Abstract
Aims
Advanced energy devices are commonly used in electrosurgery, including ultrasonic and advanced bipolar (ABP) devices. Smoke evacuation and reusable dispersive electrodes are also utilized during electrosurgery to improve staff and patient safety. This study assessed the budget impact of adopting a portfolio of Ethicon energy devices compared to devices from other manufacturers from a Spanish hospital perspective.
Methods
The main analysis compared the Ethicon advanced energy device portfolio (ultrasonic and ABP devices) to Non-Ethicon advanced energy devices. It was assumed that 4,000 procedures using one advanced energy device each were performed annually, and the cost impact of operating room time, length of stay, and transfusions were considered. A probabilistic budget impact analysis with 10,000 iterations was conducted for generalizability to other hospitals in Spain and Europe. Secondary analysis assessed whether cost savings from the Ethicon advanced energy device portfolio could offset costs of adopting smoke evacuation and reusable dispersive electrodes (Full Ethicon energy portfolio).
Results
In the main analysis, the annual budget impact of introducing the Ethicon advanced energy device portfolio was cost saving in 79.8% of probabilistic iterations (mean: -€945,214; 95% credible interval [CrI]: -€3,242,710; €1,285,942) with a mean budget impact per procedure of -€236 (95% CrI: -€811; €321). In the secondary analysis, adding smoke evacuation and reusable dispersive electrodes was still cost saving in 75.3% of iterations compared to Non-Ethicon advanced energy devices (mean: -€778,208; 95% CrI: -€3,075,086; €1,464,728) with a mean budget impact per procedure of -€97 (95% CrI: -€384; €183). Savings resulted from differences in operating room time, length of hospital stay, and volume of disposable electrodes.
Conclusions
Adopting Ethicon advanced energy devices demonstrated economic benefits compared to non-Ethicon devices. Introducing the advanced portfolio may improve surgical care quality and the full portfolio was cost saving while improving OR safety for staff and patients.
PLAIN LANGUAGE SUMMARY
This study created an economic model to calculate whether using modern electrical surgical tools with features to make cutting tissue and stopping bleeding faster and easier could save Spanish hospitals money. The electrical surgery tools from one manufacturer were compared to those from various other companies. Differences in how long surgery took to perform, how long patients stayed in hospital after their surgery, and how many blood transfusions they needed were considered in the model. The model was tested 10,000 times with random changes in the costs and settings used to be surer about the range of possible results. The results showed the devices from one manufacturer could save a Spanish hospital money in almost 80% of model runs and that savings worked out to €236 per surgery. In another analysis, savings were enough to cover the cost of introducing safety devices to remove surgical smoke from the operating room and reusable patient grounding electrodes that prevent some injuries potentially caused by small sticky electrodes. In conclusion, the model showed that Spanish hospitals may be able to save money by switching to the modern electrical surgery tools from Ethicon.
Introduction
Healthcare decision-makers are faced with increasingly complex decisions regarding improvements to operating room efficiencies while reducing complications and delivering high-quality surgical care. One frequent surgical complication is bleedingCitation1, which has been associated with longer length of hospital stay (LOS)Citation2 and operating room (OR) timeCitation3. Longer OR time has been associated with increased risk of complicationsCitation4, which is further associated with a protracted LOSCitation5. The adoption of devices that improve clinical outcomes could reduce healthcare resource utilization and provide economic savings to hospitals.
Advanced energy devices are electrosurgical devices designed to improve surgical outcomes. Ultrasonic and advanced bipolar (ABP) devices have been grouped together in the literature as advanced energy devices, characterized by their technological advancements and similar use casesCitation6–9. Both ABP and ultrasonic devices are designed to coagulate tissue causing hemostasisCitation9. ABP devices are specialized for sealing vessels up to 7 mm (examples include ENSEAL™ and LigaSure™) and ultrasonic devices are designed for fast cutting and dissection (examples include HARMONIC™ and Sonicision™)Citation9. These devices are important as they markedly reduce operating time compared to conventional techniques such as monopolar or basic bipolar electrosurgery, or clamp, cut, and tieCitation6. Ultrasonic devices convert electrical energy into high-frequency mechanical vibrations at 55 KHz that disrupt tissue hydrogen bonds and cause coagulation and sealing of vessels up to 5 mm in diameter, while cutting and dissecting tissueCitation6,Citation9. ABP devices have a mechanism to maximize compression uniformly over the target area, intelligent sensors that continuously adjust the voltage and current to achieve the desired effect, and have an integrated cutting bladeCitation6,Citation8,Citation9. ABP devices work by clamping tissue between the jaws of the device and applying high-current, low-voltage radiofrequency energy that denatures collagen and elastin in vessel wallsCitation6. Tissue impedance sensors automatically adjust the electrical energy delivered to the tissue to ensure optimal sealingCitation6. Once the clamped tissue is sealed, the user can extend the integrated blade to cut the tissue held between the device jawsCitation9. The commercially available ABP and ultrasonic devices have minor differences in design and size but the main features that define the devices are present in the respective offerings from all manufacturers. Additionally, device costs are very similar between Ethicon and to those from other manufacturers.
Hospitals are also concerned about OR safety. The application of energy devices to heat and cut tissue can produce surgical smoke, which is a potential hazard to operating room staffCitation10,Citation11. This gaseous byproduct can be absorbed through the skin, lungs, and eyes of the surgical staff and may result in symptoms such as nausea, headache, weakness, and dizziness, among othersCitation11. Many organizations have guidelines recommending the use of smoke evacuation systems during electrosurgery procedures to reduce the risk of staff exposure to surgical smokeCitation11–14. A smoke evacuator is a hand-held or trocar-compatible device that allows for the removal of surgical smoke when connected to a smoke evacuation system that filters the smoke particles from the air drawn in by the device. One element to improve patient safety in the OR during electrosurgery is through the use of non-adhesive reusable dispersive patient return electrodes, which reduce the risk of pad site burns compared to adhesive dispersive electrodesCitation15. The large surface area of a reusable capacitive patient return electrode limits the current density at the site of contact thus preventing increases in temperature that could lead to burns, which can occur when smaller adhesive electrodes lose contact with the patient’s skinCitation15. Another benefit of dispersive electrode pads is their reusability, which can help reduce OR waste compared to using disposable dispersive electrodes.
An advanced portfolio (includes ABP and ultrasonic advanced energy devices) and a full portfolio (includes ABP, ultrasonic, smoke evacuation, and reusable dispersive patient return electrodes) of energy devices has been developed by Ethicon. The objective of this study was to estimate a Spanish hospital’s budget impact over a one-year time horizon when using the Ethicon advanced energy device portfolio (includes ENSEAL™ and HARMONIC™) compared to Non-Ethicon advanced energy devices (includes ABP and ultrasonic devices from Non-Ethicon manufacturers). Previous studies have assessed the comparative efficacy of Ethicon and Non-Ethicon advanced energy devices in terms of OR time, LOS, and bleeding, among other metricsCitation16–21. This study also estimated the potential for cost savings due to the Ethicon advanced energy device portfolio being able to cover the cost of incorporating smoke evacuation and reusable dispersive patient return electrodes (MEDAGYNE™ smoke evacuation and MEGADYNE™ MEGA SOFT™ Universal Plus families of devices). The budget impact model (BIM) was informed by peer-reviewed clinical studies in five surgical specialties. Probabilistic analyses were conducted to account for comparative efficacy parameter uncertainty and to support generalizability to the broader European continent where hospital costs may differ compared to Spain. To the authors’ knowledge, this analysis represents the first to model the adoption of an entire portfolio of advanced energy devices in a European hospital setting.
Methods
Model Overview and main analysis
This BIM was developed to estimate a hospital’s budget impact when using the Ethicon advanced energy device portfolio compared to Non-Ethicon advanced energy devices from a hospital perspective over a 1-year time horizon. Discounting was not applied in light of the time horizon. This budget impact analysis was modelled for a hospital in Spain assuming 4,000 procedures were performed annually using advanced energy devices equally among colorectal, bariatric, gynecology, thoracic, and general surgery specialties (i.e. 800 procedures per specialty), with one device used per procedure. The main analysis is illustrated in . Procedure volume inputs were based on Spanish hospital data from Andalusia where, on average, hospitals performed 9,292 procedures per year from 2016–2020Citation22,Citation23. Of these 9,292 procedures, about 80% would involve electrosurgical devices (either basic or advanced energy). For this analysis it was assumed that half of the procedures using electrosurgery devices would be conducted with advanced energy devices for 4,000 procedures in total. This input reflects typical procedure volumes at an average Spanish hospital.
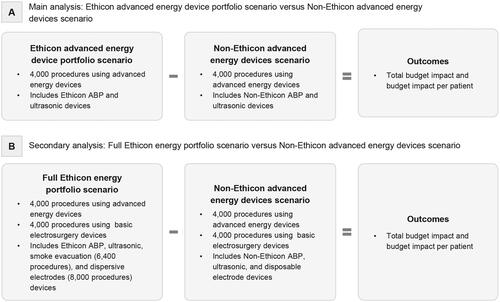
Figure 1. Schematic of budget impact analyses for the (a) main analysis, and for the (b) secondary analysis. For the main analysis, there are no non-advanced energy device differences between the scenarios. For the secondary analysis, basic electrosurgery procedures refers to the use of basic monopolar and bipolar energy devices. ABP: advanced bipolar.
Assumptions
For gynecology, thoracic, and general surgery procedures, it was assumed that half of the procedures used ABP devices and the other half used ultrasonic devices. For colorectal and bariatric procedures, it was assumed that all procedures used ultrasonic devices, since there was inadequate comparative evidence for the use of ABP procured from Ethicon versus other manufacturers in these surgical specialties. It was assumed that all procedures were conducted in eight ORs. The number of ORs used was based on Andalusian hospital data where hospitals have 14 ORs on averageCitation23,Citation24. Thus, the assumption that the procedures were performed in eight ORs is conservative when considering the capacity of an average Spanish hospital.
For the Non-Ethicon advanced energy devices scenario and the Ethicon advanced energy device portfolio scenario, it was assumed that the hospital was using disposable dispersive patient return electrodes and conventional smoke mitigation strategies without smoke evacuation, such as masks and ventilation.
Secondary Analysis
In a secondary analysis, it was assessed whether cost savings from the Ethicon advanced energy device portfolio could offset the cost of including smoke evacuation and reusable dispersive electrodes (Full Ethicon energy portfolio). Smoke evacuation and reusable dispersive electrodes can be used in procedures with basic energy devices in addition to those with advanced energy devices. It was assumed that procedures using advanced energy devices represent 50% of all electrosurgery procedures performed, thus the smoke evacuation and reusable dispersive electrodes could be used in 4,000 procedures with basic energy devices in addition to the 4,000 procedures requiring advanced energy devices (8,000 total procedures). One reusable dispersive patient return electrode was used per OR in all 8,000 annual electrosurgery procedures, and smoke evacuation was used in 80% of the 8,000 annual electrosurgery procedures based on recommendations from the Association of periOperative Registered Nurses (AORN)Citation25. This analysis is illustrated in .
Comparative Efficacy
The comparative efficacy of advanced energy devices sourced from Ethicon versus other manufacturers was based on a previously published systematic literature review and network meta-analysis (NMA) of randomized or observational studiesCitation16. The model inputs sourced from the systematic review and NMA are included in Supplementary Appendix A. The systematic review was performed to identify comparative studies of electrosurgery techniques and conventional techniques across several surgical specialties including general surgery, gynecology, thoracic, bariatric, and colorectal procedures. All studies included were on adult human patients and compared different advanced energy devices to each other (e.g. Harmonic™, Sonicision™, LigaSure™, Enseal™, and Thunderbeat™) or to conventional techniques such as bipolar or monopolar electrosurgeryCitation16. Study designs included were RCTs, and both retrospective and prospective observational studies from all regionsCitation16. Studies were excluded if they compared two different surgeries or approaches, combined advanced energy device use with another device, or were conference abstracts or narrative reviewsCitation16.
Studies were screened in duplicate at title and abstract and full-text stages. Data were extracted by one reviewer and checked for accuracy and completeness by another reviewer. Once extracted, network meta-analyses were performed based on data availability for RCTs only or RCT plus observational studiesCitation16. RCTs were used to inform comparative efficacy when advanced energy devices were directly compared in a study from the specialty of focus. The aim of the network meta-analyses was to compute indirect effect estimates via a common comparator (such as monopolar electrosurgery) for two advanced energy comparators that had not been compared directly in a clinical studyCitation16. NMAs were used for all outcomes for both general surgery and gynecology procedures comparing Enseal™ advanced bipolar (ABP) devices to competitors ABP devices, as well as all outcomes for thoracic procedures comparing Harmonic™ ultrasonic devices to competitors devicesCitation16. NMAs were performed using the NetMetaXL platform to run the Bayesian analysesCitation26.
As previously reported, a targeted literature review did not find comparative efficacy data for disposable versus reusable dispersive patient return electrodes or for conventional smoke mitigation versus smoke evacuationCitation16, hence potential differences in the efficacy of these devices were not included in the analyses and only cost differences were included.
Costs
Costs associated with healthcare resource utilization were obtained from multiple publicly available Spanish sources that align with the modelled hospital setting and inflated to 2021 Euros (Supplementary Appendix A). Costs associated with the devices used in each scenario were obtained using Spain-specific data when available. The advanced energy device costs used in the BIM are presented in Supplementary Appendix A. Costs for dispersive patient return electrodes and smoke evacuation devices were based on Spain-specific data (Supplementary Appendix A). It was assumed that 30% of procedures were open and 70% of procedures were laparoscopic, thus when smoke evacuation was used, 30% of procedures required a smoke evacuation pencil and 70% of procedures required smoke evacuation laparoscopic tubing. The cost of medical waste disposal per kilogram was based on consultation with Spanish experts.
Analysis Methods
There is uncertainty associated with the comparative efficacy for Ethicon devices compared to Non-Ethicon devices. In addition, costs can vary across hospital centers in Spain and in Europe. To address the parameter uncertainty in the model input values, a stochastic model was developed to evaluate the hospital budget impact of the Ethicon advanced energy device portfolio scenario (main analysis) or Full Ethicon energy portfolio scenario (secondary analysis) compared to the Non-Ethicon advanced energy devices scenario by conducting 10,000 Monte Carlo iterations. The objective of a stochastic analysis is to obtain a distribution of each of the model’s outputs that is informed by randomly sampled sets of input parameter values from the specified probability distributions. The data populating the model were mainly derived from the existing literature, which was analyzed to specify probability distributions describing the uncertainty around the true value of each input parameter. Depending on data availability for each parameter, the distribution parameters were derived from the range reported in the literature, the magnitude of the standard error of the pooled mean, or assumed a standard error of 12.5% of the pooled mean if only a single point estimate was available. For model inputs informed by differences between treatment groups, each group was probabilistically sampled. A summary of model input values, distributions, and parameters for the probabilistic analysis can be found in Supplementary Appendix A. Healthcare resource utilizations and costs followed a gamma distribution, probabilities followed a beta distribution, and treatment effects followed a normal distribution. Means and 95% credible intervals (CrI) were reported for each outcome. The CrI is used for reporting probabilistic analyses, since it represents a range containing a percentage of values across probabilistic analysis iterations (i.e. the 95% CrI represents the middle 95% of observed values for an outcome across the 10,000 iterations).
Scenario Analysis
In the base case, Ethicon and Non-Ethicon advanced energy devices had similar costs, with Ethicon device costs informed by data on file and Non-Ethicon device costs informed by a public tender (Supplementary Appendix A). A scenario analysis was conducted to account for different device costs that vary across hospital centers. This analysis explored the scenario where costs for Ethicon advanced energy devices were €100 higher than costs for Non-Ethicon advanced energy devices. For this scenario analysis, 10,000 Monte Carlo iterations were conducted using the same probabilistic methods described above.
Sensitivity Analyses
Deterministic one-way sensitivity analyses were performed to determine the impact of varying one parameter at a time on the magnitude of the predicted savings or cost impacts for the main analysis. Three one-way sensitivity analyses were performed including both the total and per procedure costs from the main analysis and the total costs from the full Ethicon energy portfolio secondary analysis. Time, quantity, cost, and percentage inputs were varied by ±25% in these analyses. The ten most impactful parameters were plotted on a tornado diagram depicting the change in total cost savings or impacts when the inputs were varied.
Results
Main analysis: Ethicon advanced energy device portfolio versus Non-Ethicon advanced energy devices
After switching from Non-Ethicon advanced energy devices to the Ethicon advanced energy device portfolio, the probabilistic analysis estimated the annual budget impact to the hospital was cost saving in 79.8% of iterations with a mean budget impact per procedure of -€236 (95% CrI: -€811; €321) (). The total annual budget impact and the annual budget impact per procedure are presented in and respectively. The analysis estimated mean annual cost savings with colorectal, bariatric, thoracic, and general surgery surgical specialties (). Differences in OR time, LOS, and transfusions are presented in (Supplementary Appendix B).
Figure 2. Ranked probability of budget impact per procedure following switch from Non-Ethicon advanced energy devices to the Ethicon advanced energy device portfolio. Negative values indicate cost savings. Analyses conducted for 4,000 procedures over 10,000 Monte Carlo simulations.
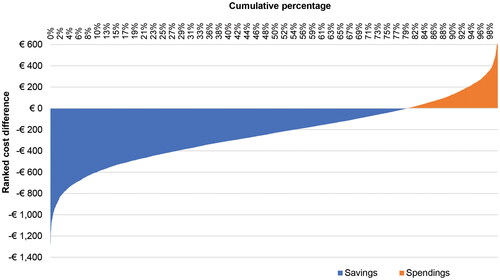
Figure 3. Distribution of annual budget impact per procedure following switch from Non-Ethicon advanced energy devices to the Ethicon advanced energy device portfolio. Negative values indicate cost savings. Analyses conducted for 4,000 procedures over 10,000 Monte Carlo simulations. Legend for the box and whisker plot: the cross represents the mean, the center line represents the median, and the box represents the interquartile range (IQR) containing the 25th to 75th percentiles of the per procedure budget impact from the simulations. The upper whisker represents the maximum per procedure budget impact from the simulations up to a distance of 1.5 IQR above the 75th percentile. The lower whisker represents the minimum per procedure budget impact from the simulations up to a distance of 1.5 IQR below the 25th percentile.
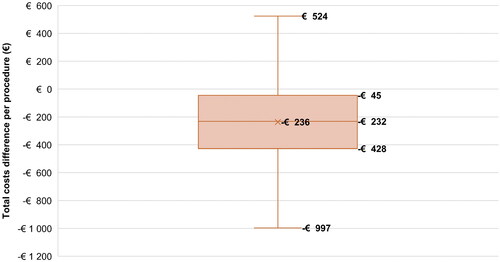
Table 1. Annual total budget impact.
Table 2. Annual budget impact with Ethicon advanced energy devices versus Non-Ethicon advanced energy devices by outcome for the five surgical specialties.
Secondary analysis: Full Ethicon energy portfolio versus Non-Ethicon advanced energy devices
With mean cost savings after switching from Non-Ethicon advanced energy devices to the Ethicon advanced energy device portfolio, it was determined whether the hospital budget would remain cost saving after switching to the Full Ethicon energy portfolio. Compared to Non-Ethicon advanced energy devices, switching to the Full Ethicon energy portfolio was still cost saving in 75.3% of iterations with a mean budget impact per procedure of -€97 (95% CrI: -€384; €183) (Supplementary Appendix C). The total annual budget impact is presented in , as well as the budget impact of adding smoke evacuation and reusable dispersive patient return electrodes. Annual budget impact results by specialty and per procedure are available in Supplementary Appendix C.
Scenario Analysis
A scenario analysis was performed where the costs of Ethicon advanced energy devices were set to a default value of €100 higher than Non-Ethicon advanced energy devices. The results of these analyses are presented in Supplementary Appendix D. In general, cost savings results were lower but aligned with those of the main analysis. After switching from Non-Ethicon advanced energy devices to the Ethicon advanced energy device portfolio or the Full Ethicon energy portfolio, the annual hospital budget impact was cost saving in 67.9% and 62.7% of the 10,000 simulations, respectively.
Sensitivity Analyses
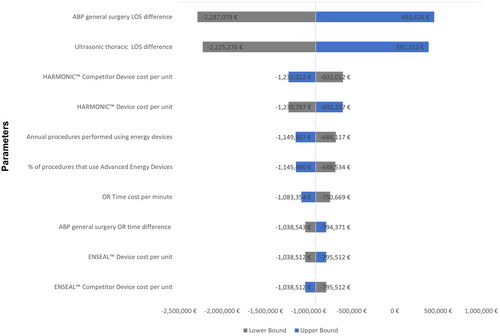
The three one-way sensitivity analyses were generally aligned with the cost-savings predicted in the base case analyses. In the one-way sensitivity analysis performed for the main analysis total budget impact, the model parameters with the greatest impact on results were the ABP general surgery LOS difference (-25%: -€2,287,079; +25%: €455,626) and the ultrasonic thoracic LOS difference (-25%: -€2,225,276; +25%: €391,252; ). These two parameters also had the greatest impact on results in the one-way sensitivity analyses on main analysis budget impact per procedure and secondary analysis total budget impact (Supplementary Appendix E). One-way sensitivity analyses indicated that when the remaining model parameters were individually varied by ±25%, cost-savings results were still predicted.
Discussion
The probabilistic budget impact analysis estimated that for a hospital in Spain that switched from Non-Ethicon advanced energy devices to the Ethicon advanced energy device portfolio, the annual budget impact was negative (cost saving) in 79.8% of iterations with a mean budget impact per procedure of -€236 (95% CrI: -€811; €321). This cost saving could be used to further enhance OR safety by incorporating smoke evacuation and reusable dispersive electrodes through the Full Ethicon energy portfolio, which was cost saving in 75.3% of iterations compared to Non-Ethicon advanced energy devices with a mean budget impact per procedure of -€97 (95% CrI: -€384; €183). Including smoke evacuation resulted in increased costs because potential reductions in healthcare resource utilization were not modelled. However, these additional costs were for devices that could improve OR safety by reducing the risk of staff exposure to surgical smokeCitation27,Citation28. Including reusable dispersive patient return electrodes yielded cost savings compared to the use of disposable dispersive patient return electrodes, while providing safety benefits to patients and reducing waste disposal costsCitation15. Cost savings were also observed in the scenario analysis where Ethicon advanced energy device costs were €100 more than advanced energy devices sourced from other manufacturers (Supplementary Appendix D).
Deterministic sensitivity analyses indicated that differences in LOS duration for general surgery and thoracic as well as device costs were some of the most impactful parameters on the model results. As expected, varying the total procedures performed using energy devices by ±25% had a large impact on the model results with an absolute difference of €465,791 for the main analysis. Since the number of ORs was used to determine the number of reusable dispersive electrodes considered in the model, it was only the 30th most impactful variable on the full portfolio model results yielding an absolute difference of €10,965.
Within this analysis, differences in clinical outcomes and healthcare resource utilization were linked to cost savings for the hospital. Devices that can lead to cost savings may be important to healthcare administrators and surgeons involved in economic decision-making who are seeking to improve resource use efficiency while improving patient outcomes and OR staff safety. The cost savings across specialties shown here warrant considering resource use efficiency for the hospital rather than by individual specialties alone. If less time is spent in the OR per procedure, the time saved could potentially be spent preparing the OR for the next procedure and allowing surgical staff to attend to other dutiesCitation29. If patient LOS is reduced post-procedure, then hospital beds could more quickly be freed up for other patients. Reducing OR time and patient LOS may have positive ramifications for hospital and staff productivity.
The clinical differences in outcomes for operating time, length of stay, and transfusions were based on results of a systematic review and network meta-analysis performed to support a deterministic analysis from a US hospital perspectiveCitation16. Some of the outcome differences between Ethicon advanced energy devices were informed by outcomes from individual comparative studies. Where there was no direct comparative evidence for ultrasonic or ABP devices in a specialty, network meta-analyses were performed when feasible to provide indirect comparative evidence instead. While not all statistically significant, the largest efficacy differences between Ethicon and non-Ethicon advanced energy devices were for OR time, followed by length of stay, with modest differences in transfusion rates (Supplementary Appendix B, see from Ferko et al. 2021Citation16) International modeling guidelines recommend that budget impact models use the best available evidenceCitation30. In this model, not all differences between outcomes were significantly different, but the best available direct and indirect evidence was used where comparisons were possible. Potential outcome differences may be caused by variation in device features included in the advanced energy devices across manufacturers. HARMONIC devices key features include the ability to seal vessels up to 7 mm in diameter and the Adaptive Tissue Technology reducing delivery of unnecessary energy and enabling more precise energy application, while key ENSEAL device features include algorithmic energy control, advanced compression, and low thermal spread to minimize tissue damageCitation31.
The comparative efficacy data used here from the Ferko budget impact analysis were from various regions including Europe based on data availabilityCitation16. However, healthcare costs in the US are very different compared to Europe and those costs may not be generalizable to Spain or other European countries. In addition, the US budget impact analysis was deterministic and therefore, only considered point estimates for model parameters when generating resultsCitation16. This Spain budget impact analysis addresses both of these gaps by providing an analysis that is more generalizable to Europe and incorporates parameter uncertainty. Despite these differences between the two studies, the US budget impact analysis also estimated cost savings when switching from Non-Ethicon devices to an Ethicon portfolioCitation16.
Limitations
This study had some limitations. There was insufficient data to compare Ethicon and Non-Ethicon devices in colorectal, bariatric, and gynecology surgical specialties for certain outcomes. In addition, the studies used to inform comparative efficacy represent one procedure each from all procedure types that are performed in the included surgical specialties. However, all available peer-reviewed literature was incorporated into this study according to the search criteria used in the previously published systematic literature review and NMACitation16. Some of effect size parameters included in the model did not reach statistical significance inducing some uncertainties that were addressed with the probabilistic analysis. The use of Spain-specific costs for healthcare resource utilization and energy devices may limit the generalizability of the model results to other countries, however, the probabilistic analysis mitigates this limitation. While the costs associated with smoke evacuation were modelled in the Full Ethicon energy portfolio, the potentially beneficial impacts on staff safetyCitation11,Citation27, such as reduced staffing costs associated with less sick-leave, were not modelled. The potential cost increase to using smoke evacuation should be considered in the context of its current recommendation for implementation by professional and safety bodies for reducing staff exposure to surgical smokeCitation11–14. In addition, while the cost of waste disposal for disposable and reusable dispersive patient return electrodes was modelled, other impacts of environmental waste were not incorporated, which is conservative when estimating the impact of introducing a reusable device to replace a disposable device. Indeed, investments in these technologies could result in OR safetyCitation15 and reduced environmental footprintCitation32,Citation33.
Strengths
This study has several notable strengths. The model was designed to incorporate clinical evidence from the literature for all surgical specialties with sufficient available data. This data was used to directly compare the relative efficacy of Ethicon devices versus other manufacturersCitation17–21, or estimate comparative efficacy based on a NMACitation16 when direct comparative evidence was unavailable. In the absence of head-to-head comparisons for some specialties, the NMAs enabled indirect comparisons of Ethicon advanced energy portfolio devices to Non-Ethicon advanced energy devices through a common comparator, usually conventional surgical methodsCitation16. Clinical evidence was incorporated into the model, regardless of whether results favored products from Ethicon or other manufacturers. Next, the use of a stochastic model allowed for the incorporation of parameter uncertainty into the results, allowing for a robust probabilistic analysis across 10,000 model iterations. Incorporating variability in costs supports the generalizability of results, since other hospital settings across Spain and Europe may have different costs. The probabilistic analysis also enabled incorporation of the uncertainty in the healthcare resource use outcomes. The finding that the Ethicon portfolios were still cost saving in the scenario with higher Ethicon device prices further support the robustness and generalizability of the analysis results to other hospital settings in Europe.
Conclusion
In conclusion, the probabilistic budget impact analysis results of adopting Ethicon devices demonstrated cost savings in most model runs. The results of these analyses suggest that switching to the Ethicon advanced energy device portfolio with advanced bipolar and ultrasonic devices results in cost savings in almost 80% of the simulations. Cost savings from the Ethicon advanced energy device portfolio were sufficient to cover the costs of smoke evacuation, with the addition of reusable dispersive patient return electrodes being cost saving as well. Using the Full Ethicon Energy portfolio presents an opportunity to improve staff and patient safety compared to the Non-Ethicon advanced energy device scenario. Savings persisted even when advanced energy device costs were €100 higher than comparator advanced energy devices. The probabilistic nature of these analyses helps to address parameter uncertainty in the model and deterministic sensitivity analyses show which factors are most impactful on the model results. Future analyses should be performed for other hospital settings in Europe with different costs compared to those used in this analysis. Future analyses should be performed once additional comparative efficacy data is available to compare advanced energy devices in specialties with limited comparative data and once studies assessing the clinical benefits of reusable patient return electrodes and smoke evacuation are available. These findings have implications for time, resource use, and cost savings for surgeons, hospitals, and economic decision-makers.
Transparency
Declaration of financial/other interests
LC and GW are employees of EVERSANA which was contracted by Ethicon to develop the model and help write the manuscript. AP, NJ, NRA, GT, and TG are employees of Johnson & Johnson MedTech who provided funding for the study and who manufacture the Ethicon devices analyzed in the study.
Author contributions
All authors contributed to the conceptualization and the design of the study. NJ and AP obtained funding for the study. LC, GW, AP, and TG developed the model, and AP, TG developed and performed the probabilistic analyses. All authors contributed to writing the manuscript, AP, NJ, NRA, GT, and TG reviewed the manuscript, LC and GW revised the manuscript, and all authors have read and approved the final version to be published and agree to be accountable for all aspects of the work.
Reviewer disclosures
Peer reviewers on this manuscript have received an honorarium from JME for their review work but have no other relevant financial relationships to disclose.
Previous presentations
This work has not been presented at any conferences and has not been published elsewhere.
Supplemental Material
Download MS Word (418.8 KB)Acknowledgements
The authors acknowledge Nicole Ferko, Imran Syed, Elena Naoumtchik, and Gaurav Gangoli for their work developing the original model for the US.
Disclosure statement of funding
Funding for this study was provided by Johnson & Johnson MedTech.
References
- Kalsekar I, Hsiao C-W, Cheng H, et al. Economic burden of cancer among patients with surgical resections of the lung, rectum, liver and uterus: results from a US hospital database claims analysis. Health Econ Rev. 2017;7(1):1–13.
- Stokes ME, Ye X, Shah M, et al. Impact of bleeding-related complications and/or blood product transfusions on hospital costs in inpatient surgical patients. BMC Health Services Res. 2011;11(1):1–13.
- Wei D, Roy S, Goldstein L, et al. editors. Economic burden of major complications in patients undergoing lower anterior resection surgery: a real-world database study. 2017.
- Cheng H, Clymer JW, Chen BP-H, et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 2018;229:134–144.
- Zoucas E, Lydrup M-L. Hospital costs associated with surgical morbidity after elective colorectal procedures: a retrospective observational cohort study in 530 patients. Patient Saf Surg. 2014;8(1):2–7.
- Bakkar S, Papavramidis TS, Aljarrah Q, et al. Energy-based devices in thyroid surgery—an overview. Gland Surg. 2020;9(Suppl 1):S14–S17.
- Patrone R, Gambardella C, Romano RM, et al. The impact of the ultrasonic, bipolar and integrated energy devices in the adrenal gland surgery: literature review and our experience. BMC surgery. 2019;18(1):1–7.
- Shiber L-DJ, Ginn DN, Jan A, et al. Comparison of industry-leading energy devices for use in gynecologic laparoscopy: articulating ENSEAL versus LigaSure energy devices. J Minim Invasive Gynecol. 2018;25(3):467–473. e1.
- Homma T. Advances and safe use of energy devices in lung cancer surgery. General Thoracic Cardiovasc Surg. 2022;70(3):207–218.
- Ulmer BC. The hazards of surgical smoke. Aorn J. 2008;87(4):721–738.
- EORNA. EORNA recommendation on: prevention and protection of surgical plume 2018. 2022. https://eorna.eu/wp-content/uploads/2019/09/Prevention-and-Protection-of-Surgical-Plume-PNC-EORNA.pdf
- Steege AL, Boiano JM, Sweeney MH. Secondhand smoke in the operating room? Precautionary practices lacking for surgical smoke. Am J Ind Med. 2016;59(11):1020–1031.
- National Institute for Occupational Safety and Health (NIOSH). Control of smoke from laser/electric surgical procedures. 2022.
- International Federation of Perioperative Nurses. IFPN guideline for smoke plume. 2022. www.ifpn.world/download_file/77/220
- Borgmeier PR, Ricketts CD, Clymer JW, et al. A Review of capacitive return electrodes in electrosurgery. J Surg. 2021;9(1):31–35.
- Ferko N, Wright GW, Syed I, et al. A device category economic model of electrosurgery technologies across procedure types: a US hospital budget impact analysis. J Med Econ. 2021;24(1):524–535.
- Koga H, Suzuki K, Nishimura K, et al. Comparison of the value of tissue-sealing devices for thoracoscopic pulmonary lobectomy in small children: a first report. Pediatr Surg Int. 2014;30(9):937–940.
- Hubner M, Demartines N, Muller S, et al. Prospective randomized study of monopolar scissors, bipolar vessel sealer and ultrasonic shears in laparoscopic colorectal surgery. Br J Surg. 2008;95(9):1098–1104.
- Roy KK, Netra G, Singhal S, et al. Impact of energy devices on the post-operative systemic immune response in women undergoing total laparoscopic hysterectomy for benign disease of the uterus. J Turk Ger Gynecol Assoc. 2018;19(1):1–6.
- Tsamis D, Natoudi M, Arapaki A, et al. Using Ligasure™ or harmonic ace® in laparoscopic sleeve gastrectomies? A prospective randomized study. Obes Surg. 2015;25(8):1454–1457.
- Badawy A, Seo S, Toda R, et al. Evaluation of a new energy device for parenchymal transection in laparoscopic liver resection. Asian J Endosc Surg. 2018;11(2):123–128.
- Ministry of Health. General Subdirection of Health Information. Register of Specialized Care Activity – RAE-CMBD. 2022. https://pestadistico.inteligenciadegestion.sanidad.gob.es/PUBLICOSNS
- Andalusian Health Service. https://www.sspa.juntadeandalucia.es/servicioandaluzdesalud/
- Ministry of Health. General Technical Secretariat. Statistics on Specialized Care Health Centers. Hospitals and Centers without Internment. 2020. https://www.sanidad.gob.es/estadEstudios/estadisticas/docs/TablasSIAE2020/INFORME_SIAE_2020.pdf
- Association of periOperative Registered Nurses. AORN Go Clear Award. https://www.aorn.org/education/education-for-facilities/go-clear-awards
- Brown S, Hutton B, Clifford T, et al. A Microsoft-Excel-based tool for running and critically appraising network meta-analyses–an overview and application of NetMetaXL. Syst Rev. 2014;3:110.
- Xie W, Dumas O, Varraso R, et al. Association of occupational exposure to inhaled agents in operating rooms With incidence of chronic obstructive pulmonary disease Among US female nurses. JAMA Netw Open. 2021;4(9):e2125749.
- Liu Y, Song Y, Hu X, et al. Awareness of surgical smoke hazards and enhancement of surgical smoke prevention among the gynecologists. J Cancer. 2019;10(12):2788–2799.
- Hoefsmit PC, Cerfolio RJ, de Vries R, et al. Systematic review of interventions to reduce operating time in lung cancer surgery. Clin Med Insights Oncol. 2021;15:1179554920987105.
- Sullivan SD, Mauskopf JA, Augustovski F, et al. Budget impact analysis—principles of good practice: report of the ISPOR 2012 budget impact analysis good practice II task force. Value Health. 2014;17(1):5–14.
- Ethicon Inc. Harmonic and Enseal device features and internal testing reports. Data on File. 2013-2021.
- Wyssusek KH, Keys MT, van Zundert AA. Operating room greening initiatives–the old, the new, and the way forward: a narrative review. Waste Manage Res. 2019;37(1):3–19.
- Conrardy J, Hillanbrand M, Myers S, et al. Reducing medical waste. Aorn J. 2010;91(6):711–721.