Abstract
Introduction and objectives: This study has two objectives: (1) to examine healthcare resource utilization in heart failure (HF) patients; and (2) to examine the treatment costs associated with HF in China.
Methods: The data used in this study was from the 2014 national insurance database sponsored by the China Health Insurance Research Association (CHIRA), that covers national urban employees and residents. ICD-10 codes and keywords indicating heart failure diagnoses were used to identify patients with heart failure. Drug utilization, hospital visits, re-admission, and treatment costs in different service categories were examined.
Results: A total of 7,847 patients were included in this analysis, of which 1,157 patients had a 1-year complete follow-up period. In total, 48.16% of patients received the combination treatment of angiotensin-converting-enzyme inhibitor (ACEI)/angiotensin II receptor blockers (ARB) and beta-blockers (BB); and 22.87% of patients received the combination treatment of ACEI/ARB, beta-blockers and Mineralocorticoid receptor antagonists (MRAs). The annual treatment cost per patient with HF diagnosis was RMB 28,974, of which 66% was for inpatient care. The cost on HF medications accounted for 8.2% of annual cost. Treatment cost was much higher in provincial-level municipalities than that of prefecture-level and other cities.
Discussion and conclusion: Hospitalization is a major driver of HF treatment cost. Compared to the requirements in international treatment guidelines, HF standard of care medication treatment was under-utilized among HF patients in China. The high re-admission rate among Chinese patients indicates that the management of HF needs to be improved. The percentage of GDP spent on treating HF patients was much lower than that in the developed countries.
Introduction
Heart failure (HF) is a severe public health issue in different regions of the world including ChinaCitation1. A survey of Chinese residents between 35–74 years old showed that the prevalence of HF is 0.9%Citation2. HF accounts for 20% of hospitalizations and 40% of deaths due to cardiovascular diseasesCitation3, and is the second highest cause of deathCitation4 in China. As the aging population grows rapidly in the country, the prevalence, morbidity, and mortality of HF will continue to increaseCitation5.
HF also imposes a significant economic burden to patients, as well as a tremendous resource use to the healthcare system, and is a global problem. In Germany, heart failure has been the most common reason for hospitalization in recent yearsCitation6. In 2006, the direct medical costs associated with heart failure in Germany were €2.9 billion, 45% of which was inpatient cost, and 21% of which was for physician office visits. In the US, cost per heart failure-related hospitalization was ∼$23,000 in 2005Citation7. Total direct costs for HF were between $60.2 billion and $115.4 billionCitation8. In addition, per a global assessment, the total direct and indirect costs associated HF annually were estimated at $5.4 billion in 2012 for ChinaCitation9. However, no local Chinese data has been employed to assess the healthcare cost and resource utilization of HF patients nationwide.
The pattern of healthcare utilization or expenditure in specific service categories of HF among Chinese patients has not been published in the literature. This study aims to estimate the economic burden of HF patients in China via the national medical insurance claims data. Specifically, this study has two objectives: (1) to examine healthcare resource utilization in HF patients; and (2) to examine the treatment costs associated with HF. The third-party payer’s perspective was adopted for this analysis. Our study aims to raise the public’s awareness of HF and guide government’s effort in improving HF treatments by providing the first nationwide real-world evidence on HF economic disease burden in China.
Methods
Overview
The data used in this study is from the national claims sampling database sponsored by the China Health Insurance Research Association (CHIRA) covering national urban employee and resident basic medical insurance beneficiaries. Under the universal coverage scheme, the database represents 0.5 billion of the urban population and 40% of the total population in China. The CHIRA database was created by a two-step sampling process. Patients were first sorted by descending ages, and then sampled by method of isometric mechanical sampling with a correspondent sample rate. The sample rate for municipalities and provincial capitals was 2% and prefecture-level cities 5%. After the patients are sampled, the whole continuous hospital visit claim records for a whole year were extracted. The CHIRA database is the first of its kind in China that contains 1-year consecutive claim records at the national level. We used the most recent data available in 2014 from the CHIRA database for this study, with HF patient claim records from 32 sampling cities, representing 2.1 million of the insured urban population in China.
Sample selection
ICD-10 codes and keywords indicating heart failure diagnoses were used to identify patients with heart failure. Specifically, patient records with the following ICD-10 codes of diagnoses were included: I50 (heart failure), I50.0 (congestive heart failure), I50.1(left ventricular failure), and I50.9 (heart failure, unspecified).
In addition, the following keywords, which appeared in primary or secondary diagnosis, were used to identify HF patients, including hear failure, chronic heart failure, left ventricular failure, cardiac insufficiency, chronic cardiac insufficiency, left cardiac insufficiency, left ventricular systolic dysfunction, and NYHA class II/III/IV.
Patients younger than 18 years were excluded.
Healthcare resource utilization and treatment cost
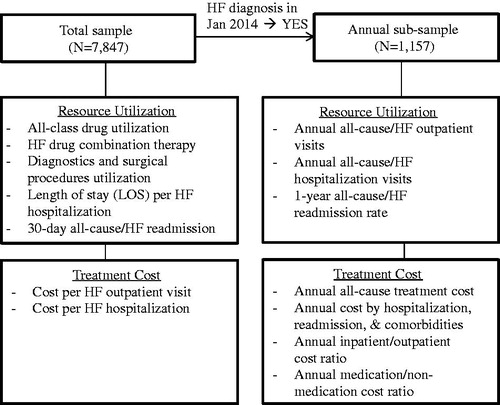
Two sample groups were employed to examine different parameters, as below ().
Total sample
In the analysis of healthcare resource utilization with the total sample, the most frequently utilized drug classes, diagnostics, and surgical procedures by HF patients were examined. International treatment guidelines recommend the standard-of-care use of angiotensin converting enzyme inhibitor (ACEI) or angiotensin receptor blockers (ARBs), beta-blockers, and mineralocorticoid receptor antagonist (MRAs)Citation10. The number and proportion of HF patients who were prescribed with guideline-recommended therapies on one or more hospital visits were also examined, i.e. use either the combination of ACEI/ARB and beta-blocker or the combination of ACEI/ARB, beta-blocker and MRA. In addition, length of stay (LOS) per HF hospitalization and 30-day all-cause/HF re-admission were examined.
In the analysis of treatment cost with total sample, both treatment cost per HF outpatient and cost per HF hospitalization were examined.
Annual sub-sample
In the analysis of hospital resource utilization with annual sub-sample, the number of all-cause/HF outpatient visits, inpatient visits per annum, and 1-year all-cause/HF re-admissions were examined.
In the analysis of treatment cost with annual sub-sample, the annual all-cause treatment costs by age, gender, and city tiers were examined. HF patients’ annual treatment cost with and without the occurrence of hospitalization, re-admission, and presence of major comorbidities (hypertension, diabetes, coronary heart disease, chronic kidney dialysis, and COPD) were compared. The annual inpatient/outpatient cost ratio and medication/non-medication cost ratio were also examined.
Data analysis
Descriptive statistics, including frequencies and percentages for categorical variables; mean for costs were used to evaluate the different variables as appropriate. The Student t-test or ANOVA was used to compare the costs between age groups, genders, and tiers of cities. Given the skewed distribution of costs, log-transformed costs were used in conducting the statistical tests. SAS was used to conduct the statistical analyses; p < .05 was considered statistically significant.
Results
Patient demographics and characteristics
There were 7,847 patients included in the total sample who had been treated for HF in 2014. The average age was 70.16 years (). Patients aged 65 years or older accounted for 69% of the patient population, and 50.8% of patients were males. Patients from municipalities, provincial capitals, and prefecture cities accounted for 41.27%, 28.36%, and 30.37% of the total sample population, respectively.
Table 1. Patient demographics.
For the annual sub-sample, 1,157 patients who had HF diagnosis in January 2014 were included, with claim records containing full-year HF treatment data. The patient demographics of the sub-sample were like that of the total sample.
Healthcare resource utilization and treatment cost
Total sample
In the analysis of healthcare resource utilization, the most frequently used drug class was antibiotics, with 70.76% of HF patients receiving the drugs (). The top five most utilized drug classes were used in over 50% of the patients. ARB was used in 37.51% of the patients; ACEi was used in 31.44% of the patients; 48.16% of patients received both ACEI/ARB and beta-blockers during their 1-year treatment period; 22.87% of patients received ACEI/ARB, beta-blockers, and MRAs. In the total sample, the top three diagnostic tests performed were glucose assay, potassium assay, and sodium assay. The top three surgical procedures performed were cardiorespiratory resuscitation, closed thoracic drainage, and tracheal intubation.
Table 2. Most frequently utilized drug classes by HF patients.
Among the hospitalized HF patients, the average length of stay was 12.04 days per HF hospitalization. The 30-day all-cause re-admission rate is 16.23%, of which HF-related is 4.13%.
In the analysis of treatment cost, the mean cost per HF outpatient visit is RMB 389 (USD 56); the mean cost per HF hospitalization is RMB 12,351 (USD 1,790).
Annual sub-sample
In the analysis of healthcare resource utilization, the average number of all-cause outpatient visits was 25.0 per patient within 1 year, of which 8.3 visits had a HF diagnosis. The average number of all-cause hospitalizations was 2.4 per patient within 1 year, of which 1.7 visits were HF-caused hospitalization. The 1-year all-cause re-admission rate was 68.98%, of which the HF-specific re-admission rate was 28.01%.
The annual all-cause treatment cost per patient with HF diagnosis was RMB 28,974 (USD 4,199). After log-transformation of the cost, there was no significant difference between patients in different age groups (p = .63), but a significant difference between patients younger than 65 years and patients of 65 years or older was observed (p = .000); increasing treatment costs were observed in patients who received care in different city tiers (p = .000). However, there was no significant difference in cost between male and female patients (p = .71) ().
Table 3. Annual cost per patient by demographics (n = 1,157).
The relationship between various impact factors and annual all-cause treatment cost was presented in . Patients with HF-caused hospitalization had significantly higher costs than patients without HF-caused hospitalization (p = .001). Patients with HF-caused re-admission had significantly higher costs than patients without HF-caused re-admission (p = .000). The number of comorbidities was positively associated with annual treatment cost (p = .000).
Table 4. Annual cost by variables per patient.
Among the annual all-cause treatment cost incurred by HF patients, 66% was for inpatient setting, and 34% was for outpatient setting. For the costs in difference service categories, 8.2% was for HF medications (HF Medication includes ACEi, ARB, MRA, BB, diuretics, organic nitrates, phosphodiesterase inhibitor, digitalis, trimetazidine, statins, and anti-arrhythmic drugs); and 45.90% was prescribed for other medications. In addition, surgical procedures (9.68%) and diagnostics (13.07%) were also major components of treatment cost in HF patients.
Discussion
Heart failure is a public health challenge in China and the world. However, in contrast with Europe and North America, there are few systematic registries or audit studies in Asian countries including ChinaCitation11. The present study is the first to examine the healthcare resource utilization and treatment cost in China using a national claims database.
In the analysis of drug utilization pattern, it was found that antibiotics were the most common drug class used among HF patients. One reason might be due to the over-utilization of antibiotics commonly observed in treating many diseases in ChinaCitation12. Another possible reason might be that more than 50% of HF patients had ≥1 hospitalization, and antibiotics were frequently used as anti-inflammatory medicine during and post surgical procedures and invasive diagnostics. Another finding was that 48.16% of patients received both ACEI/ARB and beta-blockers during their treatment, and only 22.87% of patients received ACEI/ARB, beta-blockers, and MRAs. In addition, HF medication including the above therapies only accounted for 8.2% of the total treatment cost. According to the international treatment guidelinesCitation10, such combined therapies are recommended to treat HF patients and prevent worsening of symptoms. Previous research also indicated that, when the drug compliance reached 88% or higher, the uneventful survival rate of patients was improved significantlyCitation13. This finding suggests it is imperative to improve treatment guideline adherence in the clinical practice for HF patients in China.
In terms of healthcare resource utilization among HF patients, all-cause re-admission rate within 1 year is 69% in China, the corresponding numbers in South Korea and Italy are 50% and 46.1%, respectivelyCitation14. The high re-admission rate benchmarking with developed countries where health resources are more adequate suggests the need to improve efficiency and outcome of HF treatment.
In the present study, the annual medical cost per HF patient is RMB 28,974 (USD 4,199). Compared with some other countries, the annual medical cost per HF patient in China is higher than that of Argentina, but much lower than that of the US, which are $2,258 and $12,931, respectivelyCitation15. This cost is much higher than that of other common chronic diseases. For example, the annual direct medical cost of diabetes is RMB 5,818 per patientCitation16 (USD 864), and RMB 13,566 (USD 1,966) for hypertensionCitation17. Treatment cost was much higher in municipalities than that of prefecture-level cities, suggesting poorer access to standard of care and lower awareness of HF in smaller cities and rural areas. In addition, the annual inpatient cost ratio for Chinese HF patients was higher than that of other cardiovascular diseases. The inpatient cost among diabetes and hypertension patients account for 15%Citation16 and 47% of their total cost, respectively, comparing with 66% in HF patients. The comparison showed that hospitalization is a major driver of HF treatment cost, and the finding is consistent with previous studiesCitation18.
There are several limitations in the present study. First, given that the database does not contain information to differentiate patients diagnosed with HF patients diagnosed in January 2014 from those diagnosed prior to January, the effect of disease history and stages of disease could not be examined. Second, the time horizon used in the present study is 1 year. It would be informative to compare the annual cost with cost of longer terms, e.g. 5 or 10 years, to observe the change in cost over time. Third, CHIRA claim database does not contain clinical and diagnostic tests measures such as NYHA classification, LEVF level, etc., so no outcome data is available to assess the link between drug and healthcare resource utilization to treatment outcome. Lastly, the present study did not examine the indirect cost, such as loss in productivity due to HF, which would have been combined with the current findings to estimate the burden to society as a whole. Further investigation can be conducted to understand the effect of treatment cost and healthcare resource utilization (e.g. HF drug combination therapy) on patient treatment outcome, and also to examine the indirect cost burden incurred by HF patients from the societal perspective.
Conclusion
The economic burden of heart failure is tremendous in terms of healthcare costs and resource utilization, and hospitalization is the major contributor to HF treatment burden. As heart failure becomes increasingly prevalent in China, it is imperative for clinicians to treat HF patients more effectively with interventions targeting reducing hospitalization and improving patient outcome. This analysis also indicated that HF treatments in China have low adherence to clinical treatment guidelines, which requires significant education to both clinicians and patients to improve compliance to standard of care in heart failure.
Transparency
Declaration of funding
Novartis AG sponsored this study.
Declaration of financial/other relationships
JH, HY, and JX received research funding from Novartis AG. QN and MZ are employees at Novartis AG. However, the study is not focused on specific products of Novartis AG. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- Mendez GF, Cowie MR. The epidemiological features of heart failure in developing countries: a review of the literature. Int J Cardiol 2001;80:213-19
- Gu DF, Huang GY, He J, et al. Investigation of prevalence and distributing feature of chronic heart failure in Chinese adult population. Chin J Cardiol 2003;31:3-6
- Qian JF, Jiang H, Ge JB. The epidemiology and current therapy of chronic heart failure in China. Chin J Clin Med 2009;16:700-3
- The US Centers for Disease Control and Prevention. CDC in China: factsheet. Centers for Disease Control and Prevention. Atlanta, USA. http://www.cdc.gov/globalhealth/countries/china/pdf/china.pdf. Accessed July 21, 2016
- Fu R, Xiang J, Bao H, et al. Association between process indicators and in-hospital mortality among patients with chronic heart failure in China. Eur J Public Health 2015;25:373-8
- Neumann T, Biermann J, Erbel R, et al. Heart failure: the commonest reason for hospital admission in Germany: medical and economic perspectives. Dtsch Arztebl Int 2009;106:269-75
- Wang G, Zhang Z, Ayala C, et al. Costs of heart failure-related hospitalizations in patients aged 18 to 64years. Am J Manag Care 2010;16:769-76
- Voigt J, Sasha John M, Taylor A, et al. A reevaluation of the costs of heart failure and its implications for allocation of health resources in the United States. Clin Cardiol 2014;37:312-21
- Cook C, Cole G, Asaria P, et al. The annual global economic burden of heart failure. Int J Cardiol 2014;171:368-76
- McMurray JJ, Adamopoulos S, Anker SD, et al.; ESC Committee for Practice Guidelines. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2012;14:803-69
- Reyes EB, Ha JW, Firdaus I, et al. Heart failure across Asia: Same healthcare burden but differences in organization of care. Int J Cardiol 2016;223:163-7
- Yin X, Song F, Gong Y, et al. A systematic review of antibiotic utilization in China. J Antimicrob Chemother 2013;68:2445-52
- Wu JR, Moser DK, De Jong MJ, et al. Defining an evidence-based cutpoint for medication adherence in heart failure. NIH Public Access 2009;157:285-91
- Desai AS, Stevenson LW. Rehospitalization for heart failure: predict or prevent? Circulation 2012;126:501-6
- Nicholson G, Gandra SR, Halbert RJ, et al. Patient-level costs of major cardiovascular conditions: a review of the international literature. Clinicoecon Outcomes Res 2016;8:495-506
- Zhang Z, Chen J, Tang Z, et al. Direct medical costs of diabetes mellitus in China. Chin Health Resources 2007;10:162
- Liang X, Gu D, Zhang H, et al. Drug therapy and direct medical cost among community patients with hypertension. Chinese Preventive Medicine Journal (Chinese). 2011;8:732-736
- Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 2016;68:1476-88