ABSTRACT
Objective
Previous research indicated that adults with ADHD may have deficits in metacognition, yet the evidence base is scarce. This study aims to explore the existence and nature of metacognitive deficits in adults with ADHD, how psychopathology (such as inattention and depression) may affect metacognition and whether metacognition may impact daily functioning in adults with ADHD.
Method
Forty-six adult patients with ADHD and 46 controls completed questionnaires for metacognition, psychopathology and daily functioning (subjective assessment; self- and informant report). Participants performed two attention tests in a neuropsychological assessment. After test completion, participants were asked to evaluate their performance with the help of a visual aid and this self-evaluation of test performance was compared with their actual test performance (objective assessment).
Results
Patients with ADHD reported large deficits in knowledge of cognition and medium deficits in regulation of cognition compared to controls. Self-evaluation of cognitive test performance revealed no significant deficits. Regression analyses revealed that psychopathology may explain a part of the variation in metacognition. Further regressions indicated that metacognition may account for a significant and meaningful proportion of variance in daily functioning, both self-rated and informant-rated.
Conclusions
Current findings of compromised metacognitive functioning of adults with ADHD suggest that clinicians may not want to rely on patients’ self-reports in the clinical assessment. Inattention predicted impairments in metacognition, pointing toward the importance of attention for awareness and metacognition. Finally, we recommend that metacognition is addressed in the treatment trajectory of patients with ADHD, given that aspects of metacognition were directly linked to impairments in daily functioning as rated by participants and their relatives.
Attention deficit hyperactivity disorder (ADHD) in adulthood is characterized by symptoms of inattention, impulsivity and hyperactivity. Research revealed marked cognitive deficits, especially in attention, memory and executive functions (Fuermaier et al., Citation2015; Schoechlin & Engel, Citation2005). Furthermore, adults with ADHD may experience a wide range of functional impairments in multiple life domains, such as lower educational achievement, lower employment levels and frequent job changes, financial problems, increased substance use, trouble with the law, diminished social networks and increased risk taking behavior such as risky driving (Barkley & Murphy, Citation2010; Kooij et al., Citation2019; Oie et al., Citation2011). Yet, information on which factors contribute to functional impairment in adults with ADHD is still scarce and it is unclear how cognitive impairment may relate to impairments in daily functioning (Barkley & Murphy, Citation2010; Szuromi et al., Citation2013). The influence of metacognition on functional impairment in adult ADHD is worth exploring, as metacognition may affect a wide array of functional outcomes, ranging from performance at school and the workplace to social functioning in various psychiatric disorders but also healthy populations (Hong et al., Citation2015; Krueger et al., Citation2011; Lysaker et al., Citation2011; Williamson et al., Citation2010).
Metacognition is colloquially described as “thinking about thinking”, referring to various cognitive processes by which we understand and regulate our own cognition (Krueger et al., Citation2011), such as self-awareness, self-monitoring and self-regulation (Knouse et al., Citation2005) which may influence adaptive behavior in a range of environments (Eslinger et al., Citation2005). Other conceptualizations emphasize the distinction of “knowledge of cognition” and “regulation of cognition” as central components of metacognition (Flavell, Citation1979; Schraw & Dennison, Citation1994). Knowledge of cognition is defined as the knowledge and awareness we have of our cognitive processes, whereas regulation of cognition refers to our conscious control over these processes (Harrison & Vallin, Citation2018; Schraw & Dennison, Citation1994).
Measuring metacognition is challenging; if a patient has deficits in metacognition, they might be unaware of their cognitive deficits and therefore struggle to report them realistically. Asking an informant to evaluate the patient may circumvent this problem, but the informant’s perspective is also subjective and prone to various biases (Williamson et al., Citation2010). Another approach includes the participant performing a cognitive test and asking the participant to evaluate their test performance, which may then be compared with the normed test result (Williamson et al., Citation2010). This may offer a more objective perspective on the patient’s metacognition. Consequently, it may be important to include both methods in measuring metacognition: on the one hand participants’ self-report of their metacognitive skills (subjective) and on the other hand assessing metacognition based on self-awareness of cognitive test performance (objective).
Very few studies could be found that investigate metacognition in adults with ADHD and most of the ones that are available are based on self- and informant-reports (Manor et al., Citation2012; Moerstedt et al., Citation2015; Prevatt et al., Citation2012). College students with ADHD may underestimate their symptoms on self-reports relative to the clinician’s assessment (Manor et al., Citation2012). A positive illusory bias was demonstrated in college students with ADHD, which signifies that they evaluated themselves more positively than warranted (Prevatt et al., Citation2012). Another study found that patients with ADHD seem to overestimate their symptoms compared with the clinicians’ perspective, yet patients may rate their functional impairments accurately (with some patients showing the reverse pattern), indicating that they may be unaware of a connection between their symptoms and impairment (Moerstedt et al., Citation2015). A few studies could be found that compare the self-evaluations of patients with ADHD with objective markers, such as cognitive test performance and driving simulators (Butzbach et al., Citation2021; Knouse et al., Citation2005, Citation2006). There, a mixed picture emerges, as metacognition of memory may be as accurate in adults with ADHD as in controls (Knouse et al., Citation2006). Deficits were found for metacognition of attention in adults with ADHD, but not for metacognition of executive functions or memory (Butzbach et al., Citation2021). A study exploring self-awareness of driving in adults with ADHD showed that compared to controls, adults with ADHD may overestimate their driving abilities (Knouse et al., Citation2005).
When investigating how metacognition is affected in adults with ADHD, it might be important to explore how different aspects of psychopathology (inattention, depression, anxiety) may influence this relationship, as the lifetime comorbidity rate is 60–80% in adults with ADHD (Kooij et al., Citation2019). Depression and anxiety are the most common comorbidities in adult ADHD, with prevalence rates of 38–42% for depression and 45–47% for anxiety disorders (Chen et al., Citation2018; Kessler et al., Citation2006). Depression in particular may be relevant as previous research indicates that metacognition may be affected by depression (Soderstrom et al., Citation2011). The notion of depressive realism suggests that patients with depression may be less prone to positive biases and therefore evaluate themselves more realistically than people without depression. However, the severity of symptomatology may play an important role as patients with mild depressive symptoms may evaluate themselves more accurately, but with more severe symptoms, this effect disappears (Soderstrom et al., Citation2011). Consequently, to promote understanding of metacognition in adult ADHD, it may be worthwhile to disentangle how different aspects of psychopathology may influence metacognition in adult ADHD.
Although there is a lack of research on the influence of metacognition on daily functioning in adult ADHD, the connection between metacognition and daily functioning is established in the general population and in disorders other than ADHD. In patients with schizophrenia, metacognition impacts quality of life (Lysaker et al., Citation2011) and in patients with dementia, metacognition influences coping, functional outcomes and treatment adherence (Williamson et al., Citation2010). In typically developing children, diminished metacognition impacted real-world behavior problems rated by informants (Krueger et al., Citation2011). Furthermore, even if cognitive functioning is intact, deficits in self-reflectivity may lead to problems at work and hinder growth (Lysaker et al., Citation2011). For example, even if performing well initially, if someone fails to question their interpretations of other persons or situations or fails to reflect on how individual strengths and weaknesses impact the work environment, work performance may suffer (Lysaker et al., Citation2011). Metacognition may have unique implications for optimal daily functioning (Krueger et al., Citation2011), highlighting the importance of investigating metacognition in the clinical context and leading to the proposition that metacognition should become a routine part of cognitive assessments (Krueger et al., Citation2011).
Further evidence for the connection between metacognition and daily functioning in adult ADHD may be derived from research on cognitive deficits and daily functioning. Several studies found that performance on cognitive tests was not related (Oie et al., Citation2011; Szuromi et al., Citation2013) or hardly related (Barkley & Murphy, Citation2010; Potvin et al., Citation2016) to the impairments patients with ADHD report in everyday life. Notably, patients’ subjective evaluation of their cognitive functions may be more closely related to daily functioning (Potvin et al., Citation2016). This may be affected by the type of assessment: cognitive tests may not predict daily functioning as much as questionnaires, as mostly questionnaires are used to measure daily functioning. Potential deficits in metacognition may affect patients’ ability to report their cognitive and daily functioning realistically, yet, patients with ADHD may still be able to notice that they are struggling with their cognition in everyday life. Self-rated executive deficits, for example, in self-discipline and self-motivation, were strongly associated with occupational outcomes (Barkley & Murphy, Citation2010). The self-referential aspect of these deficits and the definition of metacognition emphasizing knowledge and regulation of one’s own cognition, may suggest that metacognition may be an underlying factor for occupational deficits in adults with ADHD. The relevance of metacognition to daily functioning is supported by findings that adults with ADHD may have deficits in self-awareness of driving abilities (Knouse et al., Citation2005) and may have more adverse driving outcomes than controls (Fuermaier, Tucha, Evans, et al., Citation2017). Despite of this, there is a lack of research exploring how metacognition may affect daily function in adults with ADHD.
This study aims to 1) examine metacognition in adults with ADHD based on a combination of subjective and more objective methods, 2) explore if metacognition is related to comorbid symptomatology, and 3) investigate if metacognition may predict daily functioning. As previous research indicated impairments in metacognition based on self-reports, we expect adults with ADHD to report deficits in metacognitive abilities relative to controls (Manor et al., Citation2012; Moerstedt et al., Citation2015; Prevatt et al., Citation2012). Because the evidence base for metacognitive deficits based on cognitive test performance is mixed (Knouse et al., Citation2005, Citation2006) it will be examined if deficits in metacognition can be found in self-evaluations of cognitive test performance. Next, it will be explored whether impairments in metacognition relate to psychopathology (ADHD, anxiety, depression) and we expect that ADHD symptomatology influences metacognition. As Soderstrom et al. (Citation2011) demonstrated that depression seems to influence metacognition, one may expect that depression may relate to metacognition in the present study. Finally, it will be explored if metacognition contributes to daily functioning (both self- and informant-rated) and one may expect metacognition to exert a small effect on the complexity of functional impairments. Implications of findings for the clinical assessment of adult ADHD will be discussed in order to derive suggestions if metacognition should constitute a regular part of the clinical evaluation of adult ADHD.
Method
Participants
Patients with ADHD
Forty-six adult patients with ADHD participated in the assessment. Clinicians of the neuropsychology department of the SRH Clinic Karlsbad-Langensteinbach, Germany conducted a structured clinical interview based on DSM-5 criteria (American Psychiatric Association, DSM-5 Task Force, Citation2013) with each patient. This interview included establishing a history of ADHD symptomatology in childhood and the presence of current ADHD symptoms, in addition, clinicians assessed whether any comorbid diagnoses may be present. Further objective information was gathered to support the diagnostic evaluation such as evidence from school reports, failure in academic and/or occupational achievement and if possible from multiple informants (e.g., employer evaluation, partner or parent-reports). Patients were included based on their willingness to participate, diagnosis of adult ADHD and being at least 18 years of age. Exclusion criteria were (a) neurological disorder including head injury, (b) medications affecting the central nervous system (except medications for ADHD and antidepressants), (c) schizophrenia or acute psychosis, (d) estimated verbal IQ below 85 and (e) noncredible symptom report and performance based on scoring above the cut–off values on two established measures of symptom and performance validity, the Groningen Effort Test (GET, cutoff value > 1; Fuermaier et al., Citation2016; Fuermaier, Tucha, Koerts, et al., Citation2016) and the Infrequency Index of the Conners Adult ADHD Rating Scale (CAARS, cutoff value >21; Conners et al., Citation1999; Suhr et al., Citation2011). As several patients were treated with medications for ADHD (stimulant or nonstimulant drugs; N = 5) and/ or antidepressants (N = 12) and these medications are common in the ADHD patient population (Wilens et al., Citation2011), these patients were not to excluded as otherwise the sample may be less representative of adult patients with ADHD in general. To minimize the effects of medications for ADHD, patients were asked not to take their medication on the assessment day. Characteristics of the participants are presented in . Based on the DSM-5 diagnostic criteria for ADHD, 19 patients met the criteria of the predominantly inattentive symptom presentation, 1 the hyperactive-impulsive presentation and 26 the combined presentation. Furthermore, 34 patients with ADHD received one or more comorbid diagnoses, i.e., mood disorders (N = 23), anxiety disorders (N = 16), substance dependency (N = 3), eating disorders (N = 2), personality disorders (N = 2), migraine (N = 2), autism spectrum disorder (N = 1), psychosomatic complaints (N = 1), restless legs syndrome (N = 1), obsessive compulsive disorder (N = 1) and essential tremor (N = 1).
Table 1. Characteristics of patients with ADHD and controls (mean ± standard deviation)
Controls
Forty-six control individuals participated in the assessment. Inclusion criteria were willingness to participate in the study and being older than 18 years of age. Exclusion criteria were as described for the patient group, with the additional criteria of (a) current psychiatric or psychological disorders and (b) past diagnosis of ADHD and/or scoring above the cutoff values on both self-report scales assessing retrospective (Wender Utah Rating Scale > 30) and current ADHD symptoms (ADHD self-report scale > 18). To ensure that the two groups were roughly comparable in demographic characteristics, each of the patients with ADHD was matched with a control participant that was similar in age, IQ, educational level and gender.
After matching was completed, the groups (46 patients with ADHD and 46 controls) did not differ significantly in age (t(90) = .63, p = .530), vocabulary (t(90) = −1.00, p = .319), educational level (U(92) = 882.50, p = .159) and gender (χ2(1) = 1.57, p = .210). In line with the diagnostic status, patients with ADHD scored significantly higher in current (t(90) = 12.92, p < .001) and childhood symptomatology (t(90) = 10.48, p < .001) as well as depressive symptomatology (t(90) = 7.30, p < .001).
Materials
This study was part of a larger research project in which participants underwent an extensive neuropsychological assessment (Butzbach et al., Citation2021). Self- and informant-reports as well as neuropsychological tests were used to identify cognitive deficits and impairments. Only measures and procedure which are relevant for the current study are described below.
Questionnaires
Anamnesis
Basic demographic information and participants’ medical history were recorded with a short self-composed questionnaire. Participant indicated their age, gender, highest educational level achieved (codes: 0 = university degree; 1 = university entrance qualification; 2 = vocational degree; 3 = highschool; 4 = basic mandatory schooling; 5 = none), occupation, history of medical and psychological disorders and any medical treatment.
Beck’s Depression Inventory (BDI)
Depressive symptomatology was assessed with Beck’s Depression Inventory (Beck et al., Citation1988). The BDI includes 21 items assessing symptoms and attitudes characterizing depression. Items are rated based on the severity of the symptoms and range from 0 to 3, with statements indicating varying intensity. A sum score is computed by summing up the responses to all items, with higher scores indicating more impairment. Based on the current sample, Cronbachs’α was .73.
State-Trait Anxiety Inventory (STAI)
Anxiety was measured with the STAI (Spielberger et al., Citation1983), which distinguishes between anxiety as a trait and as a state. It includes 20 items for state anxiety and 20 items for trait anxiety. Items are scored on a 4-point Likert scale ranging from 1 (“almost never”) to 4 (“almost always”). Separate sum scores are computed for state and trait anxiety by summing up responses for each subscale, with higher scores indicating more impairment. Based on the current sample, Cronbachs’α for state anxiety was .94 and for trait anxiety .94 as well.
ADHD symptom report
To quantify the extent of symptoms, the Wender Utah Rating Scale (WURS-K; Ward et al., Citation1993) was used to assess childhood ADHD symptomatology and includes 25 items on a 5-point Likert scale. In addition, current ADHD symptoms were measured with the ADHD Self-Report Scale (ASRS; Adler et al., Citation2006; Kessler et al., Citation2005) including 18 items on a 4-point Likert scale. (American Psychiatric Association, Citation1994; Rösler et al., Citation2008). For both WURS-K and ASRS, higher scores are indicative of more impairment. The long version of the CAARS (Conners et al., Citation1999) was employed to quantify adult ADHD symptomatology based on DSM-IV criteria for ADHD and to screen for non-credible responding (Suhr et al., Citation2011). The CAARS includes 66-items on a 4-point Likert scale (ranging from “0 = not at all/never” to “3 = very much/very frequently”), which can be divided into eight subscales. In addition, the Conners Infrequency Index (CII; Suhr et al., Citation2011) is composed of items only very infrequently endorsed by genuine patients. A sum score of 21 or higher indicates that the participant may not have responded in a credible manner. Of further interest were the DSM Inattention and DSM Hyperactivitiy-Impulsivity subscales, with higher scores indicating more impairment. Based on the current sample, Cronbachs’α was .94 for DSM Inattention and .77 for DSM Hyperactivitiy-Impulsivity.
Metacognitive Awareness Inventory (MAI)
Metacognitive awareness was measured with the MAI (Schraw & Dennison, Citation1994), as it may be able to capture subtle deficits in metacognition and its 2-factor structure (knowledge and regulation of cognition) is validated (Craig et al., Citation2020). Each of the 52 items is a statement describing various aspects of metacognitive awareness. Participants indicate whether the statements apply to them by checking either “true ‘or ‘false’. The MAI is divided in two topics, the first is ‘Knowledge of Cognition’, containing three subscales: declarative knowledge, procedural knowledge and conditional knowledge. The second topic is ‘Regulation of Cognition’, including five subscales: planning, information management strategies, comprehension monitoring, debugging strategies and evaluation. For each item endorsed with ’true” a point is given and sum scores are computed for each subscale, with higher scores indicating better meta-cognitive awareness. Based on the current sample, Cronbachs’α was .80 for Knowledge of Cognition and .85 for Regulation of Cognition.
Weiss Functional Impairment Rating Scale (WFIRS)
Impairments in everyday functioning were assessed with the WFIRS (Weiss et al., Citation2007). Both a self-report and an informant-report version of the WFIRS were used. For the informant-report, relatives were asked to evaluate to what extent a given statement applied to the participant. The WFIRS contains 70 items to be rated on a 4-point Likert scale ranging from 0 (= never or not at all) to 3 (= very often or very much) and “not applicable” is given as an additional answer option. Items are grouped into 7 subscales pertaining to different life domains (family, work, school, life skills, self-concept, social and risk). For each subscale, items checked as “not applicable” are not included in the calculation, thus average scores are computed by adding up the responses for each item rated from 0–4 and then averaging by the number of items. In addition, a total score is computed by adding up the subscale scores. Higher scores indicate more impairment. Based on the current sample, Cronbachs’α was .97 for the self-rated total WFIRS and .97 for the informant-rated total WFIRS.
Verbal intelligence estimate (vocabulary skills)
Verbal intelligence was estimated with the Multiple Choice Vocabulary Test (MWT-B; Lehrl, Citation1995). As previous research indicated that this measure correlates well with traditional measures of intelligence, such as the WAIS full IQ score, it was chosen as a verbal IQ estimate (Lehrl et al., Citation1995). In this short, 37- item test of vocabulary skills participants were asked to select a real word which was mixed with 4 made-up words. For each correctly selected word, participants receive one point and by summing up these points, a total score is computed which is compared to a normative sample and transformed into a Verbal IQ estimate.
Cognitive assessment of attention
Selective attention
The Perception and Attention Functions: Selective Attention Test (WAFS) of the Vienna Test System (Schuhfried, Citation2010; Sturm, Citation2017a) was employed to measure selective attention, which refers to the ability to assign attentional resources to target stimuli and to inhibit reactions to distracting stimuli. In this test, circles, squares or triangles were presented (1500 ms) consecutively on a computer screen. In some cases, the figure changed to a lighter or darker shade of gray, more often the figure remained the same shade. This change in shade represented the target stimulus upon which participants had to press a button as fast as possible. Importantly, when a triangle changed shade, participants were asked not to react. The duration of this task was 5 minutes. The mean reaction time in milliseconds was the variable of interest for this test.
Vigilance
The Perception and Attention Functions: Vigilance Test of the VTS (Schuhfried, Citation2010; Sturm, Citation2017b) was administered to assess vigilance. In this task, participants needed to be alert over a prolonged period of time and respond to a very infrequently occurring target. During this 15-minute test, participants were shown squares in the center of a computer screen. Squares were presented consecutively for 1500 ms each with an interstimulus interval of 500 ms. The target stimulus was defined as a square becoming darker, upon which participants had to press a button as fast as possible. The color change would occur after 500 ms. Notably, the target stimuli made up only 5% of stimuli. The main variables of interest were mean reaction time in milliseconds and omission errors.
Self-evaluation of cognitive test performance
A visual aid representing a normal distribution made out of blue stick figure people was used to aid the self-evaluation of cognitive performance (Supplement A). Below the bell-shaped display of people, a line is printed with numerical markings (“1” and the verbal description “the worst”, “5”, “10”, “25”, “50” with the description “average”, “75”, “90”, “95”, “99” with the description “the best”), which represent the percentile ranks. Importantly, the numerical markings are unevenly spaced to match a normal distribution within which points at the extremes are spread out further than points at the center. Above the normal distribution a reminder specifies that participants need to compare themselves with 100 people of their age. Two versions of the visual aid were used, one as described above, and the other including two example persons to demonstrate how to use the visual aid. Person 1 is a female printed in red and positioned a bit to the right of the 75th percentile marking. A red arrow is pointing at this person and underneath the description “Person 1 Rank 81” is added. Person 2 is a male printed in green located slightly to the right of the 10th percentile marking. A green arrow with the description “Person 2 Rank 14” is printed underneath the person.
To ensure that participants understood how to use the visual aid, a standardized instruction was read out to the participants and both visual aids were shown to the participants. In the instruction, the rationale of a normal distribution was explained, i.e., how most people perform averagely and are thus clustered around the center of the distribution and how only a few people perform very well or very badly and form the extremes. It was mentioned how this relates to the numerical markings of the percentile ranks printed underneath the visual aid. Then the example persons were shown to explain the concept of percentile ranks. The participants were given the opportunity to ask questions and had to answer two practice questions. To check whether the participants understood the concept of percentile ranks, they were asked how many people perform worse and how many better than them based on the rank they indicated. If a wrong answer was given, the rationale of percentile ranks is explained to them again.
Procedure
Fifty-four patients with ADHD were referred by psychiatrists, neurologists and other professionals or self-referred to the SRH Clinic and considered for participation in the study. Eight patients with ADHD were excluded as they were not fulfilling the aforementioned inclusion and exclusion criteria. A community sample of 101 individuals was recruited based on word of mouth and contacts of the researchers involved, of which 17 were excluded. After matching, 46 patients with ADHD and 46 controls were included in the analysis. Participants were assessed individually with the assessment taking place at the SRH clinic Karlsbad-Langensteinbach for patients with ADHD. For controls, the assessments took place at home in a quiet room and experimenters were trained to remove distractions as much as possible (switch phone off, ask household members to not disturb, etc.). Participants were sent questionnaires for their relatives beforehand and asked to bring them along to the assessment. Before the start of the assessment, each participant gave written informed consent. Participation was voluntary and not rewarded. Next, the instruction of the self-evaluation of cognitive performance was read out to participants and the visual aid was introduced. Once the participants answered the practice questions appropriately, the neuropsychological tests were administered. Participants completed the respective test and then were asked to reflect on their test performance and evaluate how well they performed relative to their same aged peers (postdiction self-evaluation of cognitive performance). The self-evaluation questions were standardized to tailor them to task parameters and were phrased to relate to salient characteristics of the tests, so that participants knew which aspects to evaluate themselves on. For the WAFS (outcome variable: reaction time) the question was: “Compared to others, how fast were you in this test?”. And for the WAFV (outcome variables: reaction time and omission errors) the questions were: “Compared to others, how fast were you in this test?” and “Compared to others, how accurately did you react to the color changes?” Participants could take a short break if needed. Lastly, the participants were asked to fill in the questionnaires. After completion, participants were debriefed and thanked for their participation. The duration of measures as described above was about 1 hour, whereas the whole assessment of the larger study was about 2.5 hours in total per participant.
Ethics statement
Ethical approval (S-383/2010) was obtained from the ethics committee of the medical faculty of the University of Heidelberg, Germany. The study was conducted in adherence with the ethical standards of the Helsinki Declaration.
Statistical analysis
Firstly, different measures of metacognition were compared between adults with ADHD and healthy controls. The assumption check indicated that the homoscedasticity assumption was violated, so nonparametric analyses were used. Mann-Whitney U tests and effect sizes were computed to compare patients and controls on all MAI subscales. As eight group comparisons were computed, a Bonferroni correction (p = .05/8) was applied to control for alpha error inflation, resulting in an alpha level of .006. Cohen’s r was selected as this effect size measure does not rely on parametric assumptions. Based on Cohen (Citation1988), an effect of 0.1 was classified as small, 0.3 as medium and 0.5 as large. To explore whether deficits in metacognition could be observed in self-evaluations of neuropsychological test performance, discrepancy scores were calculated. For each variable, the normed test result (percentile rank indicated by age-based norms) was subtracted from the self-evaluated percentile rank. Furthermore, the discrepancy scores of each variable was averaged to a domain discrepancy score of attention. Mann-Whitney U tests and effect sizes were used to compare the discrepancy scores of patients with ADHD and controls to evaluate whether patients with ADHD demonstrate deficits in metacognition. As four group comparisons were computed, a Bonferroni correction (p = .05/4) was applied resulting in an alpha level of .0125.
Secondly, linear regressions were computed in order to explore the impact of psychopathology on metacognition. On scatterplots, PP-plots and QQ-plots, the assumptions of linearity, normality and homoscedasticity of the residuals were largely met. Multicollinearity was checked and the variance inflation factor (VIF) was well in the acceptable range. To investigate metacognition and symptomatology from a dimensional perspective (Bitto et al., Citation2017; Katzman et al., Citation2017) and to avoid a restricted range of scores, the whole sample was used. On the condition that patients and controls significantly differed on a measure of metacognition (attention discrepancy score, MAI knowledge of cognition scale and MAI regulation of cognition), linear regressions were computed, separately for each outcome variable (with the measure of metacognition as the outcome). Predictors for these regressions were measures of psychopathology; for depression the BDI total score, for ADHD symptomatology the DSM inattention and the DSM hyperactivity/impulsivity subscales of the CAARS and for anxiety the state and trait subscales of the STAI.
Thirdly, the potential impact of metacognition on daily functioning was also investigated through linear regression analyses. Residuals and VIF were checked and assumptions for linear regression were sufficiently met. In order to investigate metacognition from a dimensional perspective and to avoid a restricted range of scores, also for this analysis the whole sample was used. Two regression models were computed, one with self-rated daily functioning (WFIRS total score) as the outcome variable and the other with daily functioning of the participant as rated by an informant (I-WFIRS total score) as the outcome. For both regressions, measures of metacognition (attention discrepancy score, the MAI knowledge of cognition scale and the MAI regulation of cognition) were entered as predictors if a difference between patients and controls was found for the metacognition measure.
Finally, to gain a more comprehensive understanding, the dimensional analyses were supplemented by categorical analyses: in exploratory analyses additional regression models were computed that include all predictors and outcomes as stated above but that were calculated separately for the ADHD and control group. These supplemental analyses were conducted as an explorative perspective on whether metacognition may have a diverging relationship to psychopathology and daily functioning in patients as compared to controls.
Results
Descriptives of all variables used in the analyses are displayed in . Adults with ADHD reported lower metacognitive abilities than controls for all MAI subscales, with a small to medium effect for comprehension monitoring (p= .005; r= .29) and medium effects for procedural knowledge (p< .001; r= .38), information management (p = .001; r= .35), debugging (p= .004; r= .30) and evaluation (p= .001; r= .34). Large effects were found for declarative knowledge (p< .001; r= .73), conditional knowledge (p< .001; r= .57) and planning (p< .001; r= .53). For the comparisons between patients with ADHD and controls on self-evaluations of cognitive test performance, no significant effects were found and effect sizes were small.
Table 2. Descriptives (means and standard deviations) of all variables used in the analyses
A post-hoc power analysis was conducted with G*Power (Faul et al., Citation2007) to evaluate whether power was sufficient in the present study. With an alpha level of 0.05, power was good for most comparisons, i.e., .99 for knowledge of cognition, .88 for regulation of cognition, .59 for metacognition of test performance, .99 for psychopathology, .99 for self-rated daily functioning and .99 for informant rated daily functioning, but as we wanted to minimize the risk of alpha errors an alpha level of 0.006 was chosen, which comes at the expense of beta errors and lower power: .98 for knowledge of cognition, .61 for regulation of cognition, .26 for metacognition of test performance, .95 for psychopathology, .97 for self-rated daily functioning and .99 for informant-rated daily functioning.
Secondly, linear regression analyses were conducted to determine whether psychopathology (ADHD symptomatology, depression, anxiety) may predict impairments in metacognition. There was no significant difference (p = .053) between patients with ADHD and controls in the attention discrepancy score, so no regression model was calculated for this outcome variable. The regression model including MAI knowledge of cognition as an outcome variable and depression (BDI), inattention (CAARS DSM Inattention), hyperactivity-impulsivity (CAARS DSM HypImp), state anxiety (STAI State) and trait anxiety (STAI Trait) as predictors was statistically significant (R2 = .509, F= 15.96; p< .001). displays the standardized coefficients β and significance levels of predictors for the regression models. A significant model was found predicting MAI regulation of cognition on the basis of measures of psychopathology (R2 = .354, F= 8.45; p< .001). With the exception of inattention (CAARS DSM Inattention), which was a significant predictor of MAI knowledge of cognition in the first model and MAI regulation of cognition in the second, none of the other potential predictors had a significant contribution to either model.
Table 3. Regression coefficients for the models predicting MAI Knowledge and MAI Regulation in the whole sample
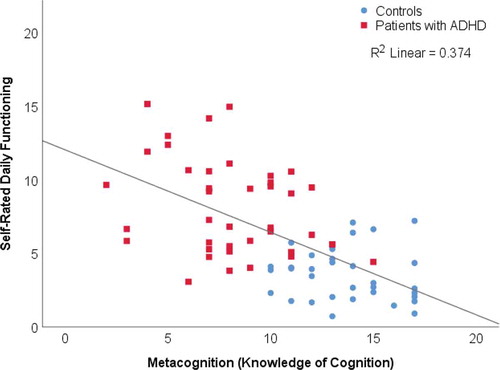
Thirdly, regression analyses were computed to investigate if self-reported metacognition may predict daily functioning (WFIRS). A model with self-rated daily functioning as an outcome and MAI knowledge of cognition and MAI regulation of cognition as predictors was significant (R2 = .378, F= 21.31, p= <.001.). Standardized coefficients β and significance levels of predictors are shown in . MAI knowledge of cognition was a significant predictor of self-rated daily functioning (, β = −.667, p< .001). MAI regulation of cognition was not significantly contributing to the model (β = .089, p = .466).
Table 4. Regressions metacognition and daily functioning
Figure 1. Knowledge of cognition and self-rated daily functioning in patients with ADHD and controls
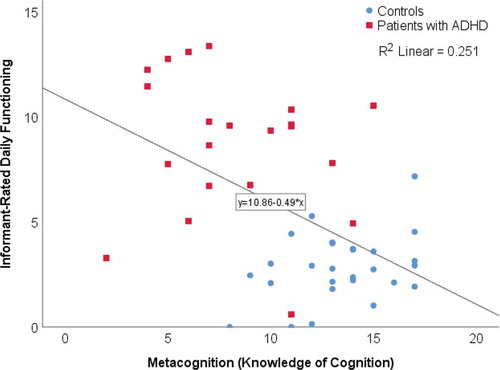
A significant model was found predicting informant-rated daily functioning (I-WFIRS) on the basis of MAI knowledge of cognition and MAI regulation of cognition (, R2 = .257, F = 7.78, p = .001). Only MAI knowledge of cognition made a significant contribution to this model (, β = −.447, p = .006). MAI regulation of cognition was not significant (β = −.096, p = .541).
Figure 2. Knowledge of cognition and informant-rated daily functioning in patients with ADHD and controls
Finally, the regression analyses to explore whether psychopathology influences metacognition and whether metacognition can predict daily functioning were computed separately for patients with ADHD and controls (Supplement B). In the patient group, a significant model was found predicting the Attention domain DS on the basis of measures of psychopathology, with the BDI, CAARS inattention, CAARS hyperactivity and STAI trait explaining a significant proportion of variance. Furthermore, CAARS inattention significantly contributed to the explanation of MAI regulation of cognition in patients with ADHD. None of the other regression models reached statistical significance. To summarize, in the patient group, psychopathology could explain a significant proportion of variance in self-evaluated metacognition based on cognitive test performance and self-rated regulation of cognition, whereas in the control group, these regression models were not statistically significant.
Discussion
The aim of this study was threefold. First, metacognition in adults with ADHD was examined based on a combination of subjective and objective methods, and impairments in metacognition were found in adults with ADHD for self-reports (subjective), but not for self-evaluation of cognitive test performance (objective). Second, it was explored if metacognition is related to comorbid symptomatology, which was the case for inattention but not anxiety or depression. Third, it was investigated if metacognition may predict daily functioning and indeed metacognition could predict both self- and informant-rated daily functioning.
Adults with ADHD were expected to report deficits in metacognition relative to controls. In line with this prediction, significant deficits were found in all self-rated aspects of metacognition in patients with ADHD compared to controls (). For knowledge of cognition, this effect was large (r = .70) and for regulation of cognition it was medium to large (r = .47). Thus, patients with ADHD experience problems in being aware of and reflecting on their own cognitive functioning (knowledge of cognition). Furthermore, patients with ADHD report deficits in regulation of cognition compared to controls, particularly in metacognition of planning. An individuals’ ability to plan may be affected if this person is not monitoring (noticing the need for planning) and regulating their cognition (developing an appropriate plan under consideration of goals) sufficiently. This finding of self-reported metacognitive deficits builds up on previous literature indicating metacognitive deficits in adult ADHD: overestimation of driving abilities in adults with ADHD (Knouse et al., Citation2005), low self-awareness of symptoms in college students with ADHD (Manor et al., Citation2012), overestimation of work and driving behaviors in college students with ADHD (Prevatt et al., Citation2012) and overestimation of symptoms in patients with ADHD (Moerstedt et al., Citation2015). Differences in whether over- or underestimations are found may be influenced by methodology, e.g., which domains are assessed (Butzbach et al., Citation2021) and whether ratings are general or specific (Prevatt et al., Citation2012). The present study is the first to directly ask patients with ADHD to reflect on their own metacognitive abilities (rather than reflecting on their symptoms etc.). The problems patients with ADHD experience in reflecting on their own cognitive abilities may be relevant for the diagnostic process. Clinicians’ evaluations largely rely on patients’ report of their symptoms, which may be distorted due to deficits in self-awareness, highlighting the need for additional outside information (e.g., informants, public records on driving, high school evaluations).
The use of self-reports to assess metacognition may raise concerns, as someone who has a deficit in metacognition may lack insight into this deficit. In studies that assess metacognition by asking patients with ADHD to evaluate their symptoms and then compare this evaluation with an informants perspective, one may indeed question the validity of patients’ evaluation, as they were shown to lack awareness of their symptoms (Manor et al., Citation2012; Moerstedt et al., Citation2015; Prevatt et al., Citation2012). However, although the MAI employs a self-report format, the conceptual approach is different. Rather than asking patients with ADHD to evaluate their symptoms or cognitive functioning, patients are encouraged to reflect on their own metacognitive processes. The MAI includes items such as “I set specific goals before I begin a task.” or “I find myself pausing regularly to check my comprehension” (Schraw & Dennison, Citation1994). This format may enable patients with ADHD to report problems in their metacognitive functioning as they indicate that the statements may not apply to them. Thus, this type of self-reported metacognition may provide clinicians with a perspective on how patients view their own metacognitive abilities (Craig et al., Citation2020).
Furthermore, it was explored if deficits in metacognition could be found in self-evaluations of cognitive test performance. No significant difference between patients with ADHD and controls was found, yet the small effect suggests that patients with ADHD may have subtle deficits in self-awareness of cognitive test performance. This aligns with findings of Knouse et al. (Citation2006), who found no evidence for deficits in metacognition of memory in adult ADHD. Yet, this finding contrasts an earlier study by Butzbach et al. (Citation2021) who found a difference between patients with ADHD and controls in metacognition of attentional functions. Importantly, both in our current and previous study (Butzbach et al., Citation2021), the size of the effect was small and the difference in whether to obtain statistical significance or not may be due to low power. Moreover, difference scores may be less reliable, as a given difference score includes the error variance of each original variable (Schmand, Citation2019). The nonsignificant and small effect found for self-evaluations of cognitive test performance stands in stark contrast to the large deficits found for self-reported metacognition. Patients with ADHD may struggle to evaluate their deficits in cognitive tests, as it might be unclear to them how the test relates to real life challenges they experience. This points to generalizability issues of neuropsychological test performance (Chaytor & Schmitter-Edgecombe, Citation2003) and concerns to what extent cognitive tests capture the difficulties patients experience in their everyday lives. In addition, it might be possible for someone to accurately evaluate their performance on a computerized attention test, yet this person may be unable to realistically evaluate their everyday life attentional skills. To overcome this issue, future research could try to develop neuropsychological tests which more clearly resemble the challenges patients with ADHD may face in their daily life.
To explore whether deficits in metacognition relate to psychopathology, it was first established whether patients with ADHD differ from controls in psychopathology. Large effects were found for all aspects (Inattention, Hyperactivity/ Impulsivity, Depression, State and Trait anxiety). The results revealed that inattention can explain variance in metacognition (in both knowledge and regulation of cognition), whereas no other aspect of psychopathology was a significant predictor in any model. The results are in line with our expectation that ADHD symptomatology influences metacognition, as inattention consistently explains variance. This effect is especially noteworthy as it was evident across analyses: inattention was a significant predictor for all outcome measures of metacognition, when the whole sample was considered (), when only patients with ADHD were considered and even for controls (Supplement B). This indicates that the more inattentive symptoms are present, the lower metacognitive abilities may be, which could point toward the relevance of bottom-up processing for attention and metacognition. Basic processes may constitute part of the foundation of cognitive deficits in adult ADHD (Butzbach et al., Citation2019; Guo et al., Citation2020). One may suggest that impairments in attention may result in impairments in higher order functions building up on them (metacognition) in adults with ADHD. This is in line with the present finding that patients with ADHD report large deficits in knowledge of cognition, which encompasses awareness of cognitive processes. Indeed, there seems to be an intricate relationship between attention and metacognition (Jaeger et al., Citation2017; Sherman et al., Citation2015) and the importance of attention for awareness strongly supports this notion, with some research even suggesting that attention may be necessary for awareness (Cohen et al., Citation2012). Thus, deficits in a basic process such as attention may manifest in a lack of awareness.
Previous research indicated that depression may influence metacognition (Soderstrom et al., Citation2011). In the current study, depression did not significantly contribute to models predicting metacognition. In both between and within group analysis, depression did not influence self-reported metacognition. Soderstrom et al. (Citation2011) found that mild depression was associated with better metacognitive accuracy, whereas this was not the case for moderate depression. It is important to note that Soderstrom et al. (Citation2011) used a convenience sample of university students, whereas in the current study patients with ADHD and in some cases comorbid depression were assessed. Therefore, the effects found for mild depressive symptoms in students may not be found in a clinical sample with more severe symptoms. Alternatively, the tendency found for mild depression to evaluate oneself more realistically may be mitigated in adult ADHD by a tendency of patients with ADHD to overestimate themselves (Moerstedt et al., Citation2015; Prevatt et al., Citation2012).
Finally, the influence of metacognition to daily functioning (self-rated and informant-rated) was explored. First, impairments in daily functioning in patients with ADHD were established and large effects were found for self- and informant-rated impairments in daily functioning. Next, it was explored whether metacognition may explain impairments in daily functioning. In line with our expectations, a model with predictors of metacognition explained variance in self-reported daily functioning (R2 = .378) and in informant-reported daily functioning (R2 = .257). Knowledge of cognition could predict both self-rated () and informant-rated daily functioning (), whereas regulation of cognition did not explain additional variance in either model. Patients with ADHD may fail to attend to their internal processes and miss cues (e.g., not noticing that information was not understood when reading), that individuals without ADHD might attend to. This may have repercussions in various aspects of daily living, such as at the work place, where assignments may miss information, or in driving, where for example, street signs may be overlooked.
Separate regressions were calculated per group to determine within group effects, whether individuals with higher scores of metacognition show fewer deficits in daily functioning than individuals with lower scores of metacognition (Supplement B). Within each individual group, no significant model was found, implying that the effect of metacognition on daily functioning should be interpreted with caution and may not be suitable for individual decision making. It may be important to replicate this with a larger sample to gain more insight, as the lack of a significant result in the patient group may represent a restriction of range problem. The finding that metacognition can explain daily functioning based on self-report () and also based on informant-report () in the whole sample supports the notion by Bitto et al. (Citation2017) that ADHD in adulthood may represent a spectrum. display the relationship between metacognition and daily functioning, illustrating both the contrast of the two groups but also the spectrum within the groups. When the whole spectrum is considered, ranging from high functioning individuals in the community to patients with ADHD experiencing impairments in many aspects of daily living, the effect of metacognition on daily functioning unfolds ().
Clinical implications
Several “metacognitive” therapies were developed for adult ADHD (Solanto et al., Citation2010; Thompson & Thompson, Citation1998; Wasserstein & Lynn, Citation2001), yet, a strong evidence base for them is missing, due to the scarcity of research on metacognition in adult ADHD. Furthermore, these therapies seemed employ a cognitive, rather than metacognitive approach (Wells & Fisher, Citation2011). To target a metacognitive process in therapy, an idea for clinicians could be to stimulate patients’ awareness by comparing patients’ perspective of their cognition with the evaluation of a clinician and/ or cognitive testing and providing the patient with feedback, to encourage the patient to adjust as necessary. However, further research is necessary to understand what may improve metacognitive functioning in adults with ADHD.
The finding that patients report large deficits in metacognition even though these deficits are not as apparent based on cognitive testing warrants further exploration, to understand in which situations patients may experience problems associated with these deficits and to investigate what could help them. As the clinical assessment of ADHD largely relies on self-report and previous research found considerable mismatch between patients perspective and other sources of information (Barkley & Murphy, Citation2010; Fuermaier et al., Citation2015; Moerstedt et al., Citation2015) including a measure of metacognition into the clinical assessment may add perspective on how patients view their own cognitive functioning (Craig et al., Citation2020) and may allow clinicians to put self-reported information in perspective. A consensus study revealed that clinicians and other experts do not seem to consider metacognition in the clinical assessment of ADHD (Fuermaier et al., Citation2019). Yet, it may be important for clinicians to be aware to what extent a given patient experiences problems in metacognitive functions. If the patient him or herself reports deficits in metacognitive awareness, this may alert the clinician to compare patients’ report of their cognitive impairments with the results of cognitive testing and other outside information.
Limitations and future directions
When considering the results of the study, several limitations should be noted. As noted before, the assessment of metacognition by self-report is problematic, because if someone has a deficit in metacognition, this may impact his or her ability on reporting such a deficit. The overlap between self-reports of metacognition and metacognitive behaviors is limited and it remains unclear how self-reports relate to the underlying construct of metacognition (Craig et al., Citation2020). The answering format of the MAI may represent another limitation, as participants can only choose whether the statement applies to them or not (true/false). Metacognition in adults with ADHD may differ per domain (Butzbach et al., Citation2021) and nuances may be lost in such a dichotomous answering format. For example, a 4-point Likert scale might have been able to capture more fine-grained variations in the participants’ responses. Another limitation might be that for questionnaires assessing attention and metacognition, results could be influenced by an overlap in how the items are understood, as in some cases items are phrased similarly. This in combination with the fact that the MAI was not developed for clinical populations, highlights the need to develop new instruments to measure metacognition in adults with ADHD. The self-evaluation method based on cognitive test performance is very promising, but its reliability may be limited and might not have been sensitive enough in the current study as indicated by the low power. Future research could replicate the study with a larger sample, a wider selection of tests and more self-evaluation measures per test to gain a better understanding of metacognition in adults with ADHD. In addition, the findings of this study are sex/ gender neutral. As some sex/ gender differences were noted in the clinical picture of adult ADHD (Kooij et al., Citation2019), possible differential effects of metacognition on men and women should be explored in future research. Furthermore, the dimensional analyses employed in the current study make the interpretation of findings for clinical populations less straightforward. While metacognition may predict daily functioning from a dimensional perspective, one cannot say that patients with ADHD who report high metacognitive abilities would be better adapted in their daily lives compared to patients with ADHD reporting low metacognitive abilities. Thus, the current study should be considered as an explorative guide to inform further studies, for which one may consult the exploratory analysis in Supplement B.
Supplemental Material
Download PDF (254.1 KB)Disclosure statement
The authors have no conflict of interest to report.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Adler, L. A., Spencer, T., Faraone, S. V., Kessler, R. C., & Secnik, K. (2006, July–September). Validity of pilot adult ADHD self- report scale (ASRS) to rate adult ADHD symptoms. Annals of Clinical Psychiatry, 18(3), 145–148. https://doi.org/10.1080/10401230600801077
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders.
- American Psychiatric Association, DSM-5 Task Force. (2013). Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.). American Psychiatric Publishing, Inc. https://doi.org/10.1176/appi.books.9780890425596
- Barkley, R. A., & Murphy, K. R. (2010). Impairment in occupational functioning and adult ADHD: The predictive utility of executive function (EF) ratings versus EF tests. Archives of Clinical Neuropsychology, 25(3), 157–173. https://doi.org/10.1093/arclin/acq014
- Beck, A., Steer, R., & Garbin, M. (1988). Psychometric properties of the beck depression inventory - 25 years of evaluation. Clinical Psychology Review, 8(1), 77–100. https://doi.org/10.1016/0272-7358(88)90050-5
- Bitto, H., Morstedt, B., Faschina, S., & Stieglitz, R. (2017). ADHD in adults: A dimensional or categorial construct? Zeitschrift fur Psychiatrie Psychologie und Psychotherapie, 65(2), 121–131. https://doi.org/10.1024/1661-4747/a000311
- Butzbach, M., Fuermaier, A. B. M., Aschenbrenner, S., Weisbrod, M., Tucha, L., & Tucha, O. (2019). Basic processes as foundations of cognitive impairment in adult ADHD. Journal of Neural Transmission, 126(10), 1347–1362. https://doi.org/10.1007/s00702-019-02049-1
- Butzbach, M., Fuermaier, A. B. M., Aschenbrenner, S., Weisbrod, M., Tucha, L., & Tucha, O. (2021). Metacognition in adult ADHD: Subjective and objective perspectives on self-awareness of cognitive functioning. Journal of Neural Transmission. Advance online publication. https://doi.org/10.1007/s00702-020-02293-w
- Chaytor, N., & Schmitter-Edgecombe, M. (2003). The ecological validity of neuropsychological tests: A review of the literature on everyday cognitive skills. Neuropsychology Review, 13(4), 181–197. https://doi.org/10.1023/B:NERV.0000009483.91468.fb
- Chen, Q., Hartman, C. A., Haavik, J., Harro, J., Klungsoyr, K., Hegvik, T., … Larsson, H. (2018). Common psychiatric and metabolic comorbidity of adult attention-deficit/hyperactivity disorder: A population-based cross-sectional study. Plos One, 13(9), e0204516. https://doi.org/10.1371/journal.pone.0204516
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates.
- Cohen, M. A., Cavanagh, P., Chun, M. M., & Nakayama, K. (2012). The attentional requirements of consciousness. Trends in Cognitive Sciences, 16(8), 411–417. https://doi.org/10.1016/j.tics.2012.06.013
- Conners, C. K., Erhardt, D., Epstein, J. N., Parker, J. D. A., Sitarenios, G., & Sparrow, E. (1999). Self-ratings of ADHD symptoms in adults I: Factor structure and normative data. Journal of Attention Disorders, 3(3), 141–151. https://doi.org/10.1177/108705479900300303
- Craig, K., Hale, D., Grainger, C., & Stewart, M. (2020). Evaluating metacognitive self-reports: Systematic reviews of the value of self-report in metacognitive research. Metacognition and Learning, 15(2), 155–213. https://doi.org/10.1007/s11409-020-09222-y
- Eslinger, P. J., Dennis, K., Moore, P., Antani, S., Hauck, R., & Grossman, M. (2005). Metacognitive deficits in frontotemporal dementia. Journal of Neurology, Neurosurgery, and Psychiatry, 76(12), 1630–1635. https://doi.org/10.1136/jnnp.2004.053157
- Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146
- Flavell, J. H. (1979). Metacognition and cognitive monitoring: A new area of cognitive–developmental inquiry. American Psychologist, 34(10), 906–911. https://doi.org/10.1037/0003-066X.34.10.906
- Fuermaier, A. B. M., Tucha, L., Koerts, J., Aschenbrenner, S., & Tucha, O. (2017). Vienna test system (VTS): The groningen effort test (GET). Schuhfried GmbH.
- Fuermaier, A. B. M., Fricke, J. A., de Vries, S. M., Tucha, L., & Tucha, O. (2019). Neuropsychological assessment of adults with ADHD: A delphi consensus study. Applied Neuropsychology: Adult, 26(4), 340–354. https://doi.org/10.1080/23279095.2018.1429441
- Fuermaier, A. B. M., Tucha, L., Evans, B. L., Koerts, J., de Waard, D., Brookhuis, K., … Tucha, O. (2017). Driving and attention deficit hyperactivity disorder. Journal of Neural Transmission, 124(1), 55–67. https://doi.org/10.1007/s00702-015-1465-6
- Fuermaier, A. B. M., Tucha, L., Koerts, J., Aschenbrenner, S., Kaunzinger, I., Hauser, J., …Tucha, O. (2015). Cognitive impairment in adult ADHD-perspective matters! Neuropsychology, 29(1), 45–58. https://doi.org/10.1037/neu0000108
- Fuermaier, A. B. M., Tucha, O., Koerts, J., Grabski, M., Lange, K. W., Weisbrod, M., … Tucha, L. (2016). The development of an embedded figures test for the detection of feigned attention deficit hyperactivity disorder in adulthood. PloS One, 11(10), e0164297–e0164297. https://doi.org/10.1371/journal.pone.0164297
- Guo, N., Fuermaier, A. B. M., Koerts, J., Mueller, B. W., Diers, K., Mroß, A., …Tucha, O. (2020). Neuropsychological functioning of individuals at clinical evaluation of adult ADHD. Journal of Neural Transmission. Advance online publication. https://doi.org/10.1007/s00702-020-02281-0
- Harrison, G. M., & Vallin, L. M. (2018). Evaluating the metacognitive awareness inventory using empirical factor-structure evidence. Metacognition and Learning, 13(1), 15–38. https://doi.org/10.1007/s11409-017-9176-z
- Hong, W. H., Vadivelu, J., Daniel, E. G. S., & Sim, J. H. (2015). Thinking about thinking: Changes in first-year medical students’ metacognition and its relation to performance. Medical Education Online, 20(1), 27561. https://doi.org/10.3402/meo.v20.27561
- Jaeger, C. B., Levin, D. T., & Porter, E. (2017). Justice is (change) blind: Applying research on visual metacognition in legal settings. Psychology Public Policy and Law, 23(2), 259–279. https://doi.org/10.1037/law0000107
- Katzman, M. A., Bilkey, T. S., Chokka, P. R., Fallu, A., & Klassen, L. J. (2017). Adult ADHD and comorbid disorders: Clinical implications of a dimensional approach. Bmc Psychiatry, 17(1), 302. https://doi.org/10.1186/s12888-017-1463-3
- Kessler, R. C., Adler, L., Ames, M., Demler, O., Faraone, S., Hiripi, E., … Walters, E. E. (2005). The world health organization adult ADHD self-report scale (ASRS): A short screening scale for use in the general population. Psychological Medicine, 35((2):), 245–256. https://doi.org/10.1017/S003329170400289256
- Kessler, R. C., Adler, L., Barkley, R., Biederman, J., Conners, C. K., Demler, O., …Zaslavsky, A. M. (2006). The prevalence and correlates of adult ADHD in the united states: Results from the national comorbidity survey replication. American Journal of Psychiatry, 163(4), 716–723. https://doi.org/10.1176/ajp.2006.163.4.716
- Knouse, L. E., Bagwell, C. L., Barkley, R. A., & Murphy, K. R. (2005). Accuracy of self-evaluation in adults with ADHD evidence from a driving study. Journal of Attention Disorders, 8(4), 221–234. https://doi.org/10.1177/1087054705280159
- Knouse, L. E., Paradise, M. J., & Dunlosky, J. (2006). Does ADHD in adults affect the relative accuracy of metamemory judgments? Journal of Attention Disorders, 10(2), 160–170. https://doi.org/10.1177/1087054706288116
- Kooij, J. J. S., Bijlenga, D., Salerno, L., Jaeschke, R., Bitter, I., Balazs, J., … Asherson, P. (2019). Updated european consensus statement on diagnosis and treatment of adult ADHD. European Psychiatry, 56, 14–34. https://doi.org/10.1016/j.eurpsy.2018.11.001
- Krueger, C. E., Rosen, H. J., Taylor, H. G., Espy, K. A., Schatz, J., Rey-Casserly, C., & Kramer, J. H. (2011). Know thyself: Real-world behavioral correlates of self-appraisal accuracy. The Clinical Neuropsychologist, 25(5), 741–756. https://doi.org/10.1080/13854046.2011.569759
- Lehrl, S. (1995). Mehrfachwahl-Wortschatz-Intelligenztest. Spitta-Verlag.
- Lehrl, S., Triebig, G., & Fischer, B. (1995). Multiple choice vocabulary test MWT as a valid and short test to estimate premorbid intelligence. Acta Neurologica Scandinavica, 91(5), 335–345. https://doi.org/10.1111/j.1600-0404.1995.tb07018.x
- Lysaker, P. H., Erickson, M., Ringer, J., Buck, K. D., Semerari, A., Carcione, A., & Dimaggio, G. (2011). Metacognition in schizophrenia: The relationship of mastery to coping, insight, self-esteem, social anxiety, and various facets of neurocognition. British Journal of Clinical Psychology, 50(4), 412–424. https://doi.org/10.1111/j.2044-8260.2010.02003.x
- Manor, I., Vurembrandt, N., Rozen, S., Gevah, D., Weizman, A., & Zalsman, G. (2012). Low self-awareness of ADHD in adults using a self-report screening questionnaire. European Psychiatry, 27(5), 314–320. https://doi.org/10.1016/j.eurpsy.2010.08.013
- Moerstedt, B., Corbisiero, S., Bitto, H., & Stieglitz, R. (2015). Attention-deficit/hyperactivity disorder (ADHD) in adulthood: Concordance and differences between self- and informant perspectives on symptoms and functional impairment. Plos One, 10(11), e0141342. https://doi.org/10.1371/journal.pone.0141342
- Oie, M., Sundet, K., & Ueland, T. (2011). Neurocognition and functional outcome in early-onset schizophrenia and attention-deficit/hyperactivity disorder: A 13-year follow-up. Neuropsychology, 25(1), 25–35. https://doi.org/10.1037/a0020855
- Potvin, S., Charbonneau, G., Juster, R., Purdon, S., & Tourjman, S. V. (2016). Self-evaluation and objective assessment of cognition in major depression and attention deficit disorder: Implications for clinical practice. Comprehensive Psychiatry, 70, 53–64. https://doi.org/10.1016/j.comppsych.2016.06.004
- Prevatt, F., Proctor, B., Best, L., Baker, L., Van Walker, J., & Taylor, N. W. (2012). The positive illusory bias: Does it explain self-evaluations in college students with ADHD? Journal of Attention Disorders, 16(3), 235–243. https://doi.org/10.1177/1087054710392538
- Rösler, M., Retz-Junginger, P., Retz, W., & Stieglitz, R. (2008). Homburger ADHS-skalen für erwachsene. untersuchungsverfahren zur syndromalen und kategorialen diagnostik der aufmerksamkeitsdefizit-/hyperaktivitätsstörung (ADHS) im erwachsenenalter. Hogrefe.
- Schmand, B. (2019). Why are neuropsychologists so reluctant to embrace modern assessment techniques? The Clinical Neuropsychologist,33(2), 1–11. https://doi.org/10.1080/13854046.2018.1523468
- Schoechlin, C., & Engel, R. (2005). Neuropsychological performance in adult attention-deficit hyperactivity disorder: Meta-analysis of empirical data. Archives of Clinical Neuropsychology, 20(6), 727–744. https://doi.org/10.1016/j.acn.2005.04.005
- Schraw, G., & Dennison, R. S. (1994). Assessing metacognitive awareness. Contemporary Educational Psychology, 19(4), 460–475. https://doi.org/10.1006/ceps.1994.1033
- Schuhfried. (2010). Vienna test system: Psychological assessment.
- Sherman, M. T., Seth, A. K., Barrett, A. B., & Kanai, R. (2015). Prior expectations facilitate metacognition for perceptual decision. Consciousness and Cognition, 35, 53–65. https://doi.org/10.1016/j.concog.2015.04.015
- Soderstrom, N. C., Davalos, D. B., & Vazquez, S. M. (2011). Metacognition and depressive realism: Evidence for the level-of-depression account. Cognitive Neuropsychiatry, 16(5), 461–472. https://doi.org/10.1080/13546805.2011.557921
- Solanto, M. V., Marks, D. J., Wasserstein, J., Mitchell, K., Abikoff, H., Alvir, J. M. J., & Kofman, M. D. (2010). Efficacy of meta-cognitive therapy for adult ADHD. American Journal of Psychiatry, 167(8), 958–968. https://doi.org/10.1176/appi.ajp.2009.09081123
- Spielberger, C., Gorsuch, R., Lushene, R., Vagg, P. R., & Jacobs, G. (1983). Manual for the state-trait anxiety inventory (form Y1 – Y2). Consulting Psychologists Press.
- Sturm, W. (2017a). Vienna test system manual perception and attention functions: Selective attention test label WAFS (24 - Revision 5 ed.). Schuhfried GmbH.
- Sturm, W. (2017b). Vienna test system manual perception and attention functions: Vigilance test label WAFV (24 - Revision 6 ed.). Schuhfried.
- Suhr, J. A., Buelow, M., & Riddle, T. (2011). Development of an infrequency index for the CAARS. Journal of Psychoeducational Assessment, 29(2), 160–170. https://doi.org/10.1177/0734282910380190
- Szuromi, B., Bitter, I., & Czobor, P. (2013). Functional impairment in adults positively screened for attention-deficit hyperactivity disorder: The role of symptom presentation and executive functioning. Comprehensive Psychiatry, 54(7), 974–981. https://doi.org/10.1016/j.comppsych.2013.04.002
- Thompson, L., & Thompson, M. (1998). Neurofeedback combined with training in metacognitive strategies: Effectiveness in students with ADD. Applied Psychophysiology and Biofeedback, 23(4), 243–263. https://doi.org/10.1023/A:1022213731956
- Ward, M. F., Wender, P. H., & Reimherr, F. W. (1993). The wender utah rating-scale: An aid in the retrospective diagnosis of childhood attention-deficit hyperactivity disorder. American Journal of Psychiatry, 150(6), 885–890. https://doi.org/10.1176/ajp.150.6.885
- Wasserstein, J., & Lynn, A. (2001). Metacognitive remediation in adult ADHD - treating executive function deficits via executive functions. Adult Attention Deficit Disorder: Brain Mechanisms and Life Outcomes, 931, 376–384. https://pubmed.ncbi.nlm.nih.gov/11462754/
- Weiss, M. D., Brooks, B. L., Iverson, G. L., Lee, B., Dickson, R., & Wasdell, M. (2007). Reliability and validity of the Weiss functional impairment rating scale. AACAP 54th Annual Meeting (pp. 23–28), Boston, MA.
- Wells, A., & Fisher, P. (2011). Meta-cognitive therapy without metacognition: A case of ADHD. American Journal of Psychiatry, 168(3), 327–327. https://doi.org/10.1176/appi.ajp.2010.10101467
- Wilens, T. E., Morrison, N. R., & Prince, J. (2011). An update on the pharmacotherapy of attention-deficit/hyperactivity disorder in adults. Expert Review of Neurotherapeutics, 11(10), 1443–1465. https://doi.org/10.1586/ERN.11.137
- Williamson, C., Alcantar, O., Rothlind, J., Cahn-Weiner, D., Miller, B. L., & Rosen, H. J. (2010). Standardised measurement of self-awareness deficits in FTD and AD. Journal of Neurology, Neurosurgery & Psychiatry, 81(2), 140–145. https://doi.org/10.1136/jnnp.2008.166041
