?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Aims
To generate utility decrements for three attributes associated with catheterization for individuals with a spinal cord injury (SCI): the process of catheterization, the physical impact of urinary tract infections (UTIs) and worry associated with hospitalization.
Materials and methods
Health state vignettes comprising various levels of the three attributes were developed. Two cohorts of respondents, corresponding to people with SCIs and a sample broadly representative of the UK population, were presented with nine vignettes (three vignettes for the mild, moderate and severe health states in addition to a random set of six vignettes). It was assumed no or a nominal decrement was associated with the mild health state. Utility decrements were derived from analysing the data obtained from the online time trade-off (TTO). A proportion of the SCI cohort (n = 57) also completed the EQ-5D-5L questionnaire.
Results
Utility decrements were generated using statistical models for the general population (n = 358), the SCI population (n = 48) and the two populations combined (merged model, n = 406). Results from the two cohorts showed minimal differences. For the merged model, SCI status was not statistically significant. All interaction terms, excluding SCI and the severe level of the physical attribute, were not statistically significant. Compared to the mild level, the greatest utility decrement calculated was the severe level of the emotional (worry) attribute (0.09, p < .001) for the SCI population. A significant decrement of 0.02 (p < .001) was calculated for the moderate level of the emotional attribute for all models. The mean utility score for those with SCI having completed the EQ-5D-5L was 0.371.
Limitations
Modest sample size of respondents from the SCI population (n = 48).
Conclusions
Worry associated with hospitalization had the greatest impact on patients’ health-related quality of life (HRQoL). The catheterization process, such as the lubrication and repositioning of the catheter, also impacted on patients’ HRQoL.
Introduction
There is a high incidence of urinary tract infection (UTI) amongst individuals with neurogenic bladder, defined as bladder dysfunction secondary to neurologic disorder.Citation1,Citation2 Incidence data for the UK are sparse, but globally, it has been previously reported that amongst spinal cord injury (SCI) patients, the UTI rate ranges from 0.8 to 3.5 episodes per year,Citation3–10 compared to just 0.1 episodes per year in the general population.Citation4 UTIs may progress to more serious complications, including bacteraemia and urosepsis. When severe, urosepsis is associated with a mortality rate of over 20%.Citation11
Clean intermittent catheterization (CIC) is the gold standard for individuals with neurogenic bladder, as it minimizes the risk of complications.Citation12,Citation13 CIC is undertaken where possible, by the patient themselves. Despite this, UTIs are a common complication of CIC, leading it to be a source of concern for individuals and their caregivers.Citation7 Individuals with SCIs can present with impaired sensations in the lower urinary tract which make it difficult to detect UTI-related symptoms.Citation6 According to European guidelines, all neurogenic bladder UTIs are considered complicated.Citation14 Furthermore, complicated catheter-associated UTIs are associated with a reported treatment failure of 52.5% in hospitalized patients (treatment failure being defined as no improvement by day 7 of antibiotic treatment, growth of a urine culture by ≥104 colony-forming units/mL, or new symptoms or death within 30 days of initial diagnosis).Citation15
Risk factors associated with UTIs in people with SCIs include incomplete bladder emptying and postvoid residual urine.Citation7 Increased residual urine may be caused by improper education given to the patient, anatomical bladder abnormalities, handling of the catheter and choice of catheter.Citation7
While there are new catheter technologies which aim to address some of the risk factors for UTI, the cost-effectiveness of these technologies needs to be assessed to inform national and regional reimbursement decisions. The National Institute for Health and Care Excellence (NICE) requires cost effectiveness (CE) studies to incorporate a health-related quality of life (HRQoL) measure in the form of health utilities.Citation16
As catheter usage and consequential UTIs have the potential to impact on patient’s HRQoL it is important that an appropriate measure is used to assess HRQoL in this population. NICE recommends that health utilities should be derived, where possible, from the EuroQol 5-dimension (EQ-5D-3L) instrument.Citation16 However, EQ-5D is a generic measure of HRQoL and, therefore, may lack the granularity to capture the specific complications of UTI in people with SCIs, such as the hazards associated with catheterization and associated worry around hospitalization. In addition, the mobility component of the EQ-5D can be misinterpreted by wheelchair users, as some people in a wheelchair may assume it equivalent to having no problems in walking about, whereas others may think the opposite.Citation17 It may also be difficult for people with SCIs to align the EQ-5D domains with the process of catheterization, meaning it is unlikely to be sensitive enough to capture potential differences between catheters. In such cases, approaches such as standard gamble (SG) and time trade-off (TTO) may be required.
TTO studies enable isolation of specific aspects of HRQoL, providing a more specific valuation without confounding health factors being included. TTO studies examining various aspects of intermittent catheterization have previously been conductedCitation18,Citation19 but have not captured the full extent of issues of catheterization associated with an SCI population.
The aim of this study was to conduct a TTO study to derive utility decrements for the process of intermittent catheterization, the physical impact from UTIs and the worry associated with potential hospitalization as a result of UTIs from people with SCIs, as well as from the general population.
Methods
The time trade-off study
The TTO methodology involves asking the respondents to consider how many years of remaining life-expectancy they would be willing to trade-off in order to live in a state of full health, rather than live for a longer period of time in an impaired health state.Citation20 In this study, full health was defined as a state where people still had an SCI requiring intermittent catheterization. Respondents are asked to consider the extent to which they value the state of “full health”, by assessing whether to spend their remaining life expectancy with the additional issues associated with intermittent-catheterization as described in the vignettes, or to shorten their lifetime and experience full health. These issues relate to process of intermittent-catheterization, physical impact of UTI and worry relating to hospitalization as a result of UTIs. From this, health state utility values (HSUV, henceforth referred to as utilities) ranging between 0 and 1 were elicited using the following equation:
This means that a utility of 1 represents “full health” and a utility of 0 is equal to “dead.” States worse than death were not considered, following insights provided by a patient advocacy group. From this, utility decrements were calculated for each attribute using the mild level as the reference case.
The standard time used for a TTO study is 10 years. However, evidence has shown that the duration chosen can be confounded by different life expectancies and can affect the values selected by the user.Citation21 In this study, respondents were presented with scenarios, which asked them to trade-off years of their remaining life expectancy. This has been done in other previously published TTO studies.Citation18 The expected remaining life expectancy for different age categories was calculated using data from a retrospective and prospective observational study of people with SCIs in the UK over a 70-year study period.Citation22 displays the sourced life expectancy for each age category.
Table 1. Life expectancy by age.
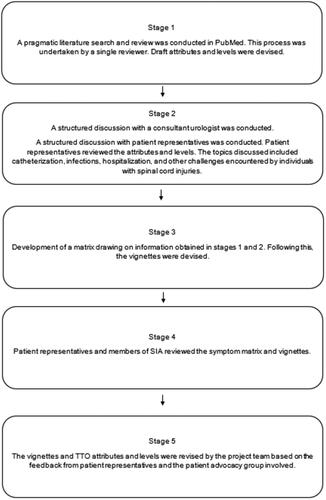
A five-stage process was used to develop the de novo vignettes for each population (see ). One clinician and people with SCIs were involved in the development process to ensure that all challenges associated with neurogenic bladder were captured. Draft health states were devised on the basis of a pragmatic literature search and presented to a consultant urologist, and five people with SCIs, including three representatives from the Spinal Injuries Association (SIA) charity.Citation23–26 All were asked to provide feedback during semi-structured interviews.
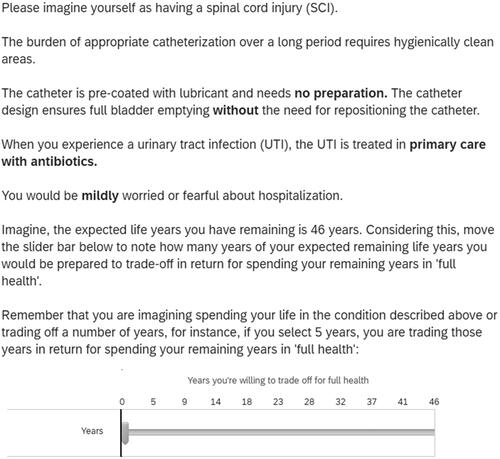
The final health states focussed on the main issues identified by people with SCIs. This study focussed on three of these attributes: the process of catheterization (the process attribute), the physical impact of having a UTI (the physical attribute), and the worry of potential hospitalization from a UTI (the emotional attribute). Each attribute was split into three levels; mild, moderate and severe (see ). It was assumed that the mild state for each attribute would be associated with either no, or nominal impact on HRQoL and so the decrements for each moderate or severe level can be interpreted directly as the associated impact on utility.
Table 2. Health states and descriptions.
The mild level for the process attribute describes a scenario comparable to using a hydrophilic catheter which does not require repositioning. The moderate level describes a scenario comparable to using a standard hydrophilic catheter (requiring repositioning) whilst the severe level describes a scenario comparable to using an uncoated catheter, which requires lubrication and repositioning.
The physical attribute relates to the symptoms experienced by individuals as a result of developing a UTI. The mild level describes a scenario whereby the individual experiences mild symptoms and is treated with antibiotics by their primary care provider. The moderate level describes a scenario comparable to attending hospital for treatment as a day patient, whilst the severe level describes a scenario whereby you are hospitalized for treatment, as an in-patient.
The emotional attribute relates to the worry or fear individuals may have of being hospitalized as a result of developing a UTI. The mild, moderate and severe levels within this attribute describe mild, moderate and severe levels of worry respectively.
Survey testing and implementation
The TTO study was conducted with two sample populations: a SCI cohort and a cohort from the general population. The sample population of interest was people with SCIs (aged 18 and over) who were self-catheterizing using intermittent catheterization with single-use coated catheters. The comparison sample was the general population which was broadly representative of the UK adult population with regard to sex and geographical location.
Survey testing was conducted using Qualtrics LLC (a third-party online platform providerCitation27) Questions were presented to survey participants on the online platform which asked participants to select the number of years of their remaining life expectancy which they would be willing to forego in order to be in a state of “full health.”
The draft general population vignettes were piloted on York Health Economics Consortium employees and members of the public who had not had any involvement in the vignette development. The draft SCI population vignettes were piloted on Coloplast employees, patient representatives and SIA members. The purpose of these pilots was to identify potential interpretation issues. Any issues raised during the pilots were discussed and changes were made where necessary.
While the vignettes within the survey for both populations were identical, that is, both the general population and the SCI sample were asked to imagine themselves as being the individual described in the scenarios, two separate surveys were distributed. This was to allow additional information in the background and information section, to help the general population envisage the perspective of an individual with a spinal injury requiring intermittent catheterization. Furthermore, the SCI population were required to complete the EQ-5D-5L, following the TTO, while the general population were not required to do so.
A power calculation was used to determine target numbers for the SCI population. This calculation determined a sample size of n = 56 was required. A sample size of n = 500 for the general population would ensure sufficient numbers per block, with an aim to recruit an additional 20% in each group to account for potential incongruent responses. However, as a result of the incongruent and incomplete responses, described in greater detail below, these numbers could not be reached. provides a summary of the final sample size for each population considered.
The initial pilot study for the general population (30 participants) returned a median time to completion of 2 min (maximum completion time of 4 min and a minimum completion time of 1 min). Upon analysis of the responses, incongruent responses – defined as respondents who had greater utilities for the worst health state (most severe scenario) compared with the mildest health state - were identified within the pilot sample. A second pilot study was conducted which returned a median time to completion of just under 6 min (maximum completion time of 75 min and a minimum completion time of 1 min). Consequently, a time limit (7 min) was implemented to ensure all participants who completed the survey in less than half the time limit (3.5 min) were eliminated from the results. This was done as it was considered unreasonable to accurately complete the survey in less than half the time limit assigned. The overall aim was to reduce the number of incongruent responses and improve the accuracy of the results.
Recruitment of people with SCIs was achieved by advertising the survey in a monthly newsletter for the SIA charity.Citation28 SCI responders were compensated with an e-voucher (£15) and the general population responders were compensated via the standard Qualtrics payment process (nominal value in e-vouchers). To align with the general population, a time limit of 7 min was imposed on the SCI survey to limit the number of incongruent responses.
The general population survey ran from 2 September to 12 October 2022, and the SCI survey from 2 September to 22 September 2022. The study was approved by the University of York Health Research Governance Committee (HSRGC/2022/498/B, 22 March 2022).
Both populations were required to complete the self-administered surveys online using the Qualtrics platform.Citation27 All general population respondents were aged 18 years or older. The sampling strategy was designed to ensure that there was an even distribution of participants across the defined age categories. This was to ensure that the sample population was representative of the general UK population.
Potential participants were taken through an informed consent procedure explaining the nature of and their right to withdraw from the study at any stage. Survey respondents were informed the survey could take up to approximately 30 min to complete. Participants who consented to take part in the study were then asked to provide basic socio-demographic details which were used to screen for eligibility. Further details regarding criteria for eligibility are provided in section S.2 of the Supplementary Material.
Within each survey, participants were provided with an explanation of the response format for the TTO and were taken through the process to familiarize themselves with the rating system. Participants in both studies were asked to imagine themselves as the person described in the scenarios. The general population sample were provided with background information about the catheterization process to help with understanding.
Participants in both samples were presented with nine vignettes. Each vignette comprised three attributes describing the process of using a catheter, the physical impact of a UTI and the worry of hospitalization associated with UTI. All participants were presented with three vignettes describing the mild, moderate and severe health states (see ). Participants were then presented with a random set of six other vignettes, to avoid order bias. An orthogonal design was used to ensure that each level was presented an equal number of times in each block, meaning that the estimates of the level effects were uncorrelated with those of the blocks. Each set of nine vignettes was referred to as a “block.” There were four blocks of nine vignettes in total. An example vignette is shown in .
Inclusion of the EQ-5D instrument for SCI population
The SCI cohort were asked to complete the EQ-5D-5L questionnaire in addition to the TTO. This was to allow a comparison of the results with other published EQ-5D utilities for the SCI population.Citation29 The general SCI population utility was collected; no details were collected on whether the individual was currently experiencing a UTI. The EQ-5D-5L was employed instead of the EQ-5D-3L, to enable improved sensitivity and precision.Citation30 The general population were not required to complete an EQ-5D-5L questionnaire.
Statistical analysis
All analyses were undertaken in R version 4.1.2 and Microsoft Excel (Microsoft Corporation, Redmond, WACitation31) Respondents who provided logically inconsistent, or incongruent responses (as defined above, i.e. where people responded to say they would trade off fewer years of life when in a fully severe state compared with a fully mild state) were rejected and a final dataset was created.
For both populations, descriptive statistics detailing the profile of responders were generated. Linear mixed-effects models were used to analyse the TTO data for each group. An initial examination of the residual plots demonstrated model suitability, such that the histograms of residuals were approximately bell-shaped. Population-specific results were generated for each of the three attributes after controlling for blocks (each set of nine vignettes) and patients as random effects, as well as age category and gender (fixed effects). Previous UTI status was not controlled for in any of the fitted models. Further details of the statistical analysis can be found in section S.3 of the Supplementary Material.
Due to the approach used to collect data within Qualtrics, age was included in all analyses as a categorical variable, with the lowest age group recorded representing the reference category. Gender was classed as a binary variable, with female representing the reference category. Where included, SCI status was incorporated into the analysis as a binary variable (present/absent). Within each of the three attributes, each individual level was modelled using a binary variable, with the mild level as baseline.
While separate results were generated for each population, the analysis also looked to reduce uncertainty in the final results via the merging of the data into one pooled dataset. Within this merged dataset, interaction terms between SCI status and each of the three attributes’ levels were included to investigate whether having an SCI would significantly affect utility for those presented with an equivalent level of a particular attribute.
The EQ-5D-5L profile data were converted to utility values using a published algorithm using the value set for EnglandCitation32,Citation33 and summary statistics comprising mean, median, standard deviation and 95% confidence intervals were generated. No additional analysis was conducted on the EQ-5D-5L data.
Results
TTO survey
There was a total of 465 completed responses to the general population survey of which 107 were eliminated from the final analyses due to incongruent or conflicting responses (23%). Participants who provided incongruent responses completed the survey in a similar time frame to those who provided congruent responses (median duration of 10.4 min versus 9.6 min, respectively). The final sample size for the general population was therefore 358.
There was a total of 91 respondents to the SCI population survey, of which 19 only completed the demographics part of the survey but failed to respond to any of the TTO questions. A further five people responded to less than three TTO vignettes, 12 responded to at least three questions but failed to complete the whole questionnaire and among those who did complete the whole survey, seven responses were classified as incongruent. All of these individuals were excluded from formal data analyses. The final sample size for the SCI population base case analysis was 48.
The demographic characteristics of the TTO survey participants for both populations used in formal data analyses are displayed in . There were proportionally more females in the general population sample. In contrast, there were proportionally more males in the SCI population.
Table 3. Summary statistics: sociodemographic details.
Impact of attributes on health-related quality of life (main findings)
Process attribute
For the general population (, Model 1), the analysis showed that both the moderate and severe levels corresponded to a statistically significant utility decrement when compared with the mild level (0.019 and 0.028 respectively, p < .001 for both results). The average decrement difference between those with uncoated catheters (Process: severe) and hydrophilic catheters requiring repositioning (Process: moderate) was 0.009.
Table 4. Utility results.
For the SCI population (, Model 2), the analysis showed a significant impact on the average utility decrement for the moderate level of 0.030 (p < .01) and a significant impact for the severe level 0.042 (p < .05), when compared with the mild level. This resulted in an average difference in decrements of 0.012 between the uncoated and hydrophilic catheters (which require repositioning).
For the merged model (, Model 3), the SCI status was not found to be statistically significant (p = .022). Therefore, the results from the SCI population were not significantly different from the TTO results of the general population. The interaction terms were not statistically significant for the moderate and severe levels of the process attribute (SCI and Process moderate, SCI and Process Severe). The resulting additional utility decrement for people with SCIs was 0.011 for the moderate level and 0.013 for the severe level, although statistical significance was not reached (moderate: p = .491; severe: p = .392).
Physical attribute
For the general population (, Model 1), the utility decrement for the moderate level, which involved treatment in hospital as a day case patient, was on average 0.007 (p = .237) whilst the decrement associated with the severe level was on average 0.031 (p < .001), when compared with the mild level. The average decrement difference between treatment as an out-patient (Physical: moderate) and an inpatient (Physical: severe) was 0.024.
For the SCI population (, Model 2), the utility decrement for the moderate level was on average 0.012 (p = .450) and 0.069 (p < .001) on average for the severe level, when compared with the mild level. This resulted in a difference in decrements of 0.057.
For the merged model, (, Model 3), the interaction term for the moderate level (SCI and moderate physical) was not statistically significant (−0.016, p = .319) whilst the interaction term for the severe level (SCI and severe physical) was statistically significant (−0.048, p < .01).
Emotional attribute
For the general population (, Model 1), the utility decrement for a moderate level of worry was on average 0.023 (p < .001) whilst a severe level of worry had a decrement of 0.082 (p < .001) when compared with the mild level. The average decrement difference between moderate and severe worry was 0.059.
For the SCI population (, Model 2), the decrement for the moderate level was on average 0.022 (p = .156) whilst the utility decrement for the severe level was on average 0.090 (p < .001) compared with the mild level. This results in a decrement difference of 0.068.
For the merged model (, Model 3), the interaction terms for the moderate decrement (0.008) and severe decrement (−0.002) when compared with the mild level were not statistically significant (SCI and Emotional Moderate: p = .643, SCI and Emotional Severe: p = .889).
EQ-5D-5L utility values (SCI population only)
There were 57 responses to the EQ-5D-5L questionnaire. The characteristics of these 57 respondents are presented in section S.5.2 of the Supplementary Material. Those who completed the EQ-5D-5L but provided incongruent responses in the TTO survey were still included in the EQ-5D-5L data analysis.
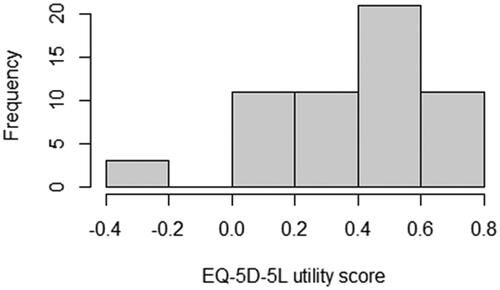
The distribution of the utility scores generated by the SCI respondents for the EQ-5D-5L was approximately normally distributed (). While the majority of EQ-5D-5L utility scores were between 0 and 1, three SCI respondents gave responses which led to negative utility values. This consequently skewed the results and lowered the summary statistics, most notably the mean.
The mean utility score for the EQ-5D-5L was 0.371; the median utility score for the EQ-5D-5L was 0.431.
Discussion
The aim of this study was to derive independent utility decrements for three attributes associated with catheterization in people with SCIs, namely, the process of catheterization, the physical impact of UTIs and the worry of hospitalization.Citation24–26 In addition, the study was designed to capture the impact of the severity of each of these attributes, each of which was posited to have a negative impact on HRQoL.
The primary finding from the study, based on a large, broadly UK representative sample, showed that as the severity of the attributes increased, the utility decrement associated with the attribute increased. The difference between the severe and mild levels was significant in all attributes examined in all models. There was variability in statistical significance between the moderate and mild levels across the models examined.
In this study, it was assumed that the mild state for each attribute would be associated with either no, or nominal impact on HRQoL and so the decrements for each moderate or severe level can be interpreted directly as the associated impact on full health utility. The largest utility decrement obtained in this study was for the severe level of worry associated with hospitalization. Furthermore, the largest utility difference between levels within each attribute was the difference between moderate and severe worry of hospitalization.
Additionally, the utility decrements isolated for the process of intermittent-catheterization demonstrated there was a greater decrement associated with a more burdensome process of catheterization (lubrication and repositioning). With regards to the physical impact of having a UTI on HRQoL, the results demonstrate that respondents from the SCI population generated a greater decrement (0.069, p < .001) than those from the general population (0.031, <.001). Furthermore, the interaction term (SCI and physical severe) was the only interaction term within the merged statistical model which was found to be statistically significant (0.048, p < .01).
NICE states that utilities should be derived using a choice method based on public preferences.Citation16 In this study, we conducted surveys with both the general population and the SCI population, to enable comparison of results. Minimal differences were observed in the results obtained between the two populations and SCI status was not found to be statistically significant in the merged model. Furthermore, all interaction terms in the merged model (which consider both SCI status and the individual levels of the attribute) excluding one, were found to be non-statistically significant.
While a limitation of the pooled results is that the number of respondents in the general population (n = 358) was far greater than those within the SCI population (n = 48), based on the analysis of the results obtained across the three models in this research it can be considered that both populations responded to the survey with similar preferences. If these results are to be considered in line with NICE’s preferences for utilities to be based on public preference, the decrements calculated for the general population can be considered to be applicable to SCI respondents, as excluding the SCI and severe physical interaction term, there was no statistical difference in the responses provided by both populations.
To the best of the authors’ knowledge, there have been no utility elicitation studies conducted to estimate the impact of worry of hospitalization on patients’ HRQoL. These results collectively underline the significant negative impact of the worry of hospitalization and the catheterization process on HRQoL. In other words, the physical impact of UTI and worry surrounding hospitalization may be linked to the process of catheterization and the consequences of burdensome catheterization. These results are in line with previous studiesCitation18,Citation19 which have shown that less complicated and faster catheterization, combined with fewer resulting UTIs, resulted in higher utility values associated with intermittent catheterization.Citation18 Worry associated with the process of catheterization and the consequences of improper technique has been well documented amongst the SCI population.Citation24–26 Furthermore, previous studies have also shown differences in patient preferences for certain catheters such as compact catheters and phthalate-free catheters.Citation19
Finally, turning to the EQ-5D-5L results, the mean EQ-5D-5L utility value from the survey distributed to people with SCIs in this study was 0.371. This result is substantively lower than other published sources identified. It is not possible to identify a specific reason for the low value. A systematic review conducted by Bermingham et al. reported a mean EQ-5D utility value of 0.831 in individuals with SCI performing intermittent catheterization.Citation34 The mean age of respondents in the study cited by Bermingham et al. was 29 years of age. In comparison, the mean age-group of respondents for the EQ-5D-5L in this research was the 56–65 age group.
The EQ-5D-5L questionnaire presents individuals with five different statements including a statement that asks them to best describe their ability to walk around and this question is open to multiple interpretations by respondents.Citation17 Furthermore, given the severity of a SCI, it is highly likely that their injuries will impact on the remaining dimensions assessed in the EQ-5D-5L questionnaire. Consequently, this raises the question of whether previously published EQ-5D utility values have overestimated the HRQoL of individuals with SCIs in the past.
Statistical analyses were not run to test the sensitivity of the EQ-5D-5L for the SCI population, but insensitivity can still be observed. Whilst catheter usage may be thought to be captured within the mobility or self-care domain, it may not be sensitive enough to capture the differences in HRQoL associated with catheters with improved functionality. This is due to the domains being restricted to questions about walking and dressing or washing. As the EQ-5D is a generic measure, it also lacks the ability to identify the root cause of low values within dimensions such as anxiety, whereas this TTO allows specific observation of utility decrements for worry related to hospitalization due to having a UTI. Overall, a TTO allows the HRQoL impact of catheterization for a person with an SCI to be captured where it might not be using the EQ-5D-5L questionnaire, increasing understanding of key drivers of quality of life in this population.
There are a few study limitations to acknowledge. Incongruent responses accounted for 23% of responses in the general population sample, although a similar proportion of incongruent responses have been reported in previous studies.Citation35,Citation36 Incongruent responses are a known disadvantage of time trade-off studies, with published research showing that incongruent responses can be because of the survey design or respondent characteristics, or both.Citation37 In this study, there were minimal differences in time to survey completion between respondents who gave incongruent responses and those who gave congruent responses. This suggests that both sets of participants were addressing the tasks carefully. While respondents who provided incongruent results were removed from the analysis, the remaining sample size for the general population was still large enough to provide robust results.
The TTO survey was conducted online as opposed to face-to-face interviews. This method can be considered to have both methodological strengths and weaknesses. One of the possible reasons for the number of incomplete or incongruent responses is the fact the survey was conducted online. Furthermore, the survey had a high task burden. However, the online method enabled a large sample generally representative of the population within the UK to be recruited. In addition, the interview process runs the risk of introducing different forms of bias, such as social compliance.
One further methodological point to note is that the use of a single question (“how many years would you be willing to trade-off”) differs from other iterative processes requiring participants to state their preferences for one scenario relative to another with the years remaining or traded-off varied up to the point of indifference.Citation38 Although these methods are different in terms of process, arguably, the single question approach is conceptually no different to the iterative approach. It requires participants implicitly rather than explicitly to arrive at their preference for years traded-off. Indeed, the single question method has been successfully applied in previous research to derive utility values.Citation35,Citation39
One potential limitation to acknowledge is that the task did not allow for “states worse than dead” (SWD). This meant that the utility values generated were bound between 0 and 1. The decision to not include the option of SWD was taken after discussions with the patient advocacy group. The absence of SWD may (or may not) have impacted on the results. It should be noted that the aim was to derive disutilities, in other words, the relative decrements, between the different levels of each attribute. It is unknown if individual parameters would have changed as a consequence of including SWD, and so, the effect on the relative differences, and therefore disutilities, is unknown. It should also be borne in mind that the EQ-5D-5L and TTO task elicited different utility values, namely the current HRQoL and the decrements associated with aspects of catheterization, respectively. That said, 3 participants in the SCI group (5.2%) rated their current HRQoL on the EQ-5D as SWD. Removing these participants from the sample increased the mean EQ-5D utility value from 0.3708 to 0.4051 (mean difference: 0.0343). Therefore, and given the different nature and aims of the tasks, although the absence of SWD may have affected utilities on the TTO task, the impact of this was negligible.
One further potential limitation of the study was the modest sample size of respondents within the SCI population. However, since the findings from the SCI and general population were broadly comparable, the SCI data can be used to validate the general population data. Further to this, only one statistically significant difference was found between populations in the pooled analysis, we do not believe that the limited sample size had a substantive impact on the conclusions.
A final possible limitation of the work is the potential framing effect of SCI individuals having completed the TTO preceding the EQ-5D. However, the impact of this is both unknown and arguably unknowable.
A major strength of this study was that we developed the vignettes in line with the NICE Decision Support Unit (DSU) report guidelines.Citation40 The NICE DSU process involves obtaining high quality information and evidence to inform the vignettes, presenting the vignettes in an easy-to-read format, refining vignettes through clinician and patient input and ensuring the vignettes can be understood by members of the general public with no experience of intermittent-catheterization.Citation40 As described in the methods, vignettes were subject to input from one clinician and patients and subject to various rounds of piloting. Additionally, conventional TTOs usually involve asking participants to trade-off life years up to 10 years, whereas the approach taken here was to employ the life expectancy approach, avoiding the problem of the time traded-off being confounded by different life expectancies.
Clean intermittent catheterization is the gold standard for neurogenic bladder management.Citation12,Citation13 There are currently two main types of intermittent catheters: hydrophilic catheters not requiring catheter lubrication and uncoated catheters (non-hydrophilic) requiring pre-lubrication prior to use requiring a greater number of preparatory steps. The study results demonstrated worry relating to hospitalization from UTI had the greatest impact on SCI patients’ HRQoL. The catheterization process also impacted on HRQoL. Our study has shown that worry of hospitalization from a UTI has the largest impact on the HRQoL of people with SCIs. Accordingly, it can be assumed that new catheter technologies that are simpler to use and carry less risk of UTIs with the aim to reduce worry about hospitalization, have the potential to improve HRQoL for people with SCIs.
Conclusions
In this study, utility decrements were calculated for three attributes associated with catheter usage in the SCI population: the process of catheterization, the physical symptoms of UTI and the worry of associated hospitalization. In conclusion, the results demonstrated that worry had the greatest utility decrement on SCI patients’ HRQoL. This suggests new catheter technologies which reduce patient’s worry associated with hospitalization as a result of a catheter induced UTI has the potential to positively impact SCI patient’s quality of life. To the best of our knowledge this is the first study which examines the worry associated with hospitalization as a result of UTIs resulting from catheterization. These data will be suitable for use in economic evaluations which assess the cost-effectiveness of new catheter technologies.
Transparency
Declaration of financial/other relationships
AS, AL, HD, BA, EL and SM work for York Health Economics Consortium (YHEC). CB (in the acknowledgements section) assisted in proof-reading the manuscript and works for YHEC. YHEC has been commissioned by Coloplast to conduct the study and write the manuscript. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
All authors read and approved the final manuscript. AL, HD, BA, AS and SM drafted and revised the manuscript. AL, AC and MC reviewed the manuscript. AL, HD, SM, AS, BA, AL, AC and MC were involved in the study design. HD, BA and EL were involved in data analysis.
Ethics statement
The study was submitted for review to the University of York’s Health Sciences Research Governance Committee and received ethics approval.
Supplemental Material
Download MS Word (42.7 KB)Acknowledgements
The authors are very grateful to Mr Nikesh Thiruchelvam, Consultant Urologist, and individuals from the spinal cord injury population and SIA who helped shape the vignettes. The authors would also like to thank Dr Catherine Bowe, who assisted in proof-reading the manuscript, and Dr Joe Moss who reviewed the data analysis. All individuals have provided permission to be acknowledged.
Data availability statement
Data can be made available upon request.
References
- Vigil HR, Hickling DR. Urinary tract infection in the neurogenic bladder. Transl Androl Urol. 2016;5(1):72–87.
- Powell CR. Not all neurogenic bladders are the same: a proposal for a new neurogenic bladder classification system. Transl Androl Urol. 2016;5(1):12–21.
- Woodbury MG, Hayes KC, Askes HK. Intermittent catheterization practices following spinal cord injury: a national survey. Can J Urol. 2008;15(3):4065–4071.
- Welk B, Lenherr S, Santiago-Lastra Y, et al. Differences in the incidence of urinary tract infections between neurogenic and non-neurogenic bladder dysfunction individuals performing intermittent catheterization. Neurourol Urodyn. 2022;41(4):1002–1011.
- Krebs J, Wöllner J, Pannek J. Risk factors for symptomatic urinary tract infections in individuals with chronic neurogenic lower urinary tract dysfunction. Spinal Cord. 2016;54(9):682–686.
- Krassioukov A, Cragg JJ, West C, et al. The good, the bad and the ugly of catheterization practices among elite athletes with spinal cord injury: a global perspective. Spinal Cord. 2015;53(1):78–82.
- Kennelly M, Thiruchelvam N, Averbeck MA, et al. Adult neurogenic lower urinary tract dysfunction and intermittent catheterisation in a community setting: risk factors model for urinary tract infections. Adv Urol. 2019;2019:2757862–2757862.
- Fisher H, Oluboyede Y, Chadwick T, et al. Continuous low-dose antibiotic prophylaxis for adults with repeated urinary tract infections (AnTIC): a randomised, open-label trial. Lancet Infect Dis. 2018;18(9):957–968.
- Esclarín De Ruz A, García Leoni E, Herruzo Cabrera R. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol. 2000;164(4):1285–1289.
- Siroky MB. Pathogenesis of bacteriuria and infection in the spinal cord injured patient. Am J Med. 2002;113(Suppl 1A):67S–79S.
- Wagenlehner FM, Lichtenstern C, Rolfes C, et al. Diagnosis and management for urosepsis. Int J Urol. 2013;20(10):963–970.
- Di Benedetto P. Clean intermittent self-catheterization in neuro-urology. Eur J Phys Rehabil Med. 2011;47(4):651–659.
- Joshi AD, Shukla A, Chawathe V, et al. Clean intermittent catheterization in long-term management of neurogenic bladder in spinal cord injury: patient perspective and experiences. Int J Urol. 2022;29(4):317–323.
- European Association of Urology. Urological infections; 2022. Available from: https://uroweb.org/guidelines/urological-infections/chapter/the-guideline
- Eliakim-Raz N, Babitch T, Shaw E, et al. Risk factors for treatment failure and mortality among hospitalized patients with complicated urinary tract infection: a multicenter retrospective cohort study (RESCUING study group). Clin Infect Dis. 2019;68(1):29–36.
- National Institute for Health and Care Excellence. NICE health technology evaluations: the manual (PMG36). Manchester, UK: National Institute for Health and Care Excellence; 2022.
- Ghislandi S, Apolone G, Garattini L, et al. Is EQ-5D a valid measure of HRQoL in patients with movement disorders? A comparison with SF-36 and FIM questionnaires. Eur J Health Econ. 2002;3(2):125–130.
- Averbeck MA, Krassioukov A, Thiruchelvam N, et al. The impact of different scenarios for intermittent bladder catheterization on health state utilities: results from an internet-based time trade-off survey. J Med Econ. 2018;21(10):945–952.
- Krassioukov A, Igawa Y, Averbeck MA, et al. Gains in health utility associated with urinary catheter innovations. Med Dev. 2018;11:345–351.
- York Health Economics Consortium. Time Trade-Off [online]; 2016. Available from: https://yhec.co.uk/glossary/time-trade-off/
- Lugnér AK, Krabbe PFM. An overview of the time trade-off method: concept, foundation, and the evaluation of distorting factors in putting a value on health. Expert Rev Pharmacoecon Outcomes Res. 2020;20(4):331–342.
- Savic G, DeVivo MJ, Frankel HL, et al. Long-term survival after traumatic spinal cord injury: a 70-year british study. Spinal Cord. 2017;55(7):651–658.
- Hearn JH, Selvarajah S, Kennedy P, et al. Stigma and self-management: an interpretative phenomenological analysis of the impact of chronic recurrent urinary tract infections after spinal cord injury. Spinal Cord Ser Cases. 2018;4:12.
- Kelly L, Spencer S, Barrett G. Using intermittent self-catheters: experiences of people with neurological damage to their spinal cord. Disabil Rehabil. 2014;36(3):220–226.
- Shaw C, Logan K, Webber I, et al. Effect of clean intermittent self-catheterization on quality of life: a qualitative study. J Adv Nurs. 2008;61(6):641–650.
- Welk B, Myers JB, Kennelly M, et al. A qualitative assessment of psychosocial aspects that play a role in bladder management after spinal cord injury. Spinal Cord. 2021;59(9):978–986.
- Qualtrics; 2022. Available from: https://www.qualtrics.com
- Spinal Injuries Association; 2022. Available from: https://www.spinal.co.uk/
- Bermingham SL, Hodgkinson S, Wright S, et al. Intermittent self catheterisation with hydrophilic, gel reservoir, and non-coated catheters: a systematic review and cost effectiveness analysis. BMJ. 2013;346:e8639.
- Janssen MF, Pickard AS, Golicki D, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res. 2013;22(7):1717–1727.
- R Core Team. A language and environment for statistical computing; 2022. Available from: https://www.r-project.org/
- Devlin NJ, Shah KK, Feng Y, et al. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ. 2018;27(1):7–22.
- Morton F, Nijjar J. Calculating EQ-5D indices and summarising profiles with eq5d. 2023.
- Bermingham SL, Ashe JF. Systematic review of the impact of urinary tract infections on health-related quality of life. BJU Int. 2012;110(11 Pt C):E830–E836.
- Smith AB, Hanbury A, Buesch K. Eliciting health state utilities for aromatic L-amino acid decarboxylase (AADC) deficiency: a UK vignette study. J Patient Rep Outcomes. 2021;5(1):130.
- Smith AB, Hanbury A, Whitty JA, et al. A discrete choice experiment to derive health utilities for aromatic L-Amino acid decarboxylase (AADC) deficiency in France. Patient Relat Outcome Meas. 2022;13:21–30.
- Yang Z, van Busschbach J, Timman R, et al. Logical inconsistencies in time trade-off valuation of EQ-5D-5L health states: whose fault is it? PLoS One. 2017;12(9):e0184883.
- Oppe M, Rand-Hendriksen K, Shah K, et al. EuroQol protocols for time trade-off valuation of health outcomes. Pharmacoeconomics. 2016;34(10):993–1004.
- Sharma S, Brown GC, Brown MM, et al. Validity of the time trade-off and standard gamble methods of utility assessment in retinal patients. Br J Ophthalmol. 2002;86(5):493–496.
- National Institute for Health and Care Excellence. CHTE methods review health-related quality of life task and finish group report; 2020.