Abstract
Aim
JointRep is a bioadhesive hydrogel arthroscopically injected to facilitate cartilage regeneration. The cost-effectiveness of JointRep with microfracture surgery compared to microfracture alone was evaluated from the Australian healthcare system perspective, in patients with symptomatic focal chondral defects (Outerbridge Grade 3 or 4) of the knee who had failed conservative treatment and were indicated for surgery.
Materials and methods
A de novo Markov model comprising two health states- ‘Alive’ and ‘Dead’ was developed. Model transition probability was based on the general population mortality rates. Clinical outcomes were assessed using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores, a validated patient-reported tool measuring pain, stiffness, and physical function. The utility was derived by mapping WOMAC scores to EQ-5D scores using a published algorithm. Cost inputs were based on published Australian costs from AR-DRGs, Medicare Benefits Schedule, and Prostheses List. Model outcomes included costs, Quality-adjusted life years (QALYs), and incremental cost-effectiveness ratio (ICER). Base-case analysis was conducted for a time horizon of 3 years and a cycle length of 1 year. Cost and health outcomes were discounted at 5% per annum. Sensitivity and scenario analyses were also conducted.
Results
Total QALYs were estimated to be higher for JointRep with microfracture surgery (2.61) compared to microfracture surgery alone (1.66), an incremental gain of 0.95 QALY. JointRep with microfracture surgery was associated with an incremental cost of $6,022 compared to microfracture surgery alone, thus leading to an ICER of $6,328. Results were substantially robust to varying parameters in the sensitivity analyses conducted, alternative model settings and assumptions in scenario analyses.
Limitations
The clinical inputs used in the model were based on data from short duration, non-randomized, post-market clinical trial.
Conclusions
JointRep with microfracture surgery is a cost-effective treatment option compared to microfracture alone from the Australian health care system perspective.
Introduction
An osteochondral defect is a localized defect of the articular cartilage and the underlying bone (subchondral bone)Citation1–3. Osteochondral defects of the knee occur due to the removal of a portion of the articular cartilage from the knee joint surface and could be a result of trauma, microtrauma, biological conditions (osteochondritis dissecans or osteonecrosis) or genetic factorsCitation4,Citation5. Articular cartilage is avascular and has poor repair ability, therefore, any injury or damage to the cartilage can seriously affect joint function and mobilityCitation6. Clinically, osteochondral defects can manifest as pain, locking, stiffness, swelling and functional impairment of the affected jointCitation4,Citation5.
As per the Outerbridge classification, chondral defects of the knee can be classified into four grades: Grade 1 – softening and swelling of the cartilage; Grade 2 – fragmentation and fissuring in an area half an inch or less in diameter; Grade 3 – fragmentation and fissuring in an area more than half an inch in diameter; Grade 4 – the erosion of cartilage down to boneCitation7.
Osteochondral defects are initially treated with conservative measures which may include restricting physical activity (weight-bearing and sports activities) and targeted physiotherapy, but these have limited ability to solve the underlying problem of cartilage damageCitation4,Citation5,Citation8. Conservative treatments do not lead to healing of the defect but may provide symptomatic relief for a time. Surgical evaluation and treatment via an arthroscopic procedure is the preferred option upon failure of conservative treatmentCitation4,Citation5. There are various surgical treatment options to mitigate osteochondral defects: chondroplasty, microfracture surgery, osteochondral autograft transplant (OAT), matrix-assisted chondrocyte implantation (MACI) and autologous chondrocyte implantation (ACI))Citation4,Citation9. While conventional surgical treatment options such as microfracture surgery are limited in their ability to generate hyaline cartilage, novel scaffold-based therapies (such as the Chitosan-based ones BST CarGel and JointRep) have been developed to promote tissue repair when administered with microfracture surgery. A randomized clinical trial reported superior short-term (1 year) and long-term (5 years) repair tissue quantity and quality with one of these chitosan-based scaffolds (BST-CarGel, Piramal Life sciences, Bio-Orthopaedics Division at the time of the trials, now the product is part of the Smith & Nephew family of products) administered with microfracture surgery in 41 knees affected by single focal cartilage lesion (Grade 3 to 4) on femoral condyles compared to 39 knees treated with microfracture aloneCitation10,Citation11.
Recently, a new cartilage bioadhesive gel technology – JointRep (Oligo Medic Inc., Laval, Quebec Canada) was introduced, which uses a modern chitosan-based hydrogel scaffold matrixCitation9,Citation12. JointRep is an arthroscopically injectable sterile, non-pyrogenic, hydrogel implant that is liquid and conforming at room temperature. It is mixed intraoperatively prior to delivery and injected into the cartilage defect immediately following bone-marrow stimulating arthroscopic surgery (such as microfracture surgery). Once injected, the solution rapidly jellifies at body temperatureCitation9. The resulting matrix provides a scaffold for chondrocyte proliferation while discouraging adhesive cell growth (osteoblasts and fibroblasts). It may eventually lead to tissue regrowth that has qualities similar to that of hyaline cartilage. This is in line with previous findings for the hyaline characteristics of the new tissue, as shown by Méthot et al.Citation13 for the predicated device, where the said characteristics of the tissue were demonstrated by blinded, multiple and independent analysis from the biopsies obtained from patients in the pivotal study. The biomechanical properties of JointRep might allow for a more aggressive progression to full weight-bearing as tolerated (WBAT) following surgeryCitation9. This is in contrast to microfracture surgery alone where a patient may remain on crutches for the first 6 weeks, with zero or limited weight bearingCitation14. Thus, JointRep in conjunction with bone marrow stimulation (like microfracture surgery) may take less time and provides a minimally invasive curative treatment for Grade 3 or 4 osteochondral defects of the kneeCitation9,Citation12.
JointRep was included on the Australian Prostheses List (PL), Part A in July 2019 (rebate code DE681) with a benefit of $6,022Citation15. The PL is a list of medical devices or prostheses, that stipulates the benefit amount (or a price) for which private health insurers (PHI) in Australia are then required to pay this benefit, for the specific prostheses used, over and above the hospital admission. The PHI is only required to pay this benefit where a member has the relevant coverage with the specific PHICitation16. The PL requirements are legislated and set out in the Private Health Insurance Act 2007Citation17. The PL is divided into Parts A, B and C, which collectively cover approximately 11,000 devices. Specifically, Part A of the PL (where JointRep is currently listed) covers devices that are used as part of a hospital or hospital substitute treatment, where a benefit must be paid to the doctor for the procedure performed. A device listed in Part A of the PL must be surgically implanted in the body, enable another device to be implanted or allow an implant to continue to function after surgery. Devices on Part A must also be approved for use by the Therapeutic Goods Administration (TGA) and further, be assessed for effectiveness and cost against other products by the Prostheses List Advisory Committee (PLAC), before they can be listed on the PL (note: these PLAC evaluations are not publicly accessible)Citation18,Citation19.
There are no published studies evaluating the cost-effectiveness of JointRep in the Australian setting. The present study reports the findings of a cost-effectiveness analysis of JointRep in combination with microfracture surgery compared to microfracture surgery alone from the perspective of the Australian healthcare system.
Methods
Patient population and interventions
Patients suffering from symptomatic focal chondral defects (Outerbridge Grade 3 or 4) of the knee, having failed conservative treatment, and indicated for surgery were included in the analysis. The intervention investigated in this analysis was JointRep in combination with microfracture surgery compared to microfracture surgery alone. Microfracture surgery alone is considered the gold standard of surgical treatment of chondral defects in the Asia Pacific, and hence was used as a comparator for this analysisCitation20.
The patient baseline characteristics for the two treatment arms were sourced from a post-market clinical trialCitation9. In the trial, patients with focal osteochondral defects of the knee (N = 69) were divided into two treatment groups: JointRep with microfracture surgery (n = 46; mean age = 54.5 years; males = 63%), and microfracture surgery alone (n = 23; mean age = 56.6 years; males = 47.8%). The weighted average age (55.2 years) and proportion of males (58%) across both treatment groups was used in the analysis.
Model structure
A de novo Markov model was developed in Microsoft Excel (Version 2016) (). The model is comprised of two health states – ‘Alive’ and ‘Dead’. A cohort of eligible patients receiving either JointRep with microfracture surgery or microfracture surgery alone, enter the model in the ‘Alive’ health state. At the end of each cycle, patients may remain in the ‘Alive’ health state or may die and move to ‘Dead’ health state. Patients in ‘Dead’ health state continue to remain there for the remaining time horizon. The complete details of the inclusion and exclusion criteria have been reported in the source trial publicationCitation9.
Model settings
Since limited evidence of long-term effectiveness data could be found in the literature, a three-year time horizon was used in the base case analysis based on the follow-up duration of the pivotal JointRep clinical trial. The model used a yearly cycle length, which reflects the time period at which outcomes were measured in the JointRep trialCitation9. A half cycle correction was implemented to account for the possibility that transition may happen throughout the cycle and not just at the beginning or end of each cycle. Future costs and outcomes were discounted using an annual discount rate of 5%, in line with the MSAC guidelinesCitation21 and this annual discount is also recommended by PBAC GuidelinesCitation22. A scenario analysis was conducted using alternative discount rates of 0% and 3.5%Citation21.
Model inputs
Transition probabilities
The Markov model developed for this analysis was a 2-health state model with ‘Dead’ as an absorbing state. Therefore, the only transition that occurs in the model is patients transitioning from ‘Alive’ to ‘Dead’ health state. The model assumes no additional mortality risk due to osteochondral defects. This is based upon the evidence from the JointRep clinical trial. No deaths were observed in either of the treatment arms until the trial follow-up duration of 3 years. Hence, the probability of patients transitioning from ‘Alive’ to ‘Dead’ health state depends on the general population mortality risk in Australia. Age- and gender-specific all-cause mortality risks for the general population were obtained from the Australian life tables (Australian Life Tables: Australian Bureau of Statistics. Life Tables, Australia, 2018–2020)Citation23. The annual death rate used in the model was then computed based on the survival probabilities adjusted for the weighted mean baseline age and gender distribution of the overall trial population. We assumed that a combination of JointRep and microfracture offered no additional survival benefit when compared with microfracture surgery alone. Thus, the survival probability of patients in both the treatment arms was assumed to be identical in the model.
Clinical inputs
Effectiveness
The key benefit of JointRep is that it improves the quality of life of patients by improving the quality of the articular cartilage and hence the function of the knee joint, reducing the symptoms associated with cartilage defects. Several generic, as well as disease-specific instruments, have been developed to measure the QoL of knee patients. Of these, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) is one of the most widely used instruments. It is a patient-reported, 24-item questionnaire encompassing three key disease areas- pain (5 items), joint stiffness (2 items) and physical function (17 items)Citation24. Hence, WOMAC scores constituted the key effectiveness inputs in our model. Our model included the patient-level WOMAC scoresCitation9,Citation25.
WOMAC Likert scores were converted into utility values using an EQ-5D-based algorithm developed by Wailoo et al.Citation26. The WOMAC to EQ-5D mapping algorithm was originally developed based on UK tariffs. We collaborated with Wailoo et al.Citation26 and adapted the original algorithm to the Australian setting by utilising Australia-specific EQ-5D weightsCitation27,Citation28. The modified WOMAC to EQ-5D algorithm used to derive Australian utility inputs for the economic model remains unpublished but accessible by Wailoo and colleagues. Since the WOMAC to EQ-5D mapping algorithm provides a separate utility estimate for males and females, final utility values incorporated in the model were weighted by gender distribution in the respective treatment arms (). The base-case utility values derived from trial WOMAC scores suggest a substantial post-operative increase from a baseline utility of 0.42 to more than 0.90 in patients receiving JointRep + Microfracture treatment. Although the post-baseline utility in JointRep + Microfracture arm exceeds the Australian population norms of this age groupCitation29,Citation30, these utility inputs were derived using the best available evidence and a published WOMAC to EQ-5D mapping algorithm. To address the uncertainty associated with the published data of a substantial improvement in WOMAC scores from baseline in the JointRep + Microfracture arm which resulted in high post-baseline utility value, we conducted a scenario analysis by reducing the post-baseline utility values by 20% in JointRep + Microfracture arm only. This was a conservative approach since the 20% reduction in post-baseline utility was applied in JointRep + Microfracture arm only, and the utility values in this scenario analysis were lower than the Australian general population norms.
Table 1. Model utilities.
In general, the WOMAC scores recorded in the trial showed high uncertainty, as seen in their high standard deviations. Hence, to reflect the uncertainty associated with the utility value, we conducted several scenario analyses by reducing the utility values by varying degrees in both treatment arms. The utility values were reduced by 20% and 30% in JointRep + microfracture arm only, or both arms (see ).
Table 2. Scenario analyses results.
In another scenario analysis, we extrapolated the model outcomes beyond 3 years for the alternative time horizons of 5 years and 10 years and assumed no deterioration in the quality of life after 3 years. This is also likely to be a conservative assumption, based on the change observed in WOMAC scores for three years in the JointRep trial. Patients receiving JointRep + Microfracture surgery demonstrated consistent improvement in WOMAC score till 2 years post-surgery which was sustained till Year 3, whereas the patients receiving microfracture alone experienced an improvement at 6 months followed by continuous deterioration in WOMAC score till year 3. Hence, assuming no further reduction in utility value after 3 years is likely to favour the microfracture alone comparator treatment arm.
Treatment failure options: re-operation and total knee arthroplasty
During the 3-year follow-up period of the JointRep trial, none of the patients required re-operation. Two patients left the trial due to secondary trauma unrelated to the intervention. One of these patients required total knee arthroplasty (TKA) 12 months after JointRep surgery. However, the TKA procedure was not found to be related to JointRep and was attributed to additional trauma. Hence, we did not incorporate re-operation and TKA in the base-case analysis.
Including TKA observed in the JointRep clinical trial
A scenario analysis was conducted by incorporating TKA-associated costs and disutility for the patient who underwent TKA after primary surgery in the JointRep arm. Cost and disutility associated with TKA were applied in the second cycle of the model i.e. 12 months after the initial procedure. A TKA-associated disutility value of 0.1 was used in the model, based on a Markov model published by Mather et al.Citation31
Including re-operation and subsequent TKA based on a published study
Since Pipino et al.Citation9 did not report data on re-operation after primary surgery, revision surgery was not considered in the base case analysis. However, an additional scenario analysis was conducted by incorporating re-operation rates and subsequent TKA post failure of primary surgery based on a published study. The re-operation rate in each treatment arm was based on Frappier et al.Citation32, which was an economic evaluation comparing microfracture surgery alone with a combination of microfracture and a chitosan-based medical device (BST-CarGel). The economic evaluation was based on the BST-CarGel trialCitation10,Citation11, which investigated the degree of lesion filling as the primary endpoint, and WOMAC score and safety as secondary endpoints. An economic model developed by Frappier et al. estimated treatment failure as the proportion of patients failing the threshold lesion fill rate of 70% in the BST-CarGel trial. The authors reported a treatment failure rate of 18.92% in the microfracture alone arm, and 2.44% in BST-CarGel with microfracture surgeryCitation32. The BST-CarGel trial further showed a significant reduction in WOMAC scores from baseline at 1 year and 5 years in patients receiving a combination of BST-CarGel and microfracture surgery (p < .0001)Citation10,Citation11. This was consistent with the effective results of JointRepCitation9. However, unlike the BST-CarGel trial, which did not show a significant difference in WOMAC score improvement between treatment groups, Pipino et al.Citation9 the trial demonstrated a significant improvement in WOMAC overall and sub-scores in the JointRep with microfracture treatment arm compared to the microfracture alone arm (p < .0001 at 24 months). Thus, we have conservatively assumed the re-operation rate of JointRep to be identical to that of BST-CarGel (as reported in Frappier et al.Citation32). Further, based on Frappier et al., re-operation rates were applied in years 3 and 5Citation32. We did not account for disutility associated with re-operation, as it will be applicable for a short duration and is not expected to cause a substantial decrement in the overall QALYs in each arm.
Further, based on Frappier et al., it was assumed that TKA would occur 7 years after re-operation. Thus, the cost and disutility associated with TKA were applied at cycle 10 and cycle 12 (to the proportion of patients undergoing re-operation in cycle 3 and cycle 5 respectively). Therefore, the appropriate time horizon for this scenario analysis was considered to be 15 years.
Cost inputs
Health care resource use and their associated costs to the Australian health system were considered in the model, which included the cost of JointRep, surgical services, follow-up visits, rehabilitation, Magnetic Resonance Imaging (MRI), TKA, and re-operation. Unit costs of the resources included in the model were sourced from 2021 to 2022 AR-DRGs and current Medical Benefits Schedule (MBS) codesCitation33–35. A rebate of 75% of the total fee was applied to MBS costs, as the microfracture procedure (with or without JointRep) is performed in an in-patient setting and the Australian Medicare system covers 75% of the Scheduled Fee. Individual items and their respective unit costs are presented in .
Table 3. Cost inputs.
The cost of JointRep, the cost of the microfracture surgical procedure and associated surgical costs were included as a one-time cost in the first cycle of the model. The cost of JointRep was obtained from the Prostheses List, Part A, Billing Code DE681Citation15. Patients undergoing microfracture surgery in either of the treatment arms require follow-up visits at 2, 6, 12 weeks and 12 months post-surgery. It was assumed that 12 months after surgery, patients would require 2 follow-up visits per year. Thus, the cost of 4 follow-up visits was applied in cycle 1 and the cost of 2 follow-up visits was applied from cycle 2 onwards, for both the treatment arms.
Patients require a rehabilitation regime following microfracture surgery with or without JointRep, which involves a total of 11 physiotherapy sessions (interview with Australian physicians, 2020). Rehabilitation cost was based on the review of protocols of orthopaedic knee surgeons of Sydney. The cost of the first physiotherapy consultation used in the model was $150, followed by $110 per subsequent consultation, with a total cost of $1,250 for the entire physiotherapy course (interview with Australian physicians, 2020) [source document available on request]. The model assumes an identical rehabilitation regime in both the treatment arms post-surgery.
Patients undergoing microfracture surgery (with or without JointRep implantation) require post-surgery MRI scans at 6 months and 12 months. The cost of two MRI scans ($604.80) was applied as a one-time cost in the first cycle of the model for both the treatment arms.
The cost of total knee arthroplasty included prosthesis cost, procedural costs as well as associated surgical costs, and was applied in cycle 2, cycle 10 and cycle 12. The total cost of re-operation in the model included the cost of revision surgery, follow-up visit, rehabilitation (physiotherapy), and MRI scans, and was applied in cycle 3 and cycle 5. The cost of revision surgery in JointRep with microfracture surgery and the microfracture surgery alone treatment arms was assumed to be the same as the cost of the initial microfracture surgery. The cost of JointRep was not included in the revision surgery. It was assumed that patients will require two additional follow-up visits in the first year after revision surgery. The cost of physiotherapy and MRI after revision surgery were assumed to be equal to the corresponding costs after initial microfracture surgery.
Sensitivity analyses
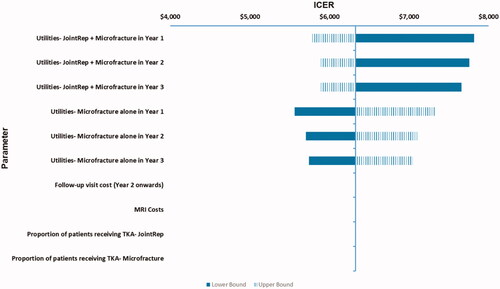
One-way sensitivity analysis (OWSA) was performed to identify the key drivers of the economic evaluation and to assess the impact of changing the parameter values on model results. In OWSA, each model input parameter was varied independently by ±20% of the base-case parameter value. It was assumed that a range of 20% variation would capture deviation from the base-case values. The results of OWSA were plotted on a tornado diagram to provide a visual representation of the sensitivity of model results to input parameters.
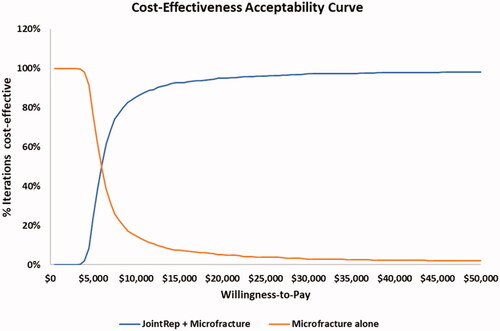
To understand the effect of uncertainty around all model inputs simultaneously, a probabilistic sensitivity analysis (PSA) was conducted with 1,000 simulations. In each simulation, a value was drawn for input parameters by random sampling based on their respective distributions. The choice of probability distribution was based on the type of parameter. Beta distribution was assigned to all probabilities and utility inputs, whereas a log-normal distribution was used for cost inputs.
Scenario analyses
Numerous scenario analyses were conducted by varying the model assumptions/settings. The following scenario analysis was conducted in this analysis:
Reducing the post-baseline utility of JointRep + Mircrofracture arm by 20%
Reducing the utility of JointRep + Mircrofracture arm by 30%
Reducing the utility of both treatment arms by 20%
Reducing the utility of both treatment arms by 30%
Varying the time horizon to 5 and 10 years
Varying the discount rate to 0% and 3.5%
Including the cost and disutility for one patient with TKA in JointRep + Microfracture arm
Varying the time horizon to 15 years. This scenario involved incorporating the following treatment failure options in the model:
Re-operation after primary treatment failure
TKA for patients undergoing re-operation post failure of initial intervention
Results
Base-case results
Over a 3-year time horizon, the mean total discounted cost per patient for JointRep with microfracture surgery was estimated to be $12,996 compared to $6,974 for microfracture surgery alone (). The total QALYs over 3 years were 2.61 and 1.66 for JointRep in combination with microfracture surgery and microfracture surgery alone, respectively.
Table 4. List of cost items and summary of cost impacts over 3 years included in the economic evaluation.
JointRep with microfracture surgery provided an incremental QALY gain of 0.95 compared to microfracture surgery alone, at an incremental cost of $6,022. JointRep with microfracture surgery was found to be cost-effective with an estimated incremental cost-effectiveness ratio (ICER) of $6,328 per QALY gained.
Sensitivity analyses
One-way sensitivity analyses
In one-way sensitivity analysis, model results were found to be most sensitive to utility values at 1 year, 2 years and 3 years after receiving either of the treatment, i.e. JointRep with microfracture surgery or microfracture surgery alone. The ICER never exceeded $8,000 in any sensitivity analyses conducted ().
Probabilistic sensitivity analyses
Probabilistic sensitivity analysis (PSA) confirmed the robustness of the base-case results. From 1,000 simulations, an average ICER of $6,293 was obtained, which was similar to the base-case ICER. At a willingness-to-pay threshold above $25,000 per QALY gain, JointRep with microfracture surgery would be 96% cost-effective compared to microfracture surgery alone ().
Scenario analyses
The model results were found to be substantially robust for the alternative model settings and assumptions. The results of scenario analyses for JointRep with microfracture surgery vs. microfracture surgery alone are presented in .
Discussion
Cost-effectiveness analysis is a comparative assessment of relative costs and health benefits of healthcare interventions, that can inform reimbursement decisions. This study evaluated the cost-effectiveness of a combination of JointRep with microfracture surgery compared to microfracture surgery alone, over a 3-year time horizon, and was conducted from the Australian healthcare system perspective. Although Health Technology Assessment (HTA) bodies in Australia (e.g. PBAC, MSAC or PLAC) do not recommend an explicit cost-effectiveness threshold in their respective guidelines or in their decision-making criteria, it has been observed that ICERs in the range of AU$45,000-AU$75,000 are usually considered cost-effectiveCitation36–39. The base-case analysis showed that JointRep with microfracture surgery led to an incremental QALY gain of 0.95, at an additional cost of $6,022 compared with microfracture surgery alone, resulting in an ICER of $6,328 per QALY gained. Hence, JointRep with microfracture surgery may be considered highly cost-effective compared to microfracture surgery alone.
No Australian published population-based series or studies identifying patients presenting with chondral defects in the Australian health system were identified. Three smaller, older studies from specific sub-populations (mostly private specialist knee surgeons’ practices) were identified and our study population, while being slightly older, is consistent with the populations from these studiesCitation40–42.
To the best of the author's knowledge, this is the first study that evaluates the cost-effectiveness of JointRep with microfracture surgery in the Australian setting. As a result, the study findings cannot be compared with any published literature. However, various factors contributed to strengthening the findings from the analysis. The analysis was developed based on the guidelines and methodologies for conducting economic evaluations recommended by MSAC, AustraliaCitation21. A key strength of this analysis is that it relied on observed clinical trial outcomes to inform the model effectiveness parameters for the base case analysis, albeit from a controlled but non-randomised trial. The time horizon for the base case analysis was restricted to 3 years based on the follow-up duration of the JointRep trial. This analysis can also be viewed as a trial-based economic evaluation; therefore, it does not have any uncertainties associated with the extrapolation of trial outcomes to a longer time horizon. However, the base case model setting of a 3-year time horizon is a conservative model setting since JointRep in conjunction with microfracture surgery may provide treatment benefits in terms of the reduced number of re-operation or TKAs which cannot be captured in a trial-based time horizon of 3 years. Therefore, a scenario analysis was also conducted with a longer time horizon of 15 years accounting for re-operations and TKAs based on published literature. Additionally, the trial used a validated tool to measure treatment effectiveness. The trial showed that JointRep with microfracture markedly improved the clinical symptoms of affected patients as seen in the markedly lower WOMAC sub-scores of the intervention group when compared to the control group. This was further reflected in our model as an improved quality of life for patients receiving JointRep. Lastly, our results were robust, as demonstrated by marginally varying estimates in sensitivity analysis and scenario analysis.
A major limitation of the present analysis was that the trial used as a source of efficacy inputs of the economic model was a small non-randomized post-marketing trial. However, the best available literature has been used, as it is the first and the only published trial evaluating JointRep. The results of our analysis can be regarded as preliminary evidence of the cost-effectiveness of JointRep with microfracture surgery as compared to microfracture alone treatment. To counteract the possible concern associated with the uncertainty of the efficacy outcome, several scenario analyses were conducted by reducing the utility by 20% and 30% in JointRep + Microfracture arm only, or in both arms of the model. A 30% reduction in both treatment arms did not have a considerable impact on the ICER and the highly conservative approach of selectively reducing the utility gain in only the JointRep + Microfracture arm by 30% (i.e. without any reduction in the utility of the microfracture arm) also resulted in a cost-effective ICER (∼$35,000). Another limitation of the trial was that it did not assess the long-term consequences of surgically treated osteochondral defects, such as re-operation. However, as part of a scenario analysis, long-term outcomes were incorporated based on conservative assumptions and the best available literature. Although inputs for the scenario analysis were based on independent literature, it is an acceptable approach in cases when direct estimates from clinical trials are not available. Moreover, sensitivity analysis showed that none of the parameters affected by trial limitations had a substantial effect on ICER.
Conclusions
JointRep with microfracture surgery may be a highly cost-effective treatment option compared to microfracture alone from the Australian health care system perspective and provides an improved quality of life outcomes for patients suffering from symptomatic focal osteochondral defects (Outerbridge Grade 3 or 4) of the knee, who had failed conservative treatment and were indicated for surgery. However, considering several limitations of the source trial, the cost-effectiveness evidence generated by this analysis should be considered preliminary, requiring further exploration based on large, randomized trials with longer follow-up duration.
Transparency
Declaration of funding
The study was funded by Device Technologies Australia Pty. Ltd and Oligo Medic Inc
Declaration of financial/other interests
Device Technologies Australia Pty Ltd and Oligo Medic Pty Ltd provided funding to conduct this study but had no role in the preparation of this article.
The Pipino 2018Citation9 trial was sponsored by Oligo Medic but otherwise independent of Oligo Medic. The extent of the sponsorship was only to provide the JointRep device used in the trial free of cost. The authors of the trial do not have any financial interest in JointRep or Oligo Medic.
Peer reviewers on this manuscript have received an honorarium from JME for their review work but have no other relevant financial relationships to disclose.
Author contributions
GP, SG, HR, and AG made significant contributions to the concept and study design. GP, SG, HR, AG, and BS helped with the data acquisition and data analysis. All authors contributed equally towards data interpretation, manuscript draft preparation and revision, and gave final approval for manuscript publication. All authors agree to be accountable for all aspects related to this study.
Previous presentations
None/Not Applicable
Acknowledgements
The authors thank Dr Allan J Wailoo and Dr Monica Hernandez Alava from Health Economics and Decision Science, School of Health and Related Research (ScHARR), University of Sheffield, Sheffield, UK for the re-estimation of the relationship between WOMAC and EQ5D-3L using the Australian tariffs.
References
- Gorbachova T, Melenevsky Y, Cohen M, et al. Osteochondral lesions of the knee: differentiating the most common entities at MRI. Radiographics. 2018;38(5):712–1495. 2018/09/01
- Wells D. Osteochondral Defect of the Knee [cited 2021 Sept 07]. Available from: https://www.atlasorthopaedics.com/osteochondral-defect-knee-orthopaedic-surgeon-woodstock-ga.html.
- Stanford Healthcare. Chondral/Osteochondral Defect [cited 2021 Sept 07]. Available from: https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/chondral-osteochondral-defect.html.
- Howell M, Liao Q, Gee CW. Surgical management of osteochondral defects of the knee: an educational review. Curr Rev Musculoskelet Med. 2021;14(1):60–66.
- Bruns J, Werner M, Habermann C. Osteochondritis dissecans: etiology, pathology, and imaging with a special focus on the knee joint. Cartilage. 2018;9(4):346–362.
- Gracitelli GC, Moraes VY, Franciozi CE, et al. Surgical interventions (microfracture, drilling, mosaicplasty, and allograft transplantation) for treating isolated cartilage defects of the knee in adults. Cochrane Database Syst Rev. 2016;9(9):Cd010675.
- Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757.
- Henn RF 3rd, Gomoll AH. A review of the evaluation and management of cartilage defects in the knee. Phys Sportsmed. 2011;39(1):101–107.
- Pipino G, Risitano S, Alviano F, et al. Microfractures and hydrogel scaffolds in the treatment of osteochondral knee defects: a clinical and histological evaluation. J Clin Orthop Trauma. 2019;10(1):67–75.
- Stanish WD, McCormack R, Forriol F, et al. Novel scaffold-based BST-CarGel treatment results in superior cartilage repair compared with microfracture in a randomized controlled trial. J Bone Joint Surg Am. 2013;95(18):1640–1650.
- Shive MS, Stanish WD, McCormack R, et al. BST-CarGel® treatment maintains cartilage repair superiority over microfracture at 5 years in a multicenter randomized controlled trial. Cartilage. 2015;6(2):62–72.
- MEDICWAVE. JOINTREP™ Cartilage Regeneration Technology [cited 2021 Sept 07]. Available from: https://medicwave.com.my/jointrep/.
- Methot S, Changoor A, Tran-Khanh N, et al. Osteochondral biopsy analysis demonstrates that BST-CarGel treatment improves structural and cellular characteristics of cartilage repair tissue compared with Microfracture. Cartilage. 2016;7(1):16–28.
- Fravel J, Shaffer M. Rehabilitation following microfracture surgery 2011. [cited 2021 Sept 07]. Available from: https://lermagazine.com/article/rehabilitation-following-microfracture-surgery.
- Australian Government Department of Health. Prostheses List [cited 2021 Sept 07]. Available from: https://www.health.gov.au/resources/publications/prostheses-list.
- Australian Government Department of Health. Prostheses cover under private health insurance [cited 2021 Sept 07]. Available from: https://www.health.gov.au/health-topics/private-health-insurance/what-private-health-insurance-covers/prostheses-cover-under-private-health-insurance?utm_source=health.gov.au&utm_medium=callout-auto-custom&utm_campaign=digital_transformation.
- Australian Government. Private Health Insurance Act 2007 [cited 2021 Sept 07]. Available from: https://www.legislation.gov.au/Details/C2019C00067.
- Australian Government Department of Health, Therapeutic Goods Administration. Australian regulatory guidelines for medical devices (ARGMD) [cited 2021 Sept 07]. Available from: https://www.tga.gov.au/publication/australian-regulatory-guidelines-medical-devices-argmd.
- Australian Government Department of Health. Prostheses List Advisory Committee (PLAC) [cited 2021 Sept 07]. Available from: https://www.health.gov.au/committees-and-groups/prostheses-list-advisory-committee-plac.
- Medina J, Garcia-Mansilla I, Fabricant PD, et al. Microfracture for the treatment of symptomatic cartilage lesions of the knee: a survey of international cartilage regeneration & joint preservation society. Cartilage. 2021;13(1_suppl):1148S–1155S.
- Medical Services Advisory Committee Australia. Technical Guidelines for preparing assessment reports for the Medical Services Advisory Committee – Service Type: Investigative (Version 3.0). [cited 2021 Sept 07]. Available from: http://www.msac.gov.au/internet/msac/publishing.nsf/Content/0BD63667C984FEEACA25801000123AD8/$File/InvestigativeTechnicalGuidelines-December-2016-Version-3.0.pdf.
- The Pharmaceutical Benefits Advisory Committee Australia. Guidelines for preparing a submission to the Pharmaceutical Benefits Advisory Committee (Version 5.0). [cited 2021 Sept 07]. Available from: https://pbac.pbs.gov.au/content/information/files/pbac-guidelines-version-5.pdf.
- Australian Bureau of Statistics. Life tables [cited 2021 Nov 20]. Available from: https://www.abs.gov.au/statistics/people/population/life-tables/2018-2020.
- Fang WH, Huang GS, Chang HF, et al. Gender differences between WOMAC index scores, health-related quality of life and physical performance in an elderly Taiwanese population with knee osteoarthritis. BMJ Open. 2015;5(9):e008542.
- Pipino G, Risitano S, Alviano F, et al. Patient level data analyses from: microfractures and hydrogel scaffolds in the treatment of osteochondral knee defects: a clinical and histological evaluation. J Clin Orthop Trauma. 2019;10(1):67–75.
- Wailoo A, Hernandez Alava M, Escobar Martinez A. Modelling the relationship between the WOMAC osteoarthritis index and EQ-5D. Health Qual Life Outcomes. 2014;12:37.
- Viney R, Norman R, Brazier J, et al. An Australian discrete choice experiment to value eq-5d health states. Health Econ. 2014;23(6):729–742.
- Viney R, Norman R, King MT, et al. Time trade-off derived EQ-5D weights for Australia. Value Health. 2011;14(6):928–936.
- Clemens S, Begum N, Harper C, et al. A comparison of EQ-5D-3L population norms in Queensland, Australia, estimated using utility value sets from Australia, the UK and USA. Qual Life Res. 2014;23(8):2375–2381.
- McCaffrey N, Kaambwa B, Currow DC, et al. Health-related quality of life measured using the EQ-5D-5L: South Australian Population Norms. Health Qual Life Outcomes. 2016;14(1):133.
- Mather RC, 3rd, Hug KT, Orlando LA, et al. Economic evaluation of access to musculoskeletal care: the case of waiting for total knee arthroplasty. BMC Musculoskelet Disord. 2014;15:22.
- Frappier J, Stanish W, Brittberg M, et al. Economic evaluation of BST-CarGel as an adjunct to microfracture vs microfracture alone in knee cartilage surgery. J Med Econ. 2014;17(4):266–278.
- IHPA. National Hospital Cost Data Collection Report, Public Sector, Round 23 (Financial year 2018–19) [cited 2021 Sept 07]. Available from: https://www.ihpa.gov.au/publications/national-hospital-cost-data-collection-report-public-sector-round-23-financial-year.
- IHPA. National Efficient Price Determination 2021–22 [cited 2021 Sept 07]. Available from: https://www.ihpa.gov.au/publications/national-efficient-price-determination-2021-22.
- Australian Government Department of Health. Medicare Benefits Schedule Handbook. November 2021 [cited 2021 Sept 07]. Available from: http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Downloads-211101.
- Australian Government Department of Health. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (PBAC) [cited 2021 Sept 07]. Available from: https://pbac.pbs.gov.au/.
- Australian Government Department of Health. Guidelines for preparing assessments for the MSAC [cited 2021 Sept 07]. Available from: http://www.msac.gov.au/internet/msac/publishing.nsf/Content/MSAC-Guidelines.
- Australian Government Department of Health. Prostheses List Guide [cited 2021 Sept 07]. Available from: https://www.health.gov.au/resources/publications/prostheses-list-guide.
- Pharmaceutical Benefits Scheme. OLAPARIB, 50 mg capsule, 4 x 112, Lynparza®, AstraZeneca Pty Ltd- Public Summary Document. March 2016. [cited 2021 Sept 07]. Available from: https://www.pbs.gov.au/industry/listing/elements/pbac-meetings/psd/2016-03/files/olaparib-psd-march-2016.pdf.
- Ebert JR, Fallon M, Zheng MH, et al. A randomized trial comparing accelerated and traditional approaches to postoperative weightbearing rehabilitation after matrix-induced autologous chondrocyte implantation: findings at 5 years. Am J Sports Med. 2012;40(7):1527–1537.
- Henderson IJ, Lavigne P. Periosteal autologous chondrocyte implantation for patellar chondral defect in patients with normal and abnormal patellar tracking. Knee. 2006;13(4):274–279.
- Henderson IJ, Tuy B, Connell D, et al. Prospective clinical study of autologous chondrocyte implantation and correlation with MRI at three and 12 months. J Bone Joint Surg Br. 2003;85(7):1060–1066.