Abstract
Aims: Post-surgical pain experienced by patients undergoing total knee arthroplasty (TKA) can be severe. Enhanced recovery after surgery programs incorporating multimodal analgesic regimens have evolved in an attempt to improve patient care while lowering overall costs. This study examined clinical and economic outcomes in hospitals using liposomal bupivacaine (LB) for pain control following TKA.
Methods: This retrospective observational study utilized hospital chargemaster data from the Premier Healthcare Database from January 2011 through April 2017 for the 10 hospitals with the highest number of primary TKA procedures using LB. Within these hospitals, patients undergoing TKA who received LB were propensity-score matched in a 1:1 ratio to a control group not receiving LB. Outcomes included hospital length of stay (LOS), discharge status, 30-day same-hospital readmissions, total hospitalization costs, and opioid consumption; only patients with Medicare or commercial insurance as the primary payer for TKA were considered.
Results: The study population included 20,907 Medicare-insured patients (LB = 10,411; control =10,496) and 12,505 patients with commercial insurance (LB = 6,242; control = 6,263). Overall, LOS was 0.6 days shorter with LB (p < 0.0001), and patients who received LB were 1.6-times more likely to be discharged home (p < 0.0001). Total hospitalization costs for the TKA procedure were lower with LB for patients with both Medicare (–$616; P < 0.0001) and commercial insurance (–$775; p < 0.0001). Opioid consumption was lower with LB in both payer populations (p < 0.0001). No significant differences for 30-day readmissions were found.
Limitations: Costs were estimated using Premier charge-to-cost ratios and limited to goods and services recorded in the chargemaster. Findings from these 10 hospitals may not be representative of other US hospitals.
Conclusions: In a sub-set of 10 US hospitals with the highest use of LB for TKA, LB use was associated with shorter hospital LOS, increased home discharge, lower total hospitalization costs, and decreased opioid use after TKA.
Introduction
Approximately 700,000 total knee arthroplasty (TKA) procedures were performed in the US in 2012, making it one of the most common hospital-based surgical procedures in the countryCitation1. The number of TKA procedures grew by nearly 5% each year between 2003 and 20121 and is estimated to reach 3.48 million procedures in 2030Citation2, driven by an aging populationCitation3,Citation4, the increasing incidence of knee osteoarthritis (OA)Citation5, and the ability to perform TKA at an earlier stage of knee OACitation3,Citation4. More than half (55%) of TKA procedures were paid for by Medicare, and 37% were paid for by commercial health plansCitation1. Total Medicare hospital reimbursement for inpatient TKA and total hip arthroplasty (collectively known as total joint arthroplasty [TJA]) was $6.6 billion in 2013Citation6, and is likely to continue rising with the projected increases in TJA procedures.
To control these costs, the Medicare Comprehensive Care for Joint Replacement (CJR) model was instituted in 2016 and provides a bundled payment to the hospital for all care related to TJA from the time of admission until 90 days after dischargeCitation7. This value-based payment model is intended to reduce the costs of TJA while maintaining or improving quality of care by providing a financial incentive for hospitals to maximize the efficiency of care over a 90-day periodCitation3,Citation7. With this approach, hospitals receive a fixed amount from Medicare for performing a TJA procedure and providing all subsequent care for a period of 90 days after discharge (i.e. the episode of care) while meeting all current Medicare quality standardsCitation3,Citation7. Similarly, the Centers for Medicare & Medicaid Services has introduced the Bundled Payments for Care Improvement (BPCI) Advanced model, a voluntary episode payment model in which providers receive a single bundled payment for 29 inpatient and three outpatient clinical episodes over a 90-day episode duration; payment is linked to performance on seven quality measuresCitation8.
Many hospitals have responded to CJR, BPCI, and other value-based payment models from commercial health plans by attempting to reduce variable costs such as hospital length of stay (LOS)Citation9,Citation10. Because post-discharge care is a major determinant of the total costs for TJACitation11, hospitals must also reconsider routine transfers to skilled nursing facilities (SNFs), inpatient rehabilitation, and other post-acute care facilities after TJA because these costs are now included in the CJR bundled paymentCitation3, and the proportion of patients discharged home is critical to the clinical and financial viability of TJA programsCitation12,Citation13. Many commercial health plans have also implemented similar value-based bundled payment programs to cover an episode of care after TJA.
Total knee arthroplasty is a painful surgical procedureCitation14, with 47% of patients reporting moderate pain and 39% reporting severe-to-extreme pain in the 2 weeks after surgeryCitation15. Inadequate pain control after TKA can delay recoveryCitation16,Citation17, increase LOSCitation16–18, increase the likelihood of readmissionsCitation17, and increase total costsCitation17–19. Although opioids are routinely used in hospitals to manage acute post-surgical pain, this places patients at risk of opioid-related adverse events (ORAEs)Citation20,Citation21 such as nausea, vomiting, constipation, pruritus, sedation, and potentially fatal respiratory depression. According to two large studies of hospital administrative databases, 11.0–13.6% of patients who receive opioids for acute post-surgical pain have documented ORAEsCitation21,Citation22. Patients with ORAEs have a 50% longer LOSCitation21,Citation22, a 3.4-fold higher risk of inpatient mortalityCitation22, more frequent readmissionsCitation21,Citation22, and increased total costs of careCitation21,Citation22. Many risk factors for ORAEs, including advanced age and obesityCitation22, are common among patients undergoing TKACitation23.
Liposomal bupivacaine (LB; EXPAREL [bupivacaine liposome injectable suspension], Pacira Pharmaceuticals, Inc., Parsippany, NJ) is a non-opioid local anesthetic approved in October 2011 for single-dose infiltration into the surgical site for the management of post-surgical pain in a variety of surgical procedures, including TKACitation24. Unlike aqueous formulations of bupivacaine HCl, LB is formulated as a suspension of multivesicular liposomes containing bupivacaine that is released over a prolonged period, extending its duration of effect at the site of actionCitation24,Citation25. Although results from studies of local infiltration analgesia with LB for TKA have not been consistentCitation26,Citation27, recent findings from the PILLAR study, a randomized controlled trial, showed that local infiltration with vs without LB is associated with significant reductions in pain scores and total post-surgical opioid requirements and increased likelihood of patients remaining opioid-free after TKA when implemented using optimal techniques as part of a multimodal post-surgical pain management protocolCitation28. Retrospective studies have suggested that, in addition to providing effective analgesia, the use of LB is associated with reduced hospital LOS and greater likelihood of home discharge after TJA compared with no LBCitation29,Citation30.
The primary purpose of this study was to examine real-world clinical and economic outcomes achieved in the first 5 years of LB in-hospital use (i.e. since market launch in the US in April 2012) for primary TKA in high-use institutions.
Methods
This retrospective, comparative cohort study assessed data from the Premier Healthcare Database (Premier, Inc., Charlotte, NC), which contains administrative chargemaster data from more than 700 US hospitals that collectively capture approximately one in every five inpatient encounters. The analysis focused on patients who underwent inpatient primary TKA (International Classification of Diseases, Ninth Revision [ICD-9] procedure code, 81.54; ICD-10 procedure codes, 0SRC0J9, 0SRC0JA, 0SRC0JZ, 0SRD0J9, 0SRD0JA, 0SRD0JZ) between January 1, 2011, and April 30, 2017, with Medicare or a commercial health plan as the primary payer.
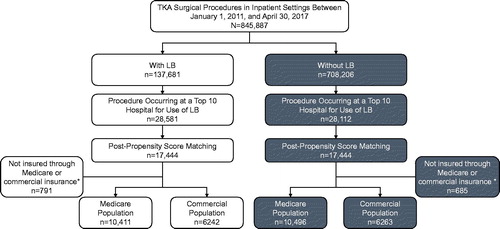
Because the outcomes of interest can vary substantially from one hospital to another, this study focused on the 10 hospitals with the highest use of LB for primary TKA during the study period of interest. This pragmatic approach was intended to provide a sufficiently large sample size for within-hospital comparisons of outcomes with and without LB (). LB use was identified in chargemaster data based on standard charge codes (e.g. 250250111850000) and charge-code descriptions (e.g. bupivacaine, EXPAREL VL 13.3MG/ML [1.3%] 20 ML).
Figure 1. Patient selection (inclusion/exclusion criteria). LB, liposomal bupivacaine; TKA, total knee arthroplasty. *Patients not insured through Medicare or commercial insurance were not included in the analyses because of the small sample size.
Once the 10 hospitals with the highest number of patients who received LB for primary TKA were identified, propensity score matching was used to identify control patients in the same hospital who underwent TKA and did not receive LB. Propensity score matching was based on age, sex, race, payer type, and Deyo-Charlson Comorbidity Index (DCCI) using a one-to-one nearest neighbor approach to matching. The overall study population, therefore, included 10 cohorts of patients (i.e. one from each hospital) and each hospital cohort had a sub-group of patients who received LB and a matched sub-group of control patients from the same hospital who did not receive LB. These analyses involved existing, deidentified administrative data and were, therefore, exempt from review by an institutional review board.
The outcomes of interest included hospital LOS, the proportion of patients discharged home, same-hospital readmissions within 30/60/90 days, total hospitalization costs (i.e. costs associated with the primary TKA procedure [supply, operating room, room and board, pharmacy, therapy, emergency room, laboratory, radiology, respiratory, and cardiology/electrocardiogram costs], excluding any readmissions or post-discharge care), and total opioid consumption during the hospital stay in oral morphine equivalent dosing (MED; see Supplementary Table 1 for oral MED conversions). Opioid use was identified based on items recorded in the chargemaster for the “Analgesic, narcotic” medication class. Total hospitalization costs were estimated using charge-to-cost ratios available in the Premier Healthcare Database for each item recorded in the hospital chargemaster, presented based on actual values for the time period of the visit. Covariates used in the analyses included patient demographics (e.g. age, gender, race), patient clinical characteristics (e.g. DCCI), and hospital characteristics (e.g. census region, number of beds).
Continuous variables were summarized using mean and SD, and categorical variables were summarized using frequency distributions and percentages. Outliers were removed if they were >3 SD from the meanCitation31; patients with $0 costs were excluded. Univariate and multivariable analyses were used to compare outcomes for patients treated with and without LB. Between-group differences were analyzed using the Pearson chi-square test for categorical variables and the Wilcoxon or Student t-test for continuous variables, depending on the normality of the data. Based on actual distributions, generalized linear mixed models (GLMMs) with log transformation were applied to LOS, costs, and opioid use, with gamma distribution controlling for demographic and clinical variables. GLMMs with logit link and binary distribution were used for home discharge, with adjustment for variables such as age, sex, race, and DCCI.
Results
Hospital matching and patient characteristics
Between January 1, 2011 and April 30, 2017, a total of 845,887 TKAs were performed at the selected hospitals; LB was used in 137,681 (16.3%) of these procedures (). The 10 hospitals with the highest number of primary inpatient TKA procedures that used LB had 28,581 such procedures, representing 20.8% of the total LB used for TKA. Most were larger (> 300 beds), urban, community hospitals located in the South census region; their characteristics are provided in Supplementary Table 2. No rural hospitals were included in this study. These hospitals all started using LB for TKA procedures between July 2012 and June 2014, after which LB use grew rapidly until it was used in ≥70% of the TKA procedures in those hospitals (Supplementary Figure 1).
After propensity score matching, the analysis included 17,444 patients treated with LB and 17,444 patients treated without LB; after excluding patients who were not insured through Medicare or commercial insurance, there were 16,653 patients treated with LB and 16,759 treated without LB, for a total of 33,412 patients (). In the LB group, 10,411 (62.5%) patients had Medicare as the primary payer for the TKA procedure, and 6,242 (37.5%) had commercial insurance. In the control group of patients treated without LB, 10,496 (62.6%) had Medicare, and 6,263 (37.4%) had commercial insurance. Patient demographics and clinical characteristics for Medicare patients with and without LB and commercial insurance patients with and without LB are shown in . Overall, the mean age was significantly higher in the Medicare group (72 years) than in the commercial insurance group (59 years; p < 0.001), as was the proportion of women (64.0% vs 57.1%; p < 0.001).
Table 1. Patient demographics and clinical characteristics.Table Footnotea
Outcomes
In univariate analyses, mean hospital LOS was significantly shorter by 0.5 days in patients treated with LB vs without LB in both the Medicare (2.4 [1.0] vs 2.9 [0.9] days; p < 0.001) and commercial insurance (2.1 [0.9] vs 2.6 [0.9] days; p < 0.001) groups; these findings were consistent across the 10 hospitals, with reductions in mean LOS with LB that varied between 0.3 and 0.8 days (). Findings from multivariable analyses, which controlled for demographic and clinical variables, were similar, and demonstrated that LOS was shorter by 0.6 days for patients treated with LB vs without LB in both the Medicare and commercial insurance groups ().
Table 2. Univariate analysis of mean LOS in the Medicare and commercial populations and LOS by hospital.
Table 3. Multivariable analysis of hospital LOS.
Among Medicare patients, 67.3% of those treated with LB (vs 57.9% without LB) were discharged home, whereas 26.7% treated with LB (vs 34.5% without LB) were discharged to a SNF, and 5.6% treated with LB (vs 7.0% without LB) were discharged to a rehabilitation center (). Similar findings were observed for patients with commercial insurance (). In multivariable analyses, patients treated with LB vs without LB were 1.6-times more likely to be discharged home in both the Medicare (odds ratio [OR] = 1.58) and commercial insurance (OR = 1.63) groups (). Despite the shorter LOS and greater proportions of patients discharged home with LB, there were no significant differences in same-hospital readmissions at 30/60/90 days in either the Medicare or commercial insurance groups ().
Figure 2. Univariate analyses of discharge location in the (a) Medicare and (b) commercial populations. In the Medicare population, 33 (0.3%) patients treated with LB and 54 (0.5%) treated without LB were discharged to locations other than home, an SNF, or a rehabilitation center; four patients in the LB group and 14 (0.1%) in the group without LB died. In the commercial population, four (0.1%) and 101 (1.6%) patients treated with and without LB, respectively, were discharged to other locations, and one and two patients, respectively, died. LB, liposomal bupivacaine; SNF, skilled nursing facility. p-value from analysis of variance for main effect of discharge status.
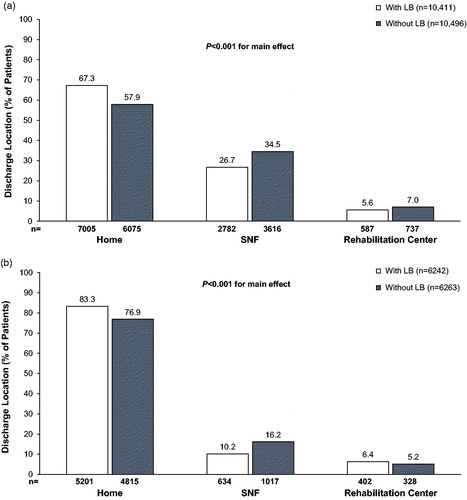
Table 4. Multivariable analysis of discharge to home status.
Table 5. Patients with same-hospital readmissions within 30/60/90 days.
Total hospitalization costs for the TKA procedure were significantly lower for patients treated with LB vs without LB in both the Medicare (mean [SD] = $15,103 [$4,461] vs $15,468 [$4,619]; p < 0.001) and commercial insurance (mean [SD] = $14,989 [$4,646] vs $15,564 [$4,866]; p < 0.001) groups (). The largest proportion of total hospitalization costs for TKA in both the Medicare and commercial insurance groups were related to supplies (e.g. knee implant), operating room (e.g. disposable supplies), room and board (e.g. daily cost of a hospital bed), pharmacy (e.g. medication), and physical or occupational therapy; additional information about the mean total costs of hospitalization by chargemaster cost category is provided in Supplementary Table 3. In multivariable analyses, mean total hospitalization costs were $616 lower for patients treated with LB vs without LB in the Medicare group, and $775 lower for patients treated with LB vs without LB in the commercial insurance group (each p < 0.0001; ).
Figure 3. Univariate analyses of total hospital costs in the Medicare and commercial populations. LB, liposomal bupivacaine.
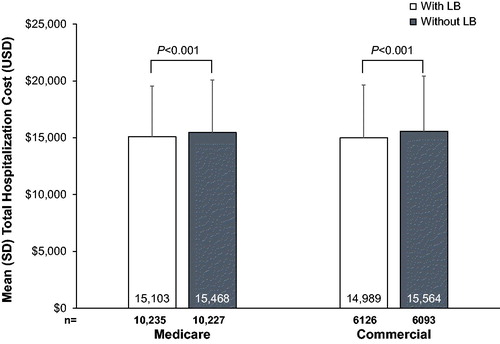
Table 6. Multivariable analysis of total hospitalization costs.
Inpatient opioid use was significantly lower for patients treated with LB vs without LB in both the Medicare (mean [SD] = 260.5 [198.0] vs 332.1 [253.9] mg MED) and commercial insurance (317.4 [220.7] vs 393.7 [266.7] mg MED) groups, representing reductions of 22% and 19%, respectively (). In multivariable analyses, when controlled for by LOS, mean inpatient opioid use was 69 mg MED lower for patients treated with LB vs without LB in the Medicare group and 64 mg MED lower for patients treated with LB vs without LB in the commercial insurance group (). When analyzed by day of administration (post-surgical days 1–4), inpatient opioid use was significantly lower with LB vs without LB on post-surgical days 1 and 2 in the Medicare group and on post-surgical days 1, 2, and 3 in the commercial insurance group (each p < 0.001; Supplementary Table 4). The most commonly used inpatient opioids were oral oxycodone 5 mg (18% of all inpatient opioid use), fentanyl 0.5 mg/mL (10% of all inpatient opioid use), and oxycodone/acetaminophen 5/325 mg (9% of all inpatient opioid use).
Figure 4. Univariate analyses of total opioid consumption in the Medicare and commercial populations. LB, liposomal bupivacaine; MED, morphine equivalent dose.
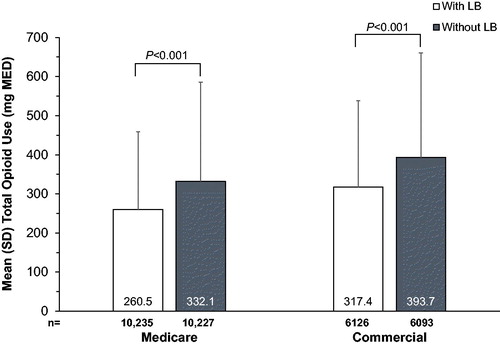
Table 7. Multivariable analysis of opioid consumption.
Additional information comparing patient demographics, clinical characteristics, LOS, discharge location, total hospitalization costs, and total inpatient opioid use for patients with LB and without LB within each of the 10 hospitals included in this study is provided in Supplementary Table 5.
Discussion
In the midst of the newly-implemented bundle payment programs for TKAs, hospitals are continually improving their enhanced recovery pathways to reduce costs and remain financially sound. Many hospitals have implemented multimodal analgesia programs to better manage acute post-surgical pain, minimize opioid use, and improve recovery after TKA.
In our retrospective analysis of real-world clinical and economic outcomes for patients undergoing primary TKA at hospitals with extensive use of LB, its use was associated with shorter hospital LOS, increased likelihood of discharge home, lower total hospitalization costs, and decreased inpatient opioid use, with no corresponding increase in same-hospital readmissions at 30/60/90 days, for patients with both Medicare and commercial insurance. These findings suggest that the cost of LB (∼ $319 for one 266-mg vial of the medication and associated suppliesCitation32) accounts for a small proportion of total hospitalization costs for TKA. The benefits resulting from utilization of LB in a multimodal analgesia protocol, such as shorter LOS and increased likelihood of discharge home, may favorably impact the profit and loss characteristics of a hospital’s TKA program under a bundled payment programCitation12. Discharge home would be expected to provide cost savings, given previous research showing that discharge to an SNF was associated with a greater risk of readmissions within 90 days, with the cost of readmissions estimated at $9,753 to $16,186Citation11.
Findings from our analyses are based on a relatively large sample size of patients with both Medicare and commercial insurance as the primary payer for the TKA procedure and a methodologically robust selection of patients in the control group using propensity score matching within each of the 10 hospitals examined. The use of matching helped to minimize differences in hospital characteristics and patient care processes that could contribute to differences in outcomes. Selecting hospitals with high volumes of LB use, and that, therefore, are likely familiar with the product, may increase the likelihood that optimal infiltration techniques are used. Findings from the PILLAR study (NCT02713490)Citation28 showed that infiltration technique is important to optimizing local infiltration analgesia with LB. Another strength of this study is the combined use of standard charge codes and charge-code descriptors, with >700 possible descriptions, which increased the robustness of our research methodology with respect to differentiating LB from other analgesics.
Although the retrospective, observational design is not able to adjust for all possible confounds, it provides realistic insight into clinical and economic outcomes that are difficult to assess under heterogeneous conditions imposed across individual randomized, controlled trial protocolsCitation33. Our results are consistent with findings from several retrospective chart reviews and randomized controlled trials with high internal validity, such as the PILLAR trialCitation28, examining the use of LB in TKACitation34–37. In PILLAR, local infiltration of LB plus bupivacaine HCl was compared to bupivacaine HCl aloneCitation28. Local infiltration with LB resulted in a 78% reduction in patient opioid consumption over 48 h, and 10% of patients treated with LB did not require any inpatient opioid rescue through 72 h after surgery. Observational studies examining the use of LB in TKA have also reported significant improvements in functional outcomes such as time to ambulation and ambulation distanceCitation35,Citation38,Citation39, shorter LOSCitation29,Citation35,Citation37,Citation38,Citation40, and increased likelihood of home dischargeCitation41, as well as lower hospitalization costs compared with other commonly used interventions intended to provide more prolonged analgesia (e.g. continuous peripheral nerve block [PNB])Citation38,Citation41,Citation42.
Our study is similar to a recent analysisCitation43 of the Premier Healthcare Database examining the real-world use and effectiveness—including opioid use, LOS, and total hospitalization costs—of LB for TKA. However, that study population included all hospitals in the Premier Healthcare Database (not only the 10 with the highest LB use) and was limited to a sub-set of patients undergoing TKA who received PNB, which was used as a proxy for “state-of-the-art pain management”. Our experience suggests that it is challenging to identify PNB in the Premier Healthcare Database since the Current Procedural Terminology (CPT) codes used by anesthesiologists to bill for services such as PNB are rarely reported in the chargemaster. Nevertheless, our findings are similar to those for the earlier analysis (e.g. median LOS of 2 days for LB vs 3 days for the control, total hospitalization costs ∼ $800 lower with LB, opioid use ∼80 mg MED lower with LB). However, clear differences are noted in the interpretation of these results. Whereas the conclusion drawn from the earlier analysis echoed the hypothesis that “LB has limited clinical influence on the studied outcomes”, we interpret our own findings as suggesting that LB was associated with meaningful clinical and economic outcomes; further reconciliation of these two studies may not be feasible.
Our study is limited by the lack of clinical data related to post-surgical pain, time to mobilization, and patient satisfaction, which are not recorded in the Premier Healthcare Database. The database is also unable to provide detailed information about the specific route of administration of local anesthetic (i.e. nerve block or local infiltration), infiltration site and techniques, including bridging with bupivacaine HCl or injectate volume expansion (e.g. admixing LB with bupivacaine HCl and/or saline) and how other medications were used (e.g. time of administration), introducing potential uncontrolled variability. Although there is no consensus regarding the most appropriate perioperative pain management approach for TKA, use of a well-defined control group, often found in prospective randomized controlled trials such as the PILLAR studyCitation28, may provide a different perspective and, when combined with real-world evidence, can help to inform clinical decision-makingCitation33. In the dataset examined, it is most likely that LB was used for periarticular injection, as previous studies have shown that peripheral nerve blocks are only used in 11–12% of TKA proceduresCitation44. Since patients in both groups were chosen from the same hospital over a relatively short timeframe (i.e. 5 years), it may be reasonable to assume that the use of specific regional anesthesia techniques such as local infiltration analgesia and nerve block was similar.
The findings observed in this study may not be solely attributable to LB, and the results obtained in the 10 hospitals with the highest use of LB for TKA (used in ≥70% of TKA procedures) may not be representative of other hospitals that do not use LB as extensively. Although one-quarter of hospitals in the Premier Healthcare Database are rural, only data from urban hospitals were used; therefore, our results may not be reflective of rural hospital environments, where distance to the facility may affect outcomes such as LOS, discharge location, and readmission. In addition, surgeons and anesthesiologists may have had differences in practice (e.g. experience, training, procedure duration) that could have affected findings. However, since patients in both groups were selected from the same hospital, they were likely to have been cared for by the same nurses and healthcare staff and to have received generally similar post-surgical care. Potential inconsistency across hospitals in defining a “day” could affect the clinical importance of the observed reduction in LOS. Furthermore, although cost savings are likely with outcomes such as increased discharge home under bundled payment programs, the costs associated with these outcomes are not included in the Premier Healthcare Database, which is limited to services provided during the inpatient stay and recorded in the chargemaster.
Conclusions
Effective post-surgical analgesia is a critical component for optimizing patient outcomes after TKA, allowing hospitals to provide high-quality care while controlling costs under surgical bundled payment programs. The use of LB as part of a multimodal analgesia program has previously been shown to improve post-surgical pain, and our real-world data suggest that its use in primary TKA is associated with shorter hospital LOS, increased likelihood of discharge home, decreased post-surgical opioid consumption, and lower hospitalization costs for both Medicare and commercial insurance plan participants. These results serve to further inform healthcare providers of the potential role of LB in improving clinical and economic outcomes for primary TKA in the hospital setting.
Transparency
Declaration of funding
This study was funded by Pacira Pharmaceuticals, Inc. Pacira Pharmaceuticals, Inc. participated in the study conception and design; collection, analysis, and interpretation of the data; and review of the manuscript. The authors were responsible for review and final approval to submit for publication.
Declaration of financial/other interests
CVA is a member of the Health Outcomes and Economics Advisory Board for Pacira Pharmaceuticals, Inc. SD and AK were employees of Pacira Pharmaceuticals, Inc. at the time of the study. JR has been a consultant for Pacira Pharmaceuticals, Inc. BTM has nothing to disclose. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Previous presentations
Data from this article were previously presented at the International Society for Pharmacoeconomics and Outcomes Research 21st Annual Meeting in Washington, DC (May 21–25, 2016).
Supplemental Material
Download MS Word (40.9 KB)Supplemental Material
Download MS Power Point (113.9 KB)Acknowledgements
Editorial support for development of this manuscript was funded by Pacira Pharmaceuticals, Inc. and provided by Krystina Neuman, PhD, at C4 MedSolutions, LLC (Yardley, PA), a CHC Group company, and Paul Cavanaugh, PhD, an employee of Pacira Pharmaceuticals, Inc.
References
- Fingar KR, Stocks C, Weiss AJ, et al. Most frequent operating room procedures performed in U.S. hospitals, 2003–2012: statistical brief #186. Healthcare Cost and Utilization Project (HCUP) statistical briefs. Rockville, MD: Agency for Healthcare Research and Quality (US), 2014, 1–15
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–5
- Bozic KJ, Ward L, Vail TP, et al. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res 2014;472:188–93
- Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 2009;467:2606–12
- Centers for Disease Control and Prevention. Vital Signs. Atlanta, GA: Arthritis in America. 2017. Available at: https://www.cdc.gov/vitalsigns/arthritis/index.html [Last accessed March 20, 2018]
- Centers for Medicare & Medicaid Services. New Medicare data available to increase transparency on hospital utilization. Baltimore, MD; 2015. Available at: https://www.cms.gov/newsroom/fact-sheets/new-medicare-data-available-increase-transparency-hospital-utilization [Last accessed February 12, 2018]
- Centers for Medicare & Medicaid Services. Comprehensive care for joint replacement model. Baltimore, MD; 2018. Available at: https://innovation.cms.gov/initiatives/cjr [Last accessed June 21, 2018]
- Centers for Medicare & Medicaid Services. BPCI Advanced. Baltimore, MD; 2018. Available at: https://innovation.cms.gov/initiatives/bpci-advanced [Last accessed July 6, 2018]
- Healy WL, Rana AJ, Iorio R. Hospital economics of primary total knee arthroplasty at a teaching hospital. Clin Orthop Relat Res 2011;469:87–94
- Auyong DB, Allen CJ, Pahang JA, et al. Reduced length of hospitalization in primary total knee arthroplasty patients using an updated enhanced recovery after orthopedic surgery (ERAS) pathway. J Arthroplasty 2015;30:1705–9
- Nichols CI, Vose JG. Clinical outcomes and costs within 90 days of primary or revision total joint arthroplasty. J Arthroplasty 2016;31:1400–06.e3
- Jubelt LE, Goldfeld KS, Blecker SB, et al. Early lessons on bundled payment at an academic medical center. J Am Acad Orthop Surg 2017;25:654–63
- Owens JM, Callaghan JJ, Duchman KR, et al. Short-term morbidity and readmissions increase with skilled nursing facility discharge after total joint arthroplasty in a Medicare-eligible and skilled nursing facility-eligible patient cohort. J Arthroplasty 2018;33:1343–7
- Gerbershagen HJ, Aduckathil S, van Wijck AJ, et al. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013;118:934–44
- Apfelbaum JL, Chen C, Mehta SS, et al. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 2003;97:534–40
- Baratta JL, Gandhi K, Viscusi ER. Perioperative pain management for total knee arthroplasty. J Surg Orthop Adv 2014;23:22–36
- Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 2017;10:2287–98
- Cherian JJ, Muzaffar A, Barrington JW, et al. Liposomal bupivacaine in total knee arthroplasty for better postoperative analgesic outcome and economic benefits. J Knee Surg 2016;29:180–7
- Elmallah RK, Cherian JJ, Pierce TP, et al. New and common perioperative pain management techniques in total knee arthroplasty. J Knee Surg 2016;29:169–78
- Oderda GM, Gan TJ, Johnson BH, et al. Effect of opioid-related adverse events on outcomes in selected surgical patients. J Pain Palliat Care Pharmacother 2013;27:62–70
- Minkowitz HS, Gruschkus SK, Shah M, et al. Adverse drug events among patients receiving postsurgical opioids in a large health system: risk factors and outcomes. Am J Health Syst Pharm 2014;71:1556–65
- Kessler ER, Shah M, Gruschkus SK, et al. Cost and quality implications of opioid-based postsurgical pain control using administrative claims data from a large health system: opioid-related adverse events and their impact on clinical and economic outcomes. Pharmacotherapy 2013;33:383–91
- Apold H, Meyer HE, Nordsletten L, et al. Risk factors for knee replacement due to primary osteoarthritis, a population based, prospective cohort study of 315,495 individuals. BMC Musculoskelet Disord 2014;15:217 [Epub]
- EXPAREL® (bupivacaine liposome injectable suspension). Full Prescribing Information. San Diego, CA: Pacira Pharmaceuticals, Inc., 2018
- Bergese SD, Ramamoorthy S, Patou G, et al. Efficacy profile of liposome bupivacaine, a novel formulation of bupivacaine for postsurgical analgesia. J Pain Res 2012;5:107–16
- Kuang MJ, Du Y, Ma JX, et al. The efficacy of liposomal bupivacaine using periarticular injection in total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2017;32:1395–402
- Zlotnicki JP, Hamlin BR, Plakseychuk AY, et al. Liposomal bupivacaine vs plain bupivacaine in periarticular injection for control of pain and early motion in total knee arthroplasty: a randomized, prospective study. J Arthroplasty 2018;33:2460–4
- Mont MA, Beaver WB, Dysart SH, et al. Local infiltration analgesia with liposomal bupivacaine improves pain scores and reduces opioid use after total knee arthroplasty: results of a randomized controlled trial. J Arthroplasty 2018;33:90–6
- Chughtai M, Cherian JJ, Mistry JB, et al. Liposomal bupivacaine suspension can reduce lengths of stay and improve discharge status of patients undergoing total knee arthroplasty. J Knee Surg 2016;29:224–7
- Cherian JJ, Barrington J, Elmallah RK, et al. Liposomal bupivacaine suspension can reduce length of stay and improve discharge status of patients undergoing total hip arthroplasty. Surg Technol Int 2015;27:235–9
- Howell DC, Rogier M, Yzerbyt V, et al. Statistical Methods in Human Sciences. New York: Wadsworth; 1998
- Corman S, Shah N, Dagenais S. Medication, equipment, and supply costs for common interventions providing extended post-surgical analgesia following total knee arthroplasty in US hospitals. J Med Econ 2018;21:11–18
- Frieden TR. Evidence for health decision making - beyond randomized, controlled trials. N Engl J Med 2017;377:465–75
- Snyder MA, Scheuerman CM, Gregg JL, et al. Improving total knee arthroplasty perioperative pain management using a periarticular injection with bupivacaine liposomal suspension. Arthroplast Today 2016;2:37–42
- Heim EA, Grier AJ, Butler RJ, et al. Use of liposomal bupivacaine instead of an epidural can improve outcomes following total knee arthroplasty. J Surg Orthop Adv 2015;24:230–4
- Emerson RH, Jr., Barrington JW, Olugbode O, et al. Femoral nerve block versus long-acting wound infiltration in total knee arthroplasty. Orthopedics 2016;39:e449–55
- Barrington JW, Olugbode O, Lovald S, et al. Liposomal bupivacaine: a comparative study of more than 1000 total joint arthroplasty cases. Orthop Clin North Am 2015;46:469–77
- Kirkness CS, Asche CV, Ren J, et al. Cost-benefit evaluation of liposomal bupivacaine in the management of patients undergoing total knee arthroplasty. Am J Health Syst Pharm 2016;73:e247–54
- Yu S, Szulc A, Walton S, et al. Pain control and functional milestones in total knee arthroplasty: liposomal bupivacaine versus femoral nerve block. Clin Orthop Relat Res 2017;475:110–17
- Surdam JW, Licini DJ, Baynes NT, et al. The use of Exparel (liposomal bupivacaine) to manage postoperative pain in unilateral total knee arthroplasty patients. J Arthroplasty 2015;30:325–9
- Kim K, Elbuluk A, Yu S, et al. Cost-effective peri-operative pain management: assuring a happy patient after total knee arthroplasty. Bone Joint J 2018;100-B:55–61
- Broome CB, Burnikel B. Novel strategies to improve early outcomes following total knee arthroplasty: a case control study of intra articular injection versus femoral nerve block. Int Orthop 2014;38:2087–9
- Pichler L, Poeran J, Zubizarreta N, et al. Liposomal bupivacaine does not reduce inpatient opioid prescription or related complications after knee arthroplasty: a database analysis. Anesthesiology 2018;129:689–99
- Cozowicz C, Poeran J, Memtsoudis SG. Epidemiology, trends, and disparities in regional anaesthesia for orthopaedic surgery. Br J Anaesth 2015;115(Suppl 2):ii57–67
