Abstract
Background
SARS-CoV-2 (COVID-19) continues to be a major public health issue. Obesity is a major risk factor for disease severity and mortality associated with COVID-19.
Objective
This study sought to estimate the healthcare resource use and cost outcomes in patients hospitalized with COVID-19 in the United States (US) according to body mass index (BMI) class.
Methods
Retrospective cross-sectional study analyzing data from the Premier Healthcare COVID-19 database for hospital length-of-stay (LOS), intensive care unit (ICU) admission, ICU LOS, invasive mechanical ventilator use, invasive mechanical ventilator use duration, in-hospital mortality, and total hospital costs from hospital charge data.
Results
After adjustment for patient age, gender, and race, patients with COVID-19 and overweight or obesity had longer durations for mean hospital LOS (normal BMI = 7.4 days, class 3 obesity = 9.4 days, p < .0001) and ICU LOS (normal BMI = 6.1 days, class 3 obesity = 9.5 days, p < .0001) than patients with normal weight. Patients with normal BMI had fewer days on invasive mechanical ventilation compared to patients with overweight and obesity classes 1–3 (6.7 days vs. 7.8, 10.1, 11.5, and 12.4, respectively, p < .0001). The predicted probability of in-hospital mortality was nearly twice that of patients with class 3 obesity compared to patients with normal BMI (15.0 vs 8.1%, p < .0001). Mean (standard deviation) total hospital costs for a patient with class 3 obesity is estimated at $26,545 ($24,433–$28,839), 1.5 times greater than the mean for a patient with a normal BMI at $17,588 ($16,298–$18,981).
Conclusions
Increasing levels of BMI class, from overweight to obesity class 3, are significantly associated with higher levels of healthcare resource utilization and costs in adult patients hospitalized with COVID-19 in the US. Effective treatment of overweight and obesity are needed to reduce the burden of illness associated with COVID-19.
PLAIN LANGUAGE SUMMARY
The COVID-19 pandemic has caused many people to be seriously ill. People who are overweight are more likely to get sicker from COVID-19 infection and to require hospitalization.
In our study, we compared patients who have normal weight to people who have overweight or obesity to understand how excess weight affects their experiences with COVID-19. We looked at: (1) how overweight and obesity is related to how long patients with COVID-19 stay in the hospital, (2) if they stayed in the intensive care unit (ICU) and how long they spent there, (3) whether they needed help breathing with the use of a ventilator and how long they needed a ventilator, (4) if they died during their hospital stay, and (5) how much their hospital stay cost.
We found that people who have overweight or obesity stayed in the hospital longer, were more likely to need to stay in the ICU, and were in the ICU longer. They were also more likely to need help breathing with the use of a ventilator and needed that help for a longer time. People who have overweight or obesity died during their hospital stay more often than people with a normal BMI. The costs associated with people who have overweight or obesity were higher than people who have a normal BMI.
Overall, this study shows that having overweight or obesity is a significant risk factor for poor outcomes from COVID-19 infection. Treatment for obesity and overweight is needed to help improve outcomes from future pandemics.
Introduction
Over 80 million people in the United States (US) have been infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), commonly referred to as COVID-19, since its emergence in early 2020Citation1. As of November 2022, over 1,000,000 patients have diedCitation1, 90% of whom had a pre-existing medical conditionCitation2,Citation3. Comorbidities such as cardiovascular disease, chronic kidney disease, diabetes, hypertension, immunocompromised conditions, liver disease, lung disease, obesity, and renal disease have been shown to significantly increase the risk of severe COVID-19 infectionCitation2,Citation3. Comparative risk assessment modeling has attributed nearly one-third of all COVID-19 hospitalizations in the US to the cardiometabolic disorders of type 2 diabetes, obesity, hypertension, and heart failureCitation4.
Obesity in particular has been identified as a major risk factor for disease severity and mortality associated with COVID-19Citation2. The impact of obesity in patients with COVID-19 is important given the increasing prevalence of obesity in the US over the last decade. The proportion of people with obesity (body mass index [BMI] of ≥30 kg/m2) has grown from 30.5% in 2000 to 42.4% in 2018Citation5. Notably, during the same time period, the prevalence of severe obesity (BMI ≥40 kg/m2) increased from 4.7 to 9.2%Citation5,Citation6.
Several aspects related to the pathophysiology of obesity could explain its adverse effects on COVID-19 outcomes. First, obesity has been shown to compromise immune function and to be characterized by systemic inflammation with increased levels of inflammatory cytokinesCitation7,Citation8. Second, patients with obesity have compromised respiratory function and reduced lung capacity due to mechanical limitations of the lung and chest wall. This can result in long-term effects including asthma and hypoventilation in patients without COVID-19 and could clearly increase the need for assisted mechanical ventilation in patients with COVID-19. Finally, obesity can exacerbate cardiometabolic disease and is associated with complications such as diabetes, metabolic syndrome, hypertension, cardiovascular disease (CVD), and chronic kidney disease (CKD) that could make patients with COVID-19 more susceptible to severe disease. Even so, it is unclear to what degree the poor outcomes for patients with COVID-19 and obesity are associated with BMI in isolation or the cardiometabolic complications of obesityCitation9. Along these same lines, the biomechanical complications including sleep apnea, decreased mobility, as well as the reductions in ventilatory volume could adversely affect outcomesCitation9.
Indeed, several studies have demonstrated that having obesity increases the risk of morbidity and mortality in patients with COVID-19Citation6,Citation10–17. Patients with overweight and obesity have been shown to be at higher risk for invasive mechanical ventilation (IMV), with the proportion of patients requiring IMV increasing with obesity classesCitation6,Citation11. Elevated BMI has been shown to be associated with increased risk of hospital admission and severe disease progressionCitation12,Citation13. While advanced age has been associated with poor outcomes among patients with COVID-19, obesity increases the risk of hospital admission, progression to severe disease, and in-hospital mortality among patients under the age of 65Citation11,Citation12. For patients with BMI >40 kg/m2, the adjusted risk ratio for invasive mechanical ventilation or death nearly doublesCitation11.
COVID-19 continues to have a significant impact on the health and wellbeing of the US population. While many studies have been conducted to understand the impact of BMI on health outcomes in patients with COVID-19, evidence is still emerging about how BMI classes 1, 2 and 3 impact healthcare resource utilization and costs. Few studies have evaluated these factors by variables such as in-hospital and ICU stays, IMV use and duration, and in-hospital mortality, all of which capture important cost-relevant dimensions of severity. Prior papers have explored per-patient hospitalization cost with obesity as one concomitant risk to COVID-19Citation15,Citation17; only one, to our knowledge, has published similar data that evaluates specifically by all three obesity classesCitation16.
Further research is needed to uncover the economic burden to the healthcare system when treating patients who also have obesity during a global pandemic, including long-term costs. To understand the greater healthcare resource use and cost impact of COVID-19 infection by varying classes of BMI, it is necessary to examine the study population across multiple facilities and geographic regions within the US. The objectives of this study were to estimate healthcare resource use, health outcomes, and total hospital costs among adults (age ≥20) hospitalized with COVID-19 infection in the US between April 2020 and October 2020 according to their BMI class.
Methods
Data source
The Premier Healthcare Database (PHD) is a large, US hospital-based, service-level, deidentified all-payer database that contains information on inpatient and outpatient encounters from geographically diverse non-profit, non-governmental, community and teaching hospitals, and health systems from rural and urban areas. Inpatient admission data include over 119 million visits with more than 10 million per year since 2012, representing approximately 25 percent of annual US inpatient admissions. This retrospective analysis utilized deidentified data from the Premier Healthcare COVID-19 database. This special release of the PHD is a standalone version of the existing database, which provides records from 1 January 2019, through 31 October 2020, and contains data from approximately 800 facilities. Based on information from the CDC’s Morbidity and Mortality Weekly Report, we found that about one-third of hospitals (n = 238) reported patient height and weight informationCitation11. This study was not reviewed by an institutional review board due to the use of deidentified data from a claims database.
Study population
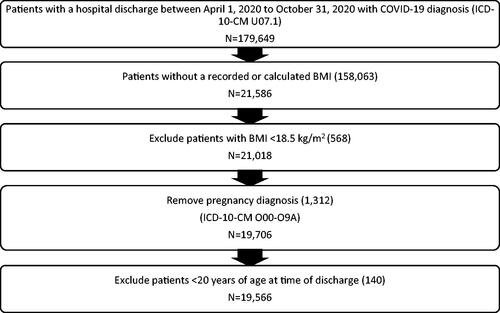
We conducted a retrospective cross-sectional study that included 179,649 patients discharged following hospitalization due to COVID-19, as reported by 873 facilities between 1 April 2020, and 31 October 2020 (). Criteria for inclusion in the study were: adult patients who were ≥20 years old at admission, hospitalized with COVID-19 defined as International Classification of Diseases – 10th edition (ICD-10) diagnosis code for 2019-nCoV related acute respiratory disease (U07.1), and had an available electronic medical record (EMR)-recorded BMI measurement or height and weight measurements that were used to calculate BMI based on data available at discharge. Age for inclusion was selected in alignment with US Centers for Disease Control (CDC) estimations, which include age 20 and above for consistency with CDC growth charts suggesting that people (primarily males) may continue to grow from 18 to 20 years, affecting their BMI calculationCitation5. Criteria for exclusion from the study were: BMI or either a height or weight measurement not available from EMR (n = 158,063, or 88% of the total population), BMI <18.5 kg/m2 (n = 568), pregnancy (n = 1,312) and <20 years of age at time of discharge (n = 140). Inclusion criteria were intentionally structured to capture a wide range of patients.
Study outcomes
The following outcomes were assessed: hospital length of stay (LOS; days), intensive care unit admission (ICU; yes/no), ICU LOS (days), invasive mechanical ventilator use (yes/no), invasive mechanical ventilator use duration (days), in-hospital mortality (yes/no), and total hospital costs based on internal cost accounting systems that evaluated a hospital’s cost of providing service (United States dollars; USD). Only published costs were used for analysis in this study, as unpublished costs related to COVID-19 were considered to be beyond the purview of this research design. We trimmed the upper and lower 1% of the dataset to account for outliers, which would have included zero and negative costs.
Statistical methods
To understand the impact of varying levels of BMI and other factors on healthcare resource use and cost outcomes within the study population, generalized linear models were conducted to test the crude and adjusted associations between BMI and the various outcomes. Hospital LOS, ICU LOS, and ventilator use duration outcomes were assessed via negative binomial or Poisson distribution. ICU admission, ventilator use, and in-hospital mortality were assessed by binomial distribution; odds ratios and predicted probabilities of these events were calculated. Total hospital costs were assessed by gamma/quantile distribution.
Primary explanatory variables were the BMI classes. The US CDC defines BMI categories as BMI values between 18.5 and <25 kg/m2 being within the normal weight range; BMI values between 25.0 and <30 kg/m2 are within the overweight range; and BMI values of 30.0 kg/m2 or higher are within the obesity rangeCitation18. Obesity can then be subdivided into categories: Class 1 includes BMI values of 30 to <35 kg/m2; class 2 includes BMI values of 35 to <40 kg/m2; class 3, sometimes referred to as severe obesity, includes BMI values of 40 kg/m2 or higher. BMI was ascertained at the time of admission from patients’ EMR.
Covariates for analysis included demographics (age at admission, gender, race/ethnicity), geography (state, region), comorbidities that could worsen outcomes of COVID-19 (Supplementary Table 1), and hospital characteristics (urban or rural population served, teaching status, bed capacity, level of care: acute care vs floor). Not all variables have been adjusted for in every model or were included in the final analysis. Clinical input and statistical tests were used to understand the relevance of each covariate in all the models. For some models, ICU stay or O2 supplementation was used as an explanatory variable and as an interaction term with BMI class variable to adjust for disease severity. Additional possible covariate interactions (e.g. age and BMI) were also explored. Finally, bivariate analysis between outcomes and covariates was used to test for associations that needed to be addressed in the final regression analysis.
Based on prior research, we have chosen to adjust outcomes based on age, gender, and race as the primary independent variables in our regression modelsCitation11,Citation19. The variable age was converted to a polynomial distribution based on the results of the Box-Tidwell test for linearity between age and the various outcomes. Distribution of the outcomes were not linear with age. Diagnostic variables such as comorbidities and respiratory-related conditions were excluded because they reside in the clinical pathway for treatment of this patient populationCitation11. To simplify resource utilization outcome comparisons between BMI classes, mean and 95% confidence limits were derived from the exponentiated values derived from the least squares mean calculation from the regression model.
Two sensitivity analyses were performed. The first sensitivity analysis was aimed at understanding the impact of changing treatment patterns and improved diagnostic tools in the later stages of the pandemic compared to the early stages. To accomplish this, the study population was divided into two groups: patients admitted between April and June 2020 and between July and October 2020. This was important because between April and June, the cases were thought to be more severe compared to the latter months of 2020. Additionally, social distancing, mask guidance, stay-at-home orders, and the general understanding of the condition were variable factors that changed during the time period and may have contributed to who was admitted to the hospital. The second sensitivity analysis was aimed to address the effect of underlying patient comorbidities and COVID-19 complications. This was not included in the main analysis because many of these comorbidities and complications lie in the intermediary causal pathway from exposure (BMI) to outcome (resource use).
Significance levels were calculated at the 0.05 level. All statistical analysis for this study was generated using SAS software (Version 9.4 for Windows). Copyright 2010, SAS Institute Inc., Cary, NC, USA.
Results
Study population
The final study population included 19,566 unique inpatient discharges (). Patients were distributed across BMI categories: normal (21.2%), overweight (32.1%), obesity class 1 (24.5%), obesity class 2 (11.6%), and obesity class 3 (10.6%). The majority of patients were over 50 with a mean age of 64.3 years, with 39.8% between 51 and 70 years old and 38.1% over 71 years old. Mean age for patients decreased with increasing obesity class, with a mean age for patients with normal BMI of 69.4 (SD = 17.4) compared to the mean age for patients with obesity class 3 of 56.2 (SD = 15.7). Patients identified as white (62.4%), black (21.2%), other (8.9%), Asian (2.4%), or unknown (5.1%).
Table 1. Patient demographics of those analyzed from Premier Healthcare Database from 1 April, 2020 to 31 October, 2020.
Clinical outcomes and healthcare resource utilization
Hospital length of stay
Increased mean hospital LOS was associated with increased BMI. Results from the unadjusted primary outcomes analysis show that total mean hospital LOS was shorter in patients with normal BMI compared to patients in the overweight and obesity classes 1 to 3 (7.8 days vs. 8.0, 8.2, 8.3, and 8.8, respectively) (Supplementary Table 2). Following adjustment for patient age, gender, and race for predicted effects of obesity class on the primary and secondary study variables, the mean hospital LOS for the normal BMI group was 7.4 days, and the corresponding adjusted LOS values for obesity classes 1 through 3 were 8.2 (p = .0037), 8.5 (p < .0001), and 9.4 (p < .0001) ().
Figure 2. Adjusted regression results: total hospital LOS, ICU LOS, and days on Invasive Mechanical Ventilation, Based on Data from the Premier Healthcare Database from 1 April 2020 to 31 October, 2020. ^Models were adjusted for patient age, gender, and race for predicted effects of obesity class on the primary and secondary study variables. Abbreviations. ICU, intensive care unit; LOS, length of stay. Normal: BMI = 18.5 to <25 kg/m2; Overweight: BMI = 25.0 to <30 kg/m2; Obesity class 1 = BMI 30 to <35 kg/m2; Obesity class 2 = BMI 35 to <40 kg/m2; Obesity class 3 = BMI 40 kg/m2 or higher. *p=.0037; **p<.0001.
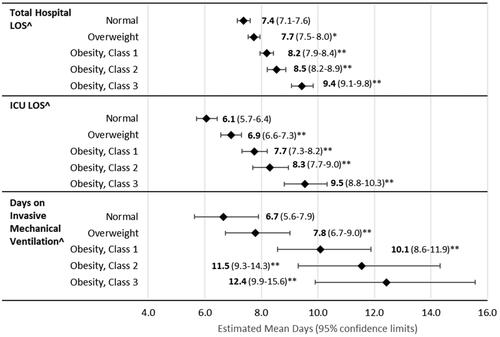
ICU LOS and admission rates
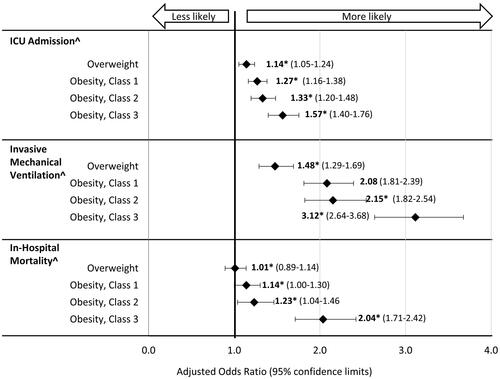
Compared to the normal BMI group, patients in the higher BMI classes had a significantly longer ICU LOS and greater rates of ICU admission rates. Unadjusted results found that total ICU LOS was shorter for patients with normal BMI compared to patients in the overweight and obesity classes 1 to 3 (6.7 days vs. 7.4, 7.9, 8.1, and 8.7, respectively) (Supplementary Table 2). After adjustment, the mean ICU LOS for the normal BMI group was 6.1 days (); in comparison, patients in the obesity class 3 group experienced a mean increase of 3.4 days for their ICU stay (p < .0001). Results of the unadjusted primary outcomes analysis show that a higher proportion of patients with COVID-19 and overweight (61.1%) and obesity (62.7–65.5%, classes 1–3) required an ICU stay compared to patients with normal BMI (58.3%) (Supplementary Table 3). In the adjusted analyses, the predicted probability of an ICU stay was higher for patients with greater BMI (56.0% for normal BMI vs 66.5% for class 3 obesity) (). Patients with overweight had 1.14 times higher odds of having an ICU stay compared to the normal BMI group (OR 1.14, 95% CI 1.05–1.24); Patients with obesity class 1, 2, and 3 had increased likelihood of an ICU admission (OR 1.27, 95% CI 1.16–1.38; OR 1.33, 95% CI 1.20–1.48; OR 1.57, 95% CI 1.40–1.57, respectively) ().
Figure 3. Adjusted regression results: predicted probabilities for ICU stay, need for invasive mechanical ventilation, and in-hospital mortality based on data from the Premier Healthcare Database from 1 April 2020 to 31 October 2020. ^Models were adjusted for patient age, gender, and race for predicted effects of obesity class on the primary and secondary study variables. Abbreviation. ICU, intensive care unit. Normal: BMI = 18.5 to <25 kg/m2; Overweight: BMI = 25.0 to <30 kg/m2; Obesity class 1 = BMI 30 to <35 kg/m2; Obesity class 2 = BMI 35 to <40 kg/m2; Obesity class 3 = BMI 40 kg/m2 or higher. *p <.0001.
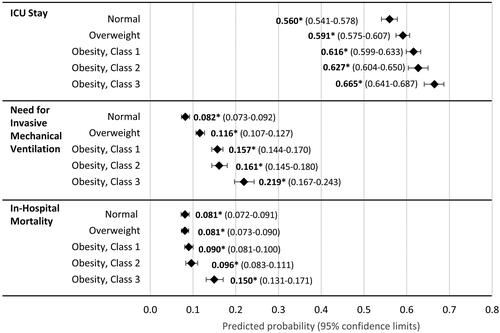
Figure 4. Adjusted regression results: odds ratios compared to normal BMI for ICU admission, invasive mechanical ventilation, and in-hospital mortality based on data from the Premier Healthcare Database from 1 April 2020 to 31 October 2020. ^Models were adjusted for patient age, gender, and race for predicted effects of obesity class on the primary and secondary study variables. Abbreviation. ICU, intensive care unit. Normal: BMI = 18.5 to <25 kg/m2; Overweight: BMI = 25.0 to <30 kg/m2; Obesity class 1 = BMI 30 to <35 kg/m2; Obesity class 2 = BMI 35 to <40 kg/m2; Obesity class 3 = BMI 40 kg/m2 or higher. *p<.0001.
Use and duration of invasive mechanical ventilation
Similarly, patients with overweight and obesity had higher predicted risk for, and significantly longer duration on, invasive mechanical ventilation. Unadjusted analysis showed higher percentages of patients with overweight (11.5%), obesity class 1 (14.6%), obesity class 2 (14.0%), and obesity class 3 (17.6%) were placed on invasive mechanical ventilation during their hospital stay compared to the patients with normal BMI (8.3%) (Supplementary Table 3). The relative risk of invasive mechanical ventilator use increased with obesity class; it was three times higher for patients with class 3 obesity compared to patients with a normal BMI (OR 3.12, 95% CI 2.64 − 3.68) (). Patients with overweight and obesity class 1 and 2 had 1.5 to 2.2 times higher odds of requiring invasive mechanical ventilator use (p < .0001). The predicted probability of invasive mechanical ventilation use was greater for patients with higher BMI classes compared to patients with normal BMI (8% for normal BMI vs. 22% for class 3 obesity, p < .0001) (). In the unadjusted primary analysis, patients with normal BMI had fewer days on invasive mechanical ventilation compared to patients with overweight and obesity classes 1 to 3 (7.2 days vs. 8.3, 9.9, 10.2, and 9.8, respectively) (Supplementary Table 2). After adjustment, patients with normal BMI had fewer days on invasive mechanical ventilation compared to patients with overweight and obesity classes 1–3 (6.7 days vs. 7.8, 10.1, 11.5, and 12.4, respectively, p < .0001) ().
In-hospital mortality
For in-hospital mortality, unadjusted results demonstrated that patients with normal BMI had a significantly higher in-hospital mortality rate (13.7%) compared to patients with overweight and obesity classes 1 to 3 (11.6, 10.9, 10.0, and 12.2%, respectively) (Supplementary Table 3). After adjustment, patients with class 2 or 3 obesity had a significantly higher likelihood of in-hospital mortality compared to patients with a normal BMI. The predicted probability of in-hospital mortality was nearly twice that of patients with higher BMI compared to normal BMI (8.1% for normal BMI vs 15.0% for class 3 obesity, p < .0001, ). The relative risk of in-hospital mortality was two times higher for patients with class 3 obesity compared to patients with a normal BMI (OR 2.04, 95% CI 1.71 − 2.42) ().
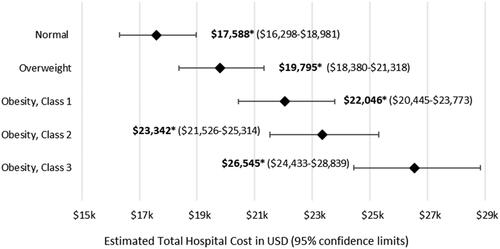
Total hospital cost
Mean total hospital cost increases as BMI increases. Unadjusted results demonstrated mean (SD) total hospital costs ranging from $18,472 ($19,924) per hospital stay in the normal BMI population to $24,206 ($29,041) per hospital stay in the obesity class 3 population (Supplementary Table 2). After adjustment, mean costs associated with patients in the overweight ($19,795, 95% CI $18,380–$21,318) and obesity class 1 ($22,046, 95% CI $20,445–$23,773), 2 ($23,342, 95% CI $21,526–$25,314), and 3 ($26,545, 95% CI $24,433–$28,839) groups were significantly higher than those of the normal BMI group (). The mean total hospital costs for a patient with class 3 obesity is 1.5 times greater than the mean for a patient with a normal BMI at $17,588 (CI $16,298– $18,981).
Figure 5. Regression results: total mean hospital cost, analyzed from Premier Healthcare Database from 1 April 2020 to 31 October 2020. Abbreviation. USD, United States dollars. Normal: BMI = 18.5 to <25 kg/m2; Overweight: BMI = 25.0 to <30 kg/m2; Obesity class 1 = BMI 30 to <35 kg/m2; Obesity class 2 = BMI 35 to <40 kg/m2; Obesity class 3 = BMI 40 kg/m2 or higher. *p <.0001.
Sensitivity analyses
Post-hoc sensitivity analyses after adjusting for treatment seasonality (Supplementary Tables 4 and 5) and comorbidities (Supplementary Tables 6 and 7) were completed. Results were not qualitatively affected by seasonality and comorbidities for all analyses except for in-hospital mortality. For in-hospital mortality, both obesity class 1 and obesity class 2 were no longer significant compared to base case analysis after adjustment for obesity complications and comorbidities (Supplementary Tables 6 and 7).
Discussion
COVID-19 remains a serious public health concern with obesity and its associated comorbidities and complications as major risk factors for poor outcomesCitation6,Citation10–14,Citation20. Our study adds to the growing body of evidence demonstrating the risks for patients with obesity during a public health crisis, such as the COVID-19 pandemic, and costs associated with these risks. Similar to other studies that found patients with underlying conditions who were hospitalized for COVID-19 incurred higher costs of medical care based on the degree of those conditionsCitation15,Citation17, our study found that obesity, in particular, was associated with both increased cost and increased healthcare resource utilization. As with Kompaniyets, et al. who found that inpatient care cost ranged from 6% or $1,131 more for adults with BMI between 25 and 29.9 to 34% or $6,108 for adults with BMI ≥45Citation16, we found that costs did, in fact, increase by obesity category but were substantially higher ($19,795 for patients with overweight and $26,545 for patients with BMI class 3). Shrestha, et al. reported similar findings to the Kompaniyets study in that patients with obesity averaged hospitalization costs 26% higher, or $5,933 more when compared to patients without the corresponding conditionCitation16,Citation17. However, our study compares the estimated mean total hospitalization cost at each BMI class, whereas Kompaniyets, et al. only provided the incremental difference.
Additionally, our time period is more focused on the initial period of the pandemic. We believe this is important because the pandemic has changed quite significantly over the past two and a half years. Our paper serves as a benchmark for the “shock” impact of the first six months of the pandemic.
The objective of this study was to understand the greater healthcare resource use and cost impact of COVID-19 infection by varying classes of BMI. As a foundation for comparison, we assessed the impact of BMI classification across a range of healthcare outcomes and identified similar trends to previously published research. We demonstrated that higher BMI is associated with greater healthcare resource utilization such as overall inpatient LOS, ICU admission, ICU LOS, invasive mechanical ventilation, length of time on invasive mechanical ventilation, and in-hospital mortality. Notably, the mean age for each patient group was lower as BMI class increased. This aligns with results from other studies demonstrating that for patients younger than 65, higher obesity classes are associated with increased risk of poor outcomesCitation11,Citation12. This study specifically demonstrated that higher obesity classes are also associated with both increased healthcare resource utilization and increased cost by specific variables, as noted above, which have not been exhaustively studied for the early period of the pandemic.
Similarly, while effects of increasing BMI were progressive, the greatest effect is seen for patients with obesity class 3, as they had an average hospital LOS of 2.0 days longer, ICU LOS of 3.4 days longer, and 5.7 more days on mechanical ventilation compared to individuals with normal weight. Patients with obesity class 3 had 1.6 times higher odds than patients with normal weight of having an ICU admission, 3.1 times higher odds of being on mechanical ventilation, and 2.0 times higher odds of dying in the hospital. Our results align closely with previous research in demonstrating that higher obesity classes are associated with increased risk of mortality, need for IMV, and progression to severe diseaseCitation6,Citation10–14,Citation20. Our study looked at outcomes that have not been previously examined by other papers, such as length of ICU stay and number of days on IMV, which capture another cost-relevant dimension of severity. Prior to adjustment, descriptive analysis of in-hospital mortality had an unexpected association of normal BMI with higher levels of in-hospital mortality. However, following adjustment, regression analysis showed that patients with lower BMI were associated with decreased risk of in-hospital mortality, suggesting that confounders were present that we were able to control for in our analysis. The primary variable that affected BMI mortality estimates was age.
Our study also highlights the total hospital costs associated with the increased healthcare resource utilization. Higher BMI is associated with increased resource utilization, which results in greater costs to hospital systems, with total mean hospital costs ranging from approximately $22,000 for obesity class 1 to over $26,000 for obesity class 3. Many of these outcomes have been examined individually; however, this study contributes to the literature by evaluating the impact of obesity among patients with COVID-19 on health systems/hospitals from a healthcare resource utilization and cost perspective using such specific variables as hospital LOS, ICU admission and length of stay, IMV use and duration of use, and in-hospital mortality.
Cardiometabolic comorbidities have been shown to significantly increase the risk of severe COVID-19 infection and have been associated with an estimated one-third of COVID-19 hospitalizations in the USCitation2–4. In our study, sensitivity analysis for comorbidities did not reveal any significant associations. This may be due to the broad analytic approach taken. Recently, it has been shown that patients with more advanced cardiometabolic disease and with social risk factors, such as racial and ethnic minorities or people with low socioeconomic status, had poorer outcomes associated with COVID-19 infectionCitation21. Additional research is needed to explore the association between cardiometabolic comorbidities, social determinants of health, and clinical outcomes with COVID-19.
Overall, obesity is associated with poor outcomes, and the COVID-19 pandemic has highlighted how obesity management must be prioritized. Managing obesity prior to development of COVID-19 and future pandemics is critical. The overall trends demonstrate that obesity is associated with poorer outcomes for patients with COVID-19. The lack of treatment and coverage for obesity treatment has created a susceptible population, which has been revealed by the COVID-19 pandemic. Care for patients with obesity resulted in greater costs during a healthcare crisis. COVID-19 has uncovered how significantly obesity impacts outcomes, and obesity must be addressed now, both for prevention of poor outcomes associated with COVID-19, and also for the future pandemics or other scenarios.
Limitations
There are several limitations to this study. Obesity involves many complex variables that were not captured in this study (e.g. social determinants of health or insulin resistance; controlling for these would attenuate the effect of BMI). This study was bound by the common limitations of administrative discharge data. These included non-clinical diagnosis methods, improper or incomplete coding, and missing data. As this is a non-interventional study, potential confounding factors cannot be ruled out. Data collection reflected routine clinical practice rather than mandatory assessments at pre-specified time points, which may have an impact on the amount of data and its interpretation.
The generalizability of the results may be limited. Although this analysis was performed on a convenience sample of hospitals submitting to the Premier Healthcare Database, these study findings only apply to the year 2020 and are expected to change over time. Due to the limited sample of hospitals providing BMI data to PHD and the inherent lack of statistical weighting based on our sample, these results may be considered marginally generalizable to the hospitalized COVID-19 population in the US. This assessment is based on the documented comparability of the geography, bed size, and services provided by the hospitals in the PHD compared to the nation as a whole. It is also worth noting that this analysis applies to the time period during which the study was conducted. COVID-19 is continually changing with respect to the proportion of disease due to different variants, and treatment will continue to improve over time. Evolving approaches to care could alter future health care resource utilization and costs in patients with obesity.
The costs associated with COVID-19 at the beginning of the pandemic may not be entirely reflective of the costs in years since, including costs for vaccines and available treatments. Further, it is possible that patients who were identified as being hospitalized for COVID-19 may have required hospitalization for another reason but were automatically tested for COVID-19 upon admission; if found positive, COVID-19 could have been incorrectly coded as the primary reason for hospitalization. This study does not evaluate unpublished costs of patients with obesity and COVID-19.
Patients who had an available EMR-recorded BMI measurement or height and weight measurements that were used to calculate BMI at discharge may represent a different population than those who did not have this information available. The costs analyzed in this study were the estimated cost for the hospital to provide services to the patient population based on internal cost accounting systems and may not be reflective of the actual costs incurred by hospitals; however, it is useful to see the relative change and trends by BMI classes. While associations between comorbidities and healthcare cost and are estimated and not necessarily causal, future research could explore to what degree poor outcomes and higher costs relate to BMI versus obesity-related complications. The trends demonstrated here show how the relative charge data is higher with the higher BMI classes.
Finally, while underlying patient comorbidities were included as variables for evaluating COVID-19 complications, this was not included in the final analysis because many of these comorbidities and complications lie in the intermediary causal pathway from exposure (BMI) to outcome (resource use).
Conclusions
This study demonstrates that increasing levels of obesity add significant burden of illness and costs for hospitalized patients with COVID-19 in the US. Measures aimed at reducing obesity in the general population could improve outcomes and health care costs for patients with COVID-19. The COVID-19 pandemic beckons a call to action to support obesity management and cover interventions that include weight management programs, pharmacological support, and surgical interventions in order to prevent similar scenarios in the future.
Transparency
Declaration of funding
Novo Nordisk Inc. funded the study and had a role in the study design, data collection, analysis, and interpretation of data, as well as writing support of the manuscript.
Declaration statement of financial/other relationships
NK was an employee of Novo Nordisk, Inc. at the time the study was conducted. AA is an employee and shareholder of Novo Nordisk, Inc. CC is an employee of Craver Research Services, which received funding to conduct the research. WTG has served as a consultant on advisory committees for Boehringer Ingelheim, Inogen, Novo Nordisk, Merck, Eli Lilly, Fractyl Health and Alnylam Pharmaceuticals. He also has served as site principal investigator for clinical trials sponsored by his university and funded by Eli Lilly, Novo Nordisk, Epitomee, and Pfizer.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Supplemental Material
Download MS Word (47 KB)Acknowledgements
The authors thank Elizabeth Tanner and Rebecca Hahn of KJT Group, Inc., Rochester, NY for providing medical writing support, which was funded by Novo Nordisk, Inc., Plainsboro, NJ in accordance with Good Publication Practice (GPP3) guidelines. These individuals have provided their permission to be acknowledged.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Centers for Disease Control and Prevention. COVID data tracker 2022; 2022 [cited 2022 Nov 28]. Available from: https://covid.cdc.gov/covid-data-tracker/#datatracker-home.
- Centers for Disease Control and Prevention. COVID-19: people with certain medical conditions 2021 [cited 2021 Nov 5]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
- Antos A, Kwong ML, Balmorez T, et al. Unusually high risks of COVID-19 mortality with age-related comorbidities: an adjusted meta-analysis method to improve the risk assessment of mortality using the comorbid mortality data. Infect Dis Rep. 2021;13(3):700–711.
- O'Hearn M, Liu J, Cudhea F, et al. Coronavirus disease 2019 hospitalizations attributable to cardiometabolic conditions in the United States: a comparative risk assessment analysis. J Am Heart Assoc. 2021;10(5):e019259.
- Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. Washington, DC: US Department of Health and Human Services; 2020.
- Simonnet A, Chetboun M, Poissy J, LICORN and the Lille COVID-19 and Obesity Study Group, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. 2020;28(7):1195–1199.
- Tanaka S, Isoda F, Ishihara Y, et al. T lymphopaenia in relation to body mass index and TNF-alpha in human obesity: adequate weight reduction can be corrective. Clin Endocrinol. 2001;54(3):347–354.
- Alwarawrah Y, Kiernan K, MacIver NJ. Changes in nutritional status impact immune cell metabolism and function. Front Immunol. 2018;9:1055.
- Nadolsky KZ, Hurley DL, Garvey WT. Covid-19 & obesity: beyond BMI. Endocr Pract. 2020;26(8):923–925.
- Docherty AB, Harrison EM, Green CA, ISARIC4C investigators, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ. 2020;369:m1985.
- Kompaniyets L, Goodman AB, Belay B, et al. Body mass index and risk for COVID-19–related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death — United States, March–December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):355–361.
- Lighter J, Phillips M, Hochman S, et al. Obesity in patients younger than 60 years is a risk factor for COVID-19 hospital admission. Clin Infect Dis. 2020;71(15):896–897.
- Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966.
- Sidhu G, Samson R, Nedunchezian SH, et al. COVID 19 in-hospital mortality, body mass index and obesity related conditions. J Diab Complic. 2021;35(12):108054.
- Di Fusco M, Shea KM, Lin J, et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Med Econ. 2021;24(1):308–317.
- Kompaniyets L, Goodman AB, Wiltz JL, et al. Inpatient care cost, duration, and acute complications associated with BMI in children and adults hospitalized for COVID-19. Obesity. 2022;30(10):2055–2063.
- Shrestha SS, Kompaniyets L, Grosse SD, et al. Estimation of coronavirus disease 2019 hospitalization costs from a large electronic administrative discharge database, March 2020–July 2021. Open Forum Infect Dis. 2021;8(12):ofab561.
- Centers for Disease Control and Prevention. Defining adult overweight and obesity; 2021 [cited 2022 Jan 12]. Available from: https://www.cdc.gov/obesity/adult/defining.html.
- Parikh R, Garcia MA, Rajendran I, et al. ICU outcomes in covid-19 patients with obesity. Ther Adv Respir Dis. 2020;14:1753466620971146.
- Garvey WT, Mechanick JI, Brett EM, Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines, et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22(Suppl 3):1–203.
- Howell CR, Zhang L, Yi N, et al. Associations between cardiometabolic disease severity, social determinants of health (SDoH), and poor COVID-19 outcomes. Obesity. 2022;30(7):1483–1494.