Abstract
Aim
To evaluate direct medical costs incurred by patients with diabetes in the periods before and after experiencing a microvascular complication from a Brazilian public healthcare system perspective.
Materials and methods
This was a retrospective, observational study using the Brazilian Unified Health System (DATASUS) database. Direct medical costs (hospitalization and outpatient) were extracted for patients with evidence of diabetes and a microvascular complication (January 2012–December 2018) and converted to 2019 US Dollars (USD). Length of hospital stays was also extracted. Mixed-effects logistic regression explored associations between demographic/clinical characteristics and incurrence of high direct medical costs (defined as the highest tertile of the annual costs ranked by median cost in the total population).
Results
In total, 2,096 patients with diabetes experienced a microvascular complication and met study inclusion/exclusion criteria. Median [interquartile range] annual costs (USD/patient) were 176.3 [91.0; 481.2] at baseline, increasing to 1,678.5 [287.0; 6,908.4] and 5,172.4 [274.8; 7,395.9] in the first and second year after the complication, respectively. Median hospital stay was 2.0 and 3.0 days at baseline and in the first year, respectively. The odds of incurring high costs were substantially elevated in the first and second years (odds ratios of 69.9 and 84.7, respectively, vs. baseline, both p < .001).
Limitations
The DATASUS database covers secondary and tertiary care (not primary), adding selection bias to our sample. Additionally, our findings may not apply to the entire Brazilian population, as around 25% have some access to private healthcare.
Conclusions
This study demonstrates a large increase in costs, from the perspective of the Brazilian public healthcare system, in patients with diabetes after experiencing a microvascular complication compared with pre-complication costs. In addition to providing up-to-date cost estimates, our findings highlight the need to appraise the cost-effectiveness of evidence-based strategies that reduce the risk of diabetes-related microvascular complications in Brazilian patients.
Introduction
The global prevalence of diabetes has steadily increased over recent decades to an estimated 463 million people in 2019 and is predicted to reach 700 million by 2045Citation1,Citation2. It is now considered one of the most prevalent and costly non-communicable diseases worldwide, imposing a substantial societal burden due to high medical costs, lost productivity, impaired quality of life, and premature deathCitation3–6. Low- and middle-income countries are disproportionally impacted by diabetes. It is estimated that four of every five individuals with diabetes currently live in a low- or middle-income country, and the prevalence of diabetes is increasing fastest in such countriesCitation1,Citation7. Brazil is a large, upper-middle-income country and was ranked fifth globally in 2019 for the number of people with diabetesCitation1. Around 16.8 million people were living with diabetes in Brazil in 2019, equivalent to an age-adjusted prevalence of 10.4% among those aged between 20 and 79 yearsCitation1. In terms of its economic burden, Brazil has the third most expensive diabetes-related healthcare bill globally, estimated to be 52.3 billion United States dollars (USD) in 2019Citation1.
Diabetes is associated with debilitating, long-term complications that account for a high proportion of medical costs and health burdenCitation5,Citation8. For example, in the United Kingdom, the treatment and management of diabetes-related complications account for 78.9% of disease-specific direct medical costsCitation9. Both macrovascular (including chronic heart disease, peripheral artery disease, and stroke) and microvascular (including nephropathy, neuropathy, and retinopathy) complications of diabetes are common and associated with significant morbidity, mortality, and healthcare costsCitation8,Citation10–12. Cardiovascular (CV) disease remains the largest cause of disability and mortality among patients with diabetesCitation13. Microvascular complications account for significant morbidity and considerably impair quality of lifeCitation10.
Evidence-based diabetes treatment guidelines now address the co-management of type 2 diabetes and microvascular complicationsCitation14,Citation15. There is robust evidence that appropriate glycemic control can reduce or delay the appearance of microvascular complications, thereby decreasing the clinical burden and associated costsCitation14,Citation16. Additionally, in patients with type 2 diabetes and chronic kidney disease (CKD), guidelines advise the use of a sodium–glucose cotransporter-2 inhibitor or glucagon-like peptide-1 receptor agonist, as these have been shown to reduce the risk of CKD progression, CV events, or bothCitation14.
To help policymakers and healthcare payers understand the financial implications of evidence-based interventions that reduce the risk of microvascular complications in patients with diabetes, we require a better understanding of the economic burden of both diabetes and microvascular complications, as well as up-to-date estimates of healthcare resource utilization (HRU) and medical costs.
The primary aim of this retrospective, observational, database study was to evaluate direct medical costs in patients with diabetes in the time periods before and after experiencing a microvascular complication, from the perspective of the Brazilian public healthcare system. A secondary aim was to explore associations between demographic or clinical characteristics and the incurrence of high direct medical costs in patients with diabetes who experienced a microvascular complication.
Methods
Detailed descriptions of the methodology and data sources utilized in this study have previously been published for an investigation of direct medical costs associated with macrovascular complications in Brazilian patients with diabetesCitation17. Here we provide a summary of the methods used in the context of evaluating costs following a microvascular complication in Brazilian patients with diabetes.
Data source
The public health Brazilian Unified Health System (Sistema Único de Saúde [SUS]) is a free-to-patient service administered through a network of healthcare units, hospitals, laboratories, and blood banks, who are responsible for collecting, processing, and disseminating health informationCitation18,Citation19. Data collected by the SUS are stored in its database DATASUSCitation20, which comprises separate epidemiological, clinical, and administrative databasesCitation18. Additionally, all admissions to public hospitals are recorded in a National Hospital Information System (Sistema de Informações Hospitalares [SIH]), providing data on hospital admissions, discharges, and costsCitation18. The Ambulatory Information System (Sistema de Informações Ambulatoriais [SIA]) stores data for public outpatient care covering emergency care, healthcare visits, and some high-complexity procedures (e.g. oncology). However, medical examinations and primary care data, including those related to medication use, are not publicly available in the databaseCitation18. Anonymized data are freely available on the DATASUS websiteCitation20. Per the Brazilian ethical resolution number 510, ethical approval for this cost study was not requiredCitation21.
Data collection
In the present study, we extracted data for eligible patients from the SUS-SIH and SUS-SIA databases between 1 January 2012 and 31 December 2018. The data extracted included administrative information (gender, age, region, hospital admission, and discharge date, healthcare unit, procedure, record date, and cost to the SUS) and medical information (diagnosis code[s]). Records for each individual were combined across these databases via record-linking methodologyCitation22.
Study population
Eligible patients had at least one record of diabetes (i.e. an International Classification of Diseases, 10th Revision [ICD-10] diagnosis code for diabetes, ) and at least one microvascular complication (per ICD-10 diagnosis codes, ) after the first record of diabetes during the study period. It should be noted that the translation of ICD-10 diagnosis codes in Brazil categorizes diabetes as insulin-dependent and non-insulin-dependent, distinct from and not interchangeable with type 1 and type 2 diabetes. Exclusion criteria included evidence of a record for cancer (per ICD-10 diagnosis codes for chemotherapy or radiotherapy); inconsistent data, which was defined as a negative age or unknown location; and an ICD-10 diagnosis code for a macrovascular complication during the study period (Table S1).
Table 1. ICD-10 diagnosis codes and frequency in patients with diabetes who experienced a microvascular complication (N = 2,096).
Study design
This analysis was conducted from the perspective of the Brazilian public healthcare system. The direct medical costs considered were to the SUS related to outpatient management, procedures, and hospitalization.
For each patient, the month of the qualifying microvascular complication was defined as the index date. Relative to this date, five study time periods were defined: baseline −1 (12–24 months before index), baseline (0–12 months before index), first-year (0–12 months after index), second-year (12–24 months after index) and third-year (24–36 months after index). All patients were required to have a minimum of two months’ data observable in the database following the index date.
The primary objective of this study was to describe the annual direct medical costs in patients with diabetes in the time periods before and after experiencing a microvascular complication. Annual direct medical costs were also described for patients stratified by gender and survival status in the overall study period. Information was available for a patient’s death if that event took place in the hospital or if the high-complexity procedures authorization (APAC) profile was closed due to death.
A secondary study objective was to explore potential associations between demographic or clinical characteristics and the incurrence of high direct medical costs, defined as the highest tertile of the annual costs ranked by median costCitation23, in the overall study cohort. Additional analyses were conducted describing the length of hospital stay and the most frequent medical procedures and medications (based on patient numbers), defined per the SUS table of procedures, medications and orthoses, prostheses, and special materials (SIGTAP)Citation24. It should be noted that data for prescribed medications available in DATASUS are limited, and mainly include those prescribed in secondary and tertiary care.
Statistical analysis
All data were summarized descriptively, and missing data were not imputed. The costs were extracted from the source in Brazilian Real (BRL), then converted to 2019 USD using the average exchange rate of BRL 1: USD 0.252 for the third quarter of 2019 (1 July 2019–30 September 2019)Citation25. All costs reported here are in USD.
Potential associations between demographic or clinical characteristics and the incurrence of high direct medical costs were investigated using mixed-effects logistic regression analyses.
Analyses were performed in R (R Foundation for Statistical Computing, software version 3.6.1, Vienna, Austria).
Results
Study cohort
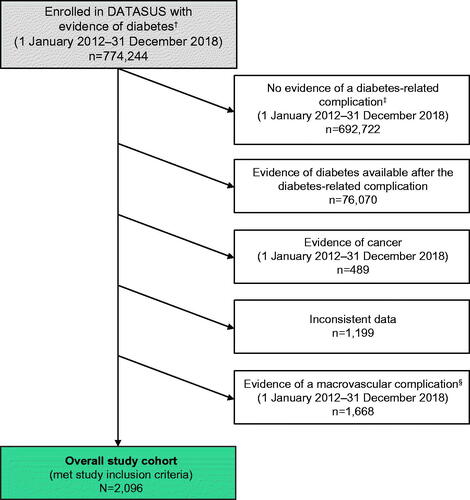
The patient flow is presented in . There were 774,244 patients with evidence of diabetes in DATASUS during the 7-year study periodCitation17. Of these patients, 692,722 patients did not have evidence of a diabetes-related complication during the study period and were excluded from the study. After applying further exclusion criteria, there were 2,096 patients with diabetes who experienced 2,270 qualifying microvascular complications during the study period and were included in the overall study cohort. In total, 1,937 patients (92.4% of the study cohort), 145 (6.9%), 13 (0.6%), and 1 (0.0%) experienced 1, 2, 3, and 4 qualifying microvascular complications for study entry, respectively. The majority of the patients (n = 1,234; 58.9% of the study cohort) were categorized as having an unspecified diabetes type (). Insulin-dependent diabetes was the second most recorded (n = 632; 30.2%), followed by non-insulin-dependent diabetes (n = 230; 11.0%). Kidney disease accounted for most of the qualifying microvascular complications (n = 1,667; 73.4% of complications). Diabetic foot and eye disease were the next most common microvascular complications in the overall study cohort (n = 191; 8.4%, and n = 117; 5.2%, respectively). Events classified as “other” accounted for 267 (11.8%) of qualifying microvascular complications ().
Figure 1. Patient flow diagram. The overall study cohort included patients enrolled in DATASUS with evidence of diabetes and a microvascular complication during the study period who did not meet any exclusion criteria. †Defined as ≥1 record with an accepted ICD-10 diagnosis code for diabetes (); ‡defined as ≥1 record with an accepted ICD-10 diagnosis code for a microvascular () or macrovascular (Table S1) complication; §defined as ≥1 record with an accepted ICD-10 diagnosis code for a macrovascular complication (Table S1). Abbreviations. DATASUS, Ministry of Health’s Information Technology Department; ICD-10, International Classification of Diseases, 10th Revision.
Overall, the study cohort was 48.0% (1,006/2,096) female and the mean (standard deviation) duration of diabetes (time since the first evidence of diabetes during the study period and the qualifying microvascular complication) was 690 (595) days. More than half of the patients (n = 1,216; 58.0%) were from the southeastern region of Brazil (northeast: n = 366, 17.5%; south: n = 340, 16.3%; midwest: n = 129, 6.2%; north: n = 45, 2.1%). The median [interquartile range; IQR] age at the index date was 57.9 [49.5, 66.0] years. Median age ranged from 60.0 years for patients who experienced eye disease up to 69.0 years for those with diabetic foot (; groups not statistically compared). In total, 815 (38.9%) patients died during the overall study period.
Table 2. Age distribution of patients with diabetes who experienced a microvascular complication (N = 2,096).
Direct medical costs
Median [IQR] annual direct medical costs in USD/patient were 176.3 [91.0; 481.2] at baseline, increasing to 1,678.5 [287.0; 6,908.4] in the first year after a microvascular complication (; time periods not statistically compared). Median direct medical costs in USD/patient peaked in the second year (5,172.4 [274.8; 7,395.9]) and remained elevated above baseline in the third year (2,525.4 [167.0; 7,311.5]) after experiencing a microvascular complication. The general trends in direct medical costs were consistent in patients stratified by gender (; groups not statistically compared) or survival status during the overall study period (Table S2; groups not statistically compared). However, the increase in direct medical costs from baseline to the first year after a microvascular complication was more pronounced in patients who died during the study period than in those who survived, before reaching greater alignment in the second and third years (Table S2).
Table 3. Direct medical costs in patients with diabetes who experienced a microvascular complication, overall and stratified by gender.
When costs were stratified by cost category, costs were more evenly distributed between most categories at baseline than in the first year after a microvascular complication (Table S3; categories not statistically compared). At baseline, median costs (USD/patient) were in rank order as follows: clinical (166.3), transplants (156.4), surgical (151.2), orthoses (105.6), other (20.7), diagnostic (14.4), and medications (0.0). In the first year, the rank order of categories by median costs remained unchanged; however, median clinical costs increased by 2,129% to 3,707.6 USD/patient accounting for the vast majority of costs in the first year.
presents the results of exploratory mixed-effects logistic regression analyses assessing potential associations between demographic or clinical characteristics and the odds of incurring high direct medical costs. Time period, age, and region were all significantly associated with the incurrence of high direct medical costs. In comparison with baseline, odds ratios (ORs) [95% CI] for high direct medical costs were 69.92 [45.01; 108.61] in the first year and 84.68 [55.66; 128.82] in the second year (both p < .001). Likewise, as compared with patients aged over 80 years, those aged <40 years (OR 4.77 [95% CI: 2.21; 10.31]) or 40–<60 years (OR 2.93 [95% CI: 1.55; 5.52]) were more likely to incur high direct medical costs (both p < .001). There were also regional differences with greater odds of incurring high direct medical costs observed among residents of the midwestern (p = .007), north-eastern (p < .001), and southern (p < .001) regions compared with those from the south-eastern region.
Figure 2. Associations between demographic and clinical characteristics with the incurrence of high direct medical costs in patients with diabetes who experienced a microvascular complication (N = 2,096). Data are odds ratio [95% CI] for associations between parameters and high direct medical costs (defined as the highest tertile of annual cost data ranked by median cost for patients in the overall study cohort) from binary logistic regression modeling. Square brackets in the first column indicate the reference category. Baseline corresponds to the year before the qualifying complication, while first and second year refers to the respective year after the qualifying complication. Abbreviation. CI, confidence interval.
![Figure 2. Associations between demographic and clinical characteristics with the incurrence of high direct medical costs in patients with diabetes who experienced a microvascular complication (N = 2,096). Data are odds ratio [95% CI] for associations between parameters and high direct medical costs (defined as the highest tertile of annual cost data ranked by median cost for patients in the overall study cohort) from binary logistic regression modeling. Square brackets in the first column indicate the reference category. Baseline corresponds to the year before the qualifying complication, while first and second year refers to the respective year after the qualifying complication. Abbreviation. CI, confidence interval.](/cms/asset/a6a04645-a222-4c12-bed0-2061ef56b59c/ijme_a_1963572_f0002_c.jpg)
Length of hospital stay
Median hospital stays were 2 days at baseline, increasing to 3 days in the first year, before decreasing to 0 days in the second and third years after experiencing a microvascular complication (; time periods not statistically compared). Patient stays were of a broadly similar length by time period when data were stratified by gender (; groups not statistically compared).
Table 4. Length of hospital stay in patients who experienced a microvascular complication, overall and stratified by gender.
Medical procedures and medications
The three most frequent procedures (median total annual cost across all patients with the stated procedure in USD) for patients experiencing a microvascular complication were hemodialysis (n = 1,203; 2,043,407.2), treatment of diabetes (n = 1,595; 83,914.2), and confection of arterial fistula for hemodialysis (n = 699; 16,711.6) (). This was generally consistent across female and male patients (Table S4; groups not statistically compared). When the most frequent procedures were stratified by time period, hemodialysis procedures took place in 310 patients at baseline, rising to 1,111 patients in the first year after the complication; this was mirrored by the median hemodialysis cost per patient, which rose from 1,200.7 to 6,013.7 USD/year over the same time period (Table S5; time periods not statistically compared). When the most frequent procedures were stratified by both the time period and the qualifying microvascular complication, the procedures tended to align with those that are associated with the complication (Table S6). For instance, those associated with kidney complications were frequently observed in patients who experienced kidney disease, and those associated with eye examinations were common in patients with eye disease and diabetic retinopathy.
Table 5. Direct medical costs for the ten most frequent medical procedures and medications for patients with diabetes who experienced a microvascular complication (N = 2,096).
The medications prescribed in mostly secondary and tertiary care settings accounted for a relatively small share of annual direct medical costs across the study period (Table S3). The most commonly utilized medications were ferric hydroxide saccharate and high-dose epoetin alfa (4,000 IU), both used in the management of anemia in patients with CKD, and which added modest direct medical costs (). The patterns of medication use were broadly similar among men and women (Table S7; groups not statistically compared). Medications were rarely used at baseline, with the most frequent (atorvastatin 10 mg) prescribed to eight patients (Table S8). Medication use dramatically increased in the first year after experiencing a microvascular complication, remaining elevated above baseline levels in the second and third years, while accounting for modest per-patient costs.
Discussion
This retrospective database study, from the perspective of the Brazilian public healthcare system, has demonstrated a large increase in direct medical costs in patients with diabetes after experiencing a microvascular complication. The costs were highest in the second year after experiencing a microvascular complication and remained elevated above baseline over three years (after which the study period ended).
Exploratory analyses suggested that the incurrence of high direct medical costs was strongly associated with the time period, with much higher odds in the first (OR 70) and second (OR 85) year after experiencing a microvascular complication, in comparison with baseline. There were some smaller regional differences in the odds of incurring high medical costs, as well as significant differences between some of the younger age groups when compared with the oldest patients. The geographical factors associated with an increased likelihood of high direct medical costs () may be partly explained by regional differences in access to tertiary care and diabetologists, as well as by the movement of patients between regions to access treatment.
These findings are in line with and add to our previous demonstration of increased direct medical costs associated with macrovascular complications in Brazilian patients with diabetesCitation17. Moreover, it should be noted that the odds of patients incurring high direct medical costs in the first and second year after the complication (vs. baseline) were substantially greater for microvascular complications (ORs of 70–85; USD/patient of 1,679 [first year] and 5,172 [second year]) here than for macrovascular complications with or without a microvascular complication (ORs of 3–6; USD/patient of 334 [first year] and 266 [second year]) in our previous studyCitation17. One potential explanation for this difference is the substantial rise in costs as nephropathy progressesCitation26; the management of patients with end-stage kidney disease consumes considerable healthcare resources, requiring long-term dialysis or kidney transplantationCitation27. Kidney disease was by far the most common qualifying microvascular complication in our study and a sizable proportion of this cohort received hemodialysis in the first and second years after experiencing the complication. This is perhaps not surprising, as DATASUS does not cover primary care, only secondary and tertiary care.
The observation of higher costs associated with microvascular vs. macrovascular complications is in agreement with findings from a cohort of patients with type 2 diabetes in ChinaCitation28, but the contrast with those from studies of type 2 diabetes in BrazilCitation29 and EuropeCitation30, where macrovascular complications were associated with the higher costs. The reasons for these contrasting findings are not entirely clear, but likely reflect important differences in the analysis and estimation of costs and between the patient populations studied.
Our results add to the growing evidence of the substantial economic burden on healthcare systems worldwide due to diabetes-related complicationsCitation8,Citation9,Citation12,Citation17,Citation31,Citation32. The high cost of managing diabetes represents a growing challenge for healthcare systems. For example, Bahia et al. estimated the total economic burden of diabetes in Brazil to be 15.7 billion international dollars from a societal perspective in 2014, i.e. 0.5% of Brazilian gross domestic productCitation31. In 2019, the International Diabetes Federation estimated that nearly 1 in every 4 BRL (24.2%) of total healthcare expenditure was attributed to diabetesCitation1.
The ongoing COVID-19 pandemic may further increase the economic burden due to diabetes and its complications. There is a widely recognized association between diabetes and the severity of COVID-19 symptoms, including the risks of admission to intensive care and mortalityCitation33–35. Therefore, the current pandemic is likely to increase diabetes-related direct medical costs, exacerbating the burden on healthcare systems. The results presented here add further evidence, specifically in a Brazilian public healthcare setting, that microvascular complications substantially contribute to direct medical costs in patients with diabetes. Accordingly, our findings provide support for the need to appraise and implement evidence-based and cost-effective strategies that help to reduce the burden of diabetes-related microvascular complications. Such strategies may include those for optimizing lifestyle managementCitation36, addressing the non-uniformity of access to and availability of essential medicines within the SUSCitation37,Citation38, for example through programs, such as the Pharmacy Network of Minas (Rede Farmácia de Minas [RFM])Citation39, and strategies to improve sub-optimal treatment adherence among patients with diabetesCitation40.
Our study has some limitations that should be highlighted. Originally, the SUS-SIH and SUS-SIA were created for administrative purposes, meaning the data source has limited clinical information and may be prone to errors. Furthermore, the DATASUS database does not cover primary care, only secondary and tertiary care. Therefore, there is a risk of selection bias in the data sample, as most patients with diabetes in Brazil will be seen in primary care and those patients with complications are likely to be transferred to secondary and/or tertiary care. It should also be noted that DATASUS is a reimbursement database, which may have an impact on the types of microvascular complications reported herein. Additionally, as with other retrospective database studies, our results are reliant on the completeness of the records, which in our case may not contain all relevant or complete information. For instance, the majority of patients are classified as having “unspecified diabetes”, rather than insulin-dependent or non-insulin-dependent disease (). Accordingly, we have minimized attention on diabetes type and concentrated on analyses in patients with diabetes (any type) according to complication status, gender, and time period. Our analyses did not include assessment of costs stratified by additional incidences of microvascular complication and this is an area for further study. While we excluded from this analysis patients with a microvascular complication who also had a macrovascular complication, medical costs data for this subgroup is reported in our recent article focusing on macrovascular complications in Brazilian patients with diabetesCitation17.
It is worth noting that the translation of ICD-10 diagnosis codes for diabetes varies between Brazil and other countries (e.g. the United Kingdom and the United States), which categorize type 1 and type 2 diabetes; these distinctions (insulin dependence vs. diabetes type) are not interchangeable and we recognize this as a study limitation. A related limitation is the different use in Brazil relative to other countries of ICD-10 codes to identify microvascular complications. Also, the diagnosis coding system may not exclusively distinguish between a microvascular and macrovascular, or mixed, origin for complications, such as foot ulcers, and this is a further limitation of our work. We also acknowledge that direct medical costs in stratified patient groups may have been influenced by differences between groups in mortality rates. A final limitation is that our findings may not be representative of the entire Brazilian population given that ∼75% of the population of Brazil depend exclusively on the SUS, while the remaining 25% have some access to private healthcare, through which treatment for diabetes and its complications may, at least in part, be provided. In using data from the SUS for our analyses, we thus could not quantify the direct medical costs within the private healthcare sector, where the standards of care and costs are likely to be higher compared with the SUSCitation19.
Conclusions
The present study has demonstrated higher medical costs in patients with diabetes after experiencing a microvascular complication when compared with the costs incurred before the complication. In addition to providing up-to-date cost estimates, our results highlight the need to appraise the cost-effectiveness of evidence-based strategies to reduce the risk of microvascular complications in patients with diabetes in Brazil.
Transparency
Declaration of funding
Sponsorship for this analysis and article processing charges were funded by Novo Nordisk A/S.
Declaration of financial/other interests
At the time of the study, GSJ and DC were full-time employees of IQVIA Brasil, which received consultancy fees from Novo Nordisk A/S to conduct the analyses. GSJ remains a full-time employee of IQVIA Brasil, while DC has left the company. LMAP and RCLAC are employees of Novo Nordisk Farmacêutica Do Brasil Ltda. NM and JBH are employees of Novo Nordisk A/S. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
GSJ is the guarantor of this work and, as such, had full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors confirm that they meet the International Committee of Medical Journal Editors (ICJME) uniform requirements for authorship and that they have contributed to the CRediT roles detailed below. GSJ: data curation; formal analysis; methodology; validation; visualization; writing – review and editing. RCLAC: writing – review and editing. NM: conceptualization; methodology; supervision; writing – review and editing. JBH: methodology; writing – review and editing. LMAP: writing – review and editing. DC: data curation; formal analysis; methodology; validation; visualization; writing – review and editing. All authors and share in the final responsibility for the content of the manuscript, as well as the decision to submit it for publication.
Geolocation information
Brazil.
Supplemental Material
Download PDF (591.2 KB)Acknowledgements
The authors would like to thank the participants of the study and acknowledge the input of Flávia Sauer Tobaruella to early discussions. The medical writing support was provided by David Floyd on behalf of, and editorial assistance was provided by Beverly La Ferla of, Ashfield MedComms, an Ashfield Health company, funded by Novo Nordisk A/S.
Data availability statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- International Diabetes Federation. IDF diabetes Atlas Brussels, Belgium; 2019 [cited 2021 Feb]. Available from: https://www.diabetesatlas.org
- NCD Risk Factor Collaboration. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530.
- Chen S, Kuhn M, Prettner K, et al. The macroeconomic burden of noncommunicable diseases in the United States: estimates and projections. PLOS One. 2018;13(11):e0206702.
- Hayes A, Arima H, Woodward M, et al. Changes in quality of life associated with complications of diabetes: results from the ADVANCE study. Value Health. 2016;19(1):36–41.
- American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–928.
- Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996–2013. JAMA. 2016;316(24):2627–2646.
- Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–149.
- Chapman D, Foxcroft R, Dale-Harris L, et al. Insights for care: the healthcare utilisation and cost impact of managing type 2 diabetes-associated microvascular complications. Diabetes Ther. 2019;10(2):575–585.
- Hex N, Bartlett C, Wright D, et al. Estimating the current and future costs of type 1 and type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med. 2012;29(7):855–862.
- Dal Canto E, Ceriello A, Rydén L, et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019;26(2_suppl):25–32.
- Einarson TR, Acs A, Ludwig C, et al. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):83.
- Einarson TR, Acs A, Ludwig C, et al. Economic burden of cardiovascular disease in type 2 diabetes: a systematic review. Value Health. 2018;21(7):881–890.
- Low Wang CC, Hess CN, Hiatt WR, et al. Clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus – mechanisms, management, and clinical considerations. Circulation. 2016;133(24):2459–2502.
- American Diabetes Association. 11. Microvascular complications and foot care: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S151–S167.
- Barrett EJ, Liu Z, Khamaisi M, et al. Diabetic microvascular disease: an endocrine society scientific statement. J Clin Endocrinol Metab. 2017;102(12):4343–4410.
- Lachin JM, Genuth S, Cleary P, et al. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. 2000;342(6):381–389.
- Julian GS, Campos D, Broe Honore J, et al. Cost of macrovascular complications in people with diabetes from a public healthcare perspective: a retrospective database study in Brazil. J Med Econ. 2020;23(9):985–993.
- Ali MS, Ichihara MY, Lopes LC, et al. Administrative data linkage in Brazil: potentials for health technology assessment. Front Pharmacol. 2019;10:984.
- The Commonwealth Fund. Brazil; 2020 [cited 2021 Feb]. Available from: https://www.commonwealthfund.org/international-health-policy-center/countries/brazil#:∼:text=Approximately%2075%20percent%20of%20Brazilian%20citizens%20rely%20solely%20on%20SUS
- Sistema Único de Saúde Department of Informatics. DATASUS [cited 2021 Feb]. Available from: https://datasus.saude.gov.br/
- Conselho Nacional de Saúde. Resolução No 510, de 07 de Abril de 2016; 2016 [cited 2021 Feb]. Available from: http://conselho.saude.gov.br/resolucoes/2016/reso510.pdf
- Campos DF, Rosim RP, Duva AS, et al. Brazilian healthcare record linkage (brhc-rlk) – a record linkage methodology for Brazilian medical claims datasets (DATASUS). Value Health. 2017;20:A321.
- Jacobs MS, van Leent MWJ, Tieleman RG, et al. Predictors for total hospital and cardiology cost claims among patients with atrial fibrillation initiating dabigatran or acenocoumarol in The Netherlands. J Med Econ. 2017;20(12):1231–1236.
- DataSUS. The SUS table of procedures, medications and orthoses, prostheses and special materials (OPM) (SIGTAP); 2019 [cited 2021 Feb]. Available from: http://www.sgc.goias.gov.br/upload/links/arq_961_tabelacompleta.pdf
- Banco Central do Brasil. Câmbio e Capitais internacionais; 2019 [cited 2021 Feb]. Available from: https://www.bcb.gov.br/estabilidadefinanceira/historicocotacoes
- Nichols GA, Vupputuri S, Lau H. Medical care costs associated with progression of diabetic nephropathy. Diabetes Care. 2011;34(11):2374–2378.
- Gordois A, Scuffham P, Shearer A, et al. The health care costs of diabetic nephropathy in the United States and the United Kingdom. J Diabetes Complications. 2004;18(1):18–26.
- Chen D, Liu S, Tan X, et al. Assessment of hospital length of stay and direct costs of type 2 diabetes in Hubei province, China. BMC Health Serv Res. 2017;17(1):199.
- Bahia LR, Araujo DV, Schaan BD, et al. The costs of type 2 diabetes mellitus outpatient care in the Brazilian public health system. Value Health. 2011;14(5 Suppl 1):S137–S140.
- Williams R, CODE-2 Advisory Board, Van Gaal L, Lucioni C. Assessing the impact of complications on the costs of type II diabetes. Diabetologia. 2002;45(7):S13–S17.
- Bahia LR, da Rosa MQM, Araujo DV, et al. Economic burden of diabetes in Brazil in 2014. Diabetol Metab Syndr. 2019;11:54.
- Chen HY, Kuo S, Su PF, et al. Health care costs associated with macrovascular, microvascular, and metabolic complications of type 2 diabetes across time: estimates from a population-based cohort of more than 0.8 million individuals with up to 15 years of follow-up. Diabetes Care. 2020;43(8):1732–1740.
- Abdi A, Jalilian M, Sarbarzeh PA, et al. Diabetes and COVID-19: a systematic review on the current evidences. Diabetes Res Clin Pract. 2020;166:108347.
- Pal R, Bhadada SK. COVID-19 and diabetes mellitus: an unholy interaction of two pandemics. Diabetes Metab Syndr. 2020;14(4):513–517.
- Roncon L, Zuin M, Rigatelli G, et al. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol. 2020;127:104354.
- American Diabetes Association. 4. Lifestyle management. Diabetes Care. 2017;40(Suppl 1):S33–S43.
- Nascimento R, Álvares J, Guerra AAJ, et al. Availability of essential medicines in primary health care of the Brazilian unified health system. Rev Saude Publica. 2017;51(suppl 2):10s.
- Rocha WH, Teodoro J, Assis Acurcio F, et al. Influence of pharmaceutical services organization on the availability of essential medicines in a public health system. J Comp Eff Res. 2021;10(6):519–532.
- Barbosa MM, Nascimento RC, Garcia MM, et al. Strategies to improve the availability of medicines in primary health care in Brazil: findings and implications. J Comp Eff Res. 2021;10(3):243–253.
- Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–1224.
