Abstract
Objectives: The aim of this literature review was to provide a comprehensive report on hospital costs, and cost components, for a range of ventral cavity surgical procedures across three regions of focus: (1) Americas, (2) Europe, Middle East and Africa (EMEA), and (3) Asia-Pacific.
Methods: A structured search was performed and utilized a combination of controlled vocabulary (e.g., “Hepatectomy”, “Colectomy”, “Costs and Cost Analysis”) and keywords (e.g. “liver resection”, “bowel removal”, “economics”). Studies were considered eligible for inclusion if they reported hospital-related costs associated with the procedures of interest. Cost outcomes included operating room (OR) time costs, total OR costs, ward stay costs, total admission costs, OR cost per minute and ward cost per day. All costs were converted to 2018 USD.
Results: Total admission costs were observed to be highest in the Americas, with an average cost of $15,791. The average OR time cost per minute was found to vary by region: $24.83 (Americas), $14.29 (Asia-Pacific), and $13.90 (EMEA). A cost-breakdown demonstrated that OR costs typically comprised close to 50%, or more, of hospital admission costs. This review also demonstrates that decreasing OR time by 30 min provides cost savings approximately equivalent to a 1-day reduction in ward time.
Conclusion: This literature review provided a comprehensive assessment of hospital costs across various surgical procedures, approaches, and geographical regions. Our findings indicate that novel processes and healthcare technologies that aim to reduce resources such as operating time and hospital stay, can potentially provide resource savings for hospital payers.
Introduction
Global spending on health is expected to increase to US$18.28 trillion by 2040Citation1. With the rise in healthcare expenditures, it is important to understand areas where efficiencies and savings can be gained to mitigate ballooning public and private budgets. A large portion of healthcare expenditures is related to surgical care. Globally, it has been estimated that between 11% and 30% of the global burden of disease could benefit from surgical managementCitation2,Citation3. In 2005, the United States spent an estimated US$572 billion on surgical care, accounting for 29% of their total health care expendituresCitation4. However, there has been much variability in surgical volume across countriesCitation2. With estimations of the rising need of surgical procedures globallyCitation2, a better understanding of opportunities to optimize surgical spending is needed to help control healthcare expenditures.
Largely, the onus is on payers, hospitals, and healthcare providers to help reduce surgical and related hospital costs. Importantly, they must function within constrained budgets, while simultaneously providing the best quality of care possibleCitation5. Surgery is generally viewed as a cost-effective public health interventionCitation6–8, but constantly evolving innovations (e.g. robotics) and practices can impact these conclusions depending on the situation. One potential path to help reduce surgically-related costs is through the adoption of innovative medical devices and technologies that improve outcomes while simultaneously reducing other hospital resource use (e.g. ward stay, operative time, surgical complications)Citation9,Citation10. Such adoption decisions may not be easy in absence of substantial data, and require tools, such as economic analyses, to better understand the value that a new technology can provide to all stakeholders, as well as the bottom line to the payer’s budget.
Although hospital cost parameters have often been used to inform numerous health technology assessments and economic analysesCitation11, such data have not been collected, evaluated, or reported in a standard comprehensive way. The cost of a hospital day, or minute of operating room time, may vary across procedure types, settings, surgical approaches, and regions and thus not be simply interchangeable. Understanding how such cost components can vary can help to inform not only economic analyses of hospital technologies, but also general decision-making on where efforts could be placed for improving efficiencies and cost reductions. Thus, the aim of this literature review was to provide a comprehensive report on hospital costs for a range of ventral cavity surgeries that involve major organs. These costs were compared across three regions of focus: (1) Americas, (2) Europe, Middle East and Africa (EMEA), and (3) Asia-Pacific.
Methods
Literature search
A structured search of Ovid MEDLINE was conducted. The search of Ovid MEDLINE also included ePub ahead of print, in-Process & other non-indexed citations, and Embase. In addition, the Health Technology Assessment and NHS EED databases in Cochrane Library on Wiley were also searched. The search strategy was developed and tested through an iterative process by the review team (APT and NF) in consultation with an experienced medical information specialist. All searches were performed on January 15, 2018.
Strategies utilized a combination of controlled vocabulary (e.g. “Hepatectomy”, “Colectomy”, “Costs and Cost Analysis”) and keywords (e.g. “liver resection”, “bowel removal”, “economics”). Results were limited to the English language and the publication years 2007 to present. Due to the large amount of initial search results, and to keep the findings relatively recent, the publication years were further restricted to 2011 to present. As the goal of this review was to provide a comprehensive assessment of hospital and operating costs in several ventral cavity procedures on major organs (excluding the heart), the review team estimated that approximately 100 relevant studies would be adequate to achieve this result. When possible, animal-only and conference abstracts were removed from the results. Specific details regarding the search strategies appear in Supplementary Appendix 1.
Study selection
Studies were considered eligible for inclusion if they reported costs associated with a selected list of ventral cavity surgical procedure involving major organs (i.e. colectomy, hysterectomy, lobectomy, gastrectomy, bariatric surgery (e.g. gastric bypass), and hepatic resection). It was beyond the scope of this study to research additional procedures.
Based on the inclusion criteria, the eligibility of each publication was evaluated in a title and abstract review. If the abstract or title review suggested potential eligibility, a full-text review was conducted. Full-text studies were excluded if they did not report relevant cost outcomes or an appropriate cost breakdown. Records were evaluated in detail for eligibility by one reviewer (APT), with review of selected abstracts by a second reviewer (NF) for quality assurance.
Outcomes and data extraction
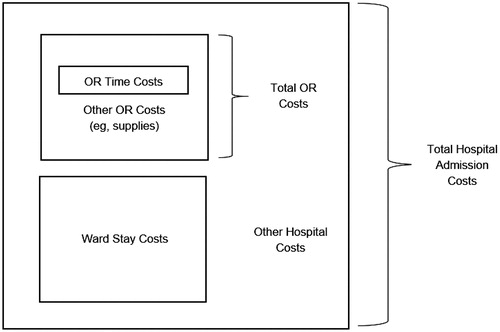
Details from the included studies were extracted using a standardized data extraction form developed in Microsoft Excel (Redmond, WA). The following study details were extracted when reported: study authors, publication year, country of origin, setting, study design, currency, cost year, type of value (i.e. cost, charge, etc.), surgical approach (i.e. open, laparoscopic, or robotic-assisted), procedure type, sample size, procedure/OR time, OR time costs, total OR costs, ward length of stay, ward stay costs, other hospital costs aside from OR and ward costs (e.g. intensive care), and total admission costs. The cost outcomes of focus included: (1) OR time costs (i.e. costs associated with rental of the OR and associated staff (e.g. nursing) costs), (2) total OR costs (i.e. OR time costs plus surgical supplies/variable costs), (3) ward stay costs (e.g. room and board, drug costs on the ward), (4) total admission costs (i.e. all costs incurred during inpatient stay), (5) OR time cost per minute and (6) ward cost per day. Consistent definitions of cost outcomes were developed to ensure a reliable extraction procedure (see ).
One reviewer conducted the detailed data extraction (APT). A second reviewer (NF) also conducted detailed data extraction for one procedure type (i.e. lobectomy) to ensure alignment. Due to variations in the reported currency and cost year across studies, all cost outcomes were inflated and converted to 2016 USD using an online tool developed by Shemilt and colleaguesCitation12. The online currency inflation and conversion tool was used to inflate and convert the costs reported by included studiesCitation13. The method used by the online tool has two stages. Stage one adjusts the original estimate of cost from the original price year to a target price year, using a gross domestic product deflator index (‘GDPD values’). Stage two converts the price-year adjusted cost estimate from the original currency to a target currency, using conversion rates based on purchasing power parities (PPP) for GDP. Since this method uses PPP, the specific basket of goods used to inform the PPP index is broader than that which would inform the medical component of consumer price index (CPI). However, PPP methods automatically adjust for international price level differences, while inflating costs using the medical component of CPI, then using exchange rates to convert currencies, does not. For consistency, it was especially important to adjust for these differences as costs reported were converted from many different currencies to USD.
Costs were further inflated to 2018 USD using a fixed rateCitation14, to reflect the most recent value in lieu of an updated online tool. Outcomes reported as charges were converted using a cost-to-charge ratio of 0.3, so that all values were represented as costsCitation15. This ratio was applied to 15 (14%) of the included studies.
For each study, if the value was not explicitly reported, OR time cost per minute and ward cost per day was derived using the total costs and total time (i.e. procedure time or days) reported. For each region, the weighted average cost was calculated for each of the 6 cost outcomes across procedures, with weighting based on study sample sizes. The ratio of the OR time cost relative to ward cost was calculated by converting OR time cost per minute and ward cost per day to a common unit (hours). These ratios were totaled, and the geometric mean was calculated. All cost outcomes are reported using heat maps, where tertile ranges for low (green), medium (yellow), and high costs (red), according to cost outcome type, were used to categorize values. Finally, for any one procedure type and region, a relative percentage breakdown of cost components comprising total hospital costs was derived based on a weighted average across studies. Please see Supplementary Appendix 2 for the 2018 cost values used for each study, along with the study sample sizes, which were used to inform the weighted averages.
Results
Search results
A total of 6,696 citations were identified (see ). After removing duplicates, 6,517 unique records were reviewed. Due to the large amount of results, 1,642 citations which were published before 2011 were excluded. Following title and abstract review of citations from 2011 to 2018, 4,516 citations were excluded due to the following reasons: did not assess relevant cost outcomes, not in humans, conference abstracts only, total or not conducted in target procedures of interest. Of the 359 full texts retrieved for review, 255 were further excluded for the following reasons: inadequate cost reporting, inability to extract surgical cost data, did not focus on a target procedure. In total, full extraction was completed for 104 included studiesCitation5,Citation16–118.
Table 1. Search strategy, including key terms, example searches, and results.
Outcome results
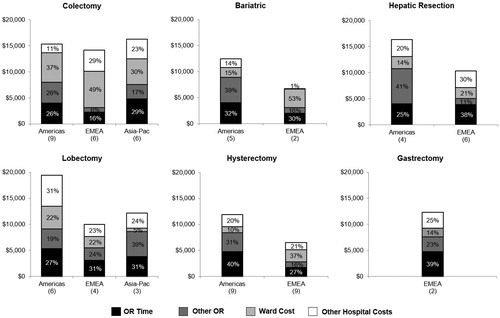
presents data for total admission costs for the procedures of interest, as well as a breakdown of several of the components of such costs, where available. With few exceptions footnoted in Supplementary appendix Tables, the literature was characterized by clinical studies that reported costs. Total admission costs were observed to be highest in the Americas, with a weighted average cost of $15,791 across procedures. In EMEA and Asia-Pacific, average total admission costs were lower at $10,063 and $5,865, respectively. Amongst procedure types, hysterectomy tended to be associated with lower total admission costs, with gastrectomy being higher, compared with other procedures and irrespective of region. Ward costs, a component of total admission costs, tended to be consistent, with low variability across regions and procedures. Ward costs were observed to be highest in Asia-Pacific, with a weighted average cost of $4,498. In Americas and EMEA, ward costs were lower at $4,291 and $3,305, respectively.
Table 2. Breakdown of hospital admission costs by region and procedure in 2018 USD.
Operating room time costs alone and total OR costs (i.e. supplies + time) are also presented in . First, the weighted average OR time cost was calculated to be highest in the Americas at $4,574. Not surprisingly, the weighted average OR total cost was also found to be highest in the Americas at $9,057. In the EMEA, a weighted average OR total costs of $4,569 was determined. The lowest average OR total cost was reported in the Asia-Pacific region at $942. No obvious trends were observed for OR cost components across different procedure types or approaches, although hysterectomy tended to have several reports of OR costs in the lower range.
and present data for outcomes that represent unit costs, either OR time cost per minute or ward cost per day, rather than total costs. The weighted average OR time cost per minute ranged from $9.81 (robotic lobectomy, EMEA) to $34.16 (robotic hepatic resection, Americas); however, the overall weighted average across procedures for each region was $13.90 (EMEA), $14.29 (Asia-Pacific) and $24.83 (Americas) (). For the ward cost per day, the weighted average cost ranged from $31.88 (open lobectomy, Asia-Pacific) to $1,148 (laparoscopic hepatic resection, Asia-Pacific); however, the overall weighted averages across procedures for each region was $216.21 (Asia-Pacific), $574.37 (EMEA), and $966.22 (Americas) (). It should be noted that unit cost data for the Asia-Pacific region was reported by very few studies; however, existing data did show values that were typically comparable or lower than EMEA. Across studies, the geometric mean of the OR time cost per hour and ward cost per hour ratio was calculated to be $51.97; thus, 1 h of OR time was calculated to be over 50 times as costly as 1 h of ward time. In other words, reducing OR time by 30 min equates to saving approximately 1 day of ward time.
Table 3. OR time cost per minute by region and procedure in 2018 USD.
Table 4. Ward cost per day by region and procedure in 2018 USD.
illustrates the percentage breakdown of the various cost components to better understand how each cost component contributes to the overall total admission cost. This cost-breakdown was performed only for laparoscopic and thoracoscopic procedures, but it is expected that the breakdown would be reasonably similar across surgical approaches. The OR time costs were found to account for approximately one third of the total admission cost, irrespective of region. When considering the OR total cost (i.e. supplies + room/staff), OR total costs accounted for close to 50% or more of the total admission costs. Comparatively, the ward cost was highly variable across procedure types and regions and it accounted for between 5% and 53% of the total admission cost.
Discussion
This review was conducted to comprehensively describe hospital admission and operating costs for a range of procedures and regions to help inform health economic analyses and decision-making that is focused on optimizing healthcare resource use related to surgical procedures. The large set of studies within our review included a range of ventral cavity procedures, including major organs (e.g. liver and lung), many of which are commonly performed, and therefore highly relevant to cost control discussions. Results of this review demonstrated that the Americas, which included studies predominantly from the United States, typically reported the highest hospital costs (i.e. OR, ward, and total admission) and this was often irrespective of procedure type. Comparatively, studies conducted in EMEA reported lower surgical costs, sometimes comparable to Asia-Pacific. This is not surprising as it is generally understood that the United States has some of the highest healthcare costs globally. In 2016, the United States spent 17.8% of its gross domestic product on healthcare, which is 5–10% higher as an absolute percentage than other developed nationsCitation119. Despite higher overall costs, the Americas showed similar hospital cost component breakdowns to other regions. Data were stratified for open, laparoscopic, and robotic procedures; however, no obvious patterns emerged amongst these approaches.
Unit costs, such as operating cost per minute and ward cost per day, are often considered as an essential component of any economic analysis involving hospital technologies, including medical devices. Our review provides an assessment of how these costs can vary across procedures and regions, allowing refined economic evaluations amenable to target settings. Specifically, surgical products that require fewer people and steps, can be more time efficient in the operating room. Technologies that help to reduce surgical complications, can lead to a reduced length of stay and thus save on overall hospital costs. Essentially, an economic analysis can help to demonstrate that the upfront cost of an innovative and effective medical device can be partially or completely offset by averted minutes (operating room) or hours (ward stay) of hospital resources. Several published analyses have shown that reducing length of stay and/or operative time can lead to significant cost savings for hospital payersCitation120–126.
When referring to operating costs, it is important to mention that time saved by medical devices may need to be applied to OR time only, rather than OR time plus supplies (i.e. total OR cost). This is because supply costs may not be expected to be altered by the medical device. However, this may not always be the case, because sometimes supply costs may also be a function of time. Our study reports that OR time costs, and OR total costs, comprise approximately one-third and one-half of hospital admission costs, respectively. In general, the concept “if you save time, you will save money” is well known with respect to operating timeCitation120. Indeed, Cheng et al.Citation127 found that as many as 87% of studies across several types of surgery (including abdominal and thoracic surgeries) found significant associations between operative time and SSI. These authors recommend measures that reduce operating time and optimize work flow so that patient burden is ultimately reduced. Similarly, ShippertCitation120 noted that use of the operating room is now an extremely costly endeavor; therefore, time-saving products have become increasingly important. In their analysis, it was reported that to save more than $100,000, the surgeon has to save only approximately 7 surgical minutes per case on 250 cases. It is important to note that their analysis focused on cosmetic surgery and reported an operating room fee per minute of $62Citation120. As this fee likely reflects a charge, it is expected that this would be higher than the average operating room cost per minute reported in our study of approximately $25 per minute for all studies included in this review. This relates to the finding of Childers and Maggard-GibbonsCitation128 who found a mean cost of $37.45 (2014 USD) per minute of OR time in California’s hospitals. These authors add that the cost of OR time significantly rose between 2004 and 2014. It is well known that charges are often much higher than the true cost/expense to deliver care in the United States due to consideration of profit margins and other factors. In our study, we chose to consistently focus on hospital costs, rather than charges, to allow full comparability. However, it is also conceivable that charges would be of interest when assessing economic value given that time saved can equate to potential revenue gained from completing additional procedures. In summary, careful assessment during economic evaluations is required to accurately incorporate economic benefits of reducing operating time, whether this involves consideration of supply costs or only time, and whether charges are ever relevant to consider.
Our assessment determined that the average ratio of operating room to ward costs per hour was approximately 50. In other words, saving a half hour of operating time equates to saving approximately 1 day of ward time in costs. This finding also illustrates the notion that operating time is perhaps one of the most valuable target measures for savings. Although not directly explored by ShippertCitation120, but illustrated by this review and other analyses, reducing length of stay can also have an important impact on reducing hospital expendituresCitation121–123. Overall, in development of innovative technologies, measures that save operative time and reduce length of stay should be prioritized as they may have a profound effect on hospital budgets.
Although not directly quantified in this review, postoperative complications can have an important impact on total hospital admission costs. Such outcomes may be indirectly reflected in several cost components, including operative, ward, and other hospital admission (e.g. intensive care) costs. Typically, innovative technologies that reduce such complications can have a beneficial impact on reducing all of these hospital resource components, in addition to hospital readmissionsCitation129. In today’s healthcare reform environment, several measures are being undertaken to penalize hospitals for complications, such as hospital-acquired infections, as well as hospital re-admissions. Quantifying such benefits should also be conducted in economic evaluations to represent the complete economic impact or savings of a new medical technology.
Our review has some important limitations. Specifically, only a subset of surgical procedures was included in the study to limit the scope of the review due to large quantity of data available. We focused on several major organ procedures (e.g. liver and lung) within the ventral cavity; however, we recognize that this may not be representative of all organ-related ventral cavity procedures (e.g. gallbladder, pancreas). Although our study did show some variation in costs across procedures, the largest variation was in fact observed across regions, thus emphasizing the importance of region-specific adaptations. Using our study as a framework, future study should evaluate such cost outcomes across a wider subset of procedures to determine if our findings are generalizable. Similarly, stratifying bariatric surgery (e.g. gastric bypass, sleeve gastrectomy), as distinct from gastrectomy may create some confusion for our readership. Bariatric surgery was included as its own category to distinguish surgeries that aimed to treat obesity from those of other indications. Second, data were largely lacking in Asia-Pacific regions, sometimes making findings for ventral procedures inconclusive for certain outcomes. As the focus on health technology assessment and economic evaluation is rising in such regions, more emphasis should be placed on the quantification of hospital costs in Asia-Pacific. Third, we did not conduct a meta-analysis of findings given the potential for high heterogeneity in resource use across various regions. Our goal was to provide more of a qualitative assessment so that findings can be uniquely interpreted according to region and procedure-specific needs. Fourth, within any one category of outcomes, the number of studies is small (typically less than 5), except for hysterectomy. This is due to a combination of limited data in the area as well as limiting the analysis to the past several years to increase relevancy of findings. As such, caution is exercised in interpreting some of these findings and readers are encouraged to review the selected original studies in context of their targeted needs to further understand generalizability. Last, our study was meant to provide a report on the variation in costs across regions and procedures rather than assess causative factors. It is unknown if enough data would be available to accurately and appropriately inform statistical analyses that could help to explain some of the observed variation. As a next step, with more defined research questions (e.g. a selected procedure type in a specific region) and abundant data on patient characteristics, regression analyses may be able to more comprehensively assess sources of cost variation.
Conclusion
This structured literature review provided a comprehensive view of hospital costs and cost components across various surgical procedures, approaches and geographical regions. The results showed high costs reported by studies performed in the Americas, with studies performed in EMEA and Asia-Pacific often reporting much lower costs. A cost-breakdown of the various cost components demonstrated that total OR costs comprise over 50% of the total admission cost and that operating room costs can be approximately 50 times that of ward cost per same unit of measure. Our findings indicate that novel medical technologies that aim to reduce operative costs, as well as other hospital resources, can potentially be associated with substantial resource savings for hospital payers, despite higher upfront costs. Future research should focus on regional data gaps identified by this review as well as explore other procedure types which were not captured here.
Transparency
Declaration of funding
This work was supported by Ethicon, Inc. who provided funding to conduct the analysis and prepare the manuscript.
Declaration of financial/other relationships
BPC and JWC are employees of Ethicon, Inc. NF and APT are employees of Cornerstone Research Group, who were sponsored to perform this study by Ethicon, Inc. A JME peer reviewer has disclosed work on a research project for Ethicon Inc. Peer reviewers on this manuscript have no other relevant financial relationships or otherwise to disclose.
Supplemental Material
Download MS Word (130.8 KB)Acknowledgements
The authors would like to acknowledge Hang Cheng for her help with the conceptualization of this study. We would also like to acknowledge Satyanand Shastri for his critical review of this manuscript.
References
- Dieleman JL, Templin T, Sadat N. National spending on health by source for 184 countries beteen 2013 and 2040. The Lancet. 2016;387(10037):2521–2535.
- Shrime MG, Daniels KM, Meara JG. Half a billion surgical cases: aligning surgical delivery with best-performing health systems. Surgery. 2015;158(1):27–32.
- Debas HT, Gosselin R, McCord C, et al. Surgery. In: Jamison DT, Breman JG, Measham AR, editors. Disease control priorities in developing countries. 2nd ed. Washington (DC): Oxford University Press; 2006.
- Munoz E, Munoz W, 3rd, Wise L. National and surgical health care expenditures, 2005–2025. Ann Surg. 2010;251(2):195–200.
- Ismail I, Wolff S, Gronfier A, et al. A cost evaluation methodology for surgical technologies. Surg Endosc. 2015;29(8):2423–2432.
- Gosselin RA, Gialamas G, Atkin DM. Comparing the cost-effectiveness of short orthopedic missions in elective and relief situations in developing countries. World J Surg. 2011;35(5):951.
- Hoang Lan N, Laohasiriwong W, Stewart JF, et al. Cost of treatment for breast cancer in central Vietnam. Glob Health Action. 2013;6(1):18872.
- Hodges AM, Hodges SC. A rural cleft project in Uganda. Br J Plast Surg. 2000;53(1):7–11.
- Snowdon A, Zur R, Shell J. Transforming Canada into a Global Centre for Medical Device Innovation and Adoption. London, ON: Ivey Centre for Health Innovation and Leadership, University of Western Ontario; 2011.
- Mercier G, Naro G. Costing hospital surgey services: the method matters. PLoS One. 2014;9(5):e97290.
- Martelli N, Lelong A-S, Prognon P, et al. Hospital-based health technology assessment for innovative medical devices in university hospitals and the role of hospital pharmacists: learning from international experience. Int J Technol Assess Health Care. 2013;29(2):185–191.
- Shemilt I, Thomas J, Morciano M. A web-based tool for adjusting costs to a specific target currency and price year. Evid Policy. 2010;6(1):51–59.
- Campbell Collaboration, Eppi-Centre. CCEMG - EPPI-Centre Cost Converter. https://eppi.ioe.ac.uk/costconversion/default.aspx.
- CPI-All Urban Consumers (Current Series) [Internet]. 2018. [cited 2018 Aug 24]. Available from: https://data.bls.gov/cgi-bin/surveymost.
- Dalton K, Freeman S, Bragg A. Refining cost to charge rations for calculating APC and MS-DRG relative payment weights. North Carolina, USA: RTI International; 2008; p. 1–266.
- Abu Hilal M, Di Fabio F, Syed S, et al. Assessment of the financial implications for laparoscopic liver surgery: a single-centre UK cost analysis for minor and major hepatectomy. Surg Endosc. 2013;27(7):2542–2550.
- Alpay L, Lacin T, Teker D, et al. A comparative cost analysis study of lobectomy performed via video-assisted thoracic surgery versus thoracotomy in Turkey. WIITM. 2014;9(3):409–414.
- Arkadopoulos N, Gemenetzis G, Danias N, et al. Cost-effective surgical management of liver disease amidst a financial crisis. World J Surg. 2016;40(7):1695–1701.
- Augustin F, Bodner J, Maier H, et al. Robotic-assisted minimally invasive vs. thoracoscopic lung lobectomy: comparison of perioperative results in a learning curve setting. Langenbecks Arch Surg. 2013;398(6):895–901.
- Avondstondt AM, Wallenstein M, D’Adamo CR, et al. Change in cost after 5 years of experience with robotic-assisted hysterectomy for the treatment of endometrial cancer. J Robot Surg. 2017;12(1):93–96.
- Baffert S, Alran S, Fourchotte V, et al. Laparoscopic hysterectomy after concurrent radiochemotherapy in locally advanced cervical cancer compared to laparotomy: A multi institutional prospective pilot study of cost, surgical outcome and quality of life. Eur J Surg Oncol. 2016;42(3):391–399.
- Bell R, Pandanaboyana S, Hanif F, et al. A cost effective analysis of a laparoscopic versus an open left lateral sectionectomy in a liver transplant unit. HPB. 2015;17(4):332–336.
- Bertani E, Chiappa A, Biffi R, et al. Assessing appropriateness for elective colorectal cancer surgery: clinical, oncological, and quality-of-life short-term outcomes employing different treatment approaches. Int J Colorectal Dis. 2011;26(10):1317–1327.
- Berto P, Lopatriello S, Aiello A, et al. Cost of laparoscopy and laparotomy in the surgical treatment of colorectal cancer. Surg Endosc. 2012;26(5):1444–1453.
- Bhojani FD, Fox A, Pitzul K, et al. Clinical and economic comparison of laparoscopic to open liver resections using a 2-to-1 matched pair analysis: an institutional experience. J Am Coll Surg. 2012;214(2):184–195.
- Bogani G, Multinu F, Dowdy SC, et al. Incorporating robotic-assisted surgery for endometrial cancer staging: Analysis of morbidity and costs. Gynecol Oncol. 2016;141(2):218–224.
- Cannon RM, Scoggins CR, Callender GG, et al. Financial comparison of laparoscopic versus open hepatic resection using deviation-based cost modeling. Ann Surg Oncol. 2013;20(9):2887–2892.
- Chang TC, Chen CC, Wang MY, et al. Gasless laparoscopy-assisted distal gastrectomy for early gastric cancer: analysis of initial results. J Laparoendosc Adv Surg Tech A. 2011;21(3):215–220.
- Cho HY, Park ST, Kim HB, et al. Surgical outcome and cost comparison between total vaginal hysterectomy and laparoscopic hysterectomy for uteri weighing >500 g. J Minim Invasive Gynecol. 2014;21(1):115–119.
- Cho S, Do YW, Lee EB. Comparison of costs for video-assisted thoracic surgery lobectomy and open lobectomy for non-small cell lung cancer. Surg Endosc. 2011;25(4):1054–1061.
- Coronado PJ, Herraiz MA, Magrina JF, et al. Comparison of perioperative outcomes and cost of robotic-assisted laparoscopy, laparoscopy and laparotomy for endometrial cancer. Eur J Obstet Gynecol Reprod Biol. 2012;165(2):289–294.
- Crawshaw BP, Chien HL, Augestad KM, et al. Effect of laparoscopic surgery on health care utilization and costs in patients who undergo colectomy. JAMA Surg. 2015;150(5):410–415.
- Daskalaki D, Gonzalez-Heredia R, Brown M, et al. Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Tech A. 2017;27(4):375–382.
- Davis BR, Yoo AC, Moore M, et al. Robotic-assisted versus laparoscopic colectomy: cost and clinical outcomes. JSLS. 2014;18(2):211–224.
- Dayaratna S, Goldberg J, Harrington C, et al. Hospital costs of total vaginal hysterectomy compared with other minimally invasive hysterectomy. Am J ObstetGynecol. 2014;210(2):120–126.
- de Angelis N, Brunetti F, Felli E, et al. Laparoscopic versus open gastric wedge resection for primary gastrointestinal tumors: clinical outcomes and health care costs analysis. Surg Laparosc Endosc Percutan Tech. 2015;25(2):143–146.
- de Angelis N, Lizzi V, Azoulay D, et al. Robotic versus laparoscopic right colectomy for colon cancer: analysis of the initial simultaneous learning curve of a surgical fellow. J Laparoendosc Adv Surg Tech A. 2016;26(11):882–892.
- Deen SA, Wilson JL, Wilshire CL, et al. Defining the cost of care for lobectomy and segmentectomy: a comparison of open, video-assisted thoracoscopic, and robotic approaches. Ann Thorac Surg. 2014;97(3):1000–1007.
- Desille-Gbaguidi H, Hebert T, Paternotte-Villemagne J, et al. Overall care cost comparison between robotic and laparoscopic surgery for endometrial and cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2013;171(2):348–352.
- Dokmak S, Raut V, Aussilhou B, et al. Laparoscopic left lateral resection is the gold standard for benign liver lesions: a case-control study. HPB (Oxford). 2014;16(2):183–187.
- Ehrlich A, Kellokumpu S, Wagner B, et al. Comparison of laparoscopic and open colonic resection within fast-track and traditional perioperative care pathways: Clinical outcomes and in-hospital costs. Scand J Surg. 2015;104(4):211–218.
- Eklind S, Lindfors A, Sjoli P, et al. A prospective, comparative study on robotic versus open-surgery hysterectomy and pelvic lymphadenectomy for endometrial carcinoma. Int J Gynecol Cancer. 2015;25(2):250–256.
- El Hachem L, Andikyan V, Mathews S, et al. Robotic single-site and conventional laparoscopic surgery in gynecology: clinical outcomes and cost analysis of a matched case-control study. J Minim Invasive Gynecol. 2016;23(5):760–768.
- Fretland AA, Dagenborg VJ, Bjornelv GMW, et al. Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg. 2018;267(2):199–207.
- Glenn JA, Turaga KK, Gamblin TC, et al. Minimally invasive gastrectomy for cancer: current utilization in US academic medical centers. Surg Endosc. 2015;29(12):3768–3775.
- Gounder ST, Wijayanayaka DR, Murphy R, et al. Costs of bariatric surgery in a randomised control trial (RCT) comparing Roux en Y gastric bypass vs sleeve gastrectomy in morbidly obese diabetic patients. N Z Med J. 2016;129(1443):43–52.
- Gu Y, Zhu L, Liu A, et al. Analysis of hysterectomies for patients with uterine leiomyomas in China in 2010. Int J Gynaecol Obstet. 2015;129(1):71–74.
- Hagen ME, Rohner P, Jung MK, et al. Robotic gastric bypass surgery in the Swiss Health Care System: analysis of hospital costs and reimbursement. Obes Surg. 2017;27(8):2099–2105.
- Halabi WJ, Kang CY, Jafari MD, et al. Robotic-assisted colorectal surgery in the United States: a nationwide analysis of trends and outcomes. World J Surg. 2013;37(12):2782–2790.
- Hanafi M. Comparative study of vaginal, abdominal, and robotic laparoscopic hysterectomy: clinical outcome and cost. J Gynecol Surg. 2015;31(5):260–265.
- Hardy KM, Kwong J, Pitzul KB, et al. A cost comparison of laparoscopic and open colon surgery in a publicly funded academic institution. Surg Endosc. 2014;28(4):1213–1222.
- Hayashi H, Ozaki N, Ogawa K, et al. Assessing the economic advantage of laparoscopic vs. open approaches for colorectal cancer by a propensity score matching analysis. Surg Today. 2017;48(4):439–448.
- Hollis RH, Cannon JA, Singletary BA, et al. Understanding the value of both laparoscopic and robotic approaches compared to the open approach in colorectal surgery. J Laparoendosc Adv Surg Tech A. 2016;26(11):850–856.
- Ijah RF, Bhatia P, Kaltan S, et al. Sleeve gastrectomy for morbid obesity: robotic vs standard laparoscopic sleeve gastrectomy methods. WJOLS. 2014;7(1):1–6.
- Ind TEJ, Marshall C, Hacking M, et al. Introducing robotic surgery into an endometrial cancer service–a prospective evaluation of clinical and economic outcomes in a UK institution. Int J Med Robotics Comput Assist Surg. 2016;12(1):137–144.
- Jiang HT, Cao JY. Impact of laparoscopic versus open hepatectomy on perioperative clinical outcomes of patients with primary hepatic carcinoma. Chin Med Sci J. 2015;30(2):80–83.
- Jonsdottir GM, Jorgensen S, Cohen SL, et al. Increasing minimally invasive hysterectomy: effect on cost and complications. Obstet Gynecol. 2011;117(5):1142–1149.
- Kawaguchi Y, Otsuka Y, Kaneko H, et al. Comparisons of financial and short-term outcomes between laparoscopic and open hepatectomy: benefits for patients and hospitals. Surg Today. 2016;46(5):535–542.
- Keller DS, Delaney CP, Hashemi L, et al. A national evaluation of clinical and economic outcomes in open versus laparoscopic colorectal surgery. Surg Endosc. 2016;30(10):4220–4228.
- Keller DS, Senagore AJ, Lawrence JK, et al. Comparative effectiveness of laparoscopic versus robot-assisted colorectal resection. Surg Endosc. 2014;28(1):212–221.
- Khullar OV, Fernandez FG, Perez S, et al. Time is money: hospital costs associated with video-assisted thoracoscopic surgery lobectomies. Ann Thorac Surg. 2016;102(3):940–947.
- Kim Y, Kim YW, Choi IJ, et al. Cost comparison between surgical treatments and endoscopic submucosal dissection in patients with early gastric cancer in Korea. Gut Liver. 2015;9(2):174–180.
- Kuwabara K, Matsuda S, Fushimi K, et al. Quantitative assessment of the advantages of laparoscopic gastrectomy and the impact of volume-related hospital characteristics on resource use and outcomes of gastrectomy patients in Japan. Ann Surg. 2011;253(1):64–70.
- Leitao MM, Jr., Bartashnik A, Wagner I, et al. Cost-effectiveness analysis of robotic-assisted laparoscopy for newly diagnosed uterine cancers. Obstet Gynecol. 2014;123(5):1031–1037.
- Li JC, Leung KL, Ng SS, et al. Laparoscopic-assisted versus open resection of right-sided colonic cancer–a prospective randomized controlled trial. Int J Colorectal Dis. 2012;27(1):95–102.
- Liu Z, Wang GY, Chen YG, et al. Cost comparison between hand-assisted laparoscopic colectomy and open colectomy. J Laparoendosc Adv Surg Tech A. 2012;22(3):209–213.
- Mafe JJ, Planelles B, Asensio S, et al. Cost and effectiveness of lung lobectomy by video-assisted thoracic surgery for lung cancer. J Thorac Dis. 2017;9(8):2534–2543.
- Marino P, Houvenaeghel G, Narducci F, et al. Cost-effectiveness of conventional vs robotic-assisted laparoscopy in gynecologic oncologic indications. Int J Gynecol Cancer. 2015;25(6):1102–1108.
- Martin RC, Mbah NA, St Hill R, et al. Laparoscopic versus open hepatic resection for hepatocellular carcinoma: improvement in outcomes and similar cost. World J Surg. 2015;39(6):1519–1526.
- Masoomi H, Nguyen NT, Stamos MJ, et al. Overview of outcomes of laparoscopic and open Roux-en-Y gastric bypass in the United States. Surg Technol Int. 2012;22:72–76.
- Medbery RL, Chadid TS, Sweeney JF, et al. Laparoscopic vs open right hepatectomy: a value-based analysis. J Am Coll Surg. 2014;218(5):929–939.
- Medbery RL, Perez SD, Force SD, et al. Video-assisted thoracic surgery lobectomy cost variability: implications for a bundled payment era. Ann Thorac Surg. 2014;97(5):1686–1692.
- Michalopoulos NV, Theodoropoulos GE, Stamopoulos P, et al. A cost-utility analysis of laparoscopic vs open treatment of colorectal cancer in a public hospital of the Greek National Health System. J BUON. 2013;18(1):86–97.
- Moawad GN, Abi Khalil ED, Tyan P, et al. Comparison of cost and operative outcomes of robotic hysterectomy compared to laparoscopic hysterectomy across different uterine weights. J Robotic Surg. 2017;11(4):433–439.
- Mohammed WE, Salama F, Tharwat A, et al. Vaginal hysterectomy versus laparoscopically assisted vaginal hysterectomy for large uteri between 280 and 700 g: a randomized controlled trial. Arch Gynecol Obstet. 2017;296(1):77–83.
- Murata A, Okamoto K, Muramatsu K, et al. Time trend of medical economic outcomes of endoscopic submucosal dissection for gastric cancer in Japan: a national database analysis. Gastric Cancer. 2014;17(2):294–301.
- Orenstein SB, Elliott HL, Reines LA, et al. Advantages of the hand-assisted versus the open approach to elective colectomies. Surg Endosc. 2011;25(5):1364–1368.
- Park JS, Choi GS, Park SY, et al. Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg. 2012;99(9):1219–1226.
- Park JY, Jo MJ, Nam BH, et al. Surgical stress after robot-assisted distal gastrectomy and its economic implications. Br J Surg. 2012;99(11):1554–1561.
- Paul S, Jalbert J, Isaacs AJ, et al. Comparative effectiveness of robotic-assisted vs thoracoscopic lobectomy. Chest. 2014;146(6):1505–1512.
- Pellegrino A, Damiani GR, Fachechi G, et al. Cost analysis of minimally invasive radical hysterectomy for cervical cancer performed by a single surgeon in an Italian center: an update in gynecologic oncological field. Updates Surg. 2017;69(4):517–522.
- Pellegrino A, Damiani GR, Fachechi G, et al. Cost analysis of minimally invasive hysterectomy vs open approach performed by a single surgeon in an Italian center. J Robotic Surg. 2017;11(2):115–121.
- Pepper VK, Rager TM, Diefenbach KA, et al. Robotic vs. laparoscopic sleeve gastrectomy in adolescents; reality or hype. Obes Surg. 2016;26(8):1912–1917.
- Piwkowski C, Gabryel P, Galecki B, et al. High costs as a slow down factor of thoracoscopic lobectomy development in Poland - an institutional experience. WIITM. 2013;8(4):334–341.
- Ramos R, Masuet C, Gossot D. Lobectomy for early-stage lung carcinoma: a cost analysis of full thoracoscopy versus posterolateral thoracotomy. Surg Endosc. 2012;26(2):431–437.
- Reynisson P, Persson J. Hospital costs for robot-assisted laparoscopic radical hysterectomy and pelvic lymphadenectomy. Gynecol Oncol. 2013;130(1):95–99.
- Rodgers-Fischl PM, Martin JT, Saha SP. Video-assisted thoracoscopic versus open lobectomy: costs and outcomes. Southern Med J. 2017;110(3):229–233.
- Rossitto C, Gueli AS, Romano F, et al. Use of robot-specific resources and operating room times: the case of Telelap Alf-X robotic hysterectomy. Int J Med Robotics Comput Assist Surg. 2016;12(4):613–619.
- Roy S, Yoo A, Yadalam S, et al. Comparison of economic and clinical outcomes between patients undergoing laparoscopic bariatric surgery with powered versus manual endoscopic surgical staplers. J Med Econ. 2017;20(4):423–433.
- Salloum C, Lim C, Lahat E, et al. Robotic-assisted versus laparoscopic left lateral sectionectomy: analysis of surgical outcomes and costs by a propensity score matched cohort study. World J Surg. 2017;41(2):516–524.
- Schraibman V, Macedo AL, Epstein MG, et al. Comparison of the morbidity, weight loss, and relative costs between robotic and laparoscopic sleeve gastrectomy for the treatment of obesity in Brazil. Obes Surg. 2014;24(9):1420–1424.
- Scozzari G, Rebecchi F, Millo P, et al. Robot-assisted gastrojejunal anastomosis does not improve the results of the laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2011;25(2):597–603.
- Scribner DR, Andre T, Lara-Torre E, et al. Cost analysis of robotic versus standard laparoscopic hysterectomies: a preliminary analysis. J Gynecol Surg. 2012;28(4):255–261.
- Sham JG, Richards MK, Seo YD, et al. Efficacy and cost of robotic hepatectomy: is the robot cost-prohibitive? J Robot Surg. 2016;10(4):307–313.
- Sheng QS, Lin JJ, Chen WB, et al. Hand-assisted laparoscopic versus open right hemicolectomy: short-term outcomes in a single institution from China. Surg Laparosc Endosc Percutan Tech. 2012;22(3):267–271.
- Stewart DB, Berg A, Messaris E. Single-site laparoscopic colorectal surgery provides similar lengths of hospital stay and similar costs compared with standard laparoscopy: results of a retrospective cohort study. J Gastrointest Surg. 2014;18(4):774–781.
- Stoot JH, van Dam RM, Coelen RJ, et al. The introduction of a laparoscopic liver surgery programme: a cost analysis of initial experience in a university hospital. Scand J Surg. 2012;101(1):32–37.
- Swanson SJ, Miller DL, McKenna RJ Jr, et al. Comparing robot-assisted thoracic surgical lobectomy with conventional video-assisted thoracic surgical lobectomy and wedge resection: results from a multihospital database (Premier). J Thorac Cardiovasc Surg. 2014;147(3):929–937.
- Tantraworasin A, Seateang S, Bunchungmongkol N. Staplers versus hand-sewing for pulmonary lobectomy: randomized controlled trial. Asian Cardiovasc Thorac Ann. 2014;22(3):309–314.
- Tapper AM, Hannola M, Zeitlin R, et al. A systematic review and cost analysis of robot-assisted hysterectomy in malignant and benign conditions. Eur J Obstet Gynecol Reprod Biol. 2014;177:1–10.
- Tegels JJ, Silvius CE, Spauwen FE, et al. Introduction of laparoscopic gastrectomy for gastric cancer in a Western tertiary referral centre: A prospective cost analysis during the learning curve. WJGO. 2017;9(5):228–234.
- Thompson BS, Coory MD, Gordon LG, et al. Cost savings for elective laparoscopic resection compared with open resection for colorectal cancer in a region of high uptake. Surg Endosc. 2014;28(5):1515–1521.
- Turunen H, Pakarinen P, Sjoberg J, et al. Laparoscopic vs robotic-assisted surgery for endometrial carcinoma in a centre with long laparoscopic experience. J Obstet Gynaecol. 2013;33(7):720–724.
- Vaid S, Tucker J, Bell T, et al. Cost analysis of laparoscopic versus open colectomy in patients with colon cancer: results from a large nationwide population database. Am Surg. 2012;78(6):635–641.
- van der Linden YT, Govaert JA, Fiocco M, et al. Single center cost analysis of single-port and conventional laparoscopic surgical treatment in colorectal malignant diseases. Int J Colorectal Dis. 2017;32(2):233–239.
- Vasudevan V, Reusche R, Wallace H, et al. Clinical outcomes and cost-benefit analysis comparing laparoscopic and robotic colorectal surgeries. Surg Endosc. 2016;30(12):5490–5493.
- Veenhof AA, van der Pas MH, van der Peet DL, et al. Laparoscopic versus transverse Incision right colectomy for colon carcinoma. Colorectal Dis. 2011;13(1):e1–e5.
- Venkat P, Chen LM, Young-Lin N, et al. An economic analysis of robotic versus laparoscopic surgery for endometrial cancer: costs, charges and reimbursements to hospitals and professionals. Gynecol Oncol. 2012;125(1):237–240.
- Villamere J, Gebhart A, Vu S, et al. Utilization and outcome of laparoscopic versus robotic general and bariatric surgical procedures at Academic Medical Centers. Surg Endosc. 2015;29(7):1729–1736.
- Wang BY, Huang JY, Ko JL, et al. A population-based cost analysis of thoracoscopic versus open lobectomy in primary lung cancer. Ann Surg Oncol. 2016;23(6):2094–2098.
- Wang XT, Wang HG, Duan WD, et al. Pure laparoscopic versus open liver resection for primary liver carcinoma in elderly patients: a single-center, case-matched study. Medicine. 2015;94(43):e1854. 2015.
- Wright KN, Jonsdottir GM, Jorgensen S, et al. Costs and outcomes of abdominal, vaginal, laparoscopic and robotic hysterectomies. JSLS. 2012;16(4):519–524.
- Yang C, Mo L, Ma Y, et al. A comparative analysis of lung cancer patients treated with lobectomy via three-dimensional video-assisted thoracoscopic surgery versus two-dimensional resection. J Thorac Dis. 2015;7(10):1798–1805.
- Yasunaga H, Horiguchi H, Kuwabara K, et al. Outcomes after laparoscopic or open distal gastrectomy for early-stage gastric cancer: a propensity-matched analysis. Ann Surg. 2013;257(4):640–646.
- Yu X, Lum D, Kiet TK, et al. Utilization of and charges for robotic versus laparoscopic versus open surgery for endometrial cancer. J Surg Oncol. 2013;107(6):653–658.
- Yu YD, Kim KH, Jung DH, et al. Robotic versus laparoscopic liver resection: a comparative study from a single center. Langenbecks Arch Surg. 2014;399(8):1039–1045.
- Zhang X, Yan L, Li B, et al. Comparison of laparoscopic radiofrequency ablation versus open resection in the treatment of symptomatic-enlarging hepatic hemangiomas: a prospective study. Surg Endosc. 2016;30(2):756–763.
- Zhou T, Zhang G, Tian H, et al. Laparoscopic rectal resection versus open rectal resection with minilaparotomy for invasive rectal cancer. J Gastrointest Oncol. 2014;5(1):36–45.
- Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319(10):1024–1039.
- Shippert RD. A study of time-dependent operating room fees and how to save $100 000 by using time-saving products. Am J Cosmet Surg. 2005;22(1):25–34.
- Corral M, Ferko N, Hogan A. A hospital cost analysis of a fibrin sealant patch in soft tissue and hepatic surgical bleeding. CEOR. 2016;8:507–519.
- Ernst FR, Chen E, Lipkin C, et al. Comparison of hospital length of stay, costs, and readmissions of alteplase versus catheter replacement among patients with occluded central venous catheters. J Hosp Med. 2014;9(8):490–496.
- Zaraca F, Vaccarili M, Zaccagna G, et al. Cost-effectiveness analysis of sealant impact in management of moderate intraoperative alveolar air leaks during video-assisted thoracoscopic surgery lobectomy: a multicentre randomised controlled trial. J Thorac Dis. 2017;9(12):5230–5238.
- Tomaszewski KJ, Ferko N, Hollmann SS, et al. Time and resources of peripherally inserted central catheter insertion procedures: a comparison between blind insertion/chest X-ray and a real time tip navigation and confirmation system. Clinicoecon Outcomes Res. 2017;9:1–11.
- Cheng H, Soleas IM, Ferko NC, et al. Hospital costs associated with thyroidectomy performed with a Harmonic device compared to conventional techniques: a systematic review and meta-analysis. J Med Econ. 2016;19(8):750–758.
- Cheng H, Clymer JW, Qadeer RA, et al. Procedure costs associated with the use of Harmonic devices compared to conventional techniques in various surgeries: a systematic review and meta-analysis. CEOR. 2018;10:399–412.
- Cheng H, Chen BP, Soleas IM, et al. Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect (Larchmt). 2017;18(6):722–735.
- Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153(4):e176233.
- Lawson EH, Hall BL, Louie R, et al. Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann Surg. 2013;258(1):10–18.