Abstract
Objective
44% of Kuwait’s population live with obesity and the health consequences place a significant burden on the public health system. This study provides an assessment of the cost burden of obesity-related comorbidities (ORC).
Methods
A retrospective micro-costing analysis was conducted to quantify the direct cost associated with ORCs. ORCs and their cost categories were informed by a systematic literature review and validated by a local steering committee comprising three experts. Seventy public sector clinicians and eight hospital procurement staff were surveyed to provide healthcare resource utilization estimates and medical resource cost data, respectively. The annual cost of each ORC and the cost drivers were also validated by the steering committee.
Results
Individuals in Kuwait with any single ORC incurred direct healthcare costs ranging 1,748–4,205 KWD annually. Asthma, chronic kidney disease and type 2 diabetes were the costliest ORCs, incurring an annual cost that exceeds 3,500 KWD per patient. Hypertension, angina and atrial fibrillation were the least costly ORCs. In general, costs were driven by drug costs and resources allocated to address treatment-related adverse events.
Limitations
In the absence of an official patient registry in Kuwait, our study provides a conservative estimate of direct costs derived from a nationwide survey. Additionally, the cost estimates in this study assumes that a patient with obesity will only experience one ORC. In reality, multi-morbid states may incur additional costs that are not currently captured.
Conclusions
Our study confirms that ORCs generate a significant financial burden to the public payer. The study provides an economic case for policymakers to recognize the exigency for obesity prevention and control in accordance with the ORC prevalence, and the need for sustainable investments towards body-mass index management to prevent individuals from developing multiple comorbidities.
Introduction
Globally, the prevalence of obesity has increased at an alarming rate, tripling between 1975 and 2016 with over 650 million adults or 13% of the world’s adult population estimated to be living with obesity (with a body mass index of 30 kg/m2 or more) in 2016Citation1. The prevalence of obesity in the Middle East region and the Gulf Cooperation Council (GCC) are no exceptions to this trend. Kuwait, a high-income country in the GCC, is of particular interest as it continually ranks as one of the most obese GCC countries in the world over the years. Obesity amongst Kuwaiti adults has been steadily increasing, with a prevalence of 19% in 1975, to 38% in 2016, and 44% in 2018Citation1–3.
Obesity is a complex and systemic issue with prominent cardiometabolic effects in multiple organ systems and therefore is considered a high-risk factor for non-communicable diseases including diabetes and cardiovascular diseases (CVD). In Kuwait, a cross-sectional study showed that adults with obesity were 1.8 times more prone to have diabetes than adults with a BMI < 25 kg/m2Citation4. Similarly, another cross-sectional study conducted in Kuwait showed that Kuwaiti males and females with a history of diabetes were 1.8 and 2.1 times more likely to have obesity than individuals without a history of diabetes, respectivelyCitation5. The same study also observed a correlation between obesity and heart diseases (myocardial infarction, angina, stroke) where men and women with a history of heart disease are 0.9 and 1.3 times more likely to be obese than individuals without a history of heart disease, respectivelyCitation5. Obesity has also been closely associated with non-alcoholic fatty liver diseaseCitation6, hypertension (patients with obesity are at 0.93–1.11 greater odds of being associated with elevated blood pressure)Citation7, restrictive respiratory impairmentCitation8 and metabolic syndromeCitation9.
In 2016, non-communicable diseases (NCD) accounted for 72% of all deaths in Kuwait – of these, 41% were due to CVDs, 3% due to chronic respiratory diseases and diabetesCitation10. In 2019, per capita healthcare expenditure in Kuwait was US$1,759 (5.5% of gross domestic product (GDP)), and 68% of the total government’s health expenditure i.e. US$1,186 per capita (3.9% of GDP) was funneled to addressing NCDs aloneCitation11,Citation12. Furthermore, overweight and obesity amounted to US$546 per capita (1.7% of GDP) and resulted in an overall economic burden of US$2.3 billion in 2019 (this includes direct medical/non-medical costs as well as indirect costs associated with premature mortality, absenteeism, and presentism). Additionally, there is a negative impact of obesity on factors such as wage and probability of employment where an additional unit of BMI lowers wages by 7% and lowers the share of years employed by 2%Citation13. At the current rate, the economic impact obesity would have on the Kuwaiti population is expected to grow exponentially with projected economic costs of US$4.2 billion in 2030 and US$33.3 billion in 2060Citation2. This raises concerns over the current management systems in place for obesity and obesity-related comorbidities (ORC) and reinforces the need for urgent policy-driven changes to tackle the high prevalence and associated economic burden.
In Kuwait, the vast majority of the services are provided by the Ministry of HealthCitation14. As the primary source of healthcare funding, the Kuwaiti government is faced with increasing fiscal pressure and escalating costs. In 2021, USD 8.9 billion was allocated to paying for public healthcare services, a 12.9% increase from 2020Citation14. Hospital services alone contributed to 91% of the healthcare expenditure, which highlights a high reliance on costly inpatient resources and conversely, low utilization of less costly primary and outpatient care servicesCitation15. A detailed understanding of healthcare resource utilization (HCRU) and cost patterns may provide clarity on the cost drivers and support policymakers with the design of more sustainable, preventative models of care.
Our research contributes to the body of international literature in defining the economic impact of obesity by providing a detailed description of the burden of obesity through the identification and quantification of HCRU and cost components in Kuwaiti public secondary and tertiary health settings. By virtue, our findings may also identify potential care inefficiencies by highlighting health resource components that are overutilized. This may ultimately guide translational research into cost-saving interventions and inform key policies that drive healthcare reform in Kuwait.
Methods
In this study, we sought to estimate all fixed and variable annual direct costs incurred by the average patient with obesity in Kuwait across the care continuum of 10 ORCs. The comorbidities included were aligned with those recently examined in a UK study assessing the effect of weight loss on obesity-related outcomesCitation16. Epidemiologic studies identified high body-mass index (BMI) as a risk factor for type 2 diabetes mellites (T2DM)Citation17–19, CVD, which include heart failure, angina, hypertension, atrial fibrillation and hyperlipidemiaCitation17–21, sleep apneaCitation18,Citation19,Citation22, osteoarthritisCitation19,Citation23,Citation24, asthmaCitation18,Citation19, and chronic kidney disease (CKD)Citation18,Citation19. These 10 ORCs were selected for inclusion in the original study because they encompass a broad range of organ systems (cardiovascular, metabolic, musculoskeletal, respiratory, and renal), and provide comprehensive quantification of the burden of obesity for our analysis.
To overcome limitations in the availability of RWD, a survey-based micro-costing approach was considered the most feasible and accurate method for estimating the cost of ORCs in Kuwait. The approach utilizes HCRU information provided by public sector specialists and unit cost data of every input consumed in the treatment of a particular patient to generate detailed estimates of economic costsCitation25,Citation26. While defined consensus standards and guidelines have yet to be developed for conducting micro-costing studies, the principles are well established in the literature. To date, micro-costing studies have used a wide range of quantity and price data collection methods with varying degrees of precision – data can be collected manually or electronically, prospectively or retrospectively, either from existing hospital records, surveys, billing systems, or trial dataCitation25–29.
Our study was conducted from the perspective of the public payer across secondary and tertiary care settings. Although health information systems in Kuwait has received significant investments and has been implemented in some primary, secondary and tertiary healthcare centers, the adoption rates vary between the centersCitation30. As a result, national databases and registries are currently unavailable in Kuwait due to poor quality of data collected and poor aggregation of data across the care continuumCitation31–33. In the absence of a prospective data source for tracking cost and resource use across all Kuwaiti public care settings throughout the care continuumCitation31–33, we implemented a retrospective micro-costing analysis using a four-tiered approachCitation34,Citation35.
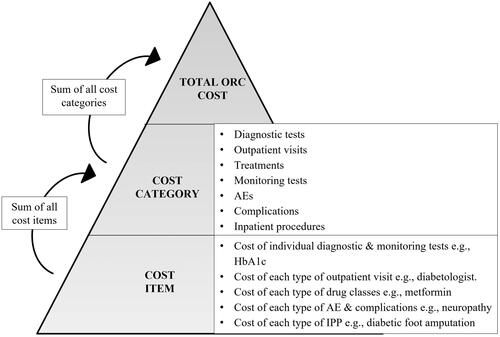
First, ‘cost categories’ (i.e. HCRU and itemized resources within each HCRU category) were identified for each ORC.
Second, the categories were then quantified, where a cost value was assigned to each cost item by weighting utilization against the corresponding unit prices or relevant quantities, as described by Drummond et al.Citation35
Third, cost categories were subsequently aggregated to produce an overall annual cost incurred by an average patient with obesity with an ORC.
Finally, aggregated costs were externally validated against published estimates in literature and by a local steering committee panel comprising a local physician academic and independent industry expert.
Identification of cost categories
The cost categories included in our micro-costing exercise were informed by a methodical development process previously established in a study conducted in Saudi Arabia that examined the national clinical and economic burden of obesityCitation29. Treatment pathways, which included screening, diagnosis, medications, and complications, were identified via a systematic literature review of clinical guidelinesCitation29. Keywords relating to each ORC and ‘guidelines’ or ‘systematic review’ were used to identify relevant references in PubMed and Google Scholar, which were then used to determine the types of healthcare cost parameters relevant to each ORCCitation29. Local validation of all cost categories was then sought from a local steering committee comprising a local academic physician and two independent industry experts.
For each ORC, the following cost categories were included in the analysis: diagnostic tests per patient, scheduled outpatient visits per patient/year, treatments received (including dose, frequency and duration), consumables and/or devices per patient/year, monitoring tests per patient/year, treatment-related adverse events (TRAE) and complications per patient/year (which included inpatient hospitalization, outpatient visits, intensive care unit (ICU) care, emergency room (ER) visits and inpatient procedures per patient/year.
Quantification of cost categories
Cost categories were consolidated in a standardized template and administered to two respondent types from Kuwait’s public sector – clinical specialists and procurement personnel via interviewer-assisted online surveys between April and July 2022. Where required, targeted secondary research was also conducted to validate the HCRU and cost data.
70 experienced specialists practicing at the consultant level were asked to provide HCRU estimates (). All respondents were required to have been working in their current specialist role for at least 3 years and be responsible for the care of at least 10 relevant patients each month. Potential participants were screened to ensure that they met the inclusion criteria and were selected from a mix of geographic regions to provide a fair representation of the local consensus. All respondents indicated that they were practicing out of a public hospital from 1 of the following 6 Kuwait governates – Ahmadi, Capital, Farwaniya, Hawalli, Jahra and Mubarak Al-Kabeer.
Table 1. Respondent type and sample size contributing to HCRU and unit cost estimates for the micro-costing analysis.
8 experienced administrator/procurement staffs were asked to provide the unit cost of medical tests, consultations, consumables/devices, hospital admissions and medical procedures (). All respondents were required to have been working in their current specialist role for at least 3 years and have a knowledge score of at least 4 in each of the cost categories. Potential participants were screened to ensure that they met the inclusion criteria and were selected from a mix of geographic regions. All respondents indicated that they were practicing out of a public hospital from 1 of the following 5 Kuwait governates – Ahmadi, Capital, Farwaniya, Hawalli, Jahra.
Unit costs for treatments for all 10 ORCs were derived from the MOH Pharmaceutical & herbal medicines – Medicine price list (Ministerial Resolution No. 25 of 2022 – Appendix (3) to Ministerial Resolution No. 17 of 2021)Citation36. The price list provides information on product name, manufacturer name, pack size/form, wholesale, and retail prices. The retail prices were extracted for the micro-costing analysis to accurately estimate the burden on the public sector.
Cost calculations
Costs were expressed in 2022 Kuwaiti dinar (KWD) and a foreign exchange rate of 1 KWD = 3.25 USD was assumed where cross-country comparisons were conducted. The cost of each item within each cost category was calculated separately. For all items except treatments, the annual cost per patient per cost item was calculated as: Annual cost per cost item = Percentage (%) of patients utilizing the healthcare resource x Number of healthcare resource units utilized per year × Unit cost.
The annual cost for each drug per patient was calculated as: Annual cost for each drug treatment = Percentage (%) of patients receiving treatment × Average consumption per day × 30 days × 12 months × Unit cost of treatment.
Following the calculation of unit costs for each ORC, the total annual cost per patient per cost categories was determined by summing all cost items (). Finally, the total annual cost per patient per ORC was calculated by summing all cost categories. Cost data are presented as mean values in KWD or % of total costs.
Data validation
Aggregated annual cost estimates were shared with the local steering committee for final validation. The local steering committee comprised of one senior academic physician practicing in Kuwait’s public health sector and a panel of two independent industry experts. Cost drivers and unit cost estimates were also validated by the steering committee. Where necessary, a targeted literature review was also conducted, to corroborate cost data.
Ethics declaration
The study was conducted according to ESOMAR guidelines, and informed consent was required for participation in surveys. Before the commencement of the survey, participants were asked to provide consent for anonymized data to be included in publications and were advised that any adverse events or product complaints raised would be reported to the relevant company. In addition, given that no subject-identifiable data were generated, and the surveillance activities implied no risk or burden for any individuals, the study authors judged that no additional ethical review board permission was required. The study was performed in accordance with the Declaration of Helsinki (1964).
Results
Total annual costs for obesity-related comorbidities
Our cost estimate findings are based on a per patient analysis and the overall prevalence of disease in Kuwait should be considered when quantifying the overall public payer burden for each ORC. Individuals in Kuwait with any ORC incurred an average annual healthcare cost ranging from 1,748 KWD for hypertension and 4,205 KWD for asthma per patient (). Asthma, CKD and T2DM were the top 3 costliest ORCs, incurring an annual cost of 4,205 KWD, 4,167 KWD and 3,921 KWD, respectively. Our study found that costs for these ORCs were mainly driven by high treatment prices associated with disease management and the substantial demands placed on tertiary-care resources in managing AEs.
Table 2. Cost categories and costs (KWD; 2022) related to each ORC.
Hypertension, angina, and atrial fibrillation were the least costly ORCs per patient (). Our study found that these CVD ORCs placed higher demands on outpatient and primary care resources, where the cost of resources are substantially lower than in the secondary or tertiary care inpatient settings. However, it is essential to note that the prevalence of hypertension, angina and atrial fibrillation in the general Kuwaiti population is high, with rates accounting to 25%, 39% and 8%, respectivelyCitation37–39. When considered at scale, these less costly ORCs will invariably pose a comparable overall economic burden to the healthcare system.
Further, our study has also accounted for the cost associated with each ORC as a standalone disease state. If any ORC is left untreated or poorly managed, patients with obesity could progress to or develop other ORCs along the disease spectrumCitation40–48. The resulting cumulative costs creates an incremental burden to public payers in the Kuwait healthcare system.
Cost drivers
To understand the variations in cost contributors across the different ORCs, we analyzed the contributions of various HCRU cost categories to the total annual cost for each ORC ( and ). In general, there was substantial heterogeneity in terms of proportion and absolute cost of each cost category across all 10 ORCs. However, for the top 3 costly ORCs (asthma, CKD and T2DM), the total ORC costs were primarily driven by ‘treatment’ and ‘AE’ costs.
Figure 2. Cost contributors to total healthcare costs across 10 ORCs (%). Abbreviations. ORC, obesity related comorbidity.
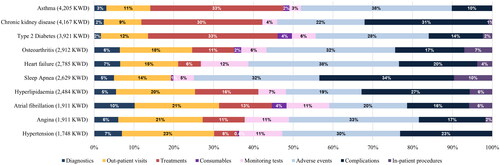
33%, 30% and 33% of the annual cost of asthma, CKD and T2DM, respectively, were driven by treatment costs. Treatments encompass pharmaceuticals and relevant treatment modalities that are used to manage the disease e.g. hemodialysis for patient with end-stage kidney disease.
The costs associated with TRAEs was another major cost driver accounting for 38%, 22% and 28% of total asthma, CKD and T2DM costs, respectively. The costs associated with TRAEs were driven by various factors which include a high recorded proportion of patients experiencing these and high utilization of tertiary care services to manage these TRAEs (i.e. inpatient, intensive care unit and emergency department services).
In the case of CKD, ‘complications’ were also a prominent cost driver which accounted for 31% of total CKD costs. This was due to the high proportion of patients experiencing CKD-related complications and the high utilization of healthcare services in corollary (i.e. outpatient, inpatient, ICU, and emergency department services).
Discussion
Kuwait’s rapid economic growth and urbanization in the last few decades has seen drastic changes to lifestyles i.e. a shift towards an increasingly sedentary lifestyle, leading to unhealthy dietary choices, which has resulted in obesity reaching epidemic proportions. The association of obesity with various diseases is knownCitation4–9,Citation49–51 and its impact on increased HCRU leading to progressive disability, morbidity and mortality is prominentCitation17–19,Citation21,Citation22.
Kuwait’s public healthcare sector accounts for more than 80%Citation12 of the healthcare spending in the country and these circumstances place pressure on the public payer to address the growing clinical, economic, and humanistic burden. National health accounts highlight incremental expenditures, with government health spending as a share of GDP increasing annually each yearCitation12. Further, a vast majority of the healthcare budget has gone towards paying for hospital servicesCitation15,Citation52. Critically, Kuwait’s high healthcare expenditure has not translated into a higher output of health indicators such as life expectancy in contrast to countries with similar or lower healthcare expenditure. Local studies have described contributing factors which include a lack of qualified workforce, patients bypassing primary care interventions for minor ailmentsCitation53 and variations in the quality of services offered at each primary care centerCitation54, which are due to overcrowding, low efficiency and over utilization of limited hospital resources. Our study confirms and illustrates this in the context of the burden of obesity on the Kuwaiti economy by highlighting areas of significant healthcare spending across the ORC care continuum.
In general, major contributors to the annual burden of ORCs were costs associated with TRAEs, complications, and drug treatments. Managing TRAEs and complications requires significant in-hospital care resources which are associated with higher costs, as well as care and manpower resources.
Costs associated with TRAEs is a major driver of the annual disease burden, consistently accounting for at least 19% of the total cost of illness across all 10 ORCs. Researchers have highlighted that medication management issues that result in TRAEs is a critical problem that plagues the under-resourced and overcrowded Kuwaiti public hospital systemCitation55,Citation56. Suboptimal drug management systems which translate to medication errors have led to 21% and 33% of all hospitalizations in tertiary and secondary hospitals, respectivelyCitation55,Citation56.
Costs related to disease complications are also a significant contributor to the total annual cost of ORCs which include CKD, hyperlipidemia, heart failure, sleep apnea and hypertension (accounting for at least 20% of the total annual cost of each ORC). Collectively, complications and TRAEs place significant demands on hospital resources where inpatient, ICU and ER care is needed. Another trend observed is the longer inpatient length of stays (LoS) required to manage these AEs and complications. Our results report an average LoS in the inpatient and ICU setting of 5.1 and 6.9 d, respectively. Our findings are consistent with hospital utilization rates reported in Kuwait for NCDs where patient with obesity and hypertension, diabetes, asthma, heart disease or angina were 0.39, 0.25, 0.32 and 1.69 times more likely to be hospitalized than individuals without any NCDsCitation57. Further, our findings also corroborate the clinical realities of CVDs requiring significant ICU care and longer hospital LoSCitation58.
For CVDs (i.e. hypertension, angina, atrial fibrillation, hyperlipidemia, and heart failure), outpatient visits were also major contributor to the annual burden of disease, accounting for at least 15% of the total annual cost. This is consistent with El-Reshaid’sCitation58 earlier findings on the demands of CVDs on outpatient care resources.
Drug treatment costs are also a significant contributor to the annual cost of illness in Kuwait. Kuwait spent 60% of its total healthcare expenditure in 2015 on medicinesCitation59. This was primarily brought on by the demand for patented drugs which has resulted in low market penetration of generics (22% market share in 2016)Citation14,Citation59. Across the 3 costliest ORCs, asthma, CKD and T2DM, costs associated with drug treatment was a major contributor to the annual burden, accounting for approximately 30% of the annual cost of illness. This was driven by expensive branded biologic agents, erythropoietin stimulating agents (ESA) and basal/GLP-1 combination & GLP-1 agonists for asthma, CKD and T2DM respectively.
In contrast to published literature within the GCC and internationally, our cost estimates for hypertension (5,682 USD vs. 1,497 USD)Citation60, asthma (13,666 USD vs. 108 USD)Citation61 and T2DM (12,742 USD vs. 3,686 USD)Citation62 are comparatively higher. Conversely, our annual cost estimates for angina (6,210 USD vs. 11,540 USD in KSA) and osteoarthritis (9,465 USD vs. 11,354 USD in the United Arab Emirates) are lower than findings reported in neighboring countries respectivelyCitation63,Citation64. Our annual cost estimate for OSA of 8,544 USD per patient was also much lower in comparison to findings reported in the UK which reported an annual cost per CPAP-treated patient of 11,758 USDCitation65. Separately, our study estimates the annual cost of HF to be 9,052 USD, which is in line with results reported by a 2021 KSA study of 9,563 USDCitation66. In addition, the annual cost per patient for hyperlipidemia in our study (8,073 USD) is also within the range of annual cost estimates observed for ‘hypercholesterolemia’ in Germany (5,371 USD) and ‘hypertriglyceridemia’ in the USA (8,567 USD)Citation67,Citation68. It is important to note that direct comparisons to other costing studies are often imprecise and difficult due to the different payer and care setting perspectives adopted. Notably, we observed that many of the published studies either excluded certain cost categories (e.g. diagnostics and monitoring testsCitation61,Citation63,Citation68) or were not comprehensive about the cost items included in the analysis (e.g. drug classesCitation63, AEs and complications under hospitalizationCitation60,Citation63,Citation64,Citation66). Certain published reference studies reported cost estimates from a single center and is therefore not representative of the true burden of illness nationwideCitation62,Citation63,Citation67.
The Kuwaiti government’s commitment to improve the quality of healthcare as part of its Kuwait National Vision 2035, is a policy focus to promote better health for the population at a lower cost. One public health initiative focuses on a ‘Preventive System Against Chronic Non‐Infectious Diseases’, which attempts to prioritize a preventive model over a curative modelCitation69. More policy initiatives in the same vein are needed to target the underlying risk factors (i.e. obesity) to prevent long-term consequences and reduce overall healthcare costsCitation70. To our knowledge, this is the first study to quantify the burden of obesity systematically and comprehensively from the perspective of Kuwait’s public sector secondary and tertiary care settings by evaluating costs and HCRU associated with managing ORCs. Our study hopes to build greater awareness of the potential health system inefficiencies in Kuwait and strengthen the healthcare funding and resource allocation for obesity-related prevention and interventions in accordance with the ORC prevalence and the per-patient costs.
Limitations
Where real world HCRU or unit costs are not available, the use of a micro-costing methodologies and survey-based data sources have been described as an alternative approachCitation28. Our study employs a broad data-collection exercise which comprised a nationwide survey with strict screening criteria for respondents. It is, however, important to note that the costs presented in this study are not derived from an official database or registry and represent our best efforts at obtaining estimates of the annual burden of obesity and its comorbidities. Notwithstanding, these estimates are essential to address the key evidence gap in the absence of comprehensive RWD in Kuwait.
A further limitation to the current study is that the cost estimates lend an assumption that a patient with obesity would only experience one ORC at any given time. Although this provides a good understanding about the cost variations between the ORCs represented in this study, cost synergies arising due to a patient with obesity having 2 or more ORCs in their lifetimeCitation71,Citation72 should be considered for an accurate reflection of the obesity economic burden.
Finally, this study provides a conservative estimate of the direct costs of ORCs and does not consider indirect costs incurred due to absenteeism or loss of productivity.
Conclusion
The findings from our study confirm that ORCs create a substantial financial burden for the Kuwaiti public healthcare system. Inefficiencies observed in secondary and tertiary care HCRU are also highlighted, which notably places further pressure on health expenditures in Kuwait amidst dwindling healthcare resources. Implicatively, leveraging primary care resources and investments in preventative models of care can potentially generate significant cost-savings for the public payer.
Our study has facilitated a comprehensive capture of HCRU and costs across the care continuum in Kuwait. It provides a systematic representation of the economic burden in the country which would otherwise not be available and is instrumental in addressing a major evidence gap in Kuwait. Findings from this study are relevant to individuals, society, policy, and decision makers and can be further used for translational research and targeted interventions against obesity and its ORCs. Our study also highlights a critical need to overcome the current lack of RWD and reliable registry sources in Kuwait. The development of a robust and reliable registry will support decision makers with useful data to develop well-targeted and cost-effective integrated care plans for obesity-related disease management.
System wide multi-stakeholder action is thus urgently needed to consider how resources can be sustainably allocated to focus on obesity control and contain burgeoning costs. Critically, when considered in the broader context of disease prevalence within the Kuwaiti population, our findings provide guidance on the need for a multi-tiered approach to healthcare funding that recognizes the overall burden of disease on the healthcare system.
Transparency
Author contributions
SA, AE, EG and AG contributed equally on study concept and design, interpretation of data and critical revision of the manuscript. SJ and KL also contributed equally to this work on acquisition, analysis, and interpretation of data; statistical analysis, drafting and critical revision of the manuscript. All authors read and approved the final manuscript.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgements
The authors would like to thank all physicians who have provided data for the study. The study team would also like to thank Malvin Kang, Ipsos, Singapore and Mohamed ElTaweel, Novo Nordisk, Kuwait, for their assistance with data cleaning for the analyses and manuscript development.
Declaration of financial/other interests
The authors report no conflicts of interest related to this manuscript.
Data availability statement
All supporting data for the analysis are presented in this manuscript or are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- World Health Organisation. Obesity and overweight [Internet]. 2021 [cited 2023 Feb 3]. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- World Obesity Federation. Global Obesity Observatory – Kuwait. [Internet]. 2018 [cited 2023 Feb 3]. https://data.worldobesity.org/country/kuwait-115/#data_overview.
- Aljulif MZ. Prevalence and reasons of increased type 2 diabetes in Gulf cooperation council countries. Saudi Med J. 2021;42:481–490.
- Alkandari A, Alarouj M, Elkum N, et al. Adult diabetes and prediabetes prevalence in Kuwait: data from the cross-sectional Kuwait diabetes epidemiology program. J Clin Med. 2020;9(11):3420. doi: 10.3390/jcm9113420.
- Weiderpass E, Botteri E, Longenecker JC, et al. The prevalence of overweight and obesity in an adult Kuwaiti population in 2014. Front Endocrinol. 2019;10:1–9. doi: 10.3389/fendo.2019.00449.
- Shaghouli AA, Aranky RM. Prevalence of non-alcoholic fatty liver disease (NAFLD) in obese type two diabetes patients in an endocrine clinic. J Endocr Soc. 2021;5(Suppl 1):A36–A36. doi: 10.1210/jendso/bvab048.070.
- Oguoma VM, Coffee NT, Alsharrah S, et al. Prevalence of overweight and obesity, and associations with socio-demographic factors in Kuwait. BMC Public Health. 2021;21(1):667. doi: 10.1186/s12889-021-10692-1.
- Al-Bader WR, Ramadan J, Nasr-Eldin A, et al. Pulmonary ventilatory functions and obesity in Kuwait. Med Princ Pract. 2008;17(1):20–26. doi: 10.1159/000109585.
- Alkazemi D, Alsouri N, Zafar T, et al. Hypomagnesemia and the metabolic syndrome among apparently healthy Kuwaiti adults: a cross-sectional study. Nutrients. 2022;14(24):5257. doi: 10.3390/nu14245257.
- World Health Organisation. Noncommunicable diseases country profiles 2018 – Kuwait [Internet]. Report No.: 9789241514620. p. 119. 2018 [cited 2023 Mar 3]. https://apps.who.int/iris/handle/10665/274512.
- Elmusharaf K, Grafton D, Jung JS, et al. The case for investing in the prevention and control of non-communicable diseases in the six countries of the Gulf cooperation council: an economic evaluation. BMJ Glob Health. 2022;7(6):e008670. doi: 10.1136/bmjgh-2022-008670.
- The World Bank. The World bank – Current health expenditure per capita (current US$) – Kuwait 2019 [Internet]. 2021 [cited 2023 Mar 3]. https://databank.worldbank.org/source/health-nutrition-and-population-statistics.
- Böckerman P, Cawley J, Viinikainen J, et al. The effect of weight on labor market outcomes: an application of genetic instrumental variables. Health Econ. 2019;28(1):65–77. doi: 10.1002/hec.3828.
- Kuwait Direct Investment Promotion Authority. Healthcare & pharmaceutical sector [Internet]. 2022. https://kdipa.gov.kw/wp-content/uploads/2023/01/Healthcare-Pharmaceutical-Sector.pdf.
- Ministry of Finance, Kuwait. Fiscal year 2020/2021: the general budget [Internet]. 2020. https://www.mof.gov.kw/MofBudget/PDF/Budget21-20eng.pdf.
- Haase CL, Lopes S, Olsen AH, et al. Weight loss and risk reduction of obesity-related outcomes in 0.5 million people: evidence from a UK primary care database. Int J Obes. 2021;45(6):1249–1258. doi: 10.1038/s41366-021-00788-4.
- Singh GM, Danaei G, Farzadfar F, et al. The Age-Specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes. PLOS One. 2013;8(7):e65174. doi: 10.1371/journal.pone.0065174.
- Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523.
- The GBD 2015 Obesity Collaborator. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
- The Emerging Risk Factors Collaboration. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0.
- Khan SS, Ning H, Wilkins JT, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018;3(4):280–287. doi: 10.1001/jamacardio.2018.0022.
- Li C, Ford ES, Zhao G, et al. Prevalence of self-reported clinically diagnosed sleep apnea according to obesity status in men and women: national health and nutrition examination survey, 2005–2006. Prev Med. 2010;51(1):18–23. doi: 10.1016/j.ypmed.2010.03.016.
- Jiang L, Tian W, Wang Y, et al. Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2012;79(3):291–297. doi: 10.1016/j.jbspin.2011.05.015.
- Jiang L, Rong J, Wang Y, et al. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2011;78(2):150–155. doi: 10.1016/j.jbspin.2010.04.011.
- Chapel JM, Wang G. Understanding cost data collection tools to improve economic evaluations of health interventions. Stroke Vasc Neurol. 2019;4(4):214–222. doi: 10.1136/svn-2019-000301.
- Gold MR, Siegel JE, Russell LB, et al. Cost-Effectiveness in Health and Medicine [Internet]. Oxford University Press; 1996 [cited 2023 Aug 3]. https://global.oup.com/academic/product/cost-effectiveness-in-health-and-medicine-9780195108248?cc=au&lang=en&.
- Frick KD. Microcosting quantity data collection methods. Med Care. 2009;47(7 Suppl 1):S76–S81. doi: 10.1097/MLR.0b013e31819bc064.
- Xu X, Lazar CM, Ruger JP. Micro-costing in health and medicine: a critical appraisal. Health Econ Rev. 2021;11(1):1–8. doi: 10.1186/s13561-020-00298-5.
- Alqahtani SA, Al-Omar HA, Alshehri A, et al. Obesity burden and impact of weight loss in Saudi Arabia: a modelling study. Adv Ther. 2023;40(3):1114–1128. doi: 10.1007/s12325-022-02415-8.
- Alhuwail D. Uncovering progress of health information management practices [Internet]. 2021. https://eprints.lse.ac.uk/108584/1/Alhuwail_uncovering_progress_of_health_information_management.pdf.
- Alnashmi M, Salman A, AlHumaidi H, et al. Exploring the health information management system of Kuwait: lessons and opportunities. Appl Syst Innov. 2022;5:1–13.
- Alhuwail D. Information management practices in public tertiary health-care facilities: an empirical investigation from the state of Kuwait. RMJ. 2021;31(1):60–73. doi: 10.1108/RMJ-10-2019-0062.
- Al-Azmi F, Enezi AL, Chowdhury N. R. Users’ attitudes to an electronic medical record system and its correlates: a multivariate analysis. Health Inf Manag J. 2009;38:33–40.
- Špacírová Z, Epstein D, García Mochón L, et al. A general framework for classifying costing methods for economic evaluation of health care. Eur J Health Econ. 2020;21(4):529–542. ‑doi: 10.1007/s10198-019-01157-9.
- Drummond MF, Sculpher MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. 4th ed. Oxford: Oxford University Press; 2015. p. 464. [cited 2023 Aug 3]. https://global.oup.com/academic/product/methods-for-the-economic-evaluation-of-health-care-programmes-9780199665884?cc=au&lang=en&.
- Ministry of health (MOH) Kuwait. Ministerial Resolution No. 25 of 2022 – Appendix (3) to Ministerial Resolution No. 17 of 2021. 2021 [Internet]. ttps://e.gov.kw/sites/kgoarabic/Pages/eServices/MOH/DrugFoodSupplementPrices.aspx#
- Zubaid M, Rashed WA, Saad H, et al. Kuwait acute coronary syndromes registry: baseline characteristics, management practices and in-hospital outcomes of patients hospitalized with acute coronary syndromes in Kuwait. Med Princ Pract. 2007;16(6):407–412. doi: 10.1159/000107732.
- World Health Organisation (WHO). Kuwait-Hypertension Fact Sheet [Internet]. 2023 [cited 2023 Apr 18]. https://cdn.who.int/media/docs/default-source/country-profiles/hypertension/kwt_en.pdf?sfvrsn=a84a0d74_9&download=true
- Khaled A-A, Mohammed B, Faiza A. The prevalence of atrial fibrillation among acute medical admission in Kuwait university hospital in Sana’a city. Clin Cardiol Cardiovasc Med. 2018;2:5–7.
- Kiss D, Veegh W, Schragel D, et al. Bronchial asthma causing symptoms suggestive of angina pectoris. Eur Respir J. 2003;21(3):473–477. doi: 10.1183/09031936.03.02582001.
- Christiansen SC, Schatz M, Yang S-J, et al. Hypertension and asthma: a comorbid relationship. J Allergy Clin Immunol Pract. 2016;4(1):76–81. doi: 10.1016/j.jaip.2015.07.009.
- Tattersall MC, Dasiewicz AS, McClelland RL, et al. Persistent asthma is associated with increased risk for incident atrial fibrillation in the MESA. Circ Arrhythm Electrophysiol. 2020;13:e007685.
- Narala KR, LaLonde TA, Hassan S, et al. Management of chronic coronary disease and acute coronary syndromes in patients with chronic kidney disease. US Cardiol. 2011;8(2):123–131. doi: 10.15420/usc.2011.8.2.123.
- Pugh D, Gallacher PJ, Dhaun N. Management of hypertension in chronic kidney disease. Drugs. 2019;79(4):365–379. doi: 10.1007/s40265-019-1064-1.
- Gadde S, Kalluru R, Cherukuri SP, et al. Atrial fibrillation in chronic kidney disease: an overview. Cureus. 2022;14(8):e27753. doi: 10.7759/cureus.27753.
- Deedwania PC. Management of patients with stable angina and type 2 diabetes. Rev Cardiovasc Med. 2015;16(2):105–113. doi: 10.3909/ricm0742.
- Sun D, Zhou T, Heianza Y, et al. Type 2 diabetes and hypertension. Circ Res. 2019;124(6):930–937. doi: 10.1161/CIRCRESAHA.118.314487.
- Sun Y, Hu D. The link between diabetes and atrial fibrillation: cause or correlation? J Cardiovasc Dis Res. 2010;1(1):10–11. doi: 10.4103/0975-3583.59978.
- Farag YM, Kari JA, Singh AK. Chronic kidney disease in the Arab world: a call for action. Nephron Clin Pract. 2012;121(3–4):c120–c123. doi: 10.1159/000345149.
- Al-Rashed F, Sindhu S, Al Madhoun A, et al. Short sleep duration and its association with obesity and other metabolic risk factors in Kuwaiti urban adults. Nat Sci Sleep. 2021;13:1225–1241. doi: 10.2147/NSS.S311415.
- Malaviya AN, Shehab D, Bhargava S, et al. Characteristics of osteoarthritis among kuwaitis: a hospital-based study. Clin Rheumatol. 1998;17(3):210–213. doi: 10.1007/BF01451049.
- Ministry of health (MOH) Kuwait. National health accounts: health expenditure of most important sectors in the state of Kuwait 2011/2012. Kuwait: Ministry of Health; 2016.
- Seddighi H, Nejad FN, Basakha M. Health systems efficiency in Eastern Mediterranean region: a data envelopment analysis. Cost Eff Resour Alloc. 2022;18:1–7.
- Nashat N, Hadjij R, Al Dabbagh AM, et al. Primary care healthcare policy implementation in the Eastern Mediterranean region; experiences of six countries: part II. Eur J Gen Pract. 2020;26(1):1–6. doi: 10.1080/13814788.2019.1640210.
- Alsaleh FM, Alsaeed S, Alsairafi ZK, et al. Medication errors in secondary care hospitals in Kuwait: the perspectives of healthcare professionals. Front. Med. 2021;8:1–10. doi: 10.3389/fmed.2021.784315.
- Ahmed Z, Saada M, Jones AJ, et al. Medical errors: healthcare professionals’ perspective at a tertiary hospital in Kuwait. PLOS One. 2019;14(5):e0217023. doi: 10.1371/journal.pone.0217023.
- Alibrahim A, AlAjeel A. Noncommunicable diseases and hospital utilization in Kuwait: a generalizable approach using the world health survey. Med Princ Pract. 2022;31(5):445–453. doi: 10.1159/000526673.
- El-Reshaid K, Al-Owaish, R, Diab. A. Hypertension in Kuwait: the past, present and future. Saudi J Kidney Transpl. 1999;10:357–364.
- Abdulsalam Y. Kuwait’s hundred million dollar supply management opportunity [Internet]. 2019 [cited 2023 Dec 3]. https://blogs.lse.ac.uk/mec/2019/01/17/kuwaits-hundred-million-dollar-supply-management-opportunity/.
- Wierzejska E, Giernaś B, Lipiak A, et al. A global perspective on the costs of hypertension: a systematic review. Arch Med Sci. 2020;16(5):1078–1091. doi: 10.5114/aoms.2020.92689.
- Khadadah M. The cost of asthma in Kuwait. Med Princ Pract. 2013;22(1):87–91. doi: 10.1159/000341154.
- Alhowaish AK. Economic costs of diabetes in Saudi Arabia. J Family Community Med. 2013;20(1):1–7. doi: 10.4103/2230-8229.108174.
- Altowaijri A, Alshehri N, Balkhi B, et al. Pcv50 economic burden of major cardiovascular diseases and ischemic stroke in Saudi Arabia: a cost of illness study. Value Health. 2020;23:S495–S496. doi: 10.1016/j.jval.2020.08.541.
- Al-Saleh JA, Albelooshi AA, Salti AA, et al. Burden, treatment patterns and unmet needs of osteoarthritis in Dubai: a retrospective analysis of the Dubai real-world claims database. Rheumatol Ther. 2022;9(1):151–174. doi: 10.1007/s40744-021-00391-z.
- Guest JF, Helter MT, Morga A, et al. Cost-effectiveness of using continuous positive airway pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax. 2008;63(10):860–865. doi: 10.1136/thx.2007.086454.
- Alghamdi A, Algarni E, Balkhi B, et al. Healthcare expenditures associated with heart failure in Saudi Arabia: a cost of illness study. Healthcare. 2021;9(8):988. doi: 10.3390/healthcare9080988.
- Nichols GA, Arondekar B, Garrison LP. Patient characteristics and medical care costs associated with hypertriglyceridemia. Am J Cardiol. 2011;107(2):225–229. doi: 10.1016/j.amjcard.2010.09.010.
- Willich SN, Wegscheider K, Sonntag F. Costs of patients with hypercholesterolemia in Germany. Eur Soc Cardiol. [Internet]. 2007;6. https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-6/Costs-of-patients-with-hypercholesterolemia-in-Germany-Title-Costs-of-patient.
- Gasana J, Vainio H, Longenecker JC, et al. Identification of public health priorities, barriers, and solutions for Kuwait using the modified Delphi method for stakeholder consensus. Int J Health Plann Mgmt. 2021;36:1830–1846.
- Sassi F, Hurst J. The prevention of lifestyle-related chronic diseases: an economic framework. [Internet]. Report No. 32. Paris: OECD; 2008. doi: 10.1787/243180781313.
- Lim Y, Boster J. Obesity and comorbid conditions. StatPearls. [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [cited 2023 Aug 3]. https://www.ncbi.nlm.nih.gov/books/NBK574535/#_NBK574535_pubdet_.
- Pi-Sunyer FX. Comorbidities of overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31(11 Suppl):S602–S608. doi: 10.1097/00005768-199911001-00019.