Abstract
Aims: This trial-based economic evaluation (EE) assesses from a societal perspective the cost-effectiveness of an intensive 3-day cognitive theory-based intervention (CDT), compared to care-as-usual, in patients with relapsing remitting multiple sclerosis (RRMS) and low disability (Expanded Disability Status Scale [EDDS] score < 4.0).
Materials and methods: The trial of the EE was registered in the Dutch Trial Register: Trial NL5158 (NTR5298). The incremental cost-effectiveness ratio (ICER) was expressed in cost on the Control sub-scale of the Multiple Sclerosis Self-Efficacy Scale (MSSES) and the incremental cost-utility ratio (ICUR) in the cost per Quality Adjusted Life Years (QALY) using the EQ-5D-5L. Bootstrap, sensitivity, and sub-group analyses were performed to determine the robustness of the findings.
Results: The two groups of 79 patients were similar in baseline characteristics. The base case ICER is situated in the northeast quadrant (€72 (40.74/€2,948)) due to a higher MSSES Control score and higher societal costs in the CDT group. The ICUR is situated in the northwest (inferior) quadrant due to losses in QALY and higher societal costs for the CDT group (−0.02/€2,948). Overall, bootstrap, sensitivity, and sub-group analyses confirm the base case findings. However, when the SF-6D is used as a study outcome, there is a high probability that the ICUR is situated in the northeast quadrant.
Limitations: The relative short follow-up time (6 months) and the unexpected increase in MSSES Control in the control group.
Conclusions: When using the EQ-5D-5L to calculate a QALY, CDT is not a cost-effective alternative in comparison to care as usual. However, when using self-efficacy or SF-6D as outcomes, there is a probability that CDT is cost-effective. Based on the current results, CDT for patients with RRMS clearly show its potential. However, an extended follow-up for the economic evaluation is warranted before a final decision on implementation can be made.
Introduction
Multiple sclerosis (MS) is a chronic disease of the central nervous system, with an estimated worldwide prevalence of 2.5 millionCitation1. Of these patients with MS, 85% have been diagnosed with relapsing remitting MS (RRMS) at onset. This type of MS is characterized by relapses that are followed by remissionsCitation2. Frequently reported problems are fatigue, pain, cognitive impairment, anxiety, and depressionCitation3. Due to the symptoms and unpredictability of the disease, patients with MS experience numerous problems in daily life. They might not able to continue working in paid jobs, doing usual household tasks, or taking care of children as healthy people of their age would doCitation4. Although there are various disease-modifying drugs available for the treatment of RRMS, the effectiveness of treatment and the resulting outcomes in individual patients are variable and unpredictable.
Self-efficacy is a psychological concept which is used to provide insight into the degree a person is confident to reach goalsCitation5. In patients with MS, low self-efficacy has been associated with low health-related quality-of-life (HRQoL) and less psychological adjustment. Several randomized clinical trials have been performed in the UK and US evaluating the effect on self-efficacy of non-pharmacological interventions in patients with MSCitation6–14. The interventions that were evaluated in five studies showed a significant positive effect on the improvement of self-efficacyCitation6,Citation7,Citation9,Citation10,Citation12. Other studies could not find a relevant difference between the treatment armsCitation8,Citation11,Citation13,Citation14. In the Netherlands, an intensive social cognitive theory-based intervention with the participation of supporting partners, the Can Do treatment (CDT), has been developed and evaluated through an uncontrolled observational study in patients with MSCitation15. The results of this study were promising: at the 6 months follow-up, control self-efficacy (i.e. confidence with managing symptoms and coping with the demands of illness) and mental HRQoL had improved by 24.8% and 22.3%, respectively, in the RRMS sub-group, and by 23.8% and 19.3%, respectively, in the low-disability group (Expanded Disability Status Scale [EDDS] score < 4.0). Comparable trends in time were observed in the effectiveness analyses of a randomized controlled trial in both the CDT and control groupCitation16. In the low-disability RRMS patients, an intensive social cognitive treatment improved self-efficacy control at 1 and 3 months, but not at 6 months compared with usual care.
Due to the continually ongoing developments of new and expensive treatment options, healthcare costs are increasing in western countries. As healthcare budgets are limited, however, there is a need for studies evaluating the cost-effectiveness of these newly-developed interventions, to keep healthcare sustainable into the future. This is also the case for chronic diseases like MS. The estimated average healthcare costs per RRMS patient range from 18,000–30,000 Euros per year in the Netherlands for those with EDSS scores lower than 4.0; these costs are higher than or comparable to other chronic diseasesCitation17. Healthcare costs are only part of the costs for society, because non-healthcare costs, such as the cost of productivity losses and informal care, must also be considered.
Based on the promising results of the single-arm studyCitation15 and the need for cost-effectiveness analyses, a randomized controlled study was designed to evaluate both the clinical and economic effectiveness of the CDT intervention as previously investigatedCitation15,Citation16. The current trial-based economic evaluation aims to evaluate the cost-effectiveness from a societal perspective in patients with RRMS with low disability. The results of the clinical effectiveness will be reported elsewhereCitation16.
Methods
Study design and participants
The current study describes the economic evaluation attached to a single-centre, parallel group, unmasked, randomized controlled trial (RCT) with two groups. Patients with MS were recruited by the National Multiple Sclerosis Foundation in the Netherlands. The Medical Ethics Committee in Tilburg (the Netherlands) has approved the protocol of the study (NL number: NL4220502812). The study was performed in agreement with the Declaration of Helsinki, version 2013Citation18. The trial of the EE was registered in the Dutch Trial Register: Trial NL5158 (NTR5298) (https://www.trialregister.nl). Detailed information on the methods of the trialCitation19 and the effectiveness study can be found elsewhereCitation16. The eligibility criteria for patients were: diagnosis of RRMS, being diagnosed at least 1 year before study participation, EDSS score ≤ 4.0, no symptoms suggestive of a relapse, no relapse in the preceding 4 weeks, willing and capable of participating in the investigations, and having access to the internet and having given written informed consent.
Procedures
Eligibility checks and baseline assessment were done before the start of the intervention. After the baseline assessment (T0), follow-up assessments took place at 1 month (T1), 3 months (T2), and 6 months (T3). The 6-month follow up of the study was chosen as the observational study previously performed in MS patients with the same intervention in the Netherlands showed an effect after 6 monthsCitation15. In addition, in a chronic disorder like MS, an effect shorter than 6 months would have limited clinical relevance.
The CDT treatment was given by a multi-disciplinary team and consists of large group sessions, small group sessions, consultations, theatre evening, and (optional) a joint activity at the start of the day. In large group sessions given by the psychiatrist and psychiatric nurse, the participants were taught the basics of how to support each other, give and provide feedback. Potential stressors were identified for every person, and one or two individual goals were formulated. In small group sessions, participants could sign up for different training groups depending on the defined goals. For instance, sessions coached by a physiotherapist focusing on exploration of physical capabilities, sessions coached by a psychiatrist and psychiatric nurse targeting the emotional potential, and “life” sessions coached by a neurologist, a registered nurse specialized in MS, and a person with MS, with the focus on the exploration of capabilities relating to daily living. There were relaxing sessions (coached by a dance therapist) and a theatre evening (guided by the team) where participants practiced changing roles to show potential by experimentation. In the morning, the participants could participate in a walk into the woodsCitation19.
The control group patients received care as usual, including treatment and care by their neurologist or other healthcare professionals, as there is no standard treatment available for the improvement of self-efficacy control in patients with MS; they also had the option to receive CDT after study participation. In the Netherlands, a National Guideline for diagnosis and treatment of MS is usedCitation20.
During the entire follow-up period, CDT patients were allowed to contact the psychiatrist of the CDT team according to need.
Randomization and blinding
Randomization was performed by Signidat, an independent statistical agency in Groningen (the Netherlands), who generated the sequence. A stratified block randomization was used for this, with disease duration and gender as blocking factors for every CDT patient. Patients who were included in the CDT group were phoned and invited by the project coordinator of the National Multiple Sclerosis Foundation of the Netherlands. Patients randomized into the control group were also informed by phone and were given the opportunity to receive CDT after the 6 months study participation.
All questionnaires on resource use and outcomes were filled in online (LimeSurvey). The items on the questionnaires were fixed, and the responses were captured automatically. Patients received reminders whenever questionnaires were not completed. Reasons for not responding were also stocked. The person (MH) who enrolled the patients was also involved in the logistics of conducting the trial and in providing a part of the CDT. The researcher (GvM) who performed all analyses was masked from the treatment group whenever possible during the analyses. It was not possible to mask patients and the clinical investigator (PJJ) for allocation of treatment.
Outcomes
For the cost-effectiveness analysis (CEA), control self-efficacy, measured by the Multiple Sclerosis Self-Efficacy Scale (MSSES), was used as the primary outcome. The MSSES is an 18-item questionnaire, containing two sub-scales, Control and Function, each with nine questions scored on a 10-point Likert scale from 10 (very uncertain) to 100 (very certain). The MSSES is a disease-specific and sensitive questionnaire with a high internal consistency and test–re-test reliabilityCitation21. For this analysis only MSSES Control data were used, with higher scores on the sub-scale indicating more confidence in managing symptoms and coping with the demands of illness. The validity and reliability of the MSSES has been determined in previous researchCitation21.
The main outcome for the cost-utility analysis (CUA) was HRQoL, as measured by the five-dimensional five-level EuroQol (EQ-5D-5L). The five EuroQol domains of health are: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The higher the score on these domains, the higher the level of complaints. To estimate the utility of health states described by patients, we used the Dutch tariffCitation22. Quality-adjusted life years (QALYs) were calculated by means of the Area Under the Curve (AUC) method. Higher QALYs indicate more improvement in quality-of-life. The Dutch guidelines for economic evaluations recommend the use of this instrument for the measurement of utilitiesCitation23,Citation24.
Costs
To calculate the total societal costs, data were collected within the above-mentioned time frame. For this, at first all volumes of resource use were measured by means of online questionnaires. Medication costs are calculated using the Dutch Pharmaceutical Therapeutic compass (https://www.farmacotherapeutischkompas.nl/). The costs of tools are valued on the basis of actual purchase prices. The costs of the CDT intervention are based on costs calculations of the National Multiple Sclerosis Foundation. The Dutch Manual for costingCitation25 was used to calculate costs for all other categories of costs. Besides healthcare costs, patient and family costs were included. The cost of informal care was valued as a “shadow price”, meaning the hourly wage rate of a professional caregiver (e.g. housekeeper). Travel costs were calculated by multiplying the average distance, with standard price weights corrected for public transport costs and parking costsCitation25.
All costs reported in this study are expressed in Euros (€); the year 2014 is used as a reference year. Discounting was not necessary, since the follow-up period of the study did not exceed 1 year. provides an overview of all cost categories, noting the unit of measurement used to measure the different costs and the unit prices.
Table 1. Unit prices for healthcare and non-healthcare costs.
Analytical methods
All statistical analyses were performed using the Statistical Package for the Social Sciences version 21 and Microsoft Excel (Office 2010). Missing values were imputed using multiple imputation methods. As predictors for matching in the various regression models, the following baseline parameters were used: age, gender, disease duration, living situation, marital status, education, work status, EDSS score, and number of co-morbidities. The clinically meaningful difference of outcomes was defined as a half of the standard deviation (SD) of that specific score at baselineCitation26.
The incremental cost-effectiveness ratios (ICERs) were calculated by dividing the incremental costs by the incremental effects; we calculated the ICER by dividing the incremental costs by the differences in MSSES Control. In the base case analyses, the costs from a societal perspective were taken into account, as well as the MSSES Control score at 6 months. For the CUA, the QALYs of every individual patient and the societal costs were used to calculate the incremental cost utility ratio’s (ICURs). Because cost data are generally known to be skewed, we used non-parametric bootstrapping, using 5,000 replications, to estimate the uncertainty surrounding the cost-effectiveness ratio. A cost-effectiveness plane (CE-plane) was drawn by presenting the bootstrapped cost-effectiveness pairs. CE-planes show differences in effect on the horizontal axis and in costs on the vertical axis. Bootstrapped cost-effectiveness pairs located in the northwest quadrant indicate the CDT to be inferior to conventional care (more costly and less effective); in the southeast quadrant to be superior (more effective and less costly), and with respect to the northeast and southwest quadrants, the preference for an intervention depends on the threshold value, i.e. what society is prepared to pay for a gain in effectiveness, or is willing to accept as savings for a loss in effectiveness.
Statistically significant differences in costs were determined by means of a 95% confidence interval (95% CI). The uncertainty interval is represented by the 2.5th and 97.5th percentiles; when the interval does not include zero, the difference is statistically significant. The probability of CDT being a cost-effective alternative in comparison with usual care is also demonstrated by a cost-effectiveness acceptability curve (CEAC). A CEAC shows the probability of an intervention being a cost-effective alternative for a certain threshold value, viz. the amount of money a society is willing to pay (WTP) for an improvement in QALY. The WTP threshold for a QALY differs per country or even within countries. In the Netherlands, the Dutch Council of Public Health and Care published a report in 2006 regarding the burden of disease in the Netherlands, estimating a QALY threshold for MS at €40,000 EurosCitation27. No WTP has been established for the MSSES Control.
Sensitivity analyses
We performed nine one-way sensitivity analyses (SEAs) to test the robustness of the findings. In two analyses, the perspective of the analyses was changed, from a societal to a healthcare perspective for both outcomes (MSSES Control (SEA1) and QALY (SEA2), meaning that all non-healthcare costs (tools, travel, informal care, over the counter medication, and productivity losses) were not taken into account. In one SEA (SEA3) the baseline MSSES Control of the control group and the 6 months MSSES Control of the intervention group were used to investigate the impact of a “waiting list effect”. In four other SEA (SEA4–SEA7) the costs of the intervention were decreased by, respectively, 500 or 1,000 Euros for both endpoints. One other SEA (SEA8) was performed to investigate the impact of the UK Tariffs for EQ-5D utilities on the study resultsCitation28. In a final SEA (SEA9), the results of the scores on the SF-26 (version 1) of the MSQol-54 were used to calculate the SF-6D utilitiesCitation29. This was done in order to investigate the possible discrepancies between EQ-5D and SF-6DCitation30. As there are no Dutch tariffs available, the UK tariffs were usedCitation31.
Sub-group analyses
In total, 12 sub-group analyses (SUAs) were performed to identify potential sub-groups of patients. For the first eight SUAs, the same sub-groups were used for both study outcomes (MSSES Control [SUA1-SUA3-SUA5-SUA7] and Dutch QALY EQ-5D [SUA2-SUA4-SUA6-SUA8]). In the first two SUAs [SUA1 and SUA2] only patients showing a clinically meaningful increase in MSSES Control at 6 months were selected (75 or more points); in two other SUAs [SUA3 and SUA4], the 50% of the patients with the lowest MSSES Control scores at baseline were selected. The selection of the other four SUAs was based on a recent report of an intense social cognitive intervention in patients with treatment-resistant chronic painCitation32; patients were included in this study if they reported (1) relational problems with their support partner, (2) stressors, and (3) distress, depression, or anxiety. Sub-groups of patients were obtained by selecting those who experienced all three factors [SUA6 and SUA8], and those having depressive or anxious symptoms [SUA5 and SUA7]. In the next SUAs [SUA9 and SUA10] the same two sub-groups were used, but now the SF-6D (UK tariff) was used as a study outcome. Protocol deviations were identified by screening all study and medical data. In the two final SUAs [SUA11 and SUA12] the impact of these protocol violations on study findings was investigated.
Results
Primary analyses
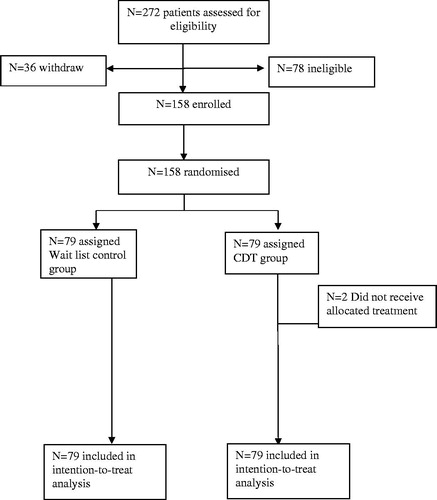
Patients with MS were recruited from January 1, 2013 to April 1, 2016, by the National Multiple Sclerosis Foundation in the Netherlands. Two hundred and seventy-two patients were assessed regarding their eligibility for participation in this study (). Seventy-eight patients (28.7%) did not meet the inclusion criteria, and 36 patients (13.2%) did not want to participate in the study. A total of 158 patients (58.1%) were included in this study. Seventy-nine patients (50%) were allocated to the CDT group, and 79 patients (50%) to the control group. Protocol violations were observed in five (6.3%) CDT patients and seven (8.9%) control patients. Two patients in the CDT group left the weekend before it ended; the other patients had psychiatric outpatient consultations before inclusion.
The mean age of the participants was 40 years, and 80% of them were females. At the start of study participation 50% of the patients had a partner, 47% had higher education, and 37% were employed. Overall, the baseline characteristics showed no differences between the two groups ().
Table 2. Baseline characteristics of patients in the CDT and control groups.
The MSSES Control scores, Dutch EQ-5D-5L utilities, Dutch QALYs, UK SF-6D utilities, and UK QALYs are reported in . At 6 months, none of these outcomes were significantly different between the two groups. At 1 month and 3 months, the MSSES Control was significantly higher in the CDT group in comparison with controls. At the follow-up period of 6 months for the CDT group, a clinically meaningful increase was reported for MSSES Control in comparison with baseline.
Table 3. Results of MSSES control, utility and QALY for both the CDT group (n = 79) and the control group (n = 79).
At 6 months the total societal costs were significantly higher for the CDT group (€13,439) in comparison with the control group (€10,490), with a mean difference (95% CI) of €2,913 (€140; €5,371). The healthcare costs were also significantly higher in the CDT group in comparison with the control group, which had a mean (95% CI) of €3,116 (€1,353; €4,929) at 6 months. Overall, the consumption of care did not differ significantly between the two groups. However, due to the higher (although not significantly so) costs of prescribed medication and intervention costs, the total costs for the CDT group were higher. On the other hand, the costs of day treatment were lower, but not significantly different, for the CDT group in comparison with care as usual. The total non-healthcare costs were similar for both groups (control €3,187; CDT €2,998), although the costs of tools, informal care, and productivity losses were different (but not significantly so) between both groups. Further details are presented in .
Table 4. Average imputed resource use and costs (Euros) at 6-month follow-up for CDT and control group patients.
Base case analysis
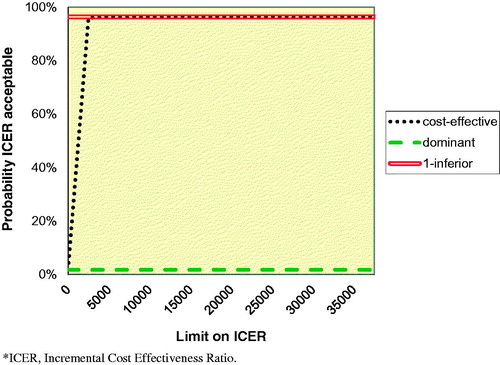
The base case CEA, from a societal perspective with MSSES Control as outcome, showed that the CDT group induced more costs (€2,948) but also more effects (40.74), resulting in a small ICER (€72) (). Almost all bootstrapped ICERs (95%) were located in the northwest quadrant of the CE-plane () indicating both higher costs and higher effects for the CDT intervention.
Figure 2. Cost-effectiveness plane with bootstrapped ICERS; societal costs and MSSES Control at 6 months. Abbreviation. ICERs, Incremental Cost Effectiveness Ratios.
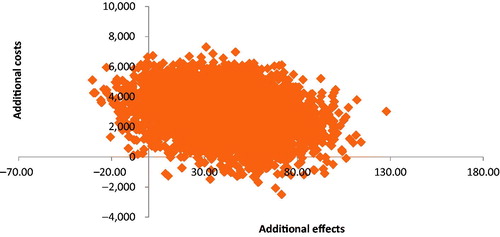
Table 5. Incremental cost-effectiveness ratios and cost-effectiveness plane distributions between CDT and control groups of 6-month follow-up for MSSES control as outcome.
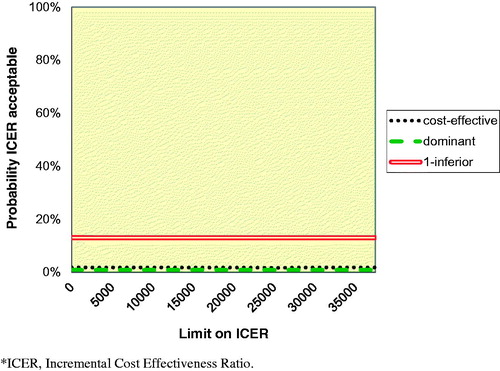
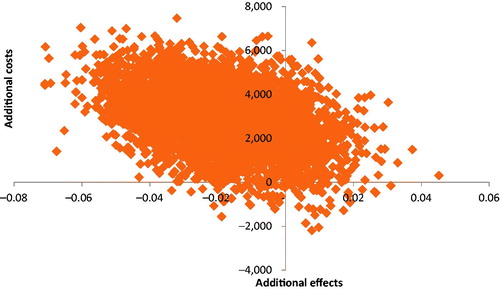
The base case CUA, from a societal perspective with Dutch QALYs (EQ-5D-5L)Citation22 as outcome, showed that CDT patients gained less QALYs in comparison with control patients (mean = −0.02). Less QALYs gained, combined with higher societal costs (€2,948) induced by CDT, resulted in an inferior ICUR. As presented in , 87% of the bootstrapped ICURs were located in the northwest quadrant (lower effects and higher costs) of the CE-plane, whereas only 10% of the bootstrapped ICURs were located in the northeast quadrant (higher effects and higher costs). An important additional observation is that the QALY difference between the two groups is very small and, as already mentioned in the ANCOVA analyses, not significantly different between the two groups.
Figure 3. Cost-effectiveness plane with bootstrapped ICURS: societal costs and Dutch (EQ-5D-5L) QALY at 6 months. Abbreviations. QALY, Quality-Adjusted Life Years; ICURS, Incremental Cost-Utility Ratios.
The CEACs of MSSES Control and QALY are presented in and . The slope of the MSSES Control CEAC indicates that, with a WTP threshold of €5,000, there is a high probability that the CDT intervention is worth investing in. For the CEACs with the QALY as an outcome, there is a small chance of the CDT treatment being cost-effective. Using a WTP threshold of €40,000, the QALY CEAC indicates that the chance that the CDT intervention will be cost-effective is zero.
Sensitivity analyses
In the first two SEAs, estimating total costs from a healthcare perspective resulted in rather similar ICER and ICUR distributions among the various quadrants of the CE-plane for both outcome measures [SEA1–2]. There was also little difference in the outcome measures for the two groups for SEA3, where the impact of having the opportunity to receive CDT after the controlled study phase was investigated. Four sensitivity analyses were performed to estimate the impact of lowering the price of the intervention on the cost-effectiveness results [SEA4–7]. The analyses proved the robustness of the base case assumption for this parameter for both the MSSES Control and QALYs; no major changes were found in distributions on the CE plane ( and ). A remarkable difference was observed in the final SEA [SEA9], in which the SF-6D with the UK tariff was used to calculate the QALYs. Eighty-five per cent of the ICURs are situated in the northeast quadrant, indicating a high chance of the CDT being cost-effective.
Table 6. Incremental cost-utility ratios and cost-effectiveness plane distributions between CDT and control groups of follow up 6 months for QALY as outcome.
Sub-group analyses
Overall, the sub-group analyses of the ICERs and ICURs show results comparable to those of the base case analyses. Thus, there is a high chance that ICERs with MSSES Control as outcome are situated in the northwest quadrant (higher costs and higher effects) and ICURs with EQ-5D-5L QALY as outcome lie in the northeast quadrant (higher costs and lower effects). When the QALYs were calculated using SF-6D [SUA4-9-10], the distribution of the ICURs among the different quadrants shows the same relevant changes as we found in the sensitivity analyses. In other words, the probability that CDT is cost-effective increases when using SF-6D as an outcome.
Discussion
This trial-based evaluation is the first economic evaluation of the intense cognitive therapy-based intervention (CDT) in patients with RRMS. The results with a 6 months follow-up are not conclusive: cost-effectiveness analyses show a high chance of CDT being the preferred treatment—although it is somewhat more expensive, it also induces more effects on the self-efficacy control scale. However, the cost-utility analysis using QALYs based on the EQ-5D-5L questionnaire indicates the opposite—a very small chance of CDT being cost-effective. Even so, when using QALYs based on SF-6D for the CUA, there is a higher probability that CDT is preferred over care as usual. All other sensitivity analyses confirm these analyses. The results of the sub-group analyses show that no relevant sub-groups of patients with RRMS could be identified.
In our opinion, there are two main reasons, which explain these study findings. First, the societal costs were significantly higher for the CDT group, in comparison with the care as usual group. Although lower costs for productivity losses (absence from work) and for day treatment were observed for the CDT group, total costs were higher for this group. The costs of the intervention and the prescribed medication costs were the main drivers for the higher costs in the CDT group. Second, the MSSES Control or the self-efficacy outcome is more sensitive than the EQ-5D-5L for detecting clinically relevant changes in patients with RRMS in the current study. This is also expected, as MSSES control is a disease-specific measure and EQ-5D is a generic measure. The use of the EQ-5D in patients with MS has some important drawbacks, which will be discussed later in this discussion section.
The potential value in MS of treatments comparable to CDT—cognitive behavioural therapy and educational interventions—has been acknowledged by othersCitation33,Citation34. Based on a systematic review, 15 randomized controlled trials were identified evaluating non-pharmacological interventions in patients with MS using self-efficacy as an outcomeCitation6–14,Citation35–40. These studies were performed in the US (n = 5), UK (n = 5), Italy (n = 1), and Australia (n = 1). The interventions were very heterogeneous (e.g. content, intensity, duration, length of each session), but could be categorized as follows; self-management (n = 5), cognitive behavioural therapy (CBT) and education (n = 2), exercise based CBT (n = 3), and other types of interventions (n = 5). FourCitation6,Citation7,Citation12,Citation35 out of five studies evaluating self-management interventions show a significant treatment effect on self-efficacy in patients with MS. For the exercise-based CBT interventions, no between-group effects were identifiedCitation14,Citation37,Citation38. For CBT and education and other interventions, mixed results were reported. Our RCT showed that self-efficacy improved in patients with MS after an intensive 3-day social cognitive treatment; however, as this intervention was not comparable to the 15 other studies, no conclusions could be drawn in relation to the findings of these studies.
The need for economic evidence on this topic is very evident as, by means of a rapid systematic review, only two trial-based (full) economic evaluations of non-pharmacological interventions in patients with MS were identified. The first study was a trial-based economic evaluation of a pragmatic exercise intervention (EXIMS) for people with MSCitation41, and used EQ-5D, SF-6D, and QALYs as outcomes. The cost-effectiveness analyses were performed from the National Health Services and personal social service provider (Third Party Payer) perspectives, in other words only taking into account the medical costs. The results of this study were the opposite of our findings. They concluded that the EXIMS intervention was cost-effective, although the costs were somewhat higher, but the QALYs were also higher (for EQ-5D and SF-6D) for EXIMS group. The second study was also a trial-based economic evaluation of a group-based fatigue management programme (FACETS) for people with MSCitation39. They included the fatigue self-efficacy scale, EQ-5D, SF-6D, and QALYs as outcomes. Cost-effectiveness analyses were performed from the same perspectives as used in the EXIMS study. The FACETS study is in line with our findings; it stays unclear whether the intervention is cost-effective, as the QALY differences are very small and costs were higher for the treatment armCitation39.
The challenges for outcome measurement in this study were considered substantial. The EQ-5D and SF-6D are recommended utility measuresCitation23 and are widely used across diseasesCitation23,Citation24,Citation42,Citation43, but in the MS population they posess some drawbacksCitation44. These two questionnaires show similarities and dissimilarities in items, domains, scoring, and valuation methods, they generate different utility scoresCitation45. In a recent systematic review, the psychometric properties of utility measures in patients with MS were summarizedCitation44. Based on the study of Fogarty et al.Citation46, the content validity of EQ-5D and SF-6D for MS was questioned. These questionnaires miss relevant domains, like “cognition”, “disability” (both questionnaires), and “fatigue” (EQ-5D). In addition, they also show problems of differentiating between the different levels of disabilityCitation44. This lack of discriminative ability could be caused by the fact that there is not enough improvement possible in the utility scores for mildly impaired patients with MS. This is confirmed in our study by a high proportion of ceiling effects in all EQ-5D domains, ranging from 19.6% in the domains “pain” and “discomfort” to 87.3% in the domain “self-care” (data not shown). In the SF-6D domains “vitality” and “role limitations”, ceiling effects were also observed, respectively, 36.7% and 22.2%. Others also reported ceiling effects in SF-6D and EQ-5D in patients with MSCitation46–48.
In our study the patients with MS were mildly impaired, with a mean EDSS score of 2.3, indicating that they have on average a mild disability in only one functional system or minimal disability in two functional systemsCitation49. Based on our data, it seems that the EQ-5D-5L was better able to detect differences in HRQoL in comparison with the SF-6D, although the observed differences were neither significantly different nor clinically relevant. In summary, it is clear that both EQ-5D and SF-6D show shortcomings for the measurement of HrQoL in patients with MS. In addition, it is also evident that they cannot generally be used interchangeably for measurement of preference utilitiesCitation30,Citation50. However, it was not possible to explain the discrepancy between EQ-5D-5L and SF-6D findings based on the results of our study.
For economic evaluations, although differences in utilities or QALYs between groups are small, they can influence the distribution of the ICURs over the CE-plane quadrants and, hence, the study conclusionsCitation51,Citation52. In our study, the impact of using EQ-5D vs SF-6D was essential for the distributions of the ICURs among the different quadrants. All analyses with the EQ-5D show inferior results for the CDT group, and when using the SF-6D there is a high probability of ICURs being cost-effective. Of five trials investigatedCitation52, in one study—evaluating a nurse-led telemedicine intervention for asthma patients—the use of the utility measures was critical for the probability of the experimental treatment being cost-effectiveCitation53. In our opinion, we are not able to judge which of the two ICUR analyses we should follow for drawing conclusions for decision-making and the implementation of CDT. This is also based on the fact (as discussed before) that the content validity and the discriminative ability of both questionnaires (EQ-5D-5L and SF-6D) are limited in patients with MSCitation47.
Strengths of the current study include the large sample size, and the recruitment of patients from all over the Netherlands, increasing the generalizability of study findings. In addition, the number of patients who were not treated according to the protocol was low (<10%), and the data analysis was performed by an independent researcher not involved in the study design or treatment. Furthermore, the current study provides new evidence, as there have been no previous economic evaluations of an intense cognitive theory-based intervention for MS performed in a randomized controlled trial setting. Finally, the cost-effectiveness analyses were conducted from a societal perspective with a bottom-up detailed method of costing, and reported according to the CHEERS guidelinesCitation54. In addition, the Dutch guidelines for performing economic evaluations were followed as much as possibleCitation23,Citation25, which we also consider to be a strength.
The study has several drawbacks. First, a 6-month follow-up may be too short to adequately evaluate the cost-effectiveness of an intervention with a potentially longer lasting effect, especially in patients with a chronic disease. Second, the increase in control self-efficacy at 6 months in care-as-usual patients, which was unexpected. In principle, the comparator should be the most cost-effective alternative intervention currently available, and in practice the comparator is usually the most widely used alternative treatmentCitation55. However, as there is no effective alternative treatment for improving control self-efficacy in patients with MS, we chose care as usual. The fact that control patients were given the opportunity to receive CDT after the controlled study phase may have induced an effect comparable to that of being on a waiting list. Actually, 77% of the control patients chose to receive CDT. It is well known that the choice of comparator is a critical design parameter in economic evaluation research, and that the comparator may influence study resultsCitation56.
Practical implications of the study findings and current knowledge base
The following findings are useful for decision-makers:
Based on the cost-effectiveness analysis, CDT improves the self-efficacy in patients with RRMS and low disability and generates higher costs compared to the care as usual patients.
The total cost of CDT was estimated to be 2.500 Euros, taking into account all healthcare provider costs and the weekend stay in a hotel. However, a substantial amount of these costs can be reduced by choosing a cheaper treatment location. For instance, instead of using a hotel, an outpatient rehabilitation clinic.
The findings related to cost-utility analyses of the CDT need to be interpreted with caution. There is a growing evidence base to suggest that the EQ-5D and SF-6D may lack both relevance and sensitivity to changesCitation47. For research this poses a question to investigate: which preference based utility instrument is the most reliable one in patients with MS and also in other disease populations?
CDT is a standardized intervention, which has been described in detail in order to make replication of the treatment and further research possibleCitation15,Citation16,Citation19.
The study population of the current study was recruited on a national level, indicating that study findings are generalizable to patients with RRMS with low disability in other western countries.
This CDT could also be applicable to other populations: in one observational study, a similar intervention was successful in patients with intractable chronic painCitation32. In addition, the effects of CDT may be expected to be generalizable to other (western) societies, as is suggested in the study by Ng et al.Citation57 on a similar intervention in American patients with MS.
No relevant sub-groups could be identified in our study. In other words, there is no reason to exclude patients for the CDT who are not anxious, have no depressive feelings, experience more health distress or stressors, and those who report relational problems. This also holds for selection of patients of MSSES control at baseline.
Conclusions
Results of this trial-based economic evaluation are not conclusive on the implementation of CDT for patients with RRMS and low disability. When using the EQ-5D-5L tariffs to calculate a QALY, CDT is not a cost-effective alternative in comparison to care as usual. However, when using self-efficacy or SF-6D as outcomes, there is a probability that CDT is cost-effective. Future research is needed to investigate whether CDT is cost-effective in comparison with care as usual. In these future studies, the follow-up time should be extended. In addition, SF-6D should be used in sensitivity analyses of economic evaluations of MS treatments, as it shows opposite effects in comparison with the EQ-5D. Another option for measurement of utilities could be the development of an MS specific utility measure for patients with MSCitation44.
Transparency
Declaration of funding
The study was initiated, funded, and co-executed by the Dutch patient organization, the National Multiple Sclerosis Foundation, Rotterdam, the Netherlands. The protocol was developed by the principal investigator, PJJ, with guidance from co-investigators RPR and LHV. The funding body had a role in the recruitment (AH) and screening (MH) of patients, and in the collection of data (MH). The funding body had no role in the analysis or interpretation of data. The researcher performing the analyses (GvM) was commissioned by the MS4 Research Institute.
Declaration of financial/other interests
GvM and SME have no interests to declare. MH is an employee of the National Multiple Sclerosis Foundation, the Netherlands. LHV received honoraria for lectures, grants for research, and honoraria for advisory boards from Sanofi Genzyme, Merck Serono, Novartis, and Teva. RPR has no interests to declare. AH is a former employee of the National Multiple Sclerosis Foundation, the Netherlands. LD has no interests to declare. JVV has no interests to declare. JC has no interests to declare. MB is a member of the supervisory board of the National Multiple Sclerosis Foundation, the Netherlands. MvD is an employee of the National Multiple Sclerosis Foundation, the Netherlands. PJJ received honoraria from Bayer, Merck Serono, and Teva for contributions to symposia as a speaker or for educational or consultancy activities.
A peer reviewer of the manuscript declares receiving speaker fees from Biogen, Sanofi-Genzyme, Genentech, Novartis, and Mallinckrodt. The same reviewer declares being currently engaged in research for Mallinckrodt and Novartis. The remaining JME peer reviewers on this manuscript have no other relevant financial or other relationships to disclose.
Author contributions
GvM performed the analysis of the data, contributed to the interpretation of the data, and drafted and finalized the manuscript. SME conceived the design of the economic study, contributed to the analysis of the economic data, contributed to the interpretation of the economic data, and has revised the manuscript critically for important intellectual content. MH was involved in the development of the CDT, was a member of the multidisciplinary team, contributed to the acquisition of the economic and clinical data, and has revised the manuscript critically for important intellectual content. LHV was involved in the development of the CDT, contributed to the design of the randomized controlled study, was a member of the multidisciplinary team, contributed to the acquisition of the clinical data, and has revised the manuscript critically for important intellectual content. RPR conceived and developed the CDT, contributed to the design of the randomized controlled study, was a member of the multidisciplinary team, contributed to the acquisition of the clinical data, contributed to the interpretation of the clinical data, and has revised the manuscript critically for important intellectual content. AH was involved in the development of the CDT, was involved in the organization of the study, was a member of the multidisciplinary team, contributed to the acquisition of the clinical data, and has revised the manuscript critically for important intellectual content. LD was involved in the development of the CDT, was a member of the multidisciplinary team, contributed to the acquisition of the clinical data, and has revised the manuscript critically for important intellectual content. JVV was involved in the development of the CDT, was a member of the multidisciplinary team, contributed to the acquisition of clinical data, has revised the manuscript critically for important intellectual content. JC was a member of the multidisciplinary team, contributed to the acquisition of clinical data, and has revised the manuscript critically for important intellectual content. MB was a member of the multidisciplinary team, contributed to the acquisition of the data, and has revised the manuscript critically for important intellectual content. MvD was involved in the development of the CDT, has organized the Can Do treatments, contributed to the acquisition of the data, and has revised the manuscript critically for important intellectual content. PJJ conceived and designed the randomized controlled study, coordinated the acquisition of the data, contributed to the acquisition of the data, contributed to the analysis of the clinical data, contributed to the interpretation of the clinical and economic data, and co-drafted the manuscript.
Acknowledgements
The authors would like to thank the patients with MS and partners who participated in the CDT study. We would also like to thank Barbara Greenberg for her English editing services.
Data availability statement
Data of the current study is publicly available through G van Mastrigt, the corresponding author of this study.
References
- Evans C, Beland SG, Kulaga S, et al. Incidence and prevalence of multiple sclerosis in the Americas: a systematic review. Neuroepidemiology. 2013;40:195–210.
- Lublin FD. New multiple sclerosis phenotypic classification. Eur Neurol. 2014;72:1–5.
- Bass A, Van Wijmeersch B, Mayer L, et al. Impact of multiple sclerosis on patients’ daily activities, emotional well-being and relationships: results of the global vsMS™ survey. Neurology. 2017;88:P3 334.
- Chiu C, Bishop M, Pionke JJ, et al. Barriers to the accessibility and continuity of health-care services in people with multiple sclerosis. Int J MS Care. 2017;19:313–321.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977; 84:191–215.
- Barlow J, Turner A, Edwards R, et al. A randomised controlled trial of lay-led self-management for people with multiple sclerosis. Patient Educ Couns. 2009;77:81–89.
- Ennis M, Thain J, Boggild M, et al. A randomized controlled trial of a health promotion education programme for people with multiple sclerosis. Clin Rehab. 2006;20:783–792.
- Forman AC, Lincoln NB. Evaluation of an adjustment group for people with multiple sclerosis: a pilot randomized controlled trial. Clin Rehab. 2010;24:211–221.
- Lincoln NB, Yuill F, Holmes J, et al. Evaluation of an adjustment group for people with multiple sclerosis and low mood: a randomized controlled trial. Mult Scler. 2011;17:1250–1257.
- Mathiowetz VG, Finlayson ML, Matuska KM, et al. Randomized controlled trial of an energy conservation course for persons with multiple sclerosis. Mult Scler. 2005;11:592–601.
- Miller DM, Moore SM, Fox RJ, et al. Web-based self-management for patients with multiple sclerosis: a practical, randomized trial. Telemed J E Health. 2011;17:5–13.
- Stuifbergen AK, Becker H, Blozis S, et al. A randomized clinical trial of a wellness intervention for women with multiple sclerosis. Arch Phys Med Rehab. 2003;84:467–476.
- Stuifbergen AK, Becker H, Perez F, et al. A randomized controlled trial of a cognitive rehabilitation intervention for persons with multiple sclerosis. Clin Rehab. 2012;26:882–893.
- Motl RW, Dlugonski D, Wojcicki TR, et al. Internet intervention for increasing physical activity in persons with multiple sclerosis. Mult Scler. 2011;17:116–128.
- Jongen PJ, Heerings M, Ruimschotel R, et al. Intensive social cognitive treatment (can do treatment) with participation of support partners in persons with relapsing remitting multiple sclerosis: observation of improved self-efficacy, quality of life, anxiety and depression 1 year later. BMC Res Notes. 2016;9:375.
- Jongen P, van Mastrigt G, Heerings M, et al. Intensive social cognitive treatment of self-efficacy in relapsing remitting multiple sclerosis patients: a randomized, open-label, controlled trial. PLOS One. Forthcoming.
- Uitdehaag B, Kobelt G, Berg J, et al. New insights into the burden and costs of multiple sclerosis in Europe: results for the Netherlands. Mult Scler. 2017;23:117–129.
- 64th WMA General Assembly. Ethical principles for medical research involving human subjects Fortaleza, Brazil, October 2013, version 2013 [cited 2019 May 6]. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
- Jongen PJ, Heerings M, Ruimschotel R, et al. An intensive social cognitive program (can do treatment) in people with relapsing remitting multiple sclerosis and low disability: a randomized controlled trial protocol. BMC Neurol. 2016;16:81.
- Neurology. Multiple sclerosis. Utrecht, The Netherlands: Dutch Federation of medical specialists. 2012 [cited 2019 May 06]. Available from: https://richtlijnendatabase.nl/richtlijn/acute_neurologie/acute_neurologie_bij_multiple_sclerose/immunomodulerende_en_-suppressieve_beh_ms.html
- Schwartz CE, Coulthard-Morris L, Zeng Q, et al. Measuring self-efficacy in people with multiple sclerosis: a validation study. Arch Phys Med Rehabil. 1996;77:394–398.
- Versteegh M, Vermeulen K, Evers S, et al. Dutch tariff for the five-level version of EQ-5D. Value Health. 2016;19:343–352.
- IJzerman M, Al M, de Boer A, et al. Guideline for performing economic evaluation research in Health Care (in Dutch). Diemen: Care Institute the Netherlands; 2015.
- Versteegh M, Knies S, Brouwer W. From good to better: new Dutch guidelines for economic evaluations in healthcare. Pharmacoeconomics. 2016;34:1071–1074.
- Hakkaart-van Roijen L, van der Linden M, Bouwmans C, et al. Guideline for cost research: Methodology and reference prices for economic evaluations in healthcare (In Dutch). Rotterdam, The Netherlands: iMTA Erasmus University Rotterdam; 2015.
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592.
- Raad voor Volksgezondheid en Samenleving (RVS). Zinnige en duurzame zorg. Zoetermeer, The Netherlands: RVS; 2006. Dutch.
- van Hout B, Janssen MF, Feng Y-S, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15:708–715.
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21:271–292.
- Sogaard R, Christensen FB, Videbaek TS, et al. Interchangeability of the EQ-5D and the SF-6D in long-lasting low back pain. Value Health. 2009;12:606–612.
- Brazier JE, Roberts J. The estimation of a preference-based measure of health from the SF-12. Med Care. 2004;42:851–859.
- Jongen PJ, Ruimschotel RP, Museler-Kreijns YM, et al. Improved health-related quality of life, participation, and autonomy in patients with treatment-resistant chronic pain after an intensive social cognitive intervention with the participation of support partners. JPR. 2017;10:2725–2738.
- Dennison L, Moss-Morris R. Cognitive–behavioral therapy: what benefits can it offer people with multiple sclerosis? Expert Rev Neurother. 2010;10:1383–1390.
- Wendebourg MJ, Heesen C, Finlayson M, et al. Patient education for people with multiple sclerosis-associated fatigue: a systematic review. PloS One. 2017;12:e0173025.
- Graziano F, Calandri E, Borghi M, et al. The effects of a group-based cognitive behavioral therapy on people with multiple sclerosis: a randomized controlled trial. Clin Rehabil. 2014;28:264–274.
- Kalina JT, Hinojosa J, Strober L, et al. Randomized controlled trial to improve self-efficacy in people with multiple sclerosis: the Community Reintegration for Socially Isolated Patients (CRISP) program. Am J Occup Ther. 2018;72:7205205030p1.
- Plow M, Bethoux F, Mai K, et al. A formative evaluation of customized pamphlets to promote physical activity and symptom self-management in women with multiple sclerosis. Health Educ Res. 2014;29:883–896.
- Suh Y, Motl RW, Olsen C, et al. Pilot trial of a social cognitive theory-based physical activity intervention delivered by nonsupervised technology in persons with multiple sclerosis. J Phys Act Health. 2015;12:924–930.
- Thomas S, Thomas PW, Kersten P, et al. A pragmatic parallel arm multi-centre randomised controlled trial to assess the effectiveness and cost-effectiveness of a group-based fatigue management programme (FACETS) for people with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2013;84:1092–1099.
- Dorstyn D, Roberts R, Murphy G, et al. Online resource to promote vocational interests among job seekers with multiple sclerosis: a randomized controlled trial in Australia. Arch Phys Med Rehabil. 2018;99:272–280.
- Tosh J, Dixon S, Carter A, et al. Cost effectiveness of a pragmatic exercise intervention (EXIMS) for people with multiple sclerosis: economic evaluation of a randomised controlled trial. Mult Scler. 2014;20:1123–1130.
- NICE. Developing NICE guidelines: the manual. Appendix H. 2014 [cited 2019 May 06]. Available from: https://www.nice.org.uk/process/pmg20/resources
- NICE. Developing NICE guidelines: the manual. 2014 [cited 2019 May 6]. Available from: https://www.nice.org.uk/process/pmg20/chapter/introduction-and-overview
- Kuspinar A, Mayo NE. A review of the psychometric properties of generic utility measures in multiple sclerosis. Pharmacoeconomics. 2014;32:759–773.
- Brazier J, Roberts J, Tsuchiya A, et al. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ. 2004;13:873–884.
- Fogarty E, Walsh C, Adams R, et al. Relating health-related quality of life to disability progression in multiple sclerosis, using the 5-level EQ-5D. Mult Scler. 2013;19:1190–1196.
- Fisk JD, Brown MG, Sketris IS, et al. A comparison of health utility measures for the evaluation of multiple sclerosis treatments. J Neurol Neurosurg Psychiatry. 2005;76:58–63.
- Kobelt G, Eriksson J, Phillips G, et al. The burden of multiple sclerosis 2015: methods of data collection, assessment and analysis of costs, quality of life and symptoms. Mult Scler. 2017;23:4–16.
- Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33:1444–1452.
- Petrou S, Hockley C. An investigation into the empirical validity of the EQ-5D and SF-6D based on hypothetical preferences in a general population. Health Econ. 2005;14:1169–1189.
- Davis JC, Liu-Ambrose T, Khan KM, et al. SF-6D and EQ-5D result in widely divergent incremental cost-effectiveness ratios in a clinical trial of older women: implications for health policy decisions. Osteoporos Int. 2012;23:1849–1857.
- Joore M, Brunenberg D, Nelemans P, et al. The impact of differences in EQ-5D and SF-6D utility scores on the acceptability of cost-utility ratios: results across five trial-based cost-utility studies. Value Health. 2010;13:222–229.
- Willems DC, Joore MA, Hendriks JJ, et al. Cost-effectiveness of a nurse-led telemonitoring intervention based on peak expiratory flow measurements in asthmatics: results of a randomised controlled trial. Cost Eff Resour Alloc. 2007;5:10.
- Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16:231–250.
- Drummond M, Schulper MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. 4th ed. Oxford: Oxford University Press; 2016.
- Wagner MM, Melnyk P, Rindress D. Systematic review of guideline recommendations on comparator selection in health economic evaluations. Value Health. 2012;15:A168.
- Ng A, Kennedy P, Hutchinson B, et al. Self-efficacy and health status improve after a wellness program in persons with multiple sclerosis. Disabil Rehabil. 2013;35:1039–1044.