Introduction
Over the past two decades, healthcare services have been revolutionized by integrating information technology tools into medical settings worldwide, with the aim of improving the quality of care and saving resources. These tools enabled health systems to adopt electronic health records (EHRs), telemedicine platforms, health monitoring devices, and AI-driven diagnostic tools [Citation1,Citation2].
Digital health tools can reduce medical errors, enhance day-to-day medical processes, and increase revenue by simplifying billing processes and attracting new patients with convenient access to care [Citation3]. In addition, these tools have proven their immense value during times of global pandemics as they helped to improve access to care, identify cases early on, and manage the supply chain [Citation4].
In developing countries, nations with limited industrialization and economic engagement where the people typically earn low incomes [Citation5], the digitization of healthcare systems holds the potential to overcome their main shortcomings, which are providing high-quality and affordable care. Akintunde and colleagues conducted a narrative review to identify available literature reporting the implementation of various telemedicine modes in Africa found that digital health can avoid the tragedy of people traveling long distances for regular healthcare services in many African countries, where the scarcity of adequately staffed medical facilities, primarily located in major urban centers [Citation6]. In the United Arab Emirates, several studies have reported that digital health alleviated the burden of COVID-19 on the healthcare system and improved access to care for older patients [Citation7,Citation8]. Furthermore, telepharmacy services and mobile health applications were found effective in reducing unnecessary hospital visits during the pandemic, hence, reducing pressure on the health system and preventing the spread of the virus [Citation9]. For example, Platforms like Teladoc, Doctor on Demand, and Amwell enabled patients to consult with physicians remotely, reducing the need for in-person hospital or clinic visits [Citation10].
Health systems in developing countries, however, encounter enormous technical and legal challenges that hinder the consistent implementation and delivery of these services. These barriers need to be effectively addressed to unlock the full potential of digital health in transforming healthcare in these regions. Therefore, these editorial aims to identify specific technical and regulatory challenges of digital health implementation in healthcare settings in developing countries.
Discussion
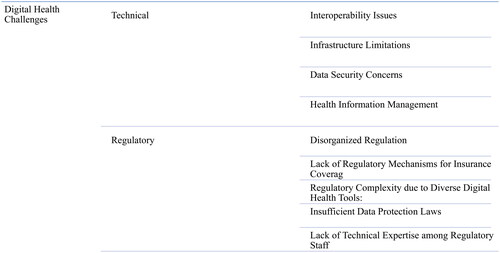
Despite their impact on the development and quality of care in developing countries, technical and regulatory challenges of digital health have been rarely studied in the literature. Addressing these barriers is of utmost importance as they are vital for establishing sustainable, inclusive, and effective healthcare systems. This editorial provides insights into the main technical and regulatory challenges of digital health development, implementation, and functioning in developing countries ().
Figure 1. Categories of technical and regulatory challenges to digital health implementation in developing countries.
Success with digital health tools in developing nations hinges on a coordinated effort among various stakeholders. Governments and policymakers play a lead role, in establishing policies and an environment that fosters the adoption of these tools. Healthcare providers, as primary users of these technologies, offer invaluable feedback, refining the tools to meet specific, on-the-ground challenges. Collaboration between technology developers and local communities often leads to solutions specifically tailored to regional needs, complemented by training initiatives to ensure optimal use. International organizations, such as the World Health Organization, contribute vital technical support and funding. Concurrently, the trust and acceptance of patients and communities amplify the reach of these tools. Meanwhile, continuous research from academia provides an indispensable roadmap, pinpointing challenges and evaluating the success of interventions, ensuring a smooth integration of technology in these regions.
Technical challenges
Technical challenges facing the integration and functioning of digital health in developing nations vary depending on the country, type of technology tool, and the health setting. Overall, there are five major technical issues surrounding this topic; infrastructure limitations, interoperability, data security, health information management, and healthcare workforce capacity and training
Infrastructure and maintenance
Poor infrastructure poses significant technical obstacles that impede the widespread implementation of technology tools in health settings. This includes a lack of access to reliable services like electricity and stable internet connectivity, which creates barriers to implementing and using digital health technologies effectively [Citation11]. This was seen in countries like India and Brazil [Citation12,Citation13]
Healthcare facilities located in remote areas often experience limited access to essential services, limiting device functioning and disrupting daily healthcare operations. Internet connectivity is essential for data transmission, remote consultations, and accessing medical records; however, slow or intermittent connections in certain regions impede the use of cloud-based applications and real-time telemedicine services affecting patient care and decision-making processes [Citation11,Citation14]. For example, in Ethiopia, a systematic review found that poor infrastructure was a major barrier to the use of electronic health records [Citation15].
Moreover, data transmission issues may lead to delays and errors when exchanging important healthcare data, potentially hindering diagnosis and treatment planning processes. Underdeveloped infrastructure also compromises telemedicine and remote monitoring services, making them unreliable or unavailable in areas with connectivity difficulties [Citation16]. For instance, in rural areas of Nigeria, regular power outages make it difficult to operate medical devices, and inconsistent internet prevents real-time consultations or data retrieval [Citation17].
Furthermore, maintenance and support of digital health equipment can be challenging due to limited access to trained technicians and spare parts, leading to prolonged downtime and difficulty replacing faulty devices [Citation18]. Sub-Saharan Africa was particularly affected. Shortages of skilled technicians and spare parts for CT scanners and MRI machines led to extended downtimes. For example, in Tanzanian hospitals, there were reported delays in repairing broken equipment due to a lack of spare parts [Citation19].
Interoperability
One more barrier across developing nations is the lack of interoperability among healthcare facilities and systems. Healthcare providers use disparate electronic health record (EHR) systems or software that cannot easily exchange patient information; as a result, sharing patient records becomes a cumbersome and error-prone process. Furthermore, the lack of interoperability leads to fragmented patient records, making it hard for healthcare professionals to gain an in-depth view of each patient’s medical history; such fragmentation hinders efficiency, delays diagnosis, and may cause medical errors due to incomplete or inaccurate data [Citation18].
Cybersecurity
Inadequate cybersecurity measures and data privacy regulations also present serious threats to digital healthcare systems in developing nations. Healthcare facilities with limited resources may find it challenging to implement effective cybersecurity protocols, leaving their systems exposed to cyber-attacks and breaches. Cybercriminals may take advantage of these weaknesses to gain unauthorized access to confidential patient data, breaching patient privacy and confidentiality and leading to serious consequences, including identity theft, medical fraud, and reputational damage to healthcare institutions. In addition, mishandling patient data may lead to legal and ethical implications, which further impede the adoption of digital health technologies [Citation20]. For example, Indian healthcare faced 1.9 million cyberattacks in 2022 [Citation21]. Dr. Lal PathLabs, one of India’s premier diagnostic chains, inadvertently left a large amount of patient data unprotected on public servers, leading to the breach and exposure of confidential patient data such as names, addresses, and test results [Citation22].
Regulatory challenges
There are several regulatory barriers to the development, implementation, and functioning of digital health in developing countries.
General challenges
In many developing nations, digital health regulations tend to be disorganized, with multiple bodies exerting control without clearly delineated responsibilities. Fragmented regulations can impede the effective use of digital health technologies, leading to potential health risks and market inefficiencies. Technological developments often outpace the regulatory bodies’ abilities to keep up with them, leading to outdated guidelines and legal grey areas that further complicate regulation processes. India, for instance, boasts multiple organizations such as the Central Drugs Standard Control Organization (CDSCO), the Ministry of Health and Family Welfare (MoHFW), and the Ministry of Electronics and Information Technology (MeitY), all playing different roles in regulating digital health. However, due to a lack of an established framework defining their responsibilities, this can sometimes cause confusion, delays, or overlaps in regulation [Citation23].
Additionally, the absence of regulatory mechanisms to ensure that insurance companies cover telemedicine and digital health services makes these potentially beneficial services financially inaccessible to many individuals, despite their promise for improving access to care.
Furthermore, the diverse nature of digital health tools, including mobile health (mHealth) apps, wearables, telemedicine platforms, and electronic health records (EHRs), further exacerbates this complexity in regulatory terms. Another difficult regulatory task is to determine whether these tools fall under medical devices, pharmaceuticals, or another category. This complexity stems from the fact that many of these tools overlap multiple categories and that the categories themselves are evolving with technology. As a result, this lack of clarity leads to uncertainty regarding regulatory processes and requirements for each tool. MHealth applications, for instance, fall into a grey area in the existing regulatory framework. Hence, some can be treated as medical devices while others fall outside of stringent regulation requirements, creating potential gaps that leave patients at risk and data security vulnerable [Citation24].
Another significant challenge in digital health regulation is the shortage of technical expertise among regulatory staff. This shortfall hinders the successful implementation and oversight of digital health technologies. Those responsible may lack an in-depth understanding of the technologies they regulate, making it difficult to fully grasp potential risks and benefits. This often leads to ineffective, misplaced, or overly restrictive regulations that stifle innovation and diminish the potential health benefits of healthcare provision.
Integrity
Digital health enterprises collect and process enormous quantities of sensitive patient data daily. This includes personal identifiers, medical histories, genetic information, and much more, all of which must be securely protected for the sake of patient security. Without adequate data protection laws in place, data breaches pose a high risk that could expose patient information, leading to potentially severe consequences such as identity theft or privacy invasion. If individuals lack trust in the security of their data, they may be disinclined to use digital health technologies, reducing their potential benefits.
Regrettably, some countries in Africa lack comprehensive laws that govern how sensitive health data should be collected, stored, and utilized. Nigeria, one of Africa’s most populous nations, only implemented its first comprehensive data protection regulation in 2019. Efforts at implementation and enforcement are still in their early stages [Citation25]. Such regulatory inadequacies leave sensitive health data vulnerable and can lead to privacy violations, potentially discouraging citizens from adopting digital health technologies due to perceived risk.
Southeast Asia presents another example where many countries are grappling with similar issues. In 2019, a breach in a Singaporean health database led to the unintended disclosure of HIV patient records, underscoring the imperative need for robust data protection measures as more healthcare services transition online [Citation26].
Conclusion
Digital health innovations offer immense promise to transform healthcare provision. However, developing countries face daunting technical and regulatory barriers to their full realization. From infrastructural limitations and interoperability issues to inadequate data security measures and regulatory complexities, these obstacles prevent digital health’s full potential from being realized. Addressing them is not merely beneficial; it is critical for creating sustainable, inclusive healthcare systems with robust infrastructure. Further research must provide context-specific solutions, fostering an enabling environment for the implementation and utilization of digital health in these regions.
Transparency
Declaration of financial/other relationships
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Author contributions
AZA developed the study design, and performed data extraction, manuscript drafting, and reviewing.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgements
None stated.
Additional information
Funding
References
- Patel S, Kongnakorn T, Nikolaou A, et al. Cost-effectiveness of targeted screening for non-valvular atrial fibrillation in the United Kingdom in older patients using digital approaches. J Med Econ. [Internet]. 2023; 26(1):326–334. doi: 10.1080/13696998.2023.217921010.1080/13696998.2023.2179210.
- Whaley CM, Bollyky JB, Lu W, et al. Reduced medical spending associated with increased use of a remote diabetes management program and lower mean blood glucose values. J Med Econ. [Internet]. 2019; 22(9):869–877. doi: 10.1080/13696998.2019.160948310.1080/13696998.2019.1609483.
- Haleem A, Javaid M, Pratap Singh R, et al. Medical 4.0 technologies for healthcare: features, capabilities, and applications. Internet Things Cyber-Physical Syst. [Internet]. 2022;2:12–30. doi: 10.1016/j.iotcps.2022.04.001.
- Lee P, Abernethy A, Shaywitz D, et al. Digital health COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. 2022;2022. doi: 10.31478/202201c.
- Cambridge Dictionary. Developing Country [Internet]. 2023 [cited 2023 Aug 11]. Available from: https://dictionary.cambridge.org/dictionary/english/developing-country.
- Akintunde TY, Akintunde OD, Musa TH, et al. Expanding telemedicine to reduce the burden on the healthcare systems and poverty in Africa for a post-coronavirus disease 2019 (COVID-19) pandemic reformation. Glob Health J. 2021; 5(3):128–134. doi: 10.1016/j.glohj.2021.07.006.
- Abdool S, Abdallah S, Akhlaq S, et al. User acceptance level of and attitudes towards telemedicine in the United Arab Emirates: a quantitative study. Sultan Qaboos Univ Med J. 2021;21(2):e203–9–e209. doi: 10.18295/squmj.2021.21.02.008.
- Jirjees F, Odeh M, Aloum L, et al. The rise of telepharmacy services during the COVID-19 pandemic: a comprehensive assessment of services in the United Arab Emirates. Pharm Pract. 2022;20(2):2634. doi: 10.18549/PharmPract.2022.2.2634.
- Kaliyadan F, A Al Ameer M, Al Ameer A, et al. Telemedicine practice in Saudi Arabia during the COVID-19 pandemic. Cureus. 2020; 12(12):e12004. doi: 10.7759/cureus.12004.
- Fierce Healthcare. This is how Amwell, doctor on demand predict telehealth visits will be different in the future [Internet]. 2020 [cited 2023 Aug 11]. Available from: https://www.fiercehealthcare.com/tech/how-amwell-doctor-demand-predict-telehealth-visits-will-be-different-future.
- Parajuli R, Bohara D, Kc M, et al. Challenges and opportunities for implementing digital health interventions in Nepal: a rapid review. Front Digit Health. 2022;4:861019. doi: 10.3389/fdgth.2022.861019.
- Anjana RM, Pradeepa R, Deepa M, et al. Acceptability and utilization of newer technologies and effects on glycemic control in type 2 diabetes: lessons learned from lockdown. Diabetes Technol Ther. 2020; 22(7):527–534. doi: 10.1089/dia.2020.0240.
- Caetano R, Silva AB, Guedes ACCM, et al. Challenges and opportunities for telehealth during the COVID-19 pandemic: ideas on spaces and initiatives in the Brazilian context. Cad Saude Publica. 2020;36(5):e00088920. doi: 10.1590/0102-311x00088920.
- Challenges in digital medicine applications in under-resourced settings. Nat Commun. [Internet]. 2022;13(1):3020. doi: 10.1038/s41467-022-30728-310.1038/s41467-022-30728-3.
- Yehualashet DE, Seboka BT, Tesfa GA, et al. Barriers to the adoption of electronic medical record system in Ethiopia: a systematic review. J Multidiscip Healthc. 2021;14:2597–2603. doi: 10.2147/JMDH.S327539.
- Jain S, Agarwal A, Bhardwaj A, et al. Remote monitoring and holistic care of home-isolated COVID-19 positive healthcare workers through digital technology during the omicron (B1.1.529) wave: a prospective cohort study from India. Front Public Health. 2022;10:936000. doi: 10.3389/fpubh.2022.936000.
- Adeloye D, David RA, Olaogun AA, et al. Health workforce and governance: the crisis in Nigeria. Hum Resour Health. 2017;15(1):32. doi: 10.1186/s12960-017-0205-4.
- Bressan T, Valdivia-Gago A, Silvera-Ccallo RM, et al. Challenges of design, implementation, acceptability, and potential for, biomedical technologies in the Peruvian Amazon. Int J Equity Health. [Internet]. 2022;21(1):183. doi: 10.1186/s12939-022-01773-710.1186/s12939-022-01773-7.
- Malkin R, Keane A. Evidence-based approach to the maintenance of laboratory and medical equipment in resource-poor settings. Med Biol Eng Comput. 2010;48(7):721–726. doi: 10.1007/s11517-010-0630-1.
- He Y, Aliyu A, Evans M, et al. Health care cybersecurity challenges and solutions under the climate of COVID-19: scoping review. J Med Internet Res. 2021;23(4):e21747. doi: 10.2196/21747.
- Mint. Indian healthcare sector suffers 1.9 million cyberattacks in 2022. [Internet]. 2022 [cited 2023 Aug 11]. Available from: https://www.livemint.com/technology/tech-news/indian-healthcare-sector-suffers-1-9-million-cyberattacks-in-2022-11669878864152.html.
- Techcrunch. Dr Lal PathLabs, one of India’s largest blood test labs, exposed patient data [Internet]. 2020 cited 2023 Aug 11]. Available from: https://techcrunch.com/2020/10/08/dr-lal-pathlabs-exposed-patient-lab-data/.
- Jain D. Regulation of digital healthcare in India: ethical and legal challenges. Healthcare. [Internet]. 2023;11(6):911. doi: 10.3390/healthcare11060911.
- Maaß L, Freye M, Pan CC, et al. The definitions of health apps and medical apps from the perspective of public health and law: qualitative analysis of an interdisciplinary literature overview. JMIR Mhealth Uhealth. 2022; Oct10(10):e37980. doi: 10.2196/37980.
- Babalola O. Nigeria’s data protection legal and institutional model: an overview. Int Data Priv Law. 2022;12(1):44–52. doi: 10.1093/idpl/ipab02310.1093/idpl/ipab023.
- Sharanjit L. Singapore HIV data leak shakes a vulnerable community [Internet]. BBC. 2019 [cited 2023 Jul 23]. Available from: https://www.bbc.com/news/world-asia-47288219.
