Abstract
Aim
This study aimed to estimate the 10-year cost-consequence of weight loss on obesity-related outcomes in a sample of privately insured adults with obesity in Saudi Arabia (KSA).
Methods
We analyzed data of adults with obesity (BMI ≥ 30 kg/m2) available in Nphies, the private health insurance platform of the Council of Health Insurance, KSA. A micro-costing analysis was used to obtain domestic cost estimates for obesity-related outcomes. Cox proportional hazard models were used to estimate the benefit of weight loss by preventing incident cases of 10 obesity-related outcomes.
Results
In the study cohort (n = 314,079), the 30–34.9 BMI category contributed two-thirds of the cohort, and no gender differences were found in the age distribution of BMI categories. The elderly population had a higher prevalence of obesity-related outcomes, such as hypertension, osteoarthritis, and type 2 diabetes mellitus (T2DM). The baseline cost (2023) for treating these outcomes was USD 1.245 billion, which could double in 10 years. A 15% weight loss could save USD 1.295 billion over 10 years, with most savings due to T2DM (USD 430 million), given its higher prevalence (27.5%). The model was most sensitive to cost variability in T2DM, dyslipidemia, and hypertension.
Limitations
The results should be interpreted within the bounds of the study cohort, and Nphies is in its early stages of implementation. The cost estimates may differ if repeated among adults with obesity only, potentially leading to increased cost savings with weight loss.
Conclusions
Moderate weight loss of 5–15% over 10 years is associated with substantial cost savings in Saudi Arabia. For a 15% weight loss, 18.8% of incidence cases of obesity-related outcomes may be prevented, and slowed increases in T2DM, dyslipidemia, and hypertension may lead to considerable cost savings. The findings would help policymakers to implement weight loss programs in KSA.
Introduction
Obesity is defined as an abnormal or excessive fat accumulation in the body, resulting in a high body mass index (BMI) of at least 30 kg/m2 Citation1. It is a chronic relapsing diseaseCitation2, with serious health risks characterized by excess body fatCitation1,Citation2. Obesity prevalence has increased sharply worldwide since the 1950sCitation3, with an estimated 800 million people currently affectedCitation4. This is particularly true for regions with a high gross domestic product (GDP), such as North AmericaCitation5, Western EuropeCitation6, and the Gulf regionCitation7. Obesity is a major public health and economic concern in Saudi Arabia. In 2019, 38% and 20% of people were estimated to be living with overweight and obesity, respectivelyCitation8. The self-reported rate of obesity in 2020 was 25%Citation8,Citation9, and a 2022 systematic review estimated the obesity prevalence to be up to 36%Citation10. This is higher than the prevalence of other countries in the Gulf Cooperation Council (GCC)Citation11,Citation12.
The clinical and economic burden of obesity is linked to numerous obesity-related complications (ORC), including, but not limited to, hypertension, dyslipidemia, type 2 diabetes mellitus (T2DM), and sleep apneaCitation13,Citation14. Diabetes accounts for 3% of all deaths in Saudi Arabia, and 37% of deaths are attributable to cardiovascular disease (CVD)Citation15. Although the age-adjusted comparative prevalence of diabetes (type 1 diabetes mellitus (T1DM) and T2DM) in Saudi Arabia (18.7%) is lower than in Qatar (19.5%) in 2021Citation16, the former, with its larger population size, has a greater absolute number of people affected by this conditionCitation17.
An estimated 13.6% of total healthcare expenditure and 4.4% of GDP in the Eastern Mediterranean region was attributable to high BMI, with 4.3% of health expenditure in Saudi Arabia in 2019 being spent on treating complications associated with overweight and obesityCitation16–18. Obesity-related outcomes cause a significant burden on health-related productivity losses and healthcare costsCitation13,Citation14,Citation19, such as T2DM and CVDCitation20. Evidence from the United States (US) suggests that costs associated with these obesity-related outcomes are higher in individuals with higher BMICitation14, emphasizing the need to consider the economic and health impacts of obesity.
According to a recent microsimulation analysis, over one million new cases of obesity-attributable T2DM are expected among working-age adults in Saudi Arabia by 2040, with cumulative healthcare costs projected to exceed 84.4 billion US dollars (USD)Citation18,Citation21. A key policy objective under ‘Vision 2030’ is a comprehensive approach to effectively tackle this challenge, including health-risk prevention, strengthened services, and a shift towards preventing and managing non-communicable diseases (NCD)Citation22. To achieve this, the use of electronic health records (EHRs) and their integration, as well as widespread implementation and training by hospitals, are crucialCitation23,Citation24. The consistency of systems and coding across different hospitals may also help to streamline the collection of EHR data and aid in assessing the national impact of obesity in Saudi ArabiaCitation24.
A United Kingdom (UK) study using the Clinical Practice Research Datalink (CPRD) GOLD database evaluated the impact of weight loss on 10 obesity-related outcomes. A 13% weight reduction was associated with reduced risks of various obesity-related outcomes, including a 40% reduction in the risk of T2DM and sleep apnea among people with the highest level of obesity (BMI = 40 kg/m2)Citation25. The estimated benefits of weight loss, based on the aforementioned risks, are publicly availableCitation26. The objective of the present study was to estimate the long-term clinical and economic benefits of 5%, 10%, and 15% weight loss (to compare with the above 13% weight reduction) based on the relative risks for weight lossCitation27 in a sample of privately insured adults with obesity in Saudi Arabia.
Methods
A model for weight loss and risk reductionCitation25 (hereafter risk model) was adapted for estimating the cost-consequence of the long-term clinical and economic benefits of weight reductions over a 10-year time horizon in the private healthcare sector of Saudi Arabia, from 2023 through 2033.
Risk model
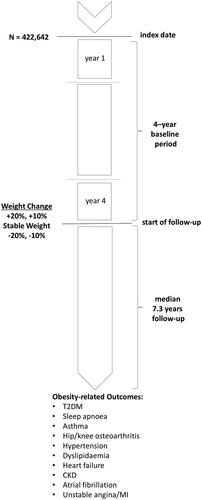
The information used in the risk model was obtained from the anonymized primary care records in the CPRD GOLD database, a commonly utilized source of primary care data in the UKCitation28. Individuals had to be between 18 and 70 years old with at least one mean BMI measurement > 30 kg/m2 measured between 2001 and 2010, with another BMI measurement after 4 years (baseline period). A retrospective cohort (n = 418,774) was analyzed with Cox proportional hazard models considering the change in BMI during the baseline periodCitation27. The risk model estimated the associations between weight loss and the relative reduction in the risk of developing obesity-related outcomes (). The analyses were adjusted for baseline BMI, age, sex, smoking, and ORC. The adjusted relative risks were used to project the relationship between percent weight change and the risk of ORC over 5 and 10 years. We also used a percent weight change to align with the approach applied in the risk model. A percent weight loss in BMI is a better measure of weight loss reduction interventions compared to measuring absolute weight loss in kilograms due to the measures ability to account for baseline differences and to reflect changes in body composition.
Patient population and clinical outcomes
There are approximately 11.8 million privately insured people (beneficiaries) in Saudi Arabia, covering Saudi (36%) and non-Saudi contributorsCitation29. All health insurance companies, providers, and third-party administrators in the private healthcare sector are regulated by the Council of Health Insurance (CHI), with the Minister of Health at its head. The CHI is an independent government authority established under Cabinet Decision No. (71) of 27/4/1420 AH (11/8/1999 AD) and mandated to improve the health of beneficiaries in the private healthcare sector through a regulatory environment that promotes prevention, transparency, fairness, quality, and efficiencyCitation30.
To this end, the CHI developed the Nphies platform to help healthcare providers gain access to health insurance benefits by facilitating real-time data exchange between healthcare providers, healthcare insurance companies, and other interested partiesCitation31. As part of its mission to improve healthcare delivery, the Nphies platform introduces a centralized channel for insurance and healthcare transactions, centralizing patient data in one digital medical record and boosting transparency and compliance. The platform consists of two parts: (i) an EHR for all economic sectors in the private economy and the foundation for an interoperable EHR; also known as the Healthcare Services System, and (ii) the Health Insurance Services System, a government-wide initiative to standardize the tracking and reporting of health care services by insurance providers and to facilitate the safe and dependable electronic interchange of health insurance transactions. The Saudi Health Council, the Saudi Ministry of Health, and the CHI sponsor the Nphies platform.
From the Nphies platform, the data of people with a BMI ≥ 30 kg/m2 and between 20 and 69 years old were extracted and included in the study, and obesity-related outcomes were identified with pre-specified ICD-10 codes. Since Nphies began processing health insurance transactions in December 2021, only EHRs for beneficiaries that required a healthcare service after that time were included in the analysis. The baseline characteristics of the study cohort were summarized and tabulated by BMI category, age range, gender, nationality, and geographical area, with the corresponding number of patients under each obesity-related outcome. We used the Cochran-Armitage test for trend, based on a chi-squared distributionCitation32, to statistically determine whether there is a significant trend across different age categories.
Costs and resource consumption
This study used the results of a systematic literature review that collected data on the prevalence of obesity and associated outcomes, prices, costs, and healthcare resource use in Saudi ArabiaCitation33. Researchers searched PubMed, Embase, and the International Federation for the Surgery of Obesity and Metabolic Disorders database from 2010 to 2021. Published costs were analyzed for adaptation of the risk model.
In order to gain further information on the economic costs of obesity-related outcomes, micro-costing exercises were necessaryCitation34 in Saudi Arabia. The micro-costing approach was used in public and private healthcare settings with resource consumption information and unit costs to generate detailed cost estimatesCitation35,Citation36. Data from only the private healthcare settings with resource consumption were used as inputs in this simulation model. The obesity-related outcomes aligned with those published in the UK risk modelCitation25, as shown in . Resource consumption and unit costs were estimated for diagnostic tests, scheduled outpatient visits, treatments, consumables/devices, health education programs, monitoring tests, treatment-related adverse events and complications, and inpatient proceduresCitation37. Estimates for services prices and unit costs were provided by hospital administrators or procurement specialists, and healthcare professionals identified the resource consumption from different geographic regions.
Services prices and unit costs for obesity-related outcomes were computed individually. The annual cost per patient per item was derived from the percentage of patients for each resource used multiplied by the unit cost. Private sector unit prices for pharmacological modalities were determined using the Saudi Food and Drug Authority drug registration price listCitation38. The private sector annual costsCitation37 were annuitized using a 5% inflation rateCitation39,Citation40 and presented in 2023 USD (1 USD = 3.75 SAR)Citation41 ().
Table 1. Obesity-related outcomes – average annual costs per patient in USD.
The direct costs associated with obesity-related outcomes were the product of case numbers and the cost per patient per outcome. Direct costs were estimated for each weight change category (5%, 10%, and 15% weight loss) at a 10-year time horizon and totaled to facilitate comparisons. Three weight change categories were chosen to present different scenarios under which savings may vary per obesity-related outcome, individually and in aggregate. The costs remained undiscounted to align with ISPOR guidelines for BIACitation42.
Sensitivity analysis
To learn what factors most affected the baseline outcomes, a one-way sensitivity analysis was conducted on the costs and relative risk reductions for obesity-related outcomes. We performed these analyses by iteratively adjusting model cost inputs between ‒50% and 50% of their initial values for a 15% weight loss over 10 years – the weight loss scenario with the highest cumulative savings. A tornado diagram was used to compile all the one-way sensitivity evaluations for review. Various scenarios of the dependency of individual outcome risk reductions on BMI across degrees of weight loss were analyzed.
Results
A sample of 3,131,189 people was identified on the Nphies platform, of which 1,537,070 (49.1%) people had a BMI measurement (). The majority were male (52.7%), less than 20 years old (32%), and located in Riyadh and the Eastern Region (74.8%). Of them, 34.7% (n = 362,898) had a BMI ≥ 30 kg/m2, and the most prevalent obesity-related outcomes were dyslipidemia, T2DM, asthma, and hypertension.
Table 2. Baseline characteristics of all patients and the cohort with BMI measurement.
Adults with a BMI ≥ 30 kg/m2 and between 20 and 69 years old were 20.4% (n = 314,079) of the population with a BMI measurement (study cohort). The ratio of women was lowest in the age category 40–49 years, and highest in the age category 20–29 years. There was a significant decreasing trend (p < .001) in the ratio of BMI category 30–34.9 with increasing age category, which contributed to approximately two-thirds of the cohort. For the proportion of individuals with BMI category 35–39.9, a significant increasing trend (p < .001) with increasing age was observed, whereas for the highest BMI category (40–50), no significant trend (p = ns) across the age categories was present (). The distribution of obesity-related outcomes by age categories showed a higher prevalence in older people. The prevalence of hypertension, osteoarthritis, and T2DM was 16.8-, 12.8-, and 10.5- fold higher, respectively, in the elder population (aged 60–69 years) than in the young people (aged 20–29 years). For all obesity-related outcomes, there was a significant trend increase in prevalence with an increased age category.
Table 3. Characteristics of patients with BMI ≥ 30 kg/m2 and aged 20–69 years (study cohort).
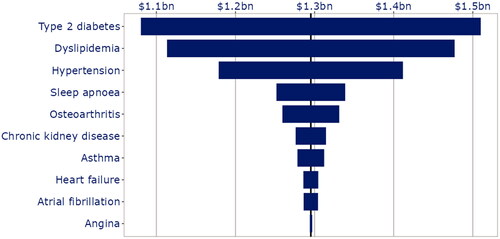
The current cost (baseline) of treating obesity-related outcomes in the study cohort was estimated to be USD 1.245 billion, mostly due to the cost of prevalent obesity-related outcomes, dyslipidemia (USD 464.3 million) and T2DM (USD 386.1 million). The total cost could double to USD 2.494 billion in 10 years () as the prevalence of all obesity-related outcomes continue to increase with age (Supplementary Material 1, Figure S3). A 15% weight loss and associated relative reductions in obesity-related outcomes could result in USD 1.295 billion in savings over 10 years. Dyslipidemia was the costliest obesity-related outcome, followed by T2DM. However, most cost savings due to weight loss could be associated with T2DM, given the higher reduction in incidence cases. Cost savings attributable to each obesity-related outcome were evaluated independently; however, reductions in T2DM incidence cases due to weight loss may lower incidence cases of other outcomes, resulting in higher cost savings than estimated above.
Table 4. Cost consequence of relative reductions in obesity-related outcomes by weight change scenarios over 10 years.
Sensitivity analysis
All possible combinations of the various parameters were analyzed using a one-way sensitivity analysis of the base-case scenario (USD 1.296 billion cumulative savings, ). T2DM, dyslipidemia, and hypertension were the top obesity-related outcomes, resulting in the most impact on cumulative savings (). A 50% increase in the T2DM annual treatment cost () resulted in higher cumulative savings ($1.5 billion). Asthma was the seventh most impactful obesity-related outcome despite being the fourth most prevalent condition (). Modifying the relative risk reductions resulted in the same tornado diagram since the total cumulative savings are the product of annual treatment costs and relative risk reduction. The dependence of individual outcome 10-year risk on BMI differed across 0 − 15% weight loss scenarios, and across age categories 30–60 years (Supplementary Material 1, Figures S1 and S2, respectively).
Discussion
The study found that modest weight losses ranging from 5–15% are associated with large cost savings in the study cohort (BMI ≥ 30 kg/m2 and between 20–69 years old) over 10 years. Cost savings were mostly attributable to T2DM, dyslipidemia, and hypertension, evaluated independently, against a background of rapid increases in prevalence as people age. The relative reductions in obesity-related outcomes due to weight loss are aimed at curbing these rapid increases, resulting in cost savings over time. , the tornado diagram, shows the 10 most influential sensitivity analyses for obesity-related outcomes, with the greatest impact on cumulative savings, indicating that the model was particularly sensitive to T2DM, dyslipidemia, and hypertension.
To our knowledge, this is one of the first studies in Saudi Arabia and the region to include data from the Nphies platform. Our research is also the largest nationally representative study on the cost-consequences of obesity-related outcomes in Saudi Arabia. A comparable study in 2021 reported cost savings of USD 274 million in a 100,000 people cohort with a 15% weight reduction and a BMI of 30–50 kg/m2 Citation33. Their synthetic cohort, derived from the UK population, sought to overcome the significant demographic differences in Saudi Arabia, namely higher T2DM prevalence and a younger population. The synthetic cohort, with combinations of characteristics to reflect those in Saudi Arabia, was used to estimate cost savings due to weight loss.
There are several benefits to using a domestic cohort obtained through the Nphies platform instead of synthetic cohorts acquired from other populations. As our research accounts for the distinct demographic characteristics and health issues experienced by the local population in Saudi Arabia, it provides a more realistic depiction of the actual cost-consequences of obesity-related outcomes. Understanding the effects of obesity on a community requires data from a wide cross-section of the local population; therefore, employing a domestic cohort offers the added benefit of including information from people of varying ages, genders, and geographical locations that represent the population in Saudi Arabia. Furthermore, our results were the actual prevalence from the Nphies platform, whereas the synthetic cohort for both the public and private sectors were based on obesity and T2DM prevalence published in the literatureCitation33. For instance, across all age groups, the synthetic cohort had a 71% higher rate of T2DM than our study cohort. The estimations presented in the literature were derived from smaller samples that showed substantial geographical variability.
Another Saudi-based study on the economic burden of overweight, obesity, and six NCDs (coronary heart disease, stroke, T2DM, breast cancer in women, colon cancer, and asthma) included direct medical, absenteeism, and presenteeism expenses arising from excess weightCitation43. The authors reported a direct cost impact of USD 3.8 billion and absenteeism and presenteeism costs of USD 15.5 billion in 2019 International USD. The estimates were based on the population attributable fraction (PAF) method, most often used at the population level as an epidemiological method for evaluating an exposure’s effects on population health. The method calculated an approximate fraction of a population’s health outcome that may be linked to obesity to estimate how much of an effect avoiding or lowering obesity might have on the health and cost outcomes of the population. One significant limitation of the PAF method is that it assumes a causal relationship between overweight and obesity (the exposure) and the six NCDs (the outcome). There may be confounding or other factors that could account for the observed association between the exposure and the outcome, resulting in overestimation or underestimation of the PAF estimates for the exposureCitation44,Citation45. Consequently, the direct cost impact reported in their research is not easily compared to our results; however, like our study, they also reported that T2DM was the largest cost driver.
A different study presented various future projections based on varying assumptions about the future prevalence of overweight and obesity, inadequate fruit and vegetable consumption, and inadequate physical activityCitation46. Ten models of possible scenarios were estimated for life expectancy, disability-adjusted life years (DALYs), deaths averted, and healthy life expectancy due to projected shifts in the NCD prevalence. These scenarios ranged from no change, moderate changes, and aggressive changes to the population’s risk factors between 2020 and 2050. They estimated, under the aggressive scenario, that 59,279 deaths in women and 110,712 deaths in men might be avoided by 2050 if overweight and obesity were reduced by 20%. The projections also suggested that, by 2050, Saudi Arabia may lower the DALY burden due to NCDs by 3.3–3.8%, assuming a moderate scenario of reductions in overweight and obesity. The study findings are insightful and comparable to the urgency for policy and interventions. However, the projections rely on assumptions that may not accurately reflect future trends, particularly as cultural and societal changes can have unpredictable impacts on health behavior over a 30-year period (2020–2050). Similarly, long-term trends seldom fully account for potential feedback loops, e.g. as health improves, people may become more physically active, further improving health outcomesCitation47,Citation48.
A recent study reported the long-term health and financial consequences of obesity-related T2DM and liver disease in Saudi Arabia’s working-age population (20–59 years)Citation49. They used a microsimulation model initially created for the UK population to estimate obesity-related outcomes in Saudi Arabia based on hypothetical populations. Their results were adjusted to reflect Saudi Arabia’s expected population growth over the study period, 2020–2040. The authors used UK costs converted to USD to estimate the financial impact of obesity-related T2DM in Saudi Arabia (USD 84.4 billion), citing a “more similar health care system” [49, S1 Table]. Several significant factors distinguish our study from the aforementioned. Our research used a study cohort retrieved from the Nphies platform, a local platform for private healthcare sector in Saudi Arabia. Through this, we could estimate the cost-consequence of obesity-related T2DM in privately insured adults in Saudi Arabia more accurately, together with the other obesity-related outcomes. We used prices and cost data collected in Saudi Arabia; thus, our findings improve the reliability and validity of the estimated cost-consequence of obesity-related outcomes, as they reflect the specific healthcare system, private healthcare sector, and economic circumstances in Saudi Arabia.
The study results have a substantial bearing on healthcare policy and practice in Saudi Arabia’s private sector. Cost savings from treating T2DM, dyslipidemia, and hypertension were the biggest factors in the long-term impact of 5–15% weight loss. It is crucial to address the epidemic of obesity and its associated comorbidities by creating and implementing successful weight loss programs and considering future enhancements to the CHI Essential Benefits PackageCitation50,Citation51. Counseling on food and exercise, medication for weight loss, and even bariatric surgery for extreme cases of obesity would all be possible components of such a programCitation52–54. Private healthcare providers may collaborate with public health authorities and the wider population to design community-wide initiatives to encourage the adoption of healthier dietary habits and reduce the consumption of processed food. Diet improvements should also be accompanied by regular physical activity and opportunities to implement both in daily life. The findings reported in our study further support the country’s effort toward promoting healthier habits in the population.
Private healthcare providers in Saudi Arabia can enhance patient health and lessen the economic burden of obesity-related disorders by encouraging investment in efficient weight loss programs and regulations. To this end, the CHI created the Population Health 5 × 5 Program in response to the concerning trends in five high-burden high-cost health conditions over the next 5 years, including but not limited to obesity, hypertension, coronary heart disease, and diabetesCitation55. The establishment of national obesity registries for disseminating evidence-based clinical recommendations and protocols may support the program’s objectives, together with technical support and education to fill knowledge gaps, as well as criteria for providers to be classified and reimbursed for effective weight loss interventions.
Limitations
We extracted a convenient sample (the study cohort) from the Nphies platform provided by CHI. The non-probability sampling approach enabled an exploratory analysis with data in a readily accessible and inexpensive format for further research. The study cohort was comprised solely of adults with private health insurance, which could introduce bias into the results. For example, the study cohort may have more disposable income or are in higher-paying positions, resulting in more access to healthcare services, including preventive care, which could affect their health outcomes and utilization patterns compared to adults without health insurance. Therefore, the study findings may not be generalizable to populations with different insurance status or healthcare access. The results herein should therefore be interpreted within the bounds of the study cohort and not for generalizing and drawing conclusions about the population of people with obesity in Saudi Arabia.
The study cohort (BMI ≥ 30 kg/m2 and between 20 and 69 years old) is approximately 10% of all patients (in ). The BMI and age criteria sought to align the study cohort with the definition of obesityCitation1 and the age categories for reporting prevalenceCitation56, respectively. The low proportion of the study cohort reflects a platform for EHR and real-time data exchange between healthcare stakeholders in its early stages of implementation. As the Nphies platform expands, more data will be available to strengthen the precision of results and improve their generalizability for privately insured individuals. Additional resources are required to ensure that BMI measurements are routinely collected and recorded and available for further analysis on the Nphies platform. Policymakers in the private health insurance market may also, under varying value-based payment modelsCitation57, include measurements on waist circumference as a better indicator of body fat distribution, which is strongly associated with health outcomes such as diabetes and cardiovascular disease. Incorporating waist circumference into risk models could lead to better identification of individuals at risk for these diseases and improved prevention effortsCitation58.
Our results are possibly conservative estimates of the cost-consequence of weight loss on obesity-related outcomes due to limitations in the micro-costing analysis. An earlier study estimated the cost of ORC among patients without obesity: “… nor did it focus specifically on people living with obesity when estimating the costs of treating complications …”Citation37 (p. 10). If the micro-costing analysis was repeated among people living with obesity, the cost estimates () would be different – perhaps higher than expected. If so, the cost savings associated with weight loss () would increase in the study cohort. We assumed that the cost per patient per obesity-related outcome remained fixed over 10 years. In reality, the cost of treating each outcome will change, and dynamic models that are continuously updated will improve the precision of results. Furthermore, we chose to focus on relative reductions in obesity-related outcomes and cost savings for males and females across all weight loss categories. In future research, we may explore gender differences in obesity-related outcomes in a separate publication.
Conclusion
We found that even moderate weight loss (between 5% and 15%) could achieve substantial cost savings over 10 years. Reducing incidence cases of obesity-related outcomes due to weight loss leads to increased cost savings over time. Our study’s domestic prices, cost inputs, and the CHI study cohort provide reliable findings. These findings may help ensure that policy and intervention decisions are based on the best available evidence and tailored to the unique characteristics of the Saudi Arabian population.
Transparency
Declaration of financial/other relationships
HAO, NAJ, SAA, AAS, AAK, and FAS are supported by their employing institutions. AA and VS are employees at Novo Nordisk. JLC is an employee at Syenza and a consultant for Novo Nordisk.
Author contributions
HAO, NAJ, AA, VS, and SAA: Study concept and design.
HAO, NAJ, SAA, and FAS: Data collection.
JLC, HAO, NAJ, SAA, AAS, AAK, FAS, and VS: Data interpretation.
JLC primarily wrote the manuscript along with HAO, SAA, and VS.
JLC, HAO, NAJ, SAA, AAS, AAK, FAS, and VS: Manuscript Revisions.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Supplemental Material
Download MS Word (649.4 KB)Acknowledgements
None stated
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- World Health Organization. Obesity. https://www.who.int/health-topics/obesity.
- About Obesity [Internet]. World Obesity Federation. https://www.worldobesity.org/about/about-obesity
- Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8.
- World Obesity Day. https://www.worldobesityday.org/.
- Mitchell NS, Catenacci VA, Wyatt HR, et al. Obesity: overview of an epidemic. Psychiatr Clin North Am. 2011;34(4):717–732. doi: 10.1016/j.psc.2011.08.005.
- Janssen F, Bardoutsos A, Vidra N. Obesity prevalence in the Long-Term future in 18 european countries and in the USA. Obes Facts. 2020;13(5):514–527. doi: 10.1159/000511023.
- Balhareth A, Meertens R, Kremers S, et al. Overweight and obesity among adults in the Gulf states: a systematic literature review of correlates of weight, weight-related behaviours, and interventions. Obes Rev. 2019;20(5):763–793. doi: 10.1111/obr.12826.
- Ministry of Health. World Health Survey Saudi Arabia 2019 Final Report. 2019. https://www.moh.gov.sa/en/Ministry/Statistics/Population-Health-Indicators/Documents/World-Health-Survey-Saudi-Arabia.pdf
- Althumiri NA, Basyouni MH, AlMousa N, et al. Obesity in Saudi Arabia in 2020: prevalence, distribution, and its current association with various health conditions. Healthcare. 2021;9(3):311. doi: 10.3390/healthcare9030311.
- Salem V, AlHusseini N, Abdul Razack HI, et al. Prevalence, risk factors, and interventions for obesity in Saudi Arabia: a systematic review. Obes Rev. 2022;23(7):e13448. doi: 10.1111/obr.13448.
- World Health Organization. Prevalence of obesity among adults, BMI ≥ 30, age-standardized - Estimates by country. https://apps.who.int/gho/data/view.main.CTRY2450A
- World Obesity Federation Global Obesity Observatory. World Obesity Federation Global Obesity Observatory. https://data.worldobesity.org/
- Shekar M, Popkin B, editors. Obesity: health and economic consequences of an impending global challenge. The World Bank; 2020. doi: 10.1596/978-1-4648-1491-4
- Divino V, Ramasamy A, Anupindi VR, et al. Complication-specific direct medical costs by body mass index for 13 obesity-related complications: a retrospective database study. J Manag Care Spec Pharm. 2021;27(2):210–222. doi: 10.18553/jmcp.2020.20272.
- World Health Organization. Noncommunicable diseases Saudi Arabia 2018 country profiles. 2018. https://cdn.who.int/media/docs/default-source/country-profiles/ncds/sau_en.pdf?sfvrsn=8305d6ca_38&download=true
- IDF Diabetes Atlas 10th Edition. https://www.diabetesatlas.org/data/
- Population, total - Saudi Arabia | Data. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=SA
- Alghnam S, Alessy SA, Bosaad M, et al. The association between obesity and chronic conditions: results from a large electronic health records system in Saudi Arabia. IJERPH. 2021;18(23):12361. doi: 10.3390/ijerph182312361.
- Lin X, Xu Y, Xu J, et al. Global burden of noncommunicable disease attributable to high body mass index in 195 countries and territories, 1990-2017. Endocrine. 2020;69(2):310–320. doi: 10.1007/s12020-020-02352-y.
- Muka T, Imo D, Jaspers L, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. 2015;30(4):251–277. doi: 10.1007/s10654-014-9984-2.
- Alqahtani S, J S, T C, et al. Poster 165: how could different obesity scenarios alter burden of diabetes and liver disease in Saudi Arabia? In: 39th Annual Meeting of the Obesity Society. 2021.
- Health Sector Transformation Program. Vision 2030. https://www.vision2030.gov.sa/v2030/vrps/hstp/
- AlSadrah SA. Electronic medical records and health care promotion in Saudi Arabia. Saudi Med J. 2020;41(6):583–589. doi: 10.15537/smj.2020.6.25115.
- Alnofal FA, Alrwisan AA, Alshammari TM. Real-world data in Saudi Arabia: current situation and challenges for regulatory decision-making. Pharmacoepidemiol Drug Saf. 2020;29(10):1303–1306. doi: 10.1002/pds.5025.
- Haase CL, Lopes S, Olsen AH, et al. Weight loss and risk reduction of obesity-related outcomes in 0.5 million people: evidence from a UK primary care database. Int J Obes (Lond). 2021;45(6):1249–1258. doi: 10.1038/s41366-021-00788-4.
- Novo Nordisk. Obesity risk calculator. https://www.rethinkobesity.global/global/en/weight-and-health/a-chronic-disease-the-health-impacts-of-obesity/obesity-risk-calculator.html
- Khunti K, Schnecke V, Haase CL, et al. Weight change and risk of obesity-related complications: a retrospective population-based cohort study of a UK primary care database. Diabetes, Obesity and Metabolism. 2023;45(6):1249–1258.
- Primary care data for public health research | CPRD. https://www.cprd.com/primary-care-data-public-health-research
- Council of Health Insurance. CHI in Numbers: Health insurance indicators [Internet]. Council of Health Insurance. https://chi.gov.sa/en/Pages/default.aspx
- Council of Health Insurance. Available from: https://chi.gov.sa/en/AboutCCHI/Pages/secretariat.aspx
- Council of Health Insurance. Nphies: Guidance Manual. 2022. https://chi.gov.sa/Uniplat/Documents/21112022.pdf
- Rosner B. Fundamentals of biostatistics. 7th ed. Boston: Cengage Learning; 2010.
- Alqahtani SA, Al-Omar HA, Alshehri A, et al. Obesity burden and impact of weight loss in Saudi Arabia: a modelling study. Adv Ther. 2023;40(3):1114–1128. doi: 10.1007/s12325-022-02415-8.
- Špacírová Z, Epstein D, García-Mochón L, et al. A general framework for classifying costing methods for economic evaluation of health care. Eur J Health Econ. 2020;21(4):529–542. doi: 10.1007/s10198-019-01157-9.
- Xu X, Lazar CM, Ruger JP. Micro-costing in health and medicine: a critical appraisal. Health Econ Rev. 2021;11(1):1. doi: 10.1186/s13561-020-00298-5.
- Frick KD. Microcosting quantity data collection methods. Med Care. 2009;47(7 Suppl 1):S76–S81. doi: 10.1097/MLR.0b013e31819bc064.
- Al-Omar HA, Alshehri A, Abanumay A, et al. The impact of obesity in Saudi Arabia: healthcare resource use and costs associated with Obesity-Related complications. Adv Ther. 2023;40(4):1430–1443. Epub ahead of print. doi: 10.1007/s12325-023-02426-z.
- Saudi Food and Drug Authority. Drugs List: Tameni Application. 2023. https://www.sfda.gov.sa/en/drugs-list
- Al Aqeel SA, Al-Sultan M. The use of pharmacoeconomic evidence to support formulary decision making in Saudi Arabia: methodological recommendations. Saudi Pharm J. 2012;20(3):187–194. doi: 10.1016/j.jsps.2011.12.006.
- Khorasani E, Davari M, Kebriaeezadeh A, et al. A comprehensive review of official discount rates in guidelines of health economic evaluations over time: the trends and roots. Eur J Health Econ. 2022;23(9):1577–1590. doi: 10.1007/s10198-022-01445-x.
- The World Bank. Official exchange rate (LCU per US$, period average) - Saudi Arabia | Data. 2023. https://data.worldbank.org/indicator/PA.NUS.FCRF?locations=SA
- Mauskopf JA, Sullivan SD, Annemans L, et al. Principles of good practice for budget impact analysis: report of the ISPOR task force on good research practices–budget impact analysis. Value Health. 2007;10(5):336–347. doi: 10.1111/j.1524-4733.2007.00187.x.
- Malkin JD, Baid D, Alsukait RF, et al. The economic burden of overweight and obesity in Saudi Arabia. PLoS One. 2022;17(3):e0264993. doi: 10.1371/journal.pone.0264993.
- Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88(1):15–19. doi: 10.2105/ajph.88.1.15.
- Morgenstern H. Uses of ecologic analysis in epidemiologic research. Am J Public Health. 1982;72(12):1336–1344. doi: 10.2105/ajph.72.12.1336.
- Lee E, Bruckner T, Alluhidan M, et al. Forecasting the health burden of overweight and obesity on noncommunicable diseases in Saudi Arabia. In: Overweight and obesity in Saudi Arabia - Consequences and solutions. Washington (DC): World Bank; 2022. http://hdl.handle.net/10986/37723
- Lee I-M, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. doi: 10.1016/S0140-6736(12)61031-9.
- Shan Z, Rehm CD, Rogers G, et al. Trends in dietary carbohydrate, protein, and fat intake and diet quality among US adults, 1999-2016. JAMA. 2019;322(12):1178–1187. doi: 10.1001/jama.2019.13771.
- Coker T, Saxton J, Retat L, et al. The future health and economic burden of obesity-attributable type 2 diabetes and liver disease among the working-age population in Saudi Arabia. PLoS One. 2022;17(7):e0271108. doi: 10.1371/journal.pone.0271108.
- Council of Health Insurance. CHI’s enhanced essential benefit package: prioritizing your health and wellbeing. Riyadh (Saudi Arabia): Council of Health Insurance; 2022.
- Council of Health Insurance. The council of health insurance rolls out updated benefits package and insurance drug formulary. Riyadh (Saudi Arabia); 2022. https://chi.gov.sa/en/MediaCenter/News/Pages/10022022.aspx
- Treatment for Overweight & Obesity - NIDDK. National institute of diabetes and digestive and kidney diseases. https://www.niddk.nih.gov/health-information/weight-management/adult-overweight-obesity/treatment
- Bariatric Surgery Procedures | ASMBS. American society for metabolic and bariatric surgery. https://asmbs.org/patients/bariatric-surgery-procedures
- Losing Weight. www.heart.org. https://www.heart.org/en/healthy-living/healthy-eating/losing-weight.
- Council of Health Insurance. Improving health in saudi arabia through population health management. 2021. https://chi.gov.sa/ResearchLibrary/CCHI%20Population%20Health%20WP.pdf
- World Obesity. Prevalence of obesity. 2023. https://www.worldobesity.org/about/about-obesity/prevalence-of-obesity
- Council of Health Insurance. Value-based health care in Saudi health insurance market. 2022. https://chi.gov.sa/ResearchLibrary/VBHC%20White%20Paper%20Version%20Final.pdf
- Snijder MB, van Dam RM, Visser M, et al. What aspects of body fat are particularly hazardous and how do we measure them? Int J Epidemiol. 2006;35(1):83–92. doi: 10.1093/ije/dyi253.