Abstract
Aim: Patients with open-angle glaucoma (OAG) whose intraocular pressure is not adequately controlled by one medication have several treatment options in the US. This analysis evaluated direct costs of unilateral eye treatment with two trabecular micro-bypass stents (two iStents) compared to selective laser trabeculoplasty (SLT) or medications only.
Materials and methods: A population-based, annual state-transition, probabilistic, cost-of-care model was used to assess OAG-related costs over 5 years. Patients were modeled to initiate treatment in year zero with two iStents, SLT, or medications only. In years 1–5, patients could remain on initial treatment or move to another treatment option(s), or filtration surgery. Treatment strategy change probabilities were identified by a clinician panel. Direct costs were included for drugs, procedures, and complications.
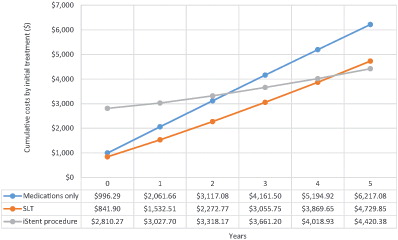
Results: The projected average cumulative cost at 5 years was lower in the two-stent treatment arm ($4,420) compared to the SLT arm ($4,730) or medications-only arm ($6,217). Initial year-zero costs were higher with two iStents ($2,810) than with SLT ($842) or medications only ($996). Average marginal annual costs in years 1–5 were $322 for two iStents, $777 for SLT, and $1,044 for medications only. The cumulative cost differences between two iStents vs SLT or medications only decreased over time, with breakeven by 5 or 3 years post-initiation, respectively. By year 5, cumulative savings with two iStents over SLT or medications only was $309 or $1,797, respectively.
Limitations: This analysis relies on clinical expert panel opinion and would benefit from real-world evidence on use of multiple procedures and treatment switching after two-stent treatment, SLT, or polypharmaceutical initial approaches.
Conclusions: Despite higher costs in year zero, annual costs thereafter were lowest in the two-stent treatment arm. Two-stent treatment may reduce OAG-related health resource use, leading to direct savings, especially over medications only or at longer time horizons.
Introduction
Glaucoma, which affects ∼60 million people worldwide and more than 2.2 million people in the US, is the second leading cause of blindness globally. Global trends show a growing prevalence of total glaucoma and open angle glaucoma (OAG) worldwideCitation1,Citation2. The most important risk factor for glaucoma is elevated intraocular pressure (IOP). Thus, a central goal of all glaucoma therapy is IOP reductionCitation3,Citation4. The management of patients with OAG should take into account the risks associated with therapy and other factors such as age, disease severity, comorbidities, tolerability of medications, desired post-operative IOP, and costCitation5–7. Treatment options for OAG have traditionally included medical therapy, laser trabeculoplasty, incisional glaucoma procedures, and cyclodestructive surgeryCitation8. Topical eye drops require adherence from patients and are not always well-tolerated. Laser therapy such as Selective Laser Trabeculoplasty (SLT) can provide a clinically significant reduction of IOP. Among OAG patients who range from newly diagnosed to those on maximally tolerated medical therapy, SLT results in a 6.9–35.9% intraocular pressure (IOP) reduction and complications are rareCitation9. However, the long-term results are questionable, as failure rates have been reported in the range of 33–74%Citation9–11.
The introduction of Micro-Invasive Glaucoma Surgery (MIGS) implants offers a viable alternative for patients with mild to moderate OAG. iStent (Glaukos Corporation, Laguna Hills, CA), one of the first and most commonly used MIGS devices, is a heparin-coated, non-ferromagnetic, titanium stent 1 mm in length and 0.3 mm in height. The iStent Trabecular Micro-Bypass is a “first in class” MIGS device that addresses mild-to-moderate open-angle glaucoma, thereby potentially filling an important gap in the current treatment algorithm for glaucomaCitation3. The stent is designed to cannulate Schlemm’s canal and create a communication from this space directly to the anterior chamber, allowing aqueous humor to egress into Schlemm’s canal more easily, thereby lowering IOP.
Understanding whether one of these treatment options confers a greater value relative to the other is important for many different stakeholders, including healthcare policy-makers, third-party payers, eye providers, and, most importantly, patients. With the dramatically increasing costs of healthcare in the US, it is essential to find ways to curtail costs, ideally without sacrificing the quality of care provided. This analysis evaluated the direct costs in the US of unilateral eye treatment with two trabecular micro-bypass stents (two iStents) compared to selective laser trabeculoplasty (SLT) or medications only over 5 years post-initiation.
Methods
An analysis of the cost impact of using the iStent device for treatment of patients whose OAG was not adequately controlled by one medication was built as a Markov model using TreeAge modeling software. The analysis was a payer-perspective, population-based, state-transition, probabilistic, cost-of-care model with an annual cycle and a 5-year time horizon. Direct costs were considered for OAG-related drugs, procedures, and complications for the treated eye. Three treatment arms were included in the analysis. Initiating treatment with an iStent procedure was compared to two alternate current treatment options: initiating treatment with an SLT procedure, or initiating treatment with medications alone.
Treatment transition probabilities
Treatment switching and other downstream filtering surgery procedures were permitted in the analysis in subsequent years (after 1 year post-initiation) (). Filtering surgery procedures considered included trabeculectomy, aqueous shunt, and an ab externo drainage device without an extraocular reservoir (Current Procedural Terminology [CPT] codes 66170; 66180 with or without 67225; and 66183, respectively); these procedures were selected and their distribution identified based on an analysis of the 2013 CMS Standard Analytical File. For each treatment arm in each cycle, the probabilities of downstream procedures, and the probabilities and numbers of concurrent medications were identified by a panel of clinicians experienced in the care of patients with glaucoma (). In establishing these probabilities, panel discussion acknowledged and accounted for the difference between effectiveness reported in clinical trials and effectiveness observed in real-world settings where patient circumstance and adherence to medication were less controlled and more varied.
Figure 1. Treatment transitions. Transitions between treatments were modeled annually and were only permitted in the directions of the arrows. Rectangular blue boxes represent initiating treatments considered in year 0. Grey ovals represent downstream treatments considered in years 1–5. Blue arrows represent the first transitions after the first model cycle (in year 0), and grey arrows represent downstream treatment transitions in subsequent cycles (years 1–5). SLT: selective laser trabeculoplasty.
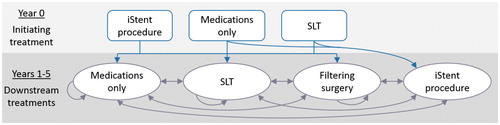
Table 1. Percentage of uncontrolled OAG patients receiving therapies.
Medications use
Medications considered in this analysis were prostaglandins, beta-blockers, carbonic anhydrase inhibitors, and alpha adrenergic agonists (). The analysis allowed for treatment with a mix of medications only, and for concurrent medication(s) use with downstream iStents, SLT, or filtering surgery procedures. During each cycle, patients being treated with iStents, SLT, or filtering procedures could have 0–4 concurrent medications, and patients being treated with medications-only treatment could have 2–4 concurrent medications. The market shares for drug manufacturers (branded and/or generic) within each class of drug were from 2014 IMS data.
Table 2. Use of concurrent and standalone medications.
Direct costs
Drug acquisition costs were from 2016 RED BOOK. Drug dosages from package inserts for each drug were applied. Calculations for liquid mediation use rate assumed 20 drops per mL based on previously published analyses of glaucoma drug costs and liquid medications wastage with patient administrationCitation11–13. These data, along with medications use treatment patterns, were used to derive the annual costs for glaucoma medications ().
Table 3. Inputs.
Costs of procedures were from the 2016 Outpatient Prospective Payment System (OPPS) Limited Data Set (LDS) (). Complication costs were $0 for both the iStent and SLT procedures based on published literature that demonstrated that complications risks with either were very lowCitation14–16. Complications costs with filtering surgeries were based on an analysis of the 2013 CMS Standard Analytical File. All costs are reported in 2016 US dollars using the consumer price indices reported by the US Bureau of Labor StatisticsCitation17. Later-year costs were discounted to year 0 using an annual time preference discount rate of 3% in accordance with the Good Research Practices for Cost-Effectiveness Analysis Alongside Clinical Trials report by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR)Citation18.
Sensitivity analyses
One-way sensitivity analyses were conducted to assess the effect of input uncertainty on the model’s results. Each input was varied across a range of values, and the resulting changes in the modeled 5-year cumulative costs were evaluated. Complication costs for all years were varied together for each treatment. Complication costs with the SLT procedure or the iStent procedure were varied between zero (basecase), and 50% of the basecase complication costs with filtering surgery (). Medication costs were varied together as a group by ±25%. The annual time preference discount rate was varied between 1–5% in accordance with ISPOR guidelines. The probability of downstream procedures (SLT, filtering surgery, or iStent procedure) after initial treatment in each treatment arm was varied by ±50%. All other cost variables were adjusted independently by ±25%. The maximum variation in results due to inputs uncertainty was identified, as were the inputs whose uncertainty range most influenced the results.
Results
The cumulative total costs over 5 years for patients initiating treatment with medications only, SLT, and iStent procedures were $6,217.08, $4,729.85, and $4,420.38 per patient on average, respectively (). Cumulative cost-savings over 5 years with the iStent procedure compared to medications only was estimated at $1,796.70 per patient on average. The cumulative cost with the iStent procedure was approximately equivalent to SLT only at 5 years ($309.47 lower with the iStent procedure).
Of the three treatment options, the initial year 0 cost was highest with the iStent procedure, due to initial device acquisition cost and lowest with SLT. These were offset by the annual marginal costs after initial treatment (years 1–5), which were lowest with the iStent procedure, and highest with medications only (). Costs in each year following SLT or medications only initial treatments were more than double that of the iStent procedure. In the first following year (year 1), the annual marginal cost was 3.2-times higher with SLT, and 4.9-times higher with medications only, compared to the iStent procedure.
Table 4. Annual marginal costs.
One-way sensitivity analyses identified the variables whose uncertainty most influenced the results (). These demonstrated that the cost of the iStent procedure, cost of medications, and probability of downstream procedures in the SLT procedure arm were the variables whose uncertainty most influenced the cost-comparison between the iStent procedure and SLT (). For the cost-comparison between the iStent procedure and medications-only, the variables whose uncertainty had the most effect were the cost of medications, cost of the iStent procedure, and probability of downstream procedures in the iStent procedure arm ().
Figure 3. Tornado diagram. (a) Incremental 5-year costs difference with the iStent procedure compared to SLT. (b) Incremental 5-year costs difference with the iStent procedure compared to medications only. SLT, selective laser trabeculoplasty. Dotted vertical line represents the base case result.
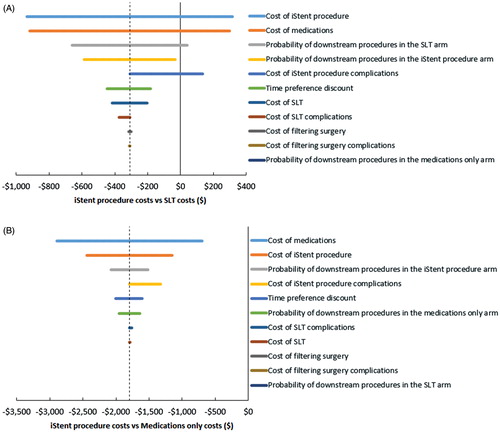
Table 5. Inputs uncertainty most influencing 5-year cumulative cost outcomes.
Discussion
Medications cumulative costs following initial treatment with the iStent procedure is cost-saving compared to initial treatment with medications-only by year 3. The cumulative cost-savings continue to increase in subsequent years. Cumulative costs with initial treatment with the iStent procedure reaches breakeven with initial SLT treatment between years 4 and 5, despite higher costs in year 0 with the iStent procedure. In combination with the lower annual marginal costs in years 1–5 after iStent procedure compared to medications-only initial treatment strategies, this suggests that analyses with longer time horizons than 5 years may show the iStent procedure to be increasingly cost-saving compared to SLT. Further research is needed to test these expectations and confirm these results in real-world settings. Despite higher costs in year zero, annual costs thereafter were lowest in the two-stent treatment arm. Five-year cumulative costs in the two-stent treatment arm were approximately equivalent to the SLT arm, and showed savings compared to the medications only arm. Two-stent treatment may reduce OAG-related health resource use, leading to direct savings, especially over medications only or at longer time horizons.
There are several study limitations that need to be acknowledged. While we were able to identify reasonable estimates of cost, in the absence of long-term comparative data, treatment transition probabilities were determined by a panel of clinicians experienced in the treatment of glaucoma. These probabilities are based on years of clinical experience, but are still theoretical. These inputs, and therefore this analysis, could be strengthened with real-world evidence. For all model assumptions, we were able to use one-way sensitivity analyses to examine the impact of changing the assumptions on the findings. The probability of downstream procedures (SLT, filtering surgery, or iStent procedure) after initial treatment in each treatment arm was varied by ±50% (). Even with this high range, the results remain relatively stable.
In addition, mortality was not considered in this 5 year model because glaucoma patients, regardless of treatment, have similar mortality rates. Also, only direct medical costs were considered. Glaucoma has a significant impact on HRQoL, even in the early stages of diseaseCitation19. HRQoL reflects a person’s wellbeing and focuses on dimensions of physical functioning, social functioning, mental health, and general health perceptions. Ongoing visual field loss can impair patients’ abilities to perform common daily activities (e.g. driving, walking, and reading). Vision loss may impose an increasing psychological burden on patients and their families. As vision worsens, patients experience increasing psychological burden, along with a growing fear of blindness, social withdrawal from impaired vision, and depressionCitation19.
This study confirms previous findings that OAG is a chronic disease which incurs substantial annual costs that increase over time as the disease progressesCitation19,Citation20. Inadequate treatment results in disease progression, leading to appreciable increases in resource utilization, costs for end-stage therapy, and indirect costsCitation21,Citation22. A medication regimen typically continues for the rest of a patient’s life. The successful management of a patient’s glaucoma, in terms of slowing the disease progression, is dependent on the patient’s ability to adhere to the recommended medication regimen and to persist with the therapy. In fact, recent research has shown that up to 90% of patients after 12 months in the US are non-adherent with their ocular hypotensive drug therapiesCitation23. The challenge with adherence has been documented in the literature, and is due to the inability to properly administer eye drops, cost considerations, and a lack of awareness of the slow but gradual loss of vision. Studies have shown that poor medication adherence is associated with worsening glaucoma. Progression rates, despite primarily medical treatment from landmark long-term longitudinal studies, are available and ranges up to 50% over 5 years or longerCitation24. This highlights the difficulty with medical adherence and the inadequacy of medical treatment to maintain patients in a safe IOP zone. Finally, caution is warranted when attempting to generalize these study findings to patients with other forms of glaucoma, those without health insurance, those outside of the US, and patients who don’t have access to iStent or SLT, as variables may differ considerably from those used in the model for these groups.
Conclusion
This analysis shows that, despite higher costs in year zero, annual costs thereafter were lowest in the two-stent treatment arm and showed savings compared to the medications only and SLT treatment arms. Two-stent treatment may reduce OAG-related health resource use, leading to direct savings, especially when compared to medications only and at longer time horizons.
Transparency
Declaration of funding
Research funding for this study was provided by Glaukos Corporation (Laguna Hills, CA).
Declaration of financial/other interests
JPB discloses consulting and lecture fees from Glaukos. AKK discloses being a speaker for Neomedix; trainer for Glaukos and Neomedix; receiving research support from Glaukos, Transcend Medical, Iridex, and InnFocus; and consulting for Iridex. LJK discloses speaker honoraria, stock, and being an employee and SAB member for Glaukos. LH discloses research support and consulting with Glaukos, SAB member for Sight Sciences, and Glaucoma Advisory Board member for Alcon. AJL and TMY are employees of Quorum Consulting, Inc. MJB is an employee of Glaukos. LBC discloses research support, consulting, and travel support from Allergan, research support from Valeant and InnFocus, and ownership interest in Mati Therapeutics. Peer reviewers on this manuscript have received an honorarium from JME for their review work, but have no other relevant financial relationships to disclose.
Previous presentation
This analysis was previously presented as a poster at the 2016 Annual International Meeting of the International Society for Pharmacoeconomics and Outcomes Research.
Acknowledgments
The authors would like to thank Heather Falvey for her assistance with writing and editing of the manuscript, and Jason Moore for his assistance with building the model structure.
References
- Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006;90:262-7
- Friedman DS, Wolfs RC, O’Colmain BJ, et al. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol 2004;122:532-8
- Corp G. In conjunction with cataract surgery, iStent reduces intraocular pressure (IOP) by improving aqueous humor outflow through the physiologic pathway. 2012
- Leske MC, Heijl A, Hyman L, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology 2007;114:1965-72
- Vizzeri G, Weinreb RN. Cataract surgery and glaucoma. Curr Opin Ophthalmol 2010;21:20-4
- Nelson P, Aspinall P, Papasouliotis O, et al. Quality of life in glaucoma and its relationship with visual function. J Glaucoma 2003;12:139-50
- Freeman EE, Munoz B, West SK, et al. Glaucoma and quality of life: the Salisbury Eye Evaluation. Ophthalmology 2008;115:233-8
- Prum BE Jr, Rosenberg LF, Gedde SJ, et al. Primary open-angle glaucoma preferred practice pattern® guidelines. Ophthalmology 2016;123:41-111
- Wong MO, Lee JW, Choy BN, Chan JC, Lai JS. Systematic review and meta-analysis on the efficacy of selective laser trabeculoplasty in open-angle glaucoma. Surv Ophthalmol 2015;60:36-50
- Freitas AL, Ushida M, Almeida I, et al. Selective laser trabeculoplasty as an initial treatment option for open-angle glaucoma. Arquivos Brasileiros de Oftalmologia 2016;79:417-21
- Stone JL, Robin AL, Novack GD, et al. An objective evaluation of eyedrop instillation in patients with glaucoma. Arch Ophthalmol 2009;127:732-6
- Rylander NR, Vold SD. Cost analysis of glaucoma medications. Am J Ophthalmol 2008;145:106-13
- Winfield AJ, Jessiman D, Williams A, et al. A study of the causes of non-compliance by patients prescribed eyedrops. Br J Ophthalmol 1990;74:477-80
- Fea AM, Belda JI, Rekas M, et al. Prospective unmasked randomized evaluation of the iStent inject® versus two ocular hypotensive agents in patients with primary open-angle glaucoma. Clin Ophthalmol 2014;8:875-82
- Realini T. Selective laser trabeculoplasty for the management of open-angle glaucoma in St. Lucia. JAMA Ophthalmol 2013;131:321-7
- Vold SD, MIGS Study Group. Prospective, randomized evaluation of micro-invasive glaucoma surgery (MIGS) with two trabecular micro-bypass stents vs prostaglandin in open-angle or pseudoexfoliative glaucoma or ocular hypertension naïve to therapy. Poster #39. American Glaucoma Society Annual Meeting. Coronado, CA; 2015
- Consumer Price Index - All Urban Consumers. 2016. http://data.bls.gov/cgi-bin/surveymost?cu. Accessed July 8, 2016
- Ramsey SD, Willke RJ, Glick H, et al. Cost-effectiveness analysis alongside clinical trials II-An ISPOR Good Research Practices Task Force report. Value Health J Int Soc Pharmacoeconom Outcomes Res 2015;18:161-72
- Varma R, Lee PP, Goldberg I, et al. An assessment of the health and economic burdens of glaucoma. Am J Ophthalmol 2011;152:515-22
- Lee PP, Walt JG, Doyle JJ, et al. A multicenter, retrospective pilot study of resource use and costs associated with severity of disease in glaucoma. Arch Ophthalmol 2006;124:12-9
- Reeder CE, Franklin M, Bramley TJ. Managed care and the impact of glaucoma. Am J Manag Care 2008;14:s5-s10
- Traverso CE, Walt JG, Kelly SP, et al. Direct costs of glaucoma and severity of the disease: a multinational long term study of resource utilisation in Europe. Br J Ophthalmol 2005;89:1245-9
- Nordstrom BL, Friedman DS, Mozaffari E, et al. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol 2005;140:598-606
- Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120:701-13; discussion 829–30