Abstract
Aim
This economic analysis evaluated the cost-effectiveness of nivolumab (NIVO) plus ipilimumab (IPI) plus two cycles of platinum-doublet chemotherapy (PDC) compared with four cycles of PDC as first-line treatment for patients with advanced NSCLC in the United States (US).
Methods
A partitioned survival model was constructed with three mutually exclusive health states: progression free, progressed disease, and death. The analysis was conducted from a US healthcare payer perspective, using a time horizon of 25 years. Costs and outcomes were discounted at 3% annually. Survival outcomes from CheckMate 9LA were extrapolated with longer follow-up data from CheckMate 227 Part 1 (NIVO + IPI) and validated against data from other relevant clinical trials and real-world registries. Health-related quality of life utility values were derived from EQ-5D-3L data collected in CheckMate 9LA. US-specific costs (2020 dollars) were used for disease management; drug acquisition, administration, and monitoring; end-of-life care; adverse events; and subsequent treatments. Model outcomes included life years (LYs) gained, quality-adjusted LYs (QALYs) gained, and incremental cost-effectiveness ratio (ICER) for NIVO + IPI + PDC versus PDC. Sensitivity and scenario analyses were conducted.
Results
NIVO + IPI + PDC was associated with higher projected health benefits than PDC, including gains in LYs (3.71 vs 1.89) and QALYs (2.86 vs 1.37), and higher costs ($317,581 vs $119,909). The ICER was $132,960/QALY gained. NIVO + IPI + PDC had a 78–100% probability of being cost-effective at a willingness-to-pay threshold of $150,000–$250,000/QALY. Sensitivity and scenario analyses indicated that the results were robust to changes in key parameters.
Limitations
The inherent limitation in extrapolating clinical trial data was mitigated using data from the more mature CheckMate 227 Part 1 trial and validating the outcomes against data from other relevant trials and real-world registries.
Conclusion
NIVO + IPI + PDC (two cycles) provides a new first-line treatment option for patients with advanced NSCLC that is cost-effective within a range considered acceptable in the US.
Introduction
Lung cancer is the second most commonly diagnosed cancer worldwide, accounting for 11.4% of all new cancer diagnoses according to GLOBOCAN 2020 dataCitation1. In 2021, it is estimated that 235,760 people in the United States (US) will be diagnosed with lung cancer, and 131,880 will die from itCitation2. Lung cancer is the leading cause of cancer-related death in both men and women, accounting for 18.0% of cancer-related deaths worldwide and almost 25% in the US in 2020Citation1,Citation2. Non-small cell lung cancer (NSCLC) accounts for 84% of all lung cancer cases, and prior to recent advances, patients with NSCLC generally had a poor prognosisCitation3. Among US patients diagnosed between 2008 and 2014, the 5-year survival rate for newly diagnosed NSCLC was 22.7%, and 5.5% for newly diagnosed NSCLC with distant metastasesCitation3. The introduction of immune checkpoint inhibitors (ICIs) to restore antitumor immunity, with the first approvals in advanced NSCLC in 2015, has substantially changed the landscape of treatment for NSCLC, with nivolumab in second-line treatment showing a 5-year survival rate of 13.4%, versus 2.6% for chemotherapyCitation4,Citation5.
While there has been significant progress in the treatment landscape for NSCLC, many patients still either fail to respond or will ultimately have progressive diseaseCitation6,Citation7. There remains a need for more treatment options that provide potential for durable long-term survival.
Nivolumab (NIVO) and ipilimumab (IPI) are immune checkpoint inhibitors with distinct but complementary mechanisms of action, targeting programmed cell death-1 (PD-1) and cytotoxic T-lymphocyte antigen 4, respectivelyCitation8–11. The combination of NIVO + IPI has been investigated in treatment-naive patients with NSCLC in two phase 3 studies: CheckMate 227 and CheckMate 9LA. In the CheckMate 227 trial (NCT02477826), NIVO + IPI was compared with platinum-doublet chemotherapy (PDC) in the first-line treatment of patients with advanced or recurrent NSCLC and a tumor PD-1 ligand 1 (PD-L1) expression level of either ≥1% (Part 1a) or <1% (Part 1 b)Citation12. In that study, NIVO + IPI significantly improved overall survival (OS) compared with chemotherapy alone, irrespective of tumor PD-L1 expressionCitation12. Evidence suggests that some patients may benefit from a limited course of chemotherapy in the early stages of treatment to augment the effects of immunotherapyCitation12–15. The finding that chemotherapy exerts its antitumor effects not only directly, but also indirectly via immunogenic activities that include inducing overexpression of PD-L1, led to the theory that chemotherapy may act synergistically with anti–PD-1/PD-L1 immunotherapyCitation16,Citation17. Thus, the aim of the ongoing, randomized, open-label, phase 3 CheckMate 9LA trial (NCT02477826) was to test whether two cycles of chemotherapy at the beginning of treatment would provide early disease control in adult patients with treatment-naive stage IV or recurrent NSCLCCitation18. Results indicated that NIVO + IPI with two cycles of PDC significantly improved OS, progression-free survival (PFS), and overall response rate versus PDC alone and had a favorable risk–benefit profile, supporting this combination treatment as a first-line option for patients with advanced NSCLCCitation18.
Based on the findings of CheckMate 227, NIVO + IPI is now approved in the US for the first-line treatment of adult patients with NSCLC with tumor PD-L1 expression ≥1% and no epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) genomic tumor aberrationsCitation8. The results of CheckMate 9LA have led to US approval of NIVO + IPI in combination with two cycles of PDC as a first-line treatment for adult patients with metastatic or recurrent NSCLC with no EGFR or ALK genomic tumor aberrationsCitation8,Citation18. National Comprehensive Cancer Network guidelines recommend both NIVO + IPI and NIVO + IPI + PDC for the treatment of advanced NSCLC, regardless of histology or tumor PD-L1 expression statusCitation19.
The objective of this study was to evaluate the cost-effectiveness of NIVO + IPI + PDC (two cycles) versus four cycles of PDC alone in the first-line treatment of stage IV or recurrent NSCLC, regardless of histology or PD-L1 expression, in the US from a healthcare payer perspective. The present analysis was based on the 9 March 2020 database lock of the CheckMate 9LA trial. At the time of the database lock, the minimum follow-up was 12.7 months for OS, with a median follow-up of 14.1 months for the NIVO + IPI + PDC arm and 10.7 months for the PDC alone armCitation18.
Methods
Model framework
The relative cost-effectiveness of NIVO + IPI + PDC versus PDC alone was assessed by developing a partitioned survival model that comprised three mutually exclusive health states: progression free (PF), progressed disease (PD), and death, based on the primary and secondary endpoints of the CheckMate 9LA and CheckMate 227 trialsCitation12,Citation18. OS and PFS data collected in CheckMate 9LA and CheckMate 227 were used directly to inform disease progression in the model. Health-state occupancy for PF, PD, and death was determined by calculating the area under the PFS curve, between the PFS and OS curves, and above the OS curve, respectively.
The intervention was NIVO (360 mg every 3 weeks) plus IPI (1 mg/kg every 6 weeks), plus two cycles of histology-based PDC, given until disease progression, unacceptable toxicity, or treatment completion at 2 yearsCitation18. The comparator was histology-based PDC given every 3 weeks for four treatment cycles, followed by optional pemetrexed maintenance therapy for patients with nonsquamous (NSQ) NSCLC that had not progressed after four cycles of chemotherapyCitation18.
Duration of treatment (DoT) data collected in CheckMate 9LA were used to model treatment costs associated with NIVO + IPI + PDC and PDC. The cost of disease management over the time horizon of the analysis was estimated by combining the time spent in the PF and PD health states with the cost of routine interventions used for patient monitoring in each of the health states (). Health outcomes included the number of life-years (LYs) and the number of quality-adjusted life-years (QALYs), which was estimated by combining LYs with health-state utilities. Costs and health outcomes were discounted at 3.0% annually, in accordance with US guidelinesCitation21. Incremental cost per LY gained and incremental cost per QALY gained were calculated and considered to be the primary outcomes of the analysis.
Table 1. Cost inputs in the models.
The analysis adopted the perspective of a US healthcare payer. Costs were collected for, or inflated to, 2020 US dollars (USD) as needed. The time horizon was 25 years, which was assumed to be the remaining lifetime for patients with advanced NSCLC, consistent with HTA guidance and appraisals as well as published manuscripts on cost-effectiveness analysis of ICIs in NSCLCCitation22–27. The cycle length was 1 week for the first 28 weeks and 4 weeks thereafter. Half-cycle correction was applied.
Survival analysis
OS, PFS, and DoT data were derived from CheckMate 9LA for the NIVO + IPI + PDC and PDC treatment armsCitation18. OS data from CheckMate 9LA were first extrapolated using standard parametric models recommended by Latimer et al.Citation28. However, with a 12.7-month minimum follow-up for OSCitation12, those data were still relatively immature. Therefore, data from Part 1(a and b) of the more mature CheckMate 227 trial (37.7-month minimum follow-up for OS) were used to inform long-term extrapolations of OS estimates for CheckMate 9LA (). This decision was supported by the similarities between CheckMate 227 and CheckMate 9LA in terms of patient characteristics and treatment regimens (Supplemental Table S1) and the expectation (based on expert clinical validation) that both trials will have comparable long-term outcomes (Supplemental Figure S1). Moreover, dual immuno-oncology (IO) therapy with NIVO + IPI was shown to confer durable responses and survival in the first-line treatment of advanced NSCLC, reaching a plateau after 2 years, as demonstrated in CheckMate 227Citation12, as well as in other indications such as metastatic melanoma and advanced renal cell carcinomaCitation30–32. Given that data from CheckMate 9LA are currently available for only 1 year of follow-up, they would not be expected to capture such a plateau effect, which appears to be unique for dual IO therapyCitation33. Clinical experts suggested that OS estimates for NIVO + IPI + PDC should be at least as good as the long-term OS estimates derived from CheckMate 227 Part 1.
Figure 1. Overall survival and progression-free survival in the NIVO + IPI + PDC and PDC arms, comparing trial KM data and selected parametric curves. OS extrapolations: NIVO + IPI + PDC 2-knot spline normal; PDC log-logistic; PFS extrapolations: NIVO + IPI + PDC 2 knot spline odds; PDC 2 knot spline normal. Abbreviations. IPI, ipilimumab; KM, Kaplan-Meier; NIVO, nivolumab; OS, overall survival; PDC, platinum-doublet chemotherapy; PFS, progression-free survival. Source: Paz-Ares et al.Citation18, Hellmann et al.Citation12, Ramalingam et al.Citation29
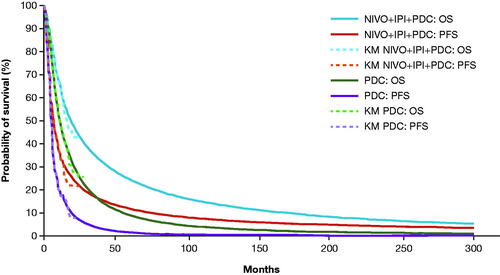
Jackson et al.Citation34 described a framework for how external data may be utilized to inform long-term survival extrapolations, provided that both data sources are sufficiently similar and demonstrate comparable long-term outcomes (for example, the mortality rate over time). Kaplan–Meier (KM) data for up to 13 months of follow-up were obtained from CheckMate 9LA. This cutoff was selected to avoid the risk of bias due to heavy censoring for OS after 13 months, a justification that was confirmed by experts. After 13 months, extrapolations based on CheckMate 227 Part 1 data were applied for OS and PFS. All survival extrapolations were derived from CheckMate 227 using the approach detailed by Latimer et al.Citation35. The “per cycle conditional survival” rates were subsequently applied to the proportion of patients having survived to 13 months.
Model fitting for the CheckMate 227 curves was conducted following National Institute for Health and Care Excellence guidanceCitation36. Statistical tests (e.g. Therneau and Grambsch correlation testCitation37) and log-cumulative hazard plots suggested that the proportional hazards assumption was violated for both OS and PFS; this was not unexpected given the different mechanisms of action of chemotherapy and IO agentsCitation33. Therefore, parametric curves were fitted independently for each treatment arm (i.e. NIVO + IPI + PDC and PDC). The base-case parametric models were selected based on goodness-of-fit statistics (Akaike information criterion and Bayesian information criterion), visual inspection, validation of extrapolations with longer-term external data from CheckMate 227, a pooled analysis of the CheckMate 017 and CheckMate 057 trials, Nordic registry data, and Surveillance, Epidemiology and End Results (SEER) program data. For more detail, see Supplementary Material, Validation of OS.
For OS, the selected model for NIVO + IPI + PDC was spline on normal 2 knots, and for PDC, the selected model was log-logistic (; Supplemental Table S2 and S3). For PFS, the selected models were spline on odds 2 knots for NIVO + IPI + PDC and spline on normal 2 knots for PDC (; Supplemental Table S4 and S5). No parametric extrapolation was needed for DoT of NIVO + IPI + PDC and PDC due to the maturity of the data; therefore, KM curves were directly used to inform DoT and related costs in the model.
Safety data
The incidence of adverse events (AEs) used in the analysis was taken from the incidence of Common Terminology Criteria for Adverse Events grade ≥3 treatment-related AEs experienced by ≥5% of patients receiving NIVO + IPI + PDC or PDC in CheckMate 9LA.
Utilities and disutilities
Patient-level quality of life data was obtained from CheckMate 9LA using the EQ-5D–3-level (EQ-5D-3L) questionnaire. The EQ-5D-3L utility index was derived using US weights. The progression-based and time-to-death (TTD)–based health state utilities are provided in Supplementary Material, Table S6. Treatment-specific progression-based utilities were selected based on model fit and used in the base-case analysis. TTD utilities and overall progression-based utilities were applied in scenario analyses.
Disutilities associated with AEs are shown in Supplementary Table S7. AE disutilities were excluded in the base case to avoid double-counting as it was assumed that treatment-specific utilities already capture decrements associated with AEs. Non-treatment-specific progression-based and TTD utilities were assumed not to capture disutilities associated with AEs; AE disutilities were therefore applied in these scenarios as a one-off utility decrement in the first model cycle.
Costs
US-specific unit costs for disease management (PF and PD health states); end-of-life care; drug acquisition, administration, and monitoring; management of AEs; and subsequent treatments were included in the model. Costs from older sources were inflated by the medical care Consumer Price Index to August 2020 USD.
Disease management costs for PF and PD states were $569 and $1,706 per 4-week cycle, respectively ( and Supplementary Material, Table S8). End-of-life costs of $15,351 were applied as a one-off fixed cost to all patients entering the death state. The end-of-life cost was obtained from a previous publication in lung cancer patientsCitation20, and inflated to 2020 USD.
Drug acquisition costs for NIVO + IPI + PDC and PDC are summarized in . The cost per dose was calculated as a weighted average of the proportion of patients receiving each drug combination in CheckMate 9LA (Supplementary Material, Table S9).
Drug administration costs are also provided in and included up to 1 h per chemotherapy intravenous infusion plus one sequential treatment of up to one additional hour. All treatments were administered in an outpatient setting. Costs were weighted based on the proportion of patients receiving each treatment. Drug-monitoring costs, in addition to disease-management costs, reflect treatment-specific resource use such as laboratory tests and scans, which are needed to ensure that patients can tolerate the treatment ().
Pemetrexed maintenance therapy was an option for patients with NSQ NSCLC receiving PDC. The additional costs associated with acquisition, administration, and monitoring are summarized in ; further details are provided in Supplementary Material, Table S10.
The cost of AE management () was based on the cost of each AE (Supplementary Material, Table S7) and the proportion of patients incurring each AE for each treatment. The cost associated with each AE was applied as a one-off cost in the first treatment cycle, as described above for AE-associated disutilities.
Drug acquisition, administration, and monitoring costs for subsequent (second-line) treatments were also included in the model. The proportion of patients receiving subsequent treatment after having failed first-line treatment was 31% for NIVO + IPI + PDC and 40% for PDC, based on data from CheckMate 9LA. The distribution of subsequent treatments is shown in Supplementary Material, Table S11. Clinical experts confirmed that the proportions of patients receiving subsequent treatment reflect current practice. The duration of second-line therapy for IO therapies was derived by calculating the 2-year restricted mean for nivolumab DoT based on the 5-year database lock of the pooled CheckMate 017 and CheckMate 057 trials in which patients with NSCLC had received chemotherapy as a first-line treatmentCitation4. This was estimated to be 6.8 months, which was confirmed to be clinically plausible by clinical expert opinion. For second-line chemotherapies, the duration was based on clinical expert opinion and was estimated at six 3-week cycles or 4.1 months. The duration of pemetrexed maintenance therapy was estimated at 5.5 months based on clinical expert opinion.
Sensitivity and scenario analysis
Sensitivity analyses were conducted to assess the impact of uncertainty in model inputs on the outcomes. One-way deterministic sensitivity analysis was conducted by varying the values for key model parameters by their standard error, 95% confidence interval, or a range of ±20%, according to data availability. Probabilistic sensitivity analysis was conducted by assigning a probabilistic distribution to each model input, running the model with model outcomes recorded for 1,000 iterations. Details of the sensitivity analyses are provided in Supplementary Material, Supplementary Methods, Sensitivity Analyses.
Scenario analyses were undertaken to investigate the effect of model inputs on costs and outcomes and are described in Supplementary Material, Supplementary Methods, Scenario Analyses, Table S10.
Results
Base-case cost-effectiveness analysis
In the base-case analysis, treatment with NIVO + IPI + PDC resulted in gains in LYs, QALYs, and total costs compared with PDC (). NIVO + IPI + PDC would therefore provide higher projected health benefits than PDC, at higher total cost. The cost breakdown indicated the higher total cost observed with NIVO + IPI + PDC compared with PDC was primarily attributable to the difference in drug acquisition costs ().
Table 2. Base-case results for NIVO + IPI + PDC versus PDC.
The incremental cost of NIVO + IPI + PDC versus PDC was $197,672 (). Treatment with NIVO + IPI + PDC would provide 1.81 incremental LYs and 1.49 incremental QALYs compared with PDC (). For NIVO + IPI + PDC compared with PDC, the incremental cost per LY gained was $108,928 and the incremental cost per QALY gained was $132,960 ().
Sensitivity analysis
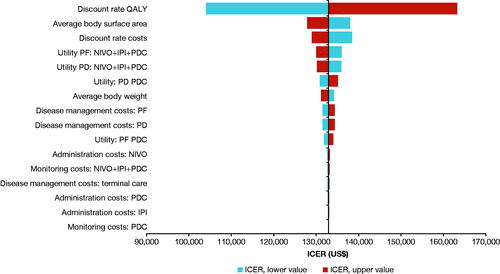
Deterministic sensitivity analysis indicated that the most influential parameters affecting the results were the discount rates applied to QALYs, average surface body area, and discount rates applied to costs (). Most parameters did not have a large effect on the ICER ().
Figure 2. Deterministic sensitivity analysis of NIVO + IPI + PDC versus PDC showing the parameters with the most impact on the ICER. Abbreviations. ICER, incremental cost-effectiveness ratio; IPI, ipilimumab; NIVO, nivolumab; PD, progressed disease; PDC, platinum-doublet chemotherapy; PF, progression free; QALY, quality-adjusted life-year. See Supplementary Material, Supplemental Methods, Sensitivity Analyses for details of the analysis. Ranges the parameters varied by in the deterministic sensitivity analysis:
- Discount rate: varied from 0% to 6%Citation21.
- Body weight and body surface area: varied by ±20%.
- Costs, including disease management, treatment acquisition, administration, and monitoring: varied by ±20%.
- Utilities, PF and PD health states (treatment specific): varied by 95% confidence intervals.
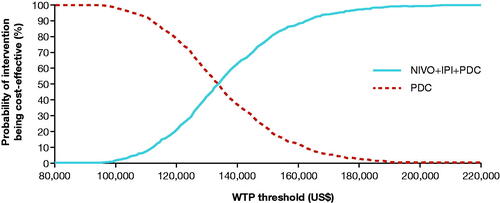
Probabilistic sensitivity analysis generated results consistent with the base case (incremental cost per QALY gained, $132,960 vs $131,410), indicating that the results were robust. The cost-effectiveness acceptability curve is shown in . At a range of willingness-to-pay (WTP) thresholds of $150,000/QALY to $250,000/QALY, NIVO + IPI + PDC had a 78–100% probability of being cost-effective compared with PDC.
Figure 3. Cost-effectiveness acceptability curve for NIVO + IPI + PDC and PDC. Abbreviations. chemo, chemotherapy; IPI, ipilimumab; NIVO, nivolumab; PDC, platinum-doublet chemotherapy; WTP, willingness-to-pay. See Supplementary Material, Supplementary Methods, Sensitivity Analyses for details of the analysis.
Scenario analysis
A broad range of scenario analyses were conducted and are listed in the Supplementary Material. summarizes the findings of the key scenario analyses that had the highest impact on the ICER. These considered the effects of using non-treatment-specific utilities by progression status and TTD, both of which incorporates treatment-related AE disutilities, and survival curve transitions from CheckMate 9LA to CheckMate 227 at 6 and 20 months to investigate the impact of using extrapolated KM data from CheckMate 9LA. None of these scenarios changed the estimated ICER by more than 10%. Additional scenarios are shown in Supplementary Material, Supplementary Methods, Table S12.
Table 3. Scenario analyses results for NIVO + IPI + PDC versus PDCa.
Discussion
The results of this economic evaluation of NIVO + IPI + PDC as a first-line treatment in advanced NSCLC in the US showed that NIVO + IPI + PDC has an incremental cost per QALY gained of $132,960 compared with PDC. Deterministic and probabilistic sensitivity analysis indicated that the results were robust to changes in input parameters and assumptions. Probabilistic sensitivity analysis indicates that at a WTP of $150,000/QALY to $250,000/QALY, NIVO + IPI + PDC has a 78–100% probability of being cost-effective. There is no explicitly defined WTP threshold in the US; however, it has been noted that the acceptable cost-effectiveness threshold in 2003 approached $200,000 or more per QALYCitation38, which when adjusted to 2020 USD exceeds $300,000Citation33. The findings of a more recent survey report suggest that acceptable thresholds for end-of-life care in metastatic cancer may be higherCitation39. Thus, the projected ICERs presented here lie well within the range considered cost-effective in the US.
We evaluated four previously published studies evaluating the cost-effectiveness of NIVO + IPI for the first-line treatment of NSCLC and noted differences and weaknesses in model structure, assumptions, and inputs. Using published data from the CheckMate 9LA trial, Peng et al. showed that NIVO + IPI + PDC conferred an additional 0.8 QALYs and an ICER of $202,275/QALY gained versus PDC aloneCitation40. The difference in findings between the study of Peng et al. and those of the present study could be attributable to differences in the modeling assumptions, inputs, and other assumptions. The authors applied a hazard ratio to the PDC reference curve to generate OS results for NIVO + IPI + PDC which disregarded that the proportional hazard assumption was violated. The long-term extrapolations of survival outcomes were not validated whereas we used longer-term CheckMate 227 data to supplement the follow-up in the CheckMate 9LA trial, and then validated the long-term OS extrapolations using pooled data from the phase 3 CheckMate 017 and CheckMate 057 trials in the pretreated setting, and real-world data (SEER and Swedish and Norwegian registry data), together with input from clinical experts.
Another recently published cost-effectiveness analysis by Courtney et al. reported that treatment with NIVO + IPI combination therapy was associated with an increase in overall cost of $201,900 and an improved effectiveness of 0.50 QALYs compared with chemotherapy, yielding an ICER of $401,700/QALYCitation41. Substantial differences in modeling methodology, assumptions, and inputs account for higher incremental costs, with lower incremental QALYs resulting in a higher ICER. Courtney et al. also applied a hazard ratio to the PDC reference curve to generate OS results for NIVO + IPI disregarding that the proportional hazard assumption was violated. Courtney et al. used published aggregate data rather than individual patient data, utilities from the literature rather than deriving them from trials, and a time horizon limited to 10 years rather than lifetime, which may not have captured the full benefits of the treatment over the lifetime of the patients. In cost-effectiveness studies of ICIs including NIVO + IPI, authors have tended to support a horizon of 20-years or more in order to capture the long-term survival of ICIs in NSCLCCitation24–27. Finally, in contrast to this study they did not validate the long-term extrapolations of OS.
Another study by Li et al. yielded an ICER of $180,307 with an incremental cost of $128,984 and an incremental QALY value of 0.715Citation42. However, the results of this study were likely influenced by their analysis being limited to standard parametric models and the selection of loglogistic analysis as a base-case. The present analysis found that other models had a better statistical fit and made use of external validation to select curves that provided realistic long-term survival results.
A study by Hu et al., which analyzed only subgroups, found NIVO + IPI to be cost-effective for both the PD-L1 ≥ 1% and ≥50% populationsCitation43. The study employed a three health-state model, and the authors selected a Weibull distribution for the survival extrapolations, although the rationale for this selection was not provided. Additionally, the source of the efficacy data for the PD-L1 ≥ 50% population analyzed in this study was unclear, as none of the cited studies reported a KM analysis for that subgroup.
Despite the recent advances in treatments for metastatic NSCLC (i.e. pembrolizumab plus chemotherapyCitation44 and pembrolizumab monotherapyCitation45, both approved in the US as first-line treatments for advanced NSCLC regardless of PD-L1 expression status and with PD-L1 ≥ 1%, respectively, and atezolizumab in combination with nab-paclitaxelCitation46) there is a need for chemotherapy-free or reduced-chemotherapy–based IO treatment options in the first-line setting that offer potential for improved long-term survival in more patients. The findings of the CheckMate 227 trial suggest that NIVO + IPI represents such an option for chemotherapy-free first-line treatment of patients with advanced NSCLC with tumor PD-L1 expression ≥1%, while those of CheckMate 9LA provide an alternative with a combination with reduced-PDC regimen in combination with NIVO + IPICitation12,Citation18.
Strengths
The cost-effectiveness analysis presented here has several strengths. The key value of NIVO + IPI + PDC is the rapid initial disease control while building on the potential for long-term durable survival benefits. Within the economic model, individual patient data from CheckMate 227, a pivotal registrational trial that directly reflects the patient population and the intervention treatments under consideration with significant data maturity (37.7-month minimum follow-up), were leveraged to inform extrapolations beyond 13 months observed in CheckMate 9LA. These long-term OS extrapolations were validated using both real-world datasets that provided OS data up to 15 years (SEER and Swedish and Norwegian registry data) and pooled 5-year data from the phase 3 CheckMate 017 and CheckMate 057 trials in the pretreated setting, as well as input from clinical experts. Health-state utility weights were derived from EQ-5D data directly collected in the CheckMate 9LA trial from patients following disease progression, and the values used in the model are considered representative of the target population. Partitioned survival models with PF, PD, and death health states have been extensively validated and applied in numerous previous technology appraisals in the metastatic setting. Sensitivity and scenario analyses indicated that the model results were robust and not sensitive to changes in input parameters.
Limitations
As this is the first step and within randomization trial analysis of this study, NIVO + IPI + PDC was assessed against PDC only and alternative IO therapies that are licensed for the first-line treatment of NSCLC in the US were not considered. Comparisons with alternative IOs are beyond the scope of this study and assessment of systematic literature reviews/network-meta-analyses to allow indirect comparisons of NIVO + IPI + PDC against other IO-based regimens is ongoing; these data will be reported once all relevant trials have reached sufficient maturity to appropriately capture both the short- and long-term benefits of NIVO + IPI + PDC. With a minimum follow-up of 12.7 months for OS, CheckMate 9LA data are still relatively immature. However, given the similarities in patient populations and treatment regimens between CheckMate 9LA and CheckMate 227, it was possible to leverage more mature CheckMate227 survival data to extrapolate OS beyond 13 months using the approach published by Jackson et al.Citation34. Long-term extrapolation of OS using data from short-term clinical trials is inherently subject to uncertainty. This study reports significant efforts to validate long-term OS extrapolations against long-term data from external sources (CheckMate 227, a pooled analysis of CheckMate 017 and CheckMate 057 trials, Nordic registry data, and SEER program data). However, real-world evidence from these registries mainly reflects outcomes from chemotherapy and potentially underestimates long-term OS outcomes with IO-based therapy.
The model may underestimate the durable response of the NIVO + IPI + PDC regimen in the long term because treatment response is not explicitly modeled as a prognostic factor for survival. It is instead assumed that treatment response from a first-line therapy will not alter future disease progression on subsequent therapies. Structural sensitivity analysis investigating alternative modeling frameworks was not explored in this study. Finally, disutilities for AEs were not directly reported in the CheckMate 9LA trial and therefore had to be sourced from the published literature.
Conclusion
The current analysis indicates that NIVO + IPI + PDC (two cycles) is a cost-effective option to treat patients with treatment-naive, advanced NSCLC, regardless of histology and PD-L1 expression level. Deterministic sensitivity analysis indicated that the results were robust and not sensitive to changes in input parameters; the most influential parameters were the discount rates for costs and outcomes, average body surface area, and the application of progression-based utilities. Probabilistic sensitivity and scenario analyses also supported the robustness of base-case ICER as well as the overall approach, as the methods used to estimate utilities and the choice of the cutoff used in the survival analysis did not substantially change the value of the ICER. NIVO + IPI + PDC (two cycles) offers a new cost-effective first-line treatment option for patients with advanced NSCLC, with an ICER that is within the range considered acceptable in the US.
Transparency
Declaration of funding
This study was funded by Bristol Myers Squibb.
Declaration of financial/other relationships
MP, HS, PD, and CJ were employees and JM is an employee of Parexel International, and were funded by Bristol Myers Squibb to conduct the analysis. YY, MAC, NV, AL, SJL, and JRP are employees of Bristol Myers Squibb.
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
All authors contributed to study conception and design, drafted the manuscript, and approved of the final version for submission. MP, HS, JM, PD, and CJ performed the analysis.
Supplemental Material
Download Zip (762.6 KB)Acknowledgements
Editorial and medical writing support was provided by Simon Foulcer, PhD, CMPP, and Russ Craddock, PhD, of Parexel International and was funded by Bristol Myers Squibb.
Data availability statement
The analysis reported in this study uses patient-level data from the CheckMate 9LA trial and CheckMate 227 Part 1 data. The patient-level data are not publicly available, but the results of the trial have been reported in a number of publications.
References
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2021;71(3):660–249.
- American Cancer Society. Key statistics for lung cancer [Internet]. [updated 12 January 2021; cited 14 September 2021]. Available from: https://www.cancer.org/cancer/lung-cancer/about/key-statistics.html.
- National Cancer Institute. SEER Cancer Statistics Review, 1975–2015 [Internet]. [updated April 2018; cited 5 November 2021]. Available from: https://seer.cancer.gov/csr/1975_2015/.
- Borghaei H, Gettinger S, Vokes EE, et al. Five-year outcomes from the randomized, phase III trials CheckMate 017 and 057: nivolumab versus docetaxel in previously treated non-small-cell lung cancer. J Clin Oncol. 2021;39(7):723–733.
- Gettinger S, Horn L, Jackman D, et al. Five-year follow-up of nivolumab in previously treated advanced non-small-cell lung cancer: results from the CA209-003 study. J Clin Oncol. 2018;36(17):1675–1684.
- Duma N, Santana-Davila R, Molina JR. Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc. 2019;94(8):1623–1640.
- Dong J, Li B, Lin D, et al. Advances in targeted therapy and immunotherapy for non-small cell lung cancer based on accurate molecular typing. Front Pharmacol. 2019;10:230.
- OPDIVO (nivolumab) [prescribing information]. Princeton (NJ): Bristol Myers Squibb; 2021.
- YERVOY (ipilimumab) [prescribing information]. Princeton (NJ): Bristol Myers Squibb; 2020.
- Das R, Verma R, Sznol M, et al. Combination therapy with anti-CTLA-4 and anti-PD-1 leads to distinct immunologic changes in vivo. J Immunol. 2015;194(3):950–959.
- Wei SC, Duffy CR, Allison JP. Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov. 2018;8(9):1069–1086.
- Hellmann MD, Paz-Ares L, Bernabe Caro R, et al. Nivolumab plus ipilimumab in advanced non-small-cell lung cancer. N Engl J Med. 2019;381(21):2020–2031.
- Carbone DP, Reck M, Paz-Ares L, et al. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N Engl J Med. 2017;376(25):2415–2426.
- Mok TSK, Wu YL, Kudaba I, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819–1830.
- Rizvi NA, Cho BC, Reinmuth N, et al. Durvalumab with or without tremelimumab vs standard chemotherapy in first-line treatment of metastatic non-small cell lung cancer: the MYSTIC phase 3 randomized clinical trial. JAMA Oncol. 2020;6(5):661–674.
- Bracci L, Schiavoni G, Sistigu A, et al. Immune-based mechanisms of cytotoxic chemotherapy: implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ. 2014;21(1):15–25.
- Peng J, Hamanishi J, Matsumura N, et al. Chemotherapy induces programmed cell death-ligand 1 overexpression via the nuclear factor-κB to foster an immunosuppressive tumor microenvironment in ovarian cancer. Cancer Res. 2015;75(23):5034–5045.
- Paz-Ares L, Ciuleanu TE, Cobo M, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(2):198–211.
- National Comprehensive Cancer Network. Non-small cell lung cancer (version 5.2021) [Internet]. [updated May 2021; cited 14 September 2021]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf.
- Bremner KE, Krahn MD, Warren JL, et al. An international comparison of costs of end-of-life care for advanced lung cancer patients using health administrative data. Palliat Med. 2015;29(10):918–928.
- Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–1103.
- Latimer NR. NICE DSU technical support document 14: survival analysis for economic evaluations alongside clinical trials - extrapolation with patient-level data [Internet]. School of Health and Related Research, University of Sheffield, UK: [updated 2021 Jul 8]. Available from: http://nicedsu.org.uk/wp-content/uploads/2016/03/NICE-DSU-TSD-Survival-analysis.updated-March-2013.v2.pdf.
- National Institute for Health and Care Excellence. NICE technology appraisal guidance [TA531]: pembrolizumab for untreated PD-L1-positive metastatic non-small-cell lung cancer [Internet]. [updated 2021 Feb 13]. Available from: https://www.nice.org.uk/guidance/ta531/resources/pembrolizumab-for-untreated-pdl1positive-metastatic-nonsmallcell-lung-cancer-pdf-82606895901637.
- Chaudhary MA, Lubinga SJ, Smare C, et al. Cost-effectiveness of nivolumab in patients with NSCLC in the United States. Am J Manag Care. 2021;27(8):e254–e260.
- Huang M, Lou Y, Pellissier J, et al. Cost effectiveness of pembrolizumab vs. standard-of-care chemotherapy as first-line treatment for metastatic NSCLC that expresses high levels of PD-L1 in the United States. Pharmacoeconomics. 2017;35(8):831–844.
- Insinga RP, Vanness DJ, Feliciano JL, et al. Cost-effectiveness of pembrolizumab in combination with chemotherapy in the 1st line treatment of non-squamous NSCLC in the US. J Med Econ. 2018;21(12):1191–1205.
- Insinga RP, Vanness DJ, Feliciano JL, et al. Cost-effectiveness of pembrolizumab in combination with chemotherapy versus chemotherapy and pembrolizumab monotherapy in the first-line treatment of squamous non-small-cell lung cancer in the US. Curr Med Res Opin. 2019;35(7):1241–1256.
- Latimer NR. Survival analysis for economic evaluations alongside clinical trials-extrapolation with patient-level data: inconsistencies, limitations, and a practical guide. Med Decis Making. 2013;33(6):743–754.
- Ramalingam SS, Ciuleanu TE, Pluzanski A, et al. Nivolumab + ipilimumab versus platinum-doublet chemotherapy as first-line treatment for advanced non-small cell lung cancer: three-year update from CheckMate 227 part 1. J Clin Oncol. 2020;38(15_suppl):9500–9500.
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2019;381(16):1535–1546.
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373(1):23–34.
- Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277–1290.
- Quinn C, Garrison LP, Pownell AK, et al. Current challenges for assessing the long-term clinical benefit of cancer immunotherapy: a multi-stakeholder perspective. J Immunother Cancer. 2020;8(2):e000648.
- Jackson C, Stevens J, Ren S, et al. Extrapolating survival from randomized trials using external data: a review of methods. Med Decis Making. 2017;37(4):377–390.
- Latimer NR. Response to "survival analysis and extrapolation modeling of time-to-event clinical trial data for economic evaluation: an alternative approach" by Bagust and Beale. Med Decis Making. 2014;34(3):279–282.
- Rutherford MJ, Lambert PC, Sweeting MJ, et al.. NICE DSU technical support document 21: flexible methods for survival analysis [Internet]. [updated 2021 Jan 23; cited 2021 Sep 14]. Available from: http://nicedsu.org.uk/wp-content/uploads/2020/11/NICE-DSU-Flex-Surv-TSD-21_Final_alt_text.pdf.
- Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81(3):515–526.
- Ubel PA, Hirth RA, Chernew ME, et al. What is the price of life and why doesn’t it increase at the rate of inflation? Arch Intern Med. 2003;163(14):1637–1641.
- Nadler E, Eckert B, Neumann PJ. Do oncologists believe new cancer drugs offer good value? Oncologist. 2006;11(2):90–95.
- Peng Y, Zeng X, Peng L, et al. Cost-effectiveness of nivolumab plus ipilimumab combined with two cycles of chemotherapy as first-line treatment in advanced non-small cell lung cancer. Adv Ther. 2021;38(7):3962–3972.
- Courtney PT, Yip AT, Cherry DR, et al. Cost-effectiveness of nivolumab-ipilimumab combination therapy for the treatment of advanced non-small cell lung cancer. JAMA Netw Open. 2021;4(5):e218787.
- Li J, Zhang T, Xu Y, et al. Cost-effectiveness analysis of nivolumab plus ipilimumab versus chemotherapy as first-line treatment in advanced NSCLC. Immunotherapy. 2020;12(14):1067–1075.
- Hu H, She L, Liao M, et al. Cost-effectiveness analysis of nivolumab plus ipilimumab vs. chemotherapy as first-line therapy in advanced non-small cell lung cancer. Front Oncol. 2020;10:1649.
- FDA approves pembrolizumab in combination with chemotherapy for first-line treatment of metastatic squamous NSCLC Internet]. White Oak (MD): U.S. Food and Drug Administration; [updated 2018 Dec 14; cited 2021 Sep 14]. Available from: https://www.fda.gov/drugs/fda-approves-pembrolizumab-combination-chemotherapy-first-line-treatment-metastatic-squamous-nsclc.
- FDA expands pembrolizumab indication for first-line treatment of NSCLC (TPS ≥1%) [Internet]. White Oak (MD): U.S. Food and Drug Administration. [updated 2019 Apr 11; cited 2021 Sep 14]. Available from: https://www.fda.gov/drugs/fda-expands-pembrolizumab-indication-first-line-treatment-nsclc-tps-1.
- FDA approves atezolizumab with nab-paclitaxel and carboplatin for metastatic NSCLC without EGFR/ALK aberrations [Internet]. White Oak (MD): U.S. Food and Drug Administration; [updated 2019 Dec 5; cited 2021 Sep 14]. Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-atezolizumab-nab-paclitaxel-and-carboplatin-metastatic-nsclc-without-egfralk.
