Abstract
Objective
Accurate and up-to-date figures of the cost of community-acquired pneumonia (CAP) hospitalization are needed to understand the associated economic burden for public health decision-makers. Recent estimates are lacking, and previously published estimates differ markedly. Our objective was to estimate the current mean cost to the UK National Health Service (NHS) for adult hospitalized CAP.
Methods
All CAP hospitalizations in 2019 for those aged ≥18 years were identified from English Hospital Episode Statistics (HES). Each hospitalization was mapped to the tariff cost paid to the care provider within the NHS, including critical care costs and accounting for length of stay and complexity of the case. Mean hospitalization costs were estimated in total and in individuals with defined underlying comorbidities.
Results
A mean cost of £3,904 was estimated for 187,251 CAP admissions providing a total cost of approximately £731 million per annum. The mean cost was £3,402, excluding critical care costs, and £11,654 for critical care episodes in the 4.4% of admissions receiving this care. Groups at high risk of CAP had higher mean costs, ranging from £4,458 for people with diabetes to £5,215 for those with heart disease aged <65 years and £4,356 for those with heart disease to £4,751 for those with liver disease aged >65 years who comprised 74.3% of admissions overall.
Conclusion
This estimate of the cost of hospitalization for CAP from the total population and in those with certain underlying comorbidities will allow a valid understanding of the cost-benefit of vaccination and evidence-based prioritization of pneumococcal vaccination to those at highest risk.
PLAIN LANGUAGE SUMMARY
Community-acquired pneumonia (CAP) is a disease that is most commonly caused in England by the bacterium Streptococcus pneumoniae, which infects patients outside of a hospital. Patients who suffer from CAP often require hospitalization, which incurs a cost to the UK National Health Service (NHS). The goal of this study was to establish the annual cost of hospitalized CAP.
The researchers used England’s national healthcare database, known as Hospital Episodes Statistics (HES), to select all adults in England who were hospitalized for CAP in 2019. For the 187,251 patients hospitalized, an average cost of £3,904 per person was estimated, amounting to a total cost of £731 million per year to the NHS. Most people admitted to hospital with CAP were at risk for the disease (due to factors such as increased age or presence of another disease) and the cost of treatment for this subgroup was disproportionately larger than that for treatment of patients not at risk. Furthermore, while approximately 5% of patients admitted for CAP received critical care during treatment, the average cost for these patients was over £8,000 higher than for those outside this subsection.
The costs of hospitalization reported in this analysis were higher than previously estimated. The researchers highlighted weaknesses in other studies and limitations of the current study which could explain the difference. This work provides up-to-date figures for the cost of treating CAP in hospital in England. Public health decision-makers can use these estimates to determine the cost-benefit of vaccines that can help protect against important causes of CAP, particularly vaccines that target S. pneumoniae.
© 2022 Pfizer Ltd. Published by Informa UK Limited, trading as Taylor & Francis Group
Introduction
Community-acquired pneumonia (CAP) is a common acute infection with an increasing rate of hospitalization in England. Streptococcus pneumoniae is the most commonly identified etiologyCitation1 and has reported to be the pathogen responsible for the highest average annual respiratory admissions in England for people aged ≥65 yearsCitation2. Older adults and individuals with certain clinical conditions, such as chronic heart or lung disease, are at an increased risk of CAPCitation1,Citation3,Citation4. Intensive care admissions and death are both reported in approximately 8% of hospitalizations for CAP in England (2013–2018)Citation1, with pneumonia noted as a cause in 18,184 deaths in England in 2020Citation5. The clinical and economic burdens resulting from CAP hospitalization are therefore considerable.
An understanding of this economic burden is important, not least to allow analysis of the cost-effectiveness of pneumococcal vaccination. However, published estimates of the cost of CAP hospitalization in UK pneumococcal vaccine cost-effectiveness analyses vary considerably, between £661 and £1,218Citation6–8. By comparison, the tariff price paid to a care provider within the NHS internal market for the least complicated non-elective admission for pneumonia was £1,836 in 2019/20 (healthcare resource group [HRG] code: DZ11V)Citation9 and an analysis of the cost of admission for “pneumonia with an unspecified organism” has been estimated as £3,256Citation10.
There are valid reasons why estimates of cost for CAP admission may vary including different methodologies, and updated prices and costing methods. However, these differences, along with uplifting to account for inflation, are unlikely to account for the scale of the disparity.
The objective of this study was to address the uncertainty in the cost of CAP hospitalization for adults in England by providing a current estimate based on Hospital Episode Statistics (HES) linked to tariff prices, which is the cost paid by the NHS.
Methods
Data source
This retrospective observational analysis of a cohort of patients admitted for CAP in the calendar year 2019 was based on HES and critical care datasets provided by NHS Digital. HES is a data warehouse which contains information for all admissions, accident and emergency (A&E) attendances, and outpatient appointments at NHS hospitals in England and at treatment centers funded by the NHSCitation11,Citation12. The calendar year 2019 was chosen as this was not affected by the COVID-19 pandemic.
The HES Admitted Patient Care (APC) file includes HRGs, admission dates, length of stay, completed consultant episodes within the overall admission spell, and current diagnoses (10th International Classification of Diseases [ICD‐10]Citation13) and procedures (Office of Population Censuses and Surveys (OPCS)-4.9 for proceduresCitation14) for inpatient admissions. Elective and non-elective admissions and critical care unit stays are flagged. On discharge, the NHS allocates the most relevant HRG code to the admission based on a combination of procedure and diagnostic codes, including comorbiditiesCitation12. HRGs are clinically meaningful groups of diagnoses and interventions that consume similar levels of NHS resources. Therefore, the HRG can reflect the complexity of the case and the most resource-intensive activity occurring within an admission rather than the initial diagnosis. The HRG code is converted into a cost, accounting for length of stay, using the national tariff cost paid to the care provider within the NHS internal systemCitation12. The dataset used in the study was the final release of HES data for financial years 2018 and 2019, the conversion of procedure and diagnostic codes to HRGs used HRG 4+ grouper software (National Casemix Office, Winchester, UK).
The HES outpatient file includes HRGs which account for first, follow-up single or multi-professional visits, and, separately, outpatient procedures. The HES A&E file includes HRGs for each attendance. The Critical Care Dataset is linked to the APC file and provides the level of care delivered and the number of bed days. Each record includes a patient identifier which links activity across care settings preventing double counting of patients. No ethics approval was required for the study as it was based on anonymous secondary data.
Study population
The study population comprised all patients in England with at least one non-elective inpatient admission with pneumonia recorded as a primary diagnosis position one (reason for admission) in the HES APC during 2019 for patients ≥18 years on admission date (study admission). Every admission was included into the study including patients who were admitted on more than one occasion during the study year. Pneumonia was defined as an ICD-10 code J12 to J18 (see Supplementary Table S1 for all ICD-10 code lists). Each study admission during 2019 was analyzed separately. Admissions which may have been hospital-acquired pneumonia were excluded (a prior admission (elective or non-elective) with discharge <28 days prior to the study admission date (N = 84,228), or a record of “nosocomial condition” (ICD-10 Y95) during the study admission (N = 47,270)).
Costs
Costs were derived from the HES dataset by mapping HRGs to an appropriate national tariff (APC, A&E, or outpatient) corresponding to the activity year (i.e. activity in 2018/2019 used tariff 2018/2019, activity in 2019/2020 used tariff in 2019/2020) and applying the appropriate market forces factor to account for regional variation in costsCitation9,Citation12. APC HRGs were mapped allowing for the activity type (elective, day case, and non-elective) with extra cost included for excess bed days, and complications and comorbidities as specified by the tariff. Outpatient attendance and procedure, and A&E HRGs were mapped directly to the appropriate tariff. Critical care activity is funded separately so the cost was obtained through the 2018/2019 Reference Costs Grouper using “CCU01 non-specific, general adult critical care” and a “reported level of care” which allows for increasing costs with a greater number of organs supported.
The primary analyses were completed for the total study population and after stratification by age <65 years or ≥65 years. Age was defined as that on the admission date throughout the analyses. The number of admissions and those with a critical care spell or receiving assisted ventilation at any time during admission were estimated. Average total costs for study admissions were estimated (including HES and critical care activity) from admission date to discharge date on the APC file and, separately, for all activity for a further 30, 60, or 90 days to account for resource use after discharge. The average cost and length of stay were estimated for admissions with and without an episode of critical care. The number of admissions with a critical care episode was estimated and broken down into the number of days spent in critical care (bed days) and the total length of stay in hospital.
The calculation of total costs was repeated for three separate sets of groupings: study admissions with pneumococcal pneumonia; in those aged 65–74 years, 75–84 years, and ≥85 years; and for first study admission in those with a history of chronic comorbidities. Pneumococcal pneumonia was defined as an entry for ICD-10 code J13 (Streptococcus pneumoniae) in any position, or ICD-10 code B953 (Streptococcus pneumoniae as the cause of diseases classified elsewhere) in position 2, on HES APC for the study admission. The comorbidities included were based on those in previous hospitalized CAP cost estimate analyses but excluding immunocompromised patients which cannot reliably be identified from HES data. The comorbidities were respiratory disease, heart disease, kidney disease, liver disease, and diabetes mellitus identified by an ICD-10 code recorded in the HES APC, outpatient, or A&E file at any time before or during the first study admission. The comorbidity code lists replicated those in Rozenbaum et al.Citation6 and van Hoek et al.Citation7 (Supplementary Table S1). However, these studies included pediatric ICD-10 codes, while the current study only included adults. We therefore ran the main analyses with and without these codes.
Results
During 2019, there were 187,251 admissions for CAP in 177,865 people, 74.3% of admissions were in those ≥65 years (). The mean cost for the CAP hospital admission only was £3,904, increasing to £5,813 when all secondary care costs in the 90 days after discharge were included. The HRG most frequently assigned was DZ11V (lobar, atypical or viral pneumonia, without interventions, with CC [comorbidity and complexity] score 0–3) in 36,532 (19.5%) of study admissions, followed by DZ11U (lobar, atypical or viral pneumonia, without interventions, with CC score 4–6) in 36,526 (19.5%) of admissions (Supplementary Table S2). There was a critical care episode in 4.4% of admissions overall and in 7.4% in those aged <65 years. The mean costs were £3,402 for admissions when critical care episodes were excluded and £11,654 for critical care costs alone. There was a record of pneumococcal pneumonia in 3,572 (1.9%) of admissions, 45.1% of which were in people aged <65 years with a mean cost of £6,574 across all groups (). Most people with an admission had one or more comorbidity, 51.4% in those <65 years and 78.3% in those aged ≥65 years. Among the subgroup with comorbidities admission costs were higher in those aged <65 years than in older adults (). In general costs increased with increasing age and were higher than the overall mean in people with either pneumococcal infections or any comorbid conditions (). Costs increased until 75 years of age, although length of stay continued to increase ().
Figure 1. Average cost of CAP hospitalization stratified by age, a diagnosis of pneumococcal pneumonia, and by comorbidity.
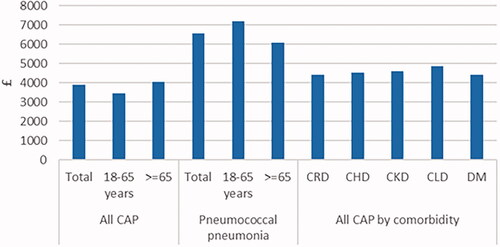
Table 1. Number, critical care, cost, and length of stay of admissions for CAP by age group.
Table 2. Number, cost, and length of stay of admissions for CAP specified as pneumococcal pneumonia by age group.
Table 3. Number and cost of admissions for CAP in people with chronic comorbidities by age group.
Table 4. Number, cost, and length of stay of admissions for CAP in older people.
Review of the data identified a positively skewed distribution of costs per admission and six outliers, each with a total cost of >£200,000. The mean total cost of £3,890 for the admission alone without outliers was estimated for the total population in a post-hoc analysis (see Supplementary Table S3). A sensitivity analysis repeated the comorbidity analysis after removing the pediatric ICD-10 codes included in previous analyses (Supplementary Table S4).
Discussion
This large study of all 187,251 hospital admissions for CAP in England in 2019 provides a mean cost to the NHS of £3,904. The total cost of hospitalized CAP in England can therefore be estimated as approximately £731 million per annum in 2019 figures. While the proportion of patients who received critical care was small, these episodes increased the overall mean cost of admission by approximately 15% which had a greater impact on the admission costs for those aged <65 years, who were more frequently admitted to critical care (7.4%) compared to all adults (4.4%). Admission costs were higher in at risk populations, including both older people and those with comorbid conditions. Costs increased with age generally, being higher in 65–74-year-olds than in those <65 years. The majority of the study population had at least one chronic comorbidity including approximately 50% of people aged 18–64 years. The higher admission costs in those with chronic comorbidities, as well as that in pneumococcal pneumonia, will partly be the result of higher costs allowed for in these groups within the NHS tariff. The costs in those with a diagnosis of pneumococcal pneumonia may also be biased upwards if the causal organism is more likely to be identified in more severe, complicated, or resistant disease. The proportion with pneumococcal pneumonia (1.9%) is low compared to 37% of admissions for CAP when more routine screening for pneumococcal pneumonia is in placeCitation1 suggesting under ascertainment.
The higher risk of hospitalization for CAP in individuals with chronic comorbidities is consistent with previous reportsCitation4,Citation15. A smaller proportion of <65s in the current study may account for the slightly fewer CAP admissions receiving critical care than reported elsewhere (4.4% compared to 5.2% or 7.7%)Citation1,Citation16, as the number of critical care stays decrease with age. When time periods after discharge are included costs increase, even in the young, suggesting that the total cost for CAP is greater than that due to the primary admission. This may be partially explained by previous findings that, in people with chronic comorbidities, there is both an increased risk of CAP hospitalization and that hospital admissions increased after CAPCitation4,Citation17,Citation18. In addition, high rates, and an increased risk, of cardiac disease are reported in the short-term after CAP hospitalizationCitation19,Citation20.
Our estimate of the cost of CAP admissions is considerably higher than the previous estimates in pneumococcal vaccine cost-effectiveness analyses which ranged from £661 to £1,218. In 2012, Rozenbaum et al.Citation6 estimated a mean cost of pneumonia admission of £661 in people at increased risk of invasive pneumococcal disease using the HRG code uncomplicated DZ11C (lobar, atypical, or viral pneumonia) and based on 2009–2010 NHS reference costs. This estimate of £661 was subsequently adjusted for inflation to £715 (to 2014 prices) in a 2016 cost-effectiveness analyses by van Hoek and MillerCitation8 in immunocompetent people aged 65 years and older. Further inflation of the £715 estimate to the 2019 costs used in the current study would provide a figure of £789 based on the Hospital and Community Health Services Index pay and prices percentage increase (see Supplementary Table S5)Citation21. To help illustrate the methodological discrepancy an unrelated estimate provided for infants by van Hoek in 2012 used the same HRG code: DZ11C combined with the cost per bed day and length of stay of about 4 days to provide a cost of CAP of £1,218 based on 2008/2009 NHS reference costs. This example, when adjusted for inflation to 2019 levels, works out to be £1,454Citation7. There are several non-inflationary reasons for the difference between our current estimates and these previous studies. The previous studies assumed that all hospitalized CAP was appropriately represented by uncomplicated lobar, atypical or viral pneumonia (HRG code DZ11C, the lowest complexity level available at that time) while the current study includes all complication and comorbidity scores, interventions (multiple, single, and without), and added critical care costs. In practice, only a fifth of study admissions were costed using the lowest complexity level pneumonia HRG code available. Focusing on the lowest complexity levels does not capture the higher resource use and costs associated with patients with more complications and comorbidities resulting in an underestimation. In addition, in all three previous studies, the estimated cost of hospitalized CAP applied in the cost-effectiveness analysis was a cost per admission (or spell) despite the unit of measure in the NHS reference costs at the time being cost per finished consultant episode (FCE)Citation22,Citation23. This further underestimates the cost per admission since there can be more than one FCE in a spell. For example, van Hoek and MillerCitation8 used a mean length of stay of 4 days based on reference costs per FCE for uncomplicated cases, whereas the current study estimated a mean length of an admission of 7 days based on HES data. Conversion of the estimates from cost per FCE to cost per spell would have required adjustment with either the number of FCEs or the length of stay for a spell. NHS reference costs in 2013/2014 (the date of the van Hoek and MillerCitation8 analysis) did report both cost per FCE and cost per spellCitation24,Citation25. Finally, our study included all CAP admissions throughout the year and did not exclude patients who had multiple admissions. We recognize that there is the potential for those patients who were admitted more than once to have higher costs compared to those attending hospital once. This, however, only applied to 5% of the dataset so the potential to skew the overall mean cost would be minimal and it is important to provide a complete datasheet. Our new hospitalization costs provide a current and robust estimate for the actual inpatient healthcare costs paid to hospitals in England for patients that were treated for pneumonia in 2019. This cost data will be valuable for future cost effectiveness analyses for potential future interventions, including adult pneumococcal vaccines. These costs, however, need to be inflated when used in further analyses. We have left this to researchers conducting further analyses to allow for a more straightforward adjustment when the appropriate year and percentage inflation will be known. Cost effectiveness analyses for interventions that target causes of adult CAP in the UK generally only consider hospitalization costs, which provided the rationale this study, however further costs are incurred by the NHS within primary care. Further work analyzing primary care costs is needed to provide an estimate for the total cost to the NHS for pneumonia in England. Furthermore, cost estimates for other diseases related to CAP such as IPD would help strengthen future, specific cost effectiveness analyses.
The strengths of the current analysis are the almost universal coverage of secondary care activity in EnglandCitation26. All adult hospitalizations for CAP were included, as well as subgroups and critical care stays. In addition, the reported costs reflect the actual money paid by the Department of Health and Social Care to healthcare providers who treat hospitalized CAP, including critical care costs. Increased costs for more complex admissions are taken into account. As the study was based on the secondary source data HES, it was limited to the data routinely collected. CAP is not specifically coded and was deduced using several variables. Misclassification of pneumonia as a primary diagnosis code has been reported against a case definition which required a chest X-rayCitation16,Citation27. This misclassification will include lower respiratory tract infections, such as CAP or COPD, with no radiology workup and may be biased toward older age groupsCitation27. Some cases of hospital-acquired pneumonia may remain despite exclusion of records with a code for nosocomial disease or recent previous admission. Similarly, CAP diagnosis during a hospitalization for other illness or procedures and readmissions within 28 days may be missed but the use of ICD-10 code Y95 will have minimized this and excluded the majority of cases of hospital acquired pneumonia. Furthermore, in the rare scenario whereby patients were admitted for a new spell of hospitalized CAP between days 29 and 90 post-discharge there would have been double-counting of the spend for these patients. Severity could not be studied as pneumonia severity index or CURB scores are not available in HES. The study data source does not lend itself to a multivariate analysis exploring cost predictors such as age and comorbidities as the costs derived from HRGs are influenced by these variables to some extent. However, such an analysis would provide valuable further insight on the cost of CAP and could form the basis of a subsequent bespoke study.
Conclusions
This analysis provides a contemporary estimate of the cost of hospitalization to the NHS for CAP from the total population and in certain high-risk subgroups. Such estimates are essential to allow a valid understanding of the cost-benefit of vaccination and therefore to inform national vaccine policy of new and existing immunizations that target causes of pneumonia. Information on subgroups allows appropriate, evidence-based, prioritization of pneumococcal vaccination to those at highest risk.
Transparency
Declaration of funding
This study was funded by Pfizer Ltd, UK. Editorial support was provided by Elizabeth Jennings, Lucid Group and was funded by Pfizer Ltd, UK.
Declaration of financial/other interests
JC, HW, TM, AV, DM, GE are employees of Pfizer Ltd, UK, and hold stock or stock options. MS has received personal fees from GlaxoSmithKline, Pfizer, Merck, AstraZeneca, and Sanofi Pasteur as a speaker at international meetings and as a member of advisory boards and is currently undertaking contract work for Pfizer. GH received payment from Open Health for her contribution to the current study and has received funding for research and scientific consultancy from several pharmaceutical and healthcare companies outside the submitted work.
All reviewers on this manuscript have received an honorarium from JME for their review work. A reviewer on this manuscript has disclosed that they are a consultant for Merk and their institution has received research funding from Seres Therapeutics. The other reviewers have no conflicts of interest.
Supplemental Material
Download MS Word (113.6 KB)Acknowledgements
Dave Heaton provided advice on the HES dataset and data analysis, and Matthew O’Connell for data analysis. Hospital Episode Statistics (HES) Data were re-used with the permission of NHS Digital via Harvey Walsh, Open Health Group.
References
- Pick H, Daniel P, Rodrigo C, et al. Pneumococcal serotype trends, surveillance and risk factors in UK adult pneumonia, 2013–18. Thorax. 2020;75(1):38–49.
- Sharp A, Minaji M, Panagiotopoulos N, et al. Estimating the burden of adult hospital admissions due to RSV and other respiratory pathogens in England. Influenza Other Respir Viruses. 2021;16(1):125–131.
- Rodrigo C, Bewick T, Sheppard C, et al. Impact of infant 13-valent pneumococcal conjugate vaccine on serotypes in adult pneumonia. Eur Respir J. 2015;45(6):1632–1641.
- Campling J, Jones D, Chalmers JD, et al. The impact of certain underlying comorbidities on the risk of developing hospitalised pneumonia in England. Pneumonia (Nathan). 2019;11(1):4.
- Office for National Statistics. Deaths due to pneumonia; 2020. Available from: https://www.ons.gov.uk/search?q=pneumonia%20statistics.
- Rozenbaum MH, van Hoek AJ, Fleming D, et al. Vaccination of risk groups in England using the 13 valent pneumococcal conjugate vaccine: economic analysis. BMJ. 2012;345:e6879.
- van Hoek AJ, Choi YH, Trotter C, et al. The cost-effectiveness of a 13-valent pneumococcal conjugate vaccination for infants in England. Vaccine. 2012;30(50):7205–7213.
- van Hoek AJ, Miller E. Cost-Effectiveness of vaccinating immunocompetent ≥65 year olds with the 13-valent pneumococcal conjugate vaccine in England. PLOS One. 2016;11(2):e0149540.
- NHS. National tariff payment system: national prices and prices for emergency care services. 2019. Available from: https://www.england.nhs.uk/publication/national-tariff-payment-system-documents-annexes-and-supporting-documents/.
- Jones D, Campling J, Ellsbury G, et al. Establishing the cost of hospitalised community acquired pneumonia (CAP): a hospital episode statistics (HES) analysis. Thorax. 2017;72(S3):A116.
- NHS Digital. Hospital episode statistics (HES); 2021. Available from: https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics.
- Department of Health Payment by Results Team. A simple guide to payment by results. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213150/PbR-Simple-Guide-FINAL.pdf.
- World Health Organisation. International statistical classification of diseases and health problems ICD-102016; 2021. Available from: https://www.who.int/standards/classifications/classification-of-diseases.
- Office of Population Censuses and Surveys. OPCS-4 classification of interventions and procedures; 2022. Available from: https://datadictionary.nhs.uk/supporting_information/opcs_classification_of_interventions_and_procedures.html.
- Grant LR, Slack MPE, Yan Q, et al. The epidemiologic and biologic basis for classifying older age as a high-risk, immunocompromising condition for pneumococcal vaccine policy. Expert Rev Vaccines. 2021;20(6):691–615.
- British Thoracic Society. National audit report: adult community acquired pneumonia audit 2018–2019 national audit period: 1 December 2018 – 31 January 2019; 2019. https://www.brit-thoracic.org.uk/document-library/quality-improvement/audit-reports/adult-community-acquired-pneumonia-201819/.
- Campling J, Jones D, Chalmers J, et al. Clinical and financial burden of hospitalised community-acquired pneumonia in patients with selected underlying comorbidities in England. BMJ Open Resp Res. 2020;7(1):e000703.
- Park CM, Kim W, Rhim HC, et al. Frailty and hospitalization-associated disability after pneumonia: a prospective cohort study. BMC Geriatr. 2021;21(1):111.
- Bartlett B, Ludewick HP, Lee S, et al. Cardiovascular complications following pneumonia: focus on pneumococcus and heart failure. Curr Opin Cardiol. 2019;34(2):233–239.
- Corrales-Medina VF, Alvarez KN, Weissfeld LA, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313(3):264–274.
- Personal Social Services Research Unit. Unit costs of health and social care; 2022. Available from: https://www.pssru.ac.uk/project-pages/unit-costs/.
- Department of Health and Social Care. National schedule of reference costs 2008–09 for NHS Trusts; 2010. Available from: http://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/dh_111607.xls.
- Department of Health and Social Care. National schedule of reference costs 2009–10 for NHS Trusts; 2011. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216308/dh_123455.xls.
- Department of Health and Social Care. National schedule of reference costs - year 2013–14 – NHS Trusts and NHS Foundation Trusts (FCE); 2014. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/397469/03a_2013-14_National_Schedule_-_CF-NET_updated.xls.
- Department of Health and Social Care. Spell level data: national schedule of reference costs 2013–14 data for NHS Trusts and NHS Foundation Trusts; 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/380038/03b_2013-14_National_Schedule_-_Spells.xls.
- Herbert A, Wijlaars L, Zylbersztejn A, et al. Data resource profile: hospital episode statistics admitted patient care (HES APC). Int J Epidemiol. 2017;46(4):1093–1093.
- Daniel P, Bewick T, Welham S, et al. Adults miscoded and misdiagnosed as having pneumonia: results from the British Thoracic Society pneumonia audit. Thorax. 2017;72(4):376–379.
