aging populations, but still high rates of smoking, air pollution, and less well-developed healthcare systems compared to Western EuropeCitation7. An assessment of the clinical and economic burden of COPD is deemed essential for patients, healthcare professionals, decision-makers, and society. In particular, the indirect costs of COPD seem considerable, with significant impact on lost productivity, early retirement, and reduced ability to workCitation8–11. The Confronting COPD study confirmed the societal burden of COPD in North-America and (Western) EuropeCitation12. Notably, also this study did not include any Eastern European countries. Therefore, the impact of COPD in Eastern Europe remains uncertain and hampers targeted allocation of resources to reduce its burden on patients and societyCitation13. Moreover, without proper actions, inequality of respiratory care availability within Europe remains.
According to experts from the Bulgarian Society of Pulmonary Diseases, the total number of COPD patients in Bulgaria is ∼480,000, but only 25% of them are diagnosed, and no official studies or records exist. We aimed to determine the clinical and economic impact of COPD in Bulgaria.
Materials and methods
Study design
An observational study was conducted among COPD patients in the five main regions of Bulgaria: Northwestern, Northeastern, Southwest, Southeast Bulgaria, and Sofia-town in 2015 (see the Appendix).
Setting, patient recruitment, and sample size
COPD patients in Bulgaria are registered with a pulmonologist and they are obliged to visit their physician for regular checking at least twice per year, but in case of emergencies can visit them more frequently. Only pulmonologists are licensed to perform spirometry and change therapy. The patients’ GPs follow pulmonologist treatment instructions without changing the therapy. Therefore, we asked pulmonologists to choose COPD patients to include from their registries (every 5th, 10th, or 15th patient). A sample size of 405 COPD Bulgarian patients was considered nationally representative (see the Appendix for sample sizes per region). Sample sizes were determined based on expert-opinion-based estimated number of COPD patients and the number of citizens in every region. Statistical calculations were applied in order to define the sample size—the standard error was 5% and the probability was 99%.
Inclusion and exclusion criteria
Eligibility criteria were age ≥40 years, a physician and spirometry-confirmed COPD diagnosis (FEV1/FVC ratio <0.7) dated ≥1 year ago according to the revised GOLD recommendations (2011), and COPD pharmacotherapy prescriptions in the last year. The presence of other respiratory diseases, such as asthma, allergic rhinitis, lung carcinoma, sarcoidosis, bronchiectasis, pulmonary fibrosis, pulmonary tuberculosis, as well as exacerbation of COPD during the last month, were the main exclusion criteria.
Characteristics, risk factors, and clinical outcomes
Collected data included demographic characteristics (age, gender); smoking status (non, former, or current smoker and number of pack years); occupational status; occupational risk factorsCitation14–16; clinical data (COPD duration, spirometry, GOLD status based on airflow limitation (I–IV) and on combined assessment (A-D)Citation17); pharmacotherapy (2014 and 2015); comorbidity and co-medication; healthcare resource utilization (general practitioner [GP] visits, specialists’ visits, hospitalizations); disability; days off work due to COPD; and quality-of-life as measured using the COPD Assessment Test (CAT), specifically translated and validated for Bulgaria. Clinical data was provided by the pulmonologist and the patient provided the remaining data through an interview performed by the physician.
Health economic outcomes
Direct and indirect costs were calculated using a bottom-up approach. Healthcare resources consumed because of COPD were measured and valued. Costs paid by the National Health Insurance Fund (NHIF) and patients’ co-payment were identified separately. Comorbidity costs were not included. Hospitalization costs were calculated using the NHIF tariff at €45.13 per dayCitation18. GP visits costed €4.86, inclusive of a patient co-payment of €1.48Citation19. In Bulgaria, reimbursement of COPD drugs can be full or partial, at 75%. Salbutamol and some LABAs such as salmeterol, LABA + ICS, and ICS are 100% reimbursed. The NHIF pays 75% for LABAs (indacaterol, olodaterol), LAMA, LABA + LAMA, methylxantines, roflumilast, and 50% for systemic corticosteroids. This difference in reimbursement level is because pharmacotherapy primarily aimed at asthma is 100% reimbursed and targeted COPD therapy only 75%. This could be explained with Ordinance on the terms, rules, and procedure for regulation and registration of prices for medicinal products/2013. According to this ordinance the proposed level of reimbursement of the medicinal products for diseases with a chronic course, leading to severe disruptions in the quality-of-life or disablement and requiring prolonged treatment is 100%, and of the medicinal products for diseases with a chronic course and widespread prevalence is 75%Citation20.
Indirect costs were based on the number of days out of work (absenteeism) and reduced productivity (presentism). The human capital approach was applied to calculate absenteeism:
with GDP reflecting gross domestic product and total annual number of working days assumed at 252. Some patients reported reduced productivity (e.g. 50 or 70%) due to COPD while working. These losses were valued by multiplying the GDP per capita per year with the percentage reduced productivity. GDP per capita in 2015 in Bulgaria was €5,700Citation21.
Statistics
Descriptive statistics, non-parametric analysis, Kruskal-Wallis tests, and parametric analyses ANOVA were applied to assess correlations among data of interest.
Ethics
Every patient was acquainted with the study design and purposes and provided informed consent. The Bulgarian National Science Fund approved the study.
Results
Demographics
In total, 426 COPD patients were enrolled. The majority were 61–80 years, over two-thirds were male, 40% reported occupational risk factors, 74% were current or ex-smokers, and one quarter had been retired early due to COPD ().
Table 1. Demographics of the Bulgarian COPD study population (n = 426).
Clinical characteristics
Classified by GOLD I–IV, the majority had moderate (44%) or severe (45%) COPD, i.e. classified as GOLD II–III. About 60% were diagnosed less than 10 years ago. Based on the GOLD combined assessment, the majority had GOLD B or D ().
Table 2. Clinical characteristics of COPD patients in Bulgaria.
A predominant number of patients had CAT scores ≥10 at the time of study visit. CAT scores were normally distributed in both genders, as well per severity of the disease (A–D). Mean CAT score for males (n = 295) was 22.79 (SD = 6.87) and for females (n = 130) it was 22.30 (SD = 7.08; p = .503). Mean CAT scores for patients in classes A–D were 13.80 (SD = 6.28), 21.80 (SD = 5.68), 17.35 (SD = 4.12), and 26.70 (SD = 5.83), with the parametric ANOVA indicating statistically significant differences (p < .001). Over 80% had an mMRC scores ≥2.
Co-morbidity
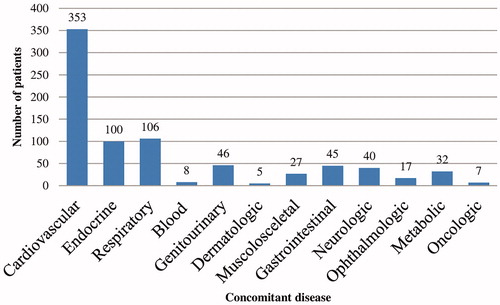
Within the COPD patients, 87% had at least one concomitant disease, and, of those, 78% had ≥2 comorbidities (). Most common were cardiovascular diseases (83%), followed by (other) respiratory (25%) and endocrine diseases (23%) (). Respiratory co-morbidity mostly comprised respiratory failure.
Table 3. Concomitant diseases in patients with COPD (n = 426).
Pharmacotherapy and costs
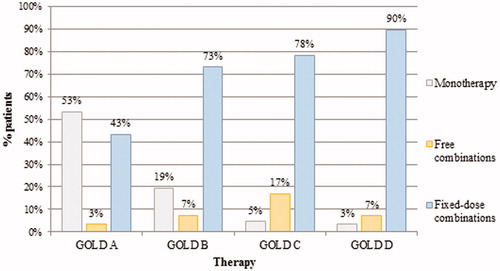
Fixed-dose combinations of inhaled corticosteroids and long-acting β2-agonists (ICS/LABA) were mostly prescribed in GOLD C and D patients; however, also a large part of GOLD A (43%) and B (73%) were prescribed LABA/ICS ().
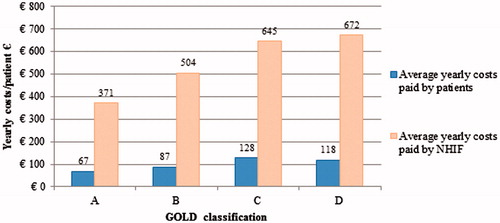
Mean annual pharmacotherapy costs were €693 (). Pharmacotherapy costs were rising with increasing COPD severity ().
Table 4. Healthcare resource use, direct, and indirect costs (€) per Bulgarian COPD patient per year.
Healthcare resources utilization and costs
The average number of days in hospital due to COPD, GPs’ visits, and specialists’ visits were 12.0, 2.2, and 2.4 visits, equaling costs of €545, €10.70, and €23.17, respectively (). Annual per-patient costs of healthcare utilization were €579.
The median hospitalization costs were €215.94 for stage B, €361.08 for stage C, and €451.35 for stage D (p < .001). Median GP visits costs for GOLD B, C, and D patients were €6.95, €10.11, and €12.34, respectively (non-parametric Kruskal-Wallis test, p < .001). Specialist visit costs were €15.89 for A, €19.03 for B, €22.18 for C, and €27.78 for D (p < .001).
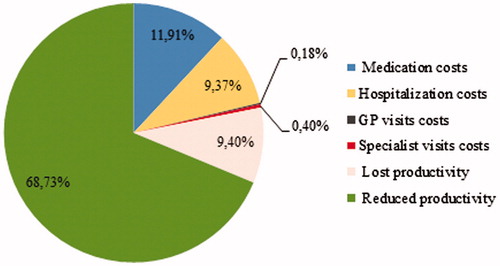
Indirect costs
The average number of days out of work per year for 84 patients reported by the patients was 24 (SD = 17), accounting for €546.63 (SD = 381.46). Reduced productivity was reported by 133 of the 249 patients (53.4%) of working-age (). The mean indirect costs among the patients in GOLD-stages A, B, and D were €575.11, €692.51, and €1349.29, respectively (non-parametric Kruskal-Wallis test, p < .001). Total direct medical and indirect non-medical costs for COPD are presented in . The indirect costs (78%) far outnumber the direct costs (22%).
Discussion
We aimed to assess the demographic, clinical, and economic characteristics of COPD patients in Bulgaria. It was found that most of the Bulgarian patients with COPD were male (69%), 40% were exposed to occupational risk factors, and 56% had severe or very severe COPD. Regarding economic impact, over 50% of the direct medical costs were spent on medication, and the remainder on healthcare provider visits and hospitalization. Notably, indirect costs (impaired and lost work productivity) were more than three times higher than the direct medical costs.
Our findings on the high percentage of patients being severe or very severe is remarkably different from studies in Western Europe. In Italy, the percentage of patients with moderate severity was greater than those with severe (53.7% vs 16.8%), while numbers in The Netherlands were even lower (15% severe; 3% very severe)Citation22. In Belgium, 41.8% had (very) severe COPD, while the situation in Eastern European country Serbia more closely resembles Bulgaria, with 61.8% (very) severeCitation23. The high rate of severe COPD in our study may be explained by late diagnoses (60% was diagnosed less than 10 years ago), high rates of under-diagnoses, high number of risk factors (smoking, air pollution, and occupational exposure), and non-compliance to therapy due to co-payments or inappropriate treatment. Regarding diagnosis, in Bulgaria, GPs cannot perform spirometry in patients with COPD-like symptoms. These patients are referred to a pulmonologist who has to conduct spirometry to confirm the diagnosis and to prescribe therapy. This may explain the fact that COPD patients in Bulgaria are diagnosed relatively late and in more severe stages.
While some studies recently reported that genders almost equalize, our study still reveals gender differences, possibly related to the significantly higher smoking prevalence in Bulgarian menCitation24. Of note, the percentage of never-smokers (26%) is higher than percentages in e.g. SpainCitation25 or DenmarkCitation26, possibly related to risk factors other than cigarette smokingCitation27. While in countries like Uganda indoor cooking seems to be responsibleCitation28, Bulgarian cooking traditions do not much differ from Western European countries. However, occupational risk factors and air pollution are higher, as of heavy former-Soviet industries. Indeed, 40% were exposed to occupational risk factors, comparable with a previous study on COPD in RussiaCitation29. Also, Bulgaria has the highest European mortality because of air pollution (http://env-health.org/IMG/pdf/heal_briefing_air_bulgaria_eng.pdf). Comorbidity patterns align with previous studies, with cardiovascular disease as a major comorbidityCitation30,Citation31.
Regarding healthcare utilization, the numbers of specialists’ visits and hospital admissions were significantly higher in Bulgaria than in Italy, at 99% vs 77% and 53% vs 33%, respectively, probably due to the greater COPD severity among Bulgarian patients. Severity, and outpatient and inpatient costs align with Serbia, confirming that Bulgaria may be representative for other Eastern European countriesCitation32.
Healthcare resource utilization costs were significantly lower than in the COPD uncovered surveyCitation33 for Brazil, China, Germany, Turkey, the US, and the UK, which could be explained by differences in healthcare systems and relatively low hospitalization and physician costs compared to medication prices in Bulgaria. With regard to medication, there seemed to be a profound over-use of LABA/ICS in GOLD A and B patients. Especially with the current evidence that ICS may be of limited value in COPDCitation34, this warrants active education of healthcare professionals.
Most COPD patients were of working-age, but COPD did not lead to much early retirement. Only 11% were early retired due to COPD and 20% had work absence, which could be explained by the low economic status of Bulgarian pensioners and the necessity of continuing working despite the disease. However, their work productivity was affected by the disease.
Indirect costs (lost productivity and reduced productivity) exceeded ∼3.5-times direct medical costs (hospitalization and visits), which is different from ratios calculated for seven other European countries (€1,091 vs €1,013)Citation35.
To our knowledge, this is the first study conducted at a national level in an Eastern European country, i.e. Bulgaria, focusing on the clinical and socio-economic impact of COPD. So far, such data were limited, and we anticipate that this study will make in-depth international comparisons with Western European countries possible. Moreover, it will serve as a starting point for national COPD strategies and as a role model for other Eastern European countries. A potential limitation is that the study was conducted in already diagnosed COPD patients, which makes the estimation of under-diagnosis rates impossible. Future studies should focus on the prevalence in the general population.
Regarding clinical practice, the results of this study stress the importance of improvement in diagnostic methods, active case finding, screening, as well as health educational programs on rational treatment in Bulgaria. Regarding national health policy, strategies should focus on early detection of COPD, awareness of occupational and environmental risk factors, and smoking prevention through active anti-tobacco campaigns. In addition, efforts are currently on the way for a better clinical characterization of the Eastern European COPD populationCitation36.
Conclusions
We demonstrated a significant clinical and socio-economic burden of COPD in Bulgaria. Besides high rates of smoking, occupational risk factors and air pollution may explain these findings. Notably, indirect costs outnumbered direct costs more than 3-fold. Bulgarian COPD strategies should focus on prevention, risk-factor awareness, and early detection.
Transparency
Declaration of funding
This study was financed by the National Science Fund in Bulgaria (Contract DFNI B-02/12 from December 12, 2014).
Declaration of financial/other relationships
The authors declare that they have no conflicting interests regarding the submitted work. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- Buist AS, McBurnie MA, Vollmer WM, et al. BOLD Collaborative Research Group. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 2007;370:741-50
- Bridevaux PO, Probst-Hensch NM, Schindler C. Prevalence of airflow obstruction in smokers and never smokers in Switzerland. Eur Respir J 2010;36:1259-69
- Halbert RJ, Natoli JL, Gano A, et al. Global burden of COPD: systematic review and meta-analysis. EurRespir J 2006;28:523-32
- Atsou K, Chouaid C, Hejblum G. Variability of the chronic obstructive pulmonary disease key epidemiological data in Europe: systematic review. BMC Med 2011;9:7
- Adeloye D, Chua S, Lee C, et al. Global health epidemiology reference group (GHERG). Global health epidemiology reference group (GHERG). Global and regional estimates of COPD prevalence: Systematic review and meta?analysis J Glob Health 2015;5:1-17
- Mitsiki E, Bania E, Varounis C, et al. Characteristics of prevalent and new COPD cases in Greece: the GOLDEN study, Int J Chron Obstruct Pulmon Dis 2015;10:1371-82
- Kavalski E. Balkansmoke: tobacco and the making of modern Bulgaria. EurAsiaStud 2014;66:1194-5
- Jansson SA, Backman H, Stenling A, et al. Health economic costs of COPD in Sweden by disease severity – Has it changed during a ten years period? Respir Med 2013;107:1931-8
- Patel JG, Nagar SP, Dalal AA. Indirect costs in chronic obstructive pulmonary disease: a review of the economic burden on employers and individuals in the United States. Int J Chron Obstruct Pulmon Dis 2014;9:289-300
- Trupin L, Earnest G, San Pedro M. The occupational burden of chronic obstructive pulmonary disease. Eur Respir J 2003;22:462-469
- van Boven JFM, Vegtera S, van der Molen T, et al. COPD in the working age population: the economic impact on both patients and government. COPD: J Chron Obstruct Pulmon Dis 2013;10:629-39
- Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects’ perspective of Confronting COPD International Survey. Eur Respir J 2002;20:799-805
- Cupurdija V. Economic impact of leading prosperity diseases: COPD in South East Europe. Front Public Health 2015;3:50
- Würtz ET, Schlünssen V, Malling TH, et al. Occupational COPD among Danish never-smokers: a population-based study. Occup Environ Med 2015;72:456-9
- Josephs L, Johnson M, Orlando R, et al. An observational study of age-related smoking status in COPD patients stratified by severity of airflow obstruction. Eur Respir J 2015;46:59
- Guillien A, Puyraveau M, Soumagne T, et al. Prevalence and risk factors for COPD in farmers: a cross-sectional controlled study. Eur Respir J 2015;47:16-18
- Pocket guide to COPD diagnosis, management and prevention, A guide for healthcare professionals. Updated 2015. http://www.goldcopd.it/materiale/2015/GOLD_Pocket_2015.pdf. Accessed June 25, 2016
- National Health Insurance Fund. National Framework contract. 2015. http://www.nhif.bg/web/guest/699. http://www.nsi.bg/bg. Accessed June 25, 2016
- Contract No RD-SB-01-2 from 29/12/2014 for acceptance on volumes and prices on medical care or 2015 between national Health case and Bulgarian medical union. 2015. http://www.nhif.bg/c/document_library/get_file?uuid=383568bd-ec85-4c46-882a-b79a9fd9417b&filename=DOGOVOR_RDNS012_ot_29122014_g_za_priemane_na_obemi_i_ceni_na_medicinskata_pomos_za_2015_g_mejdu_Naci.pdf&groupId=10139. Accessed June 25, 2016
- Ordinance on the terms, rules and procedure for regulation and registration of prices for medicinal products. Effective as from April 30, 2013. www.ncpr.bg. Accessed July 4, 2016
- Real GDP per capita and growth rate. 2016. http://www.nsi.bg/bg. Accessed June 25, 2016
- Hoogendoorn M, Feenstra TL, Schermer TR, et al. Severity distribution of chronic obstructive pulmonary disease (COPD) in Dutch general practice. Respir Med 2006;100:83-6
- Jakovljevic M, Lazic Z, Verhaeghe N, et al. Direct medical costs of COPD diagnosis and treatment, Eastern vs Western European country – examples of Serbia and Belgium. Health Econ Ther Pathw 2013;14:161-8
- Aryal S, Diaz-Guzman E, Mannino DM. COPD and gender differences: an update. Transl Res 2013;162:208-18
- van Boven JFM, Román-Rodríguez M, Palmer JF, et al. Comorbidome, pattern and impact of asthma-COPD overlap syndrome (ACOS) in real life. Chest 2016;149:1011-20
- Thomsen M, Nordestgaard, B, Vestbo J, et al. Characteristics and outcomes of chronic obstructive pulmonary disease in never smokers in Denmark: a prospective population study. Lancet Respir Med 2013;1:543-50
- Mehta AJ, Miedinger D, Keidel D, et al. SAPALDIA Team. Occupational exposure to dusts, gases, and fumes and incidence of chronic obstructive pulmonary disease in the Swiss cohort study on air pollution and lung and heart diseases in adults. Am J Respir Crit Care Med 2012;185:1292-300
- van Gemert F, Kirenga B, Chavannes N, et al. Prevalence of chronic obstructive pulmonary disease and associated risk factors in Uganda (FRESH AIR Uganda): a prospective cross-sectional observational study. Lancet Glob Health 2015;3:e44-51
- Mazitova NN, Saveliev AA, Berheeva ZM, et al. COPD and occupation: a retrospective cohort study of industrial workers. Arh Hig Rada Toksikol 2012;63:345-56
- Nagorni-Obradovic LM, Vukovic DS. The prevalence of COPD co-morbidities in Serbia: results of a national survey. NPJ Prim Care Respir Med 2014;24:14008
- Battaglia S, Basile M, Scichilone N, et al. Prevalence of Cco-morbidities and severity of COPD. COPD 2015;12:390-4
- Lazic Z, Gajovıc O, Tanaskovic I, et al. GOLD stage impact on COPD direct medical costs in elderly. J Health Behav Public Health 2012;2:1-7
- Fletcher M, Upton J, Taylor-Fishwick J, et al. COPD uncovered: an international survey on the impact of chronic obstructive pulmonary disease [COPD] on a working age population. BMC Public Health 2011;11:612
- Magnussen H, Disse B, Rodriguez-Roisin R, et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med 2014;371:1285-94
- The economic burden of lung disease. European Lung White Book. 2015. http://www.erswhitebook.org/chapters/the-economic-burden-of-lung-disease/. Accessed June 25, 2016
- Zbozinkova Z, Barczyk A, Tkacova R, et al. POPE study: rationale and methodology of a study to phenotype patients with COPD in Central and Eastern Europe. Int J Chron Obstruct Pulmon Dis 2016;11:611-22