Abstract
Aim: We investigated cost effectiveness of benralizumab vs. standard of care (SOC) plus oral corticosteroids (OCS) for patients with severe, eosinophilic OCS-dependent asthma in Sweden.
Materials and methods: A three-state, cohort-based Markov model of data from three Phase III benralizumab clinical trials (ZONDA [NCT02075255], SIROCCO [NCT01928771], and CALIMA [NCT01914757]) was used to assess the incremental cost-effectiveness ratio of benralizumab vs. SOC plus OCS. Health outcomes were estimated in terms of quality-adjusted life-years (QALYs). The model included costs and disutilities associated with extrapolated OCS-related adverse events. Patients with severe asthma were defined as those receiving OCS ≥5 mg/day.
Results: Benralizumab demonstrated a cost-effectiveness ratio vs. SOC plus OCS of 2018 Swedish Kronor (SEK) 366,855 (€34,127) per QALY gained, based on increases of 1.33 QALYs and SEK 488,742 (€45,344) per patient. Benralizumab treatment costs contributed most to incremental costs. The probability of benralizumab’s being cost-effective with willingness-to-pay (WTP) thresholds between SEK 429,972 (€40,000) and SEK 752,452 (€70,000) ranged from 75% to 99%.
Limitations: Potential limitations of these analyses include the use of combined data from three different clinical trials, a one-way sensitivity analysis that did not include mortality and transition estimates, and Observational & Pragmatic Research Institute (OPRI) data from the UK as a proxy of the Swedish health care system.
Conclusions: The results of these analyses demonstrate that benralizumab has a high probability of being cost-effective compared with SOC plus OCS for a subgroup of patients with severe, eosinophilic asthma receiving regular OCS treatment and may support clinicians, payers and patients in making treatment decisions.
Introduction
The burden of severe asthma includes direct costs of medical treatments and health care services as well as indirect costs such as lost productivity, absenteeism and reduction in health-related quality of life (HRQOL)Citation1‒5. For the 30–40% of patients with severe asthma who require maintenance treatment with oral corticosteroids (OCS)Citation6‒11, the burden is even greater, including chronic comorbidities and adverse events such as cardiovascular, metabolic and gastrointestinal complicationsCitation12‒14. To optimally address both the clinical and economic burdens associated with severe asthma, treatment must be clinically efficacious and cost-effective, and the relevant patient population must be clearly defined.
OCS exposure constitutes a relevant marker for severe asthma. Treatment with OCS is common during recovery from exacerbations, and clinical trial inclusion criteria often employ OCS use as a marker of exacerbation severityCitation15–17. Defining a threshold of regular OCS use as an indicator of severe asthma is consistent with recommendations from the Global Initiative for Asthma (GINA), which indicate that treatment needed to control exacerbations and other symptoms should be considered in determining disease severityCitation18. OCS use is clinically important because health care professionals seek to minimize OCS exposure and the associated long-term comorbidities and adverse effects for their patients. OCS exposure can also be verified in databases that follow treatments administered over time, such as the Swedish pharmaceutical registry.
Reduction or elimination of OCS use was an outcome for the benralizumab clinical trial, ZONDA (NCT02075255)Citation17. Benralizumab is an interleukin (IL)-5 receptor alpha–directed cytolytic monoclonal antibody that induces direct, rapid and nearly complete depletion of eosinophils via enhanced antibody-dependent cell-mediated cytotoxicity, an apoptotic process of eosinophil elimination involving natural killer cellsCitation19,Citation20. The purpose of benralizumab treatment is to achieve asthma control for OCS-dependent patients while reducing OCS use, thereby minimizing or eliminating OCS-related adverse effects. In Phase III trials, benralizumab 30 mg administered subcutaneously every 8 weeks (every 4 weeks for the first three doses) reduced asthma exacerbations, improved lung function and decreased symptoms for patients with severe uncontrolled eosinophilic asthmaCitation15‒Citation17. The ZONDA trial also demonstrated that benralizumab treatment allowed patients with severe, uncontrolled eosinophilic asthma (baseline blood eosinophil counts ≥150 cells/µL) to achieve asthma control and maintain symptoms with reduced OCS treatment. Benralizumab-treated patients experienced a 75% reduction from baseline in median OCS dosage vs. 25% with placebo and a 70% reduction in mean annual exacerbation rate vs. placebo (p < 0.001)Citation17.
Availability of clinically effective and cost-effective treatments for severe asthma would be beneficial to patients. The biologics mepolizumab and reslizumab have been reported to be cost-effective for well-defined subsets of patients with severe asthma when substantial pricing discounts are appliedCitation21–25. In the UK, incremental cost-effectiveness ratio per quality-adjusted life-year (QALY) for mepolizumab was reported to be £29,163 to £32,557 for patients with severe eosinophilic asthma experiencing four or more exacerbations in the previous yearCitation21,Citation22. For reslizumab, a monoclonal anti–IL-5 antibody, incremental cost-effectiveness ratio per QALY compared with best standard care in the UK was £27,509 to £29,870 per QALY gained for adults with inadequately controlled asthma despite maintenance therapy with high-dosage inhaled corticosteroids plus another drug, blood eosinophil counts ≥400 cells/µL and ≥3 asthma exacerbations in the past 3 yearsCitation23,Citation24. Both mepolizumab and reslizumab required substantial pricing discounts to achieve these incremental cost-effectiveness ratiosCitation21–24. When the analyses included US pricing, biologic treatments for asthma, including omalizumab, dupilumab and benralizumab, were cost-effective only if prices were markedly reducedCitation25–27.
Using data primarily from ZONDA, we investigated the cost effectiveness of benralizumab treatment vs. standard of care (SOC), defined as high-dosage inhaled corticosteroids and additional controller(s), plus OCS for OCS-dependent patients with severe eosinophilic asthma in the Swedish health care system. The patients who would receive biologics for severe eosinophilic asthma in the open-care setting are treated with SOC plus OCS, making it the relevant comparator.
Methods
A cost-effectiveness model was designed to simulate the purpose of treatment with benralizumab. The model employed reduction of annual exacerbations as an indicator of improvement in asthma control. Health outcomes were estimated by QALYs. Data from the most severe patients in the benralizumab clinical study program populated the model. The ZONDA (NCT02075255) trial was used for most input variables, and when data from ZONDA had too few observations or were not available, the analysis was supplemented with data from the SIROCCO (NCT01928771) and CALIMA (NCT01914757) clinical trials. In these analyses, patients with severe asthma were defined as those receiving OCS ≥5 mg/day for a year, as there is consensus among Swedish clinicians that this defines a population with asthma with great medical needs.
Cost-effectiveness modelling approach
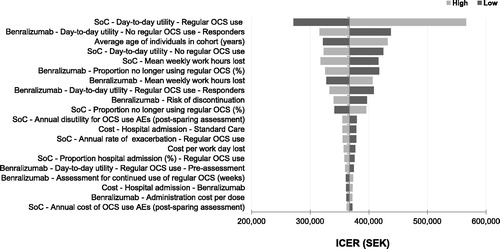
Given the cyclical and chronic nature of asthma, a three-state, cohort-based Markov model with 4-week cycles and a lifetime horizon was deemed appropriate for assessing the incremental cost-effectiveness ratio of benralizumab vs. SOC plus OCS. The incremental cost-effectiveness ratio is the difference between the cost of two interventions divided by the difference between the number of QALYs gained from each intervention. The model was developed in Microsoft Excel (Microsoft Corporationi) 2010; its structure is outlined in . At baseline, all patients in the model had OCS-dependent asthma (Group A, ). From baseline to Week 16 of the model, utilities, annualized exacerbation rates and cost data were mean values based on data from the ZONDA trial. To measure utilities, EQ-5D-5L was collected in the SIROCCO and CALIMA trials. Asthma Quality of Life Questionnaire (AQLQ) data from the ZONDA trial were converted to utilities based on an established mapping algorithmCitation28. At Week 16 of the model, patients were assumed to be assessed for treatment response (defined as any reduction in OCS use). The model takes into account the clinical and economic outcomes of both responders and non-responders throughout the lifetime horizon. For the non-responder subset (patients with no OCS reduction at Week 16; Group B, ), the model assumed that benralizumab treatment stopped and patients received SOC plus OCS. For this nonresponder subset, utilities, exacerbation rates and cost data after Week 16 were based on data from patients treated with SOC plus OCS in the ZONDA trial. For the responder subset (patients with any reduction in OCS use at Week 16; Group C, ), the model assumed that benralizumab treatment continued. For the responder subset, utilities, exacerbation rates and costs after Week 16 were assigned according to the mean values for the benralizumab group from the ZONDA trial. At Week 28, patients who responded were assumed to be assessed for achievement of OCS elimination, defined as complete discontinuation of OCS use by Week 28 (Group D, ). The comparatively small number of patients in ZONDA who achieved complete elimination of OCS (n = 22) reached this goal late in the study. Therefore, for patients with no OCS use after Week 28, utilities, exacerbation rates and cost data were extracted from the SIROCCO and CALIMA trials. Costs were evaluated from both a payer perspective, which includes only direct medical costs, and a societal perspective, which includes effects on patient welfare, other resource use and indirect costs such as time lost from work. The discount rate was 3% for both costs and benefits.
Figure 1. Structure of the Model for Predicting Cost Effectiveness. Abbreviations. ED, emergency department; OCS, oral corticosteroids.
To account for treatment discontinuation for reasons other than nonresponse, a fixed treatment discontinuation rate, derived from real-world evidence on biologic treatment for severe asthmaCitation29, was applied at each Markov cycle (every 4 weeks). Real-world evidence indicates that 17.5% of patients discontinued treatment with omalizumab. Of these patients, 23.5% discontinued for lack of efficacyCitation29; thus, 76.5% discontinued for reasons other than lack of efficacy. In the current model, lack of efficacy was captured as discontinuing benralizumab treatment at Week 16. Based on the above, the percentage of patients who would discontinue benralizumab treatment each year for reasons other than lack of efficacy was estimated as 76.5% × 17.5% which was 13.4%. This estimate is similar to the assumptions in the National Institute for Health and Care Excellence (NICE) appraisal committee guidance for mepolizumab in the UKCitation21,Citation22.
Patients could move between three health states: day-to-day asthma symptoms, asthma exacerbation or mortality. For day-to-day asthma symptoms (a state with no active exacerbations), a utility was applied to reflect the day-to-day HRQOL of patients with severe asthma (day-to-day utility; Supplementary Material 1). The exacerbation state is characterized by a worsening of asthma that required OCS burst, emergency department visit or hospitalizationCitation30. Mortality encompassed both age-specific all-cause mortality and asthma-related mortality. For exacerbations and mortality, the probabilities of movement between states were calculated based on annual exacerbation rates in the SIROCCO, CALIMA and ZONDA trials. Age-specific all-cause and asthma-attributable annual mortality rates were calculated from Statistics Sweden and The National Board of Health and Welfare. Costs in Swedish Kronor (SEK) were converted to Euros via the 2018 mean exchange rate (Euro 1 = SEK 10.75) from the European Central BankCitation31.
Model parameters and data sources
Parameters for patients treated with benralizumab and SOC plus OCS used in this model are presented in . Supplementary Material 2 presents mean daily dosage at baseline and at Week 16 for patients in the ZONDA clinical trial with baseline OCS dosages 7.5–15 mg/day (inclusive). Because of the structure of the step-wise OCS dosage reduction procedure in the ZONDA trial, only patients with baseline OCS dosages 7.5–15 mg/day could achieve complete OCS dosage reduction during the ZONDA trial. Annual exacerbation rates from ZONDA and SIROCCO/CALIMA are in Supplementary Material 3. Transitional probabilities for day-to-day asthma and exacerbation states, derived from the SIROCCO, CALIMA and ZONDA trialsCitation15–17, for benralizumab and SOC plus OCS are given in Supplementary Material 4. Model inputs for the impact of comorbid conditions and adverse events associated with OCS use were generated per Observational & Pragmatic Research Institute (OPRI) guidance (Supplementary Material 5).
Table 1. Regular OCS Inputs in the Base Case Model.
Based on previously published studiesCitation12,Citation32, additional cost data specific to Sweden were generated. Day-to-day utility values for patients with regular OCS treatment were mappedCitation28 from AQLQ data from the ZONDA trial. Utility decrements for exacerbations were derived from Lloyd et al.Citation33 while disease-specific utility data related to long term OCS comorbidities were derived from Sullivan et al.Citation34. For patients able to stop OCS treatment completely, or when data were not available in ZONDA, values were derived as pooled data from SIROCCO/CALIMA. Supplementary Material 6 shows unit costs sources. Costs are expressed in 2018 SEK (costs were converted to 2018 prices based on consumer price index available from Statistics Sweden; Supplementary Material 7). The list price for benralizumab was applied in the model, and because we assumed that all patients in both arms incurred costs for SOC plus OCS, these medical costs were not included. Indirect costs, including work hours lost for working age adults (below 65), were included in the base case analysis according to the guidelines of the Swedish Dental and Pharmaceutical Benefits AgencyCitation35. Mean hours worked per week in 2018 for employed persons in Sweden aged 15–74 years (37.13 h) was extracted from Statistics SwedenCitation36. Data collected from benralizumab clinical trialsCitation15–17 were used to determine average weekly work loss compared with placebo. Benralizumab treatment was associated with 10.23 work hours lost per week (4.82 because of health problems, 5.41 for other reasons). With SOC, these values were 12.96 h per week (5.12 because of health problems, 7.84 for other reasons). Discount rates of 3% were used for both costs and QALYs, in line with guidance from the Swedish Dental and Pharmaceutical Benefits AgencyCitation35.
Sensitivity analyses
A probabilistic sensitivity analysis was conducted to assess uncertainty around the cost-effectiveness results. For this analysis, the dosing of and unit cost for benralizumab values were the same as for the base cost-effectiveness analysis. All other parameters were varied. When information on the standard error (SE) or a parameter was missing, the SE was estimated by assuming variance of 10% and dividing the mean by 10Citation37. The values used in the probabilistic sensitivity analysis are specified in Supplementary Material 1.
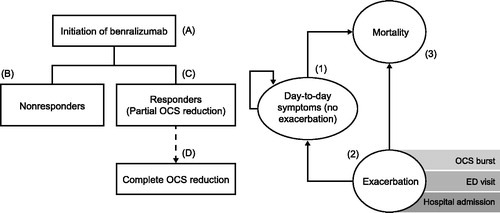
For the one-way sensitivity analysis, the impact of each parameter (except dosing of and unit cost for benralizumab) on the incremental cost-effectiveness ratio was determined by varying the parameter by 10% of the mean value. Proportions and utilities could not exceed a value of 1. A 10% variance in response assessment week was unfeasible because of the 4-week cycle length within the model. Therefore, response assessment week was varied to 14 weeks and 19 weeks. The parameters in the model, their distributions and their outer limits are provided in Supplementary Material 1.
Willingness-to-Pay threshold
There is no officially stated willingness-to-pay (WTP) threshold in Sweden. The World Health Organization’s CHOosing Interventions that are Cost-Effective (WHO-CHOICE) project encourages the use of thresholds based on per capita national incomesCitation38,Citation39. According to WHO, an intervention is considered cost-effective if it costs less than three times the national annual gross domestic product (GDP) per capita for each disability-adjusted life-year (DALY) avoided. An intervention that costs less than the national annual GDP per capita per DALY is considered very cost-effective. With this approach to a cost-per-QALY threshold for Sweden (GDP per capita: US $56,900), the threshold for very cost-effective interventions would be SEK 514,000 (€47,815) per QALY gained. This is similar to thresholds used in previous reimbursement decisions for drugs targeting diseases deemed similar to severe asthmaCitation40. However, because an official WTP threshold in Sweden is not published, probabilistic sensitivity analysis with the model was also used to estimate probability of cost-effectiveness across a range of WTP per QALY thresholds to test robustness of results.
Results
From a societal perspective, cost-effectiveness analysis results for benralizumab vs. SOC plus OCS demonstrated an incremental cost-effectiveness ratio of 2018 SEK 366,855 (€34,127), per QALY gained, based on increases of 1.33 QALYs and an incremental cost of SEK 488,742 (€45,467) per patient (). Treatment costs associated with benralizumab were the greatest contributor to incremental costs (). Applying a payer perspective resulted in an incremental cost-effectiveness ratio of SEK 465,972 (€43,349). The total costs were SEK 1,140,488 (€106,098) for benralizumab and SEK 519,697 (€48,347) for SOC plus OCS. The average discounted total cost of treatment per patient for Year 1 (when patients received one additional loading dose injection) and Year 2 were SEK 165,031 (€15,352) and SEK 107,020 (€9,956) for benralizumab and SEK 6,747 (€602) and SEK 6,013 (€559) for SOC plus OCS, respectively.
Table 2. Results from Base Case Cost-effectiveness Analysis.
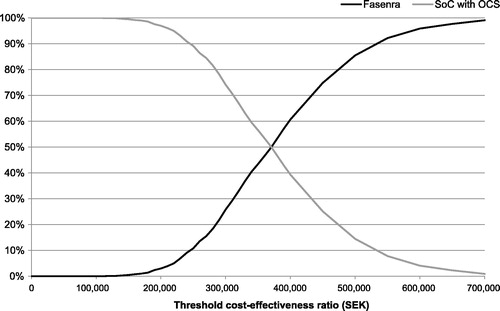
Uncertainty around the cost-effectiveness results is illustrated by plotting the results from the probabilistic sensitivity analysis providing incremental costs per incremental QALYs (). Through a WTP threshold of SEK 514,000 (€47,817), the probabilistic sensitivity analysis demonstrates low uncertainty of the cost-effectiveness results (). All iterations of benralizumab treatment for patients with severe eosinophilic asthma in the model were associated with a gain in QALYs and an increase in costs compared with SOC plus OCS. With an SEK 514,000 (€47,817) per QALY threshold, benralizumab has a strong probability (86%) of being cost-effective compared with SOC plus OCS (). Furthermore, as displayed in , the probability of benralizumab’s being cost-effective with WTP thresholds between SEK 429,972 (€40,000) and SEK 752,452 (€70,000) ranges from 75% to 99%.
Figure 2. Cost-effectiveness Plane for Benralizumab vs. SOC Plus OCS from Probabilistic Sensitivity Analysis. Abbreviations. OCS, oral corticosteroids; QALY, quality-adjusted life-year; SEK, Swedish Kronor (2018); SOC, standard of care. Values shown indicate the uncertainty around the incremental cost-effectiveness ratio.
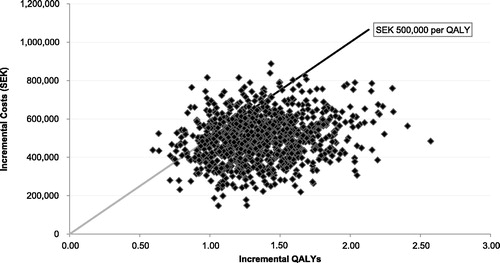
Figure 3. Cost-effectiveness Acceptability Curve for Benralizumab vs. SOC plus OCS. Abbreviations. OCS, oral corticosteroid; SEK, Swedish Kronor (2018); SOC, standard of care.
The results of the one-way sensitivity analysis indicated that day-to-day utilities, especially for SOC with and without regular OCS use (increases of SEK 199,354 [€18,545] and SEK 57,703 [€5,367], respectively), are the parameters with the greatest impact on the incremental cost-effectiveness ratio (). The day-to-day utilities for benralizumab responders with and without regular OCS use had a smaller impact on the incremental cost-effectiveness ratio (increase of SEK 41,846 [€3,893] and SEK 70,719 [€6,578], respectively). The proportion of benralizumab-treated patients who stopped OCS use completely was also one of the top five most impactful parameters. When this proportion decreased by 10%, the incremental cost-effectiveness ratio increased by SEK 51,075 (€4,751). When mean weekly work-hour loss was varied for benralizumab and SOC plus OCS, the incremental cost-effectiveness ratio increased by SEK 39,583 (€3,682) and SEK 49,495 (€4,604), respectively.
Discussion
Benralizumab is the first IL-5 biologic to demonstrate cost effectiveness for severe asthma. Interim cost-effectiveness analyses for benralizumab in different populations are available on Web sites of the UK NICECitation41 and the Institute for Clinical and Economic ReviewCitation26. However, this is the first publication demonstrating the cost effectiveness in patients with OCS-dependent severe asthma and blood eosinophil counts ≥150 cells/µL. Cost-effectiveness analysis results for benralizumab vs. SOC plus OCS demonstrated that for each QALY gained, the incremental cost-effectiveness ratio is SEK 366,855 (€34,127). Interventions that cost less than the annual gross domestic product per capita per DALY can be considered very cost-effective. When this approach is applied to a cost-per-QALY threshold for Sweden, the threshold would be SEK 514,000 (€47,817) per QALY gained, indicating benralizumab has a high probability (86%) of being cost-effective compared with SOC plus OCS for a selected subgroup of patients with severe, eosinophilic asthma receiving regular OCS treatment. The high probability of benralizumab’s being cost-effective was found to be a robust result when we examined a range of alternative WTP values between SEK 429,972 (€40,000) and SEK 752,452 (€70,000) per QALY gain.
The results of the one-way and probabilistic sensitivity analyses support the high probability of cost effectiveness for benralizumab and the robustness of the model results. The most important parameters in the one-way sensitivity analysis included day-to-day utilities for benralizumab and for SOC plus OCS, as well as the proportion of patients who were able to eliminate OCS treatment completely. This highlights the important role treatment decisions play in overall costs for patients with severe asthma.
This analysis defined severe asthma by OCS usage, rather than by exacerbation frequency and severity or eosinophil count. In clinical trials, OCS bursts define severe exacerbationCitation15–17,Citation30. In Swedish clinical practice, OCS use is a clear and measurable way to assess exacerbations. For patients with the most severe asthma, OCS can also be used as regular asthma treatment. Because OCS treatment is associated with adverse events and chronic comorbidities, reduction of OCS use is an important clinical goal in the treatment of asthma. This study defined patients with severe asthma as those receiving OCS ≥5 mg/day for the previous 12 months. This measure can be used by health care professionals in assessing the treatment needs of their patients. All patients with asthma may benefit from avoiding triggers and improving inhaler technique and adherence, possibly through use of recently introduced smart inhalersCitation42,Citation43.
Health care systems and treatment approaches for severe asthma may vary from country to country, but there are enough similarities to suggest that these cost-effectiveness results have implications beyond Sweden. Sweden and the UK, among other countries, use the Beveridge model of health careCitation44, and thus have similarities in how costs are paid and how services are delivered. Similar frequencies of regular OCS use for patients with severe asthma have been reported across countriesCitation6‒Citation11, suggesting that the burden of OCS-related adverse events and chronic comorbidities may also be similar.
Systematic reviews of the cost effectiveness of biologics for the treatment of asthma demonstrated that time horizon and drug price are among the key drivers of the incremental cost-effectiveness ratioCitation45,Citation46. Differences in drug prices between countries strongly impact cost effectiveness. For instance, mepolizumab, a humanized anti–IL-5 monoclonal antibody, was reported to be cost-effective for treatment of severe, uncontrolled eosinophilic asthma in the UKCitation22 but was found to be not cost-effective for similar patients in the United States at commonly cited thresholds for WTPCitation25.
Cost-effectiveness analyses of biologics focus on the defined subpopulations of patients with severe disease for whom these treatments are most clinically effectiveCitation45,Citation46. The incremental cost-effectiveness ratio from our analysis of benralizumab of SEK 366,855 (€34,127) is comparable to values reported for use of mepolizumab and reslizumab in the UK, although those values required substantial discounts in UK pricingCitation22–24. When US pricing was used, benralizumab, mepolizumab and reslizumab were all found to be cost-effective only when prices were significantly reducedCitation26.
Strengths of this study included the use of patient data from the ZONDA trial, in which OCS reduction was the primary endpoint. Clinical response to benralizumab has been demonstrated to be strongest for patients with severe, uncontrolled eosinophilic asthmaCitation15‒Citation17. Patients enrolled in the ZONDA trial, which provided the key data for this studyCitation17, were representative of benralizumab-treated patients. The model used a robust approach for capturing adverse effects of regular OCS use. The assumptions of this model were conservative and may have underestimated the cost-effectiveness of benralizumab. The inclusion of an assessment step at 16 weeks, which assumed patients who were unable to reduce OCS use during benralizumab treatment returned to treatment with SOC plus OCS, was also a key strength. Health care professionals might also find it useful to assess a patient’s response to benralizumab after 16 weeks and continue benralizumab treatment only for responding patients.
The use of OPRI data as a proxy of the Swedish health care system may be a limitation of these analyses because these data are from the UK health care system. However, the UK and Swedish systems have similar modes of service delivery and financing. Further limitations of this study were that data from different clinical trials were combined, and mortality and transition estimates were not included in the one-way sensitivity analysis.
Conclusions
Per WHO guidelinesCitation38,Citation39, interventions that cost less than the national annual GDP per capita per DALY can be considered very cost-effective. When this approach is applied to a cost-per-QALY threshold for Sweden, the threshold would be SEK 514,000 (€47,815) per QALY gained, indicating that benralizumab has a high probability of being cost-effective compared with SOC plus OCS for a selected subgroup of patients with severe, eosinophilic asthma receiving regular OCS treatment. This cost-effectiveness study will support clinicians, payers and patients in their decision-making on the treatment options available for severe eosinophilic asthma with OCS dependency.
Transparency
Declaration of funding
This study was funded by AstraZeneca.
Declaration of financial/other interests
MA and SG are employees of AstraZeneca. TK was an employee of AstraZeneca at the time these analyses were conducted. He is now an employee of Shire. CJ has received honoraria for lectures from AstraZeneca, TEVA and Novartis. AS is an employee of Covance working under contract for AstraZeneca.
JME peer reviewers on this manuscript have received an honorarium from JME for their review work, but have no other relevant financial relationships to disclose.
Author contribution
All authors are accountable for and contributed to study conception, design, analysis and interpretation of data. All authors were involved in the drafting and revision of the paper and approved the final manuscript.
06_Swedish_CEA_ms_supplemental_material_FINAL.docx
Download MS Word (136.5 KB)Acknowledgements
Editorial support was provided by Jennie G. Jacobson, PhD, CMPP, of JK Associates, Inc., and Michael A. Nissen, ELS, of AstraZeneca. This support was funded by AstraZeneca. Some of the data in this paper were part of a submission to the Swedish Dental and Pharmaceutical Benefits Agency (TLV), which is publicly available.
Note
Notes
i Redmond, WA, USA.
References
- Melero Moreno C, Quirce S, Huerta A, et al. Economic impact of severe asthma in Spain: multicentre observational longitudinal study. J Asthma. 2019;56:861–871.
- Jansson S-A, Backman H, Andersson M, et al. Societal costs of severe asthma in Sweden. Eur Respir J. 2018;52:PA1157.
- Janson C, Lisspers K, Stallberg B, et al. Health care resource utilization and cost for asthma patients regularly treated with oral corticosteroids - a Swedish observational cohort study (PACEHR). Respir Res. 2018;19:168.
- Lisspers K, Janson C, Larsson K, et al. Comorbidity, disease burden and mortality across age groups in a Swedish primary care asthma population: An epidemiological register study (PACEHR). Respir Med. 2018;136:15–20.
- Souliotis K, Kousoulakou H, Hillas G, et al. Direct and indirect costs of asthma management in Greece: an expert panel approach. Front Public Health. 2017;5:67.
- The ENFUMOSA cross-sectional European multicentre study of the clinical phenotype of chronic severe asthma. European Network for Understanding Mechanisms of Severe Asthma. Eur Respir J. 2003;22:470–477.
- Nwaru B, Ekström M, Wiklund F, et al. Oral corticosteroids exposure in a Swedish nationwide asthma population during 2006–2016. European Respiratory Society; 2018 [cited 2018 Nov 27] Available from: https://www.ers-education.org/events/international-congress/paris-2018.aspx?idParent=213239
- Van Ganse E, Antonicelli L, Zhang Q, et al. Asthma-related resource use and cost by GINA classification of severity in three European countries. Respir Med. 2006;100:140–147.
- Antonicelli L, Bucca C, Neri M, et al. Asthma severity and medical resource utilisation. Eur Respir J. 2004;23:723–729.
- Moore WC, Bleecker ER, Curran-Everett D, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. J Allergy Clin Immunol. 2007;119:405–413.
- Heaney LG, Brightling CE, Menzies-Gow A, et al.; on behalf of the British Thoracic Society Difficult Asthma Network. Refractory asthma in the UK: cross-sectional findings from a UK multicentre registry. Thorax. 2010;65:787–794.
- Price DB, Trudo F, Voorham J, et al. Adverse outcomes from initiation of systemic corticosteroids for asthma: long-term observational study. JAA. 2018;11:193–204.
- Zazzali JL, Broder MS, Omachi TA, et al. Risk of corticosteroid-related adverse events in asthma patients with high oral corticosteroid use. Allergy Asthma Proc. 2015;36:268–274.
- Bloechliger M, Reinau D, Spoendlin J, et al. Adverse events profile of oral corticosteroids among asthma patients in the UK: cohort study with a nested case-control analysis. Respir Res. 2018;19:75.
- Bleecker ER, FitzGerald JM, Chanez P, et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting beta2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet. 2016;388:2115–2127.
- FitzGerald JM, Bleecker ER, Nair P, et al. Benralizumab, an anti-interleukin-5 receptor alpha monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388:2128–2141.
- Nair P, Wenzel S, Rabe KF, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376:2448–2458.
- Global Initiative for Asthma. Global strategy for asthma management and prevention. Global Initiative for Asthma; 2018 [cited 2018 Oct 31] Available from: https://ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention/
- Pham TH, Damera G, Newbold P, et al. Reductions in eosinophil biomarkers by benralizumab in patients with asthma. Respir Med. 2016;111:21–29.
- Kolbeck R, Kozhich A, Koike M, et al. MEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity function. J Allergy Clin Immunol. 2010;125:1344–1353.
- National Institute for Health and Care Excellence. Mepolizumab for treating severe refractory eosinophilic asthma. Technology appraisal guidance [TA431]. National Institute for Health and Care Excellence; 2017 Jan 25 [cited 2019 Apr 11]. Available from: https://www.nice.org.uk/guidance/ta431
- Bermejo I, Stevenson M, Cooper K, et al. Mepolizumab for treating severe eosinophilic asthma: an evidence review group perspective of a NICE single technology appraisal. Pharmacoeconomics. 2018;36:131–144.
- National Institute for Health and Care Excellence. Reslizumab for treating severe eosinophilic asthma. Technology appraisal guidance [TA479]. National Institute for Health and Care Excellence; 2017 Oct 4; [cited 2019 Apr 11]. Available from: https://www.nice.org.uk/guidance/ta479
- Cooper K, Frampton G, Harris P, et al. Reslizumab for treating asthma with elevated blood eosinophils inadequately controlled by inhaled corticosteroids: an evidence review group perspective of a NICE single technology appraisal. Pharmacoeconomics. 2018;36:545–553.
- Whittington MD, McQueen RB, Ollendorf DA, et al. Assessing the value of mepolizumab for severe eosinophilic asthma: a cost-effectiveness analysis. Ann Allergy Asthma Immunol. 2017;118:220–225.
- Institute for Clinical and Economic Review. Biologic therapies for treatment of asthma associated with type 2 inflammation: effectiveness, value, and value-based price benchmarks. Institute for Clinical and Economic Review; 2018 Dec 20 [cited 11 Apr 2019]. Available from: https://icer-review.org/wp-content/uploads/2018/04/ICER_Asthma_Final_Report_122018-1.pdf
- Tice JA, Campbell JD, Synnott PG, et al. The effectiveness and value of biologic therapies for the treatment of uncontrolled asthma. JMCP. 2019;25:510–514.
- Tsuchiya A, Brazier J, Mccoll E, et al. Deriving preference-based single indices from non-preference based condition-specific instruments: converting AQLQ into EQ5D indices. White Rose University Consortium; 2002 May [cited 2018 Nov 19]. Available from: http://eprints.whiterose.ac.uk/10952/1/HEDS_DP_02-01.pdf
- Caminati M, Senna G, Stefanizzi G, et al.; on behalf of North East Omalizumab Network study group. Drop-out rate among patients treated with omalizumab for severe asthma: literature review and real-life experience. BMC Pulm Med. 2016;16:128.
- Fuhlbrigge A, Peden D, Apter AJ, et al. Asthma outcomes: exacerbations. J Allergy Clin Immunol. 2012;129:S34–S48.
- European Central Bank. Swedish krona (SEK). Frankfurt: Euopean Central Bank; 2017 [cited 2018 Nov 20]. Available from: https://www.ecb.europa.eu/stats/policy_and_exchange_rates/euro_reference_exchange_rates/html/eurofxref-graph-sek.en.html
- Voorham J, Xu X, Price D, et al. Health care resource utilization and costs associated with incremental systemic corticosteroid exposure in asthma. Allergy. 2019;74:273–283.
- Lloyd A, Price D, Brown R. The impact of asthma exacerbations on health-related quality of life in moderate to severe asthma patients in the UK. Prim Care Respir J. 2007;16:22–27.
- Sullivan PW, Slejko JF, Sculpher MJ, et al. Catalogue of EQ-5D scores for the United Kingdom. Med Decis Making. 2011;31:800–804.
- Lundgren S, Lundquist L. Ändring i Tandvårds- och läkemedelsförmånsverkets allmänna råd (TLVAR 2003:2) om ekonomiska utvärderingar [Change in the General Council of the Dental and Medicines Benefit Agency (TLVAR 2003: 2) on financial evaluations]. Stockholm: Tandvårds och läkemedelsförmånsverkets; 2017 [cited 2018 Nov 27]. Swedish. Available from: https://www.tlv.se/download/18.467926b615d084471ac3230c/1510316374332/TLVAR_2017_1.pdf
- Statistics Sweden [internet]. Stockholm: Statistics Sweden; 2019 [cited 2019 Apr 3]. Available from: https://www.scb.se/en/
- Strong M, Oakley JE, Chilcott J. Managing structural uncertainty in health economic decision models: a discrepancy approach. J Royal Stat Soc. 2012;61:25–45.
- World Health Organization. Cost effectiveness and strategic planning (WHO-CHOICE). World Health Organization; 2019 [cited 2019 Jun 25]. Available from: http://www.who.int/choice/en/
- Marseille E, Larson B, Kazi DS, et al. Thresholds for the cost–effectiveness of interventions: alternative approaches. Bull World Health Organ. 2015;93:118–124.
- Svensson M, Nilsson FOL, Arnberg K. Reimbursement decisions for pharmaceuticals in Sweden: the impact of disease severity and cost effectiveness. Pharmacoeconomics. 2015;33:1229–1236.
- National Institute for Health and Care Excellence. Benralizumab for treating severe eosinophilic asthma. National Institute for Health and Care Excellence; 2018 Jul [cited 2018 Nov 27]. Available from: https://www.nice.org.uk/guidance/gid-ta10192/documents/appraisal-consultation-document-2
- Mokoka MC, Lombard L, MacHale EM, et al. In patients with severe uncontrolled asthma, does knowledge of adherence and inhaler technique using electronic monitoring improve clinical decision making? A protocol for a randomised controlled clinical trial. BMJ Open. 2017;7:e015367.
- Sulaiman I, Greene G, MacHale E, et al. A randomised clinical trial of feedback on inhaler adherence and technique in patients with severe uncontrolled asthma. Eur Respir J. 2018;51:1701126.
- Bevan G, Helderman J-K, Wilsford D. Changing choices in health care: implications for equity, efficiency and cost. HEPL. 2010;5:251–267.
- Rodriguez-Martinez CE, Sossa-Briceño MP, Castro-Rodriguez JA. Cost effectiveness of pharmacological treatments for asthma: a systematic review. Pharmacoeconomics. 2018;36:1165–1200.
- McQueen RB, Sheehan DN, Whittington MD, et al. Cost-effectiveness of biological asthma treatments: a systematic review and recommendations for future economic evaluations. Pharmacoeconomics. 2018;36:957–971.