ABSTRACT
Objective
Problems with finding one’s way around are frequently reported by neurological patients. However, no dedicated standardized tools exist to assess whether such reports indicate navigation impairment or not. We provide a standardized three-step method to assess navigation ability in neurological patients, based on two recently developed diagnostic tools and normative data. The objective of this method is to assess navigation ability in detail, to allow for appropriate rehabilitation training for navigation impairment.
Method
A population-based sample of 7150 Dutch individuals (age 18–89) filled out the Wayfinding Questionnaire (WQ), to assess their self-reported navigation ability and level of spatial anxiety. Additionally, the participants completed the Leiden Navigation Test (LNT), a brief digital test consisting of five subtasks, assessing distinct domains of navigation ability. Both the WQ and LNT can be found online, free of charge.
Results
Normative data stratified by gender and age are reported for each of the three subscales of the WQ, and for each of the five subtasks of the LNT.
Conclusions
Based on performance data of a very large population-based sample of participants, navigation performance of neurological patients with specific navigation complaints can be assessed in three steps. First, we recommend to inquire about potential problems concerning navigation. Next, in case of navigation complaints, the extent of potential navigation impairment can first be measured with the WQ. Lastly, if impaired scores are found, the LNT can provide objective verification of the perceived impairment, as well as insight into which navigation domains are affected. Such insight will allow for prediction of the practical consequences of the impairment and can be used for informed and tailored rehabilitation.
Introduction
Spatial navigation is an essential element of many daily activities, such as driving to work or walking to a friend’s house, but also to find every item we need in a grocery store. Many patients with acquired brain damage report impaired spatial navigation (e.g., Bell, Citation2012; Busigny et al., Citation2014; Cushman et al., Citation2008; Lemoncello et al., Citation2010; Livingstone & Skelton, Citation2007), with rates ranging from 30% to 60% (Cerman et al., Citation2018; Van der Ham et al., Citation2013; Van der Kuil et al., Citation2021). Not only does a lower level of navigation ability negatively impact their mobility and autonomy in many daily life activities, navigation ability is also positively correlated with measures of quality of life (Stroke Specific Quality of Life Scale, Post et al., Citation2011; e.g., Van der Ham et al., Citation2013). Empirical evidence for navigation impairment primarily concerns stroke patients, but recent studies also showed that navigation abilities can be affected by pathological aging (Cerman et al., Citation2018; Cushman et al., Citation2008; Gazova et al., Citation2012) and epilepsy (Bell, Citation2012; Grewe et al., Citation2014). More specifically, navigation impairment has been observed as a significant behavioral marker of pathological aging, particularly in early stages of the condition. As early diagnosis of Alzheimer’s disease has obvious benefits, a suitable behavioral measure of navigation ability could have a significant role in the diagnostic process (see e.g., Allison et al., Citation2016; Boccia et al., Citation2019; Coughlan et al., Citation2018; Lester et al., Citation2017; Tuena et al., Citation2021).
Despite the common occurrence of navigation impairment, the assessment of navigation ability is typically not included in clinical practice. Moreover, it has been found that existing standardized materials are unable to provide a measure of navigation ability (Nadolne & Stringer, Citation2001; Van der Ham et al., Citation2010). Therefore, any indication of the level of navigation ability is typically absent in neuropsychological examinations. In recent years, numerous studies have assessed navigation ability in neurological populations with experimental methods. Emerging technological tools such as computerized and virtual environments allow for the examination of navigation performance in a highly controlled environment (e.g., Laczó et al., Citation2014; Grewe et al., Citation2014; Claessen et al., Citation2016a; M.H.G. Claessen et al., Citation2017; Cogné et al., Citation2017). However, these measures have yet to reach regular clinical practice as part of widely available standardized, neuropsychological testing materials. Therefore, the main goal of this article is to present a clinical guide to navigation impairment, as a suggested method to approach navigation complaints. Such a guide will not only support a detailed diagnostic outcome, but will also provide valuable input for the subsequent rehabilitation trajectory. To this end we have integrated the theoretical and clinical findings concerning navigation impairment after acquired brain injury to provide a systematic practical course of action to be used when navigation complaints are reported. This guide consists of a three-step method to examine navigation ability in patients with acquired brain injury, when they indicate to have trouble finding their way around. The outcome of this clinical guide is to obtain a detailed, objective description of navigation impairment in an individual. Consequently, the needs of the patient can be understood in light of the characteristics of the impairment. Such needs can consist of personalized cognitive rehabilitation treatment or assistance to enhance navigation performance and reduce negative consequences of the impairment.
Method
Target population
The target audience for the diagnostic approach for navigation impairment concerns neuropsychological patients in a broad sense. As mentioned, previous findings indicate that within neuropsychological patients with acquired brain injury navigation complaints are highly prevalent (30–50%). As mentioned, recent literature highlights the importance of measuring navigation ability in a clinically sound manner, as an impaired level of navigation ability could be a valuable early marker of pathological aging and contribute to the diagnostic process.
It should be noted that the questionnaire and test used, require a certain level of cognitive functioning of the patient to be informative. It requires sufficient verbal understanding of the instructions and questionnaire items, and sufficient visual acuity to perceive the visual input on a computer screen. Very low working memory performance or processing speed may also result in low performance, in the absence of navigation impairment.
Diagnostic procedure
The three steps of the proposed diagnostic procedure concern the recommended course of action when navigation impairment may be present in a patient.
Step 1: Navigation complaints First of all, we recommend to explicitly ask a patient if he or she has any complaints about their navigation skills. Often, such a question is not typically included in the diagnostic procedure and may lead to missing navigation impairment. We consider the self-report of a complaint concerning navigation skills an essential part of the diagnostic procedure we present. The main goal of following the diagnostic procedure is to identify the specific characteristics of navigation impairment in an individual, to optimize subsequent cognitive rehabilitation. In order for such cognitive rehabilitation to be effective, at least some awareness of the impairment is key. The patient needs to be aware of the situations they get lost in, and how the learnt strategies during training can help to find their way in those situations. It is possible that peer evaluation may detect an issue with navigation before patient self-evaluation, in progressive neurological conditions for instance, (e.g., a partner may detect an increase in errors during walks). In such cases, peer evaluation could precede self-reported complaints in the diagnostic procedure. If a patient indicates to have trouble navigation, we suggest to proceed to the second step; which includes the Wayfinding Questionnaire (WQ).
Step 2: Wayfinding Questionnaire
Next, the extent of the complaint should be assessed. The first step of the suggested approach entails the use of a validated self-report questionnaire to assess subjective navigation ability and spatial anxiety. The WQ has recently been developed and validated to specifically assess navigation performance in neurological patients (Van der Ham et al., Citation2013; Claessen, Visser-Meily, de Rooij, Postma, & van der Ham, Citation2016b; De Rooij et al., Citation2019). The questionnaire consists of 22 questions distributed over three subscales; Navigation and Orientation, Distance Estimation, and Spatial anxiety, which are of particular relevance to the neurological patient population. Navigation and Orientation directly addresses the ability to navigate and orient oneself in space, whereas Distance Estimation focuses on the spatial ability to process metric information. Additionally, Spatial Anxiety is of importance, especially in a clinical context. Spatial anxiety was first coined in 1994 by Lawton, and defined as “anxiety about environmental navigation,” and operationalized by a brief questionnaire in which participants rated their level of anxiety in specific spatial situations, concerning e.g., finding the way in complex or unfamiliar environments (Lawton, Citation1994). In short, spatial anxiety reflects the level of anxiety experienced in navigation-related situations. Spatial anxiety has been proven to have a negative impact on navigation ability (e.g., He & Hegarty, Citation2020; Lyons et al., Citation2018) and is frequently reported by neurological patients who indicate problems with navigation (e.g., Kremmyda et al., Citation2016; Van der Ham et al., Citation2010). All three subscales have shown very high internal consistency (range alpha = 0.83–0.92) for stroke patients and medium to high correlation between the subscales and total score (range r = 0.67–0.88) (Claessen et al., Citation2016b). Furthermore, validity and clinical usefulness have been demonstrated in a comparison between stroke patients and healthy controls (De Rooij et al., Citation2019).
As navigation problems are typically encountered in healthy aging (e.g., Gazova et al., Citation2012; Lester et al., Citation2017; Moffat, Citation2009) and may differ substantially in time due to aging itself, a standardized assessment of navigation impairment is in order. Additionally, substantial differences due to gender have been observed in subjective measures of cognition, and navigation ability in particular (e.g., Lemieux et al., Citation2019; Sieverding & Koch, Citation2009; Van der Ham et al., Citation2020). Therefore, we provide normative data for each of the subscales of the Wayfinding Questionnaire, stratified by age and gender. In a large-scale public experiment, a sufficient number of participants was reached to provide a detailed normative dataset (Van der Ham et al., Citation2020).
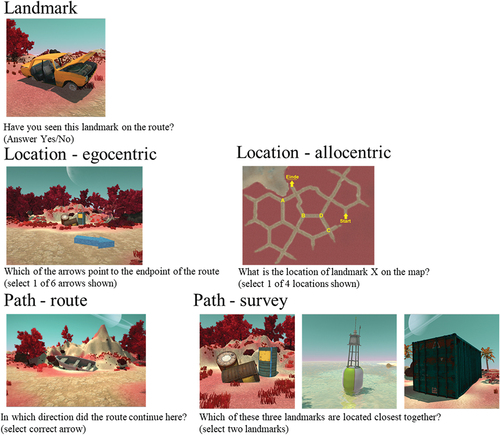
Step 3: Leiden Navigation Test
If performance on the Wayfinding Questionnaire gives rise to further examination, a digital test to objectively determine navigation performance can be used. The Leiden Navigation Test concerns a brief five part assessment, which can be performed fully digitally. This test has recently been published (Van der Ham et al., Citation2020) and it entails the presentation of a short video through a virtual environment, along eight different landmarks on a route, and five subtasks to reflect the functional domains of navigation impairment. Participants are instructed to pay attention to the route shown to them, and are questioned about their knowledge of the landmarks, route, and environment after the video ends. The five subtasks systematically address functionally separate domains of navigation ability, as determined in earlier work. Claessen and van der Ham (Citation2017) and M.H.G. Claessen et al. (Citation2017) have identified three distinct domains of navigation; landmarks, locations, and paths. Extensive literature review of case studies on navigation impairment resulted in this categorization, as all case descriptions could be meaningfully assigned to one of these three domains. The landmark domain addresses the “What?” question in navigation and concerns the ability to identify spatially relevant elements in an environment. Landmark knowledge can be assessed by measuring recognition of previously viewed landmarks (e.g., Janzen et al., Citation2008). The location domain concerns the “Where?” question and reflects the processing of spatial locations in an environment. Location knowledge fits well with the commonly drawn distinction between egocentric and allocentric processing (Klatzky, Citation1998). A particular location can be coded either as being “to my left” (egocentric location knowledge), or “north of city hall” (allocentric location knowledge). Adopting an egocentric perspective is generally easier and only requires exposure to an environment from one particular viewing angle. An allocentric perspective, on the other hand, relies on the mental map of an environment, in which viewing angle is disregarded. The third category, paths, is the most complex and concerns the question of “How to get there?.” It involves the spatial context of a given landmark, which reflects how the landmark location relates to one or multiple other elements in an environment. The frequently made distinction between route versus survey knowledge (Montello, Citation1998; Siegel & White, Citation1975) is applicable here: path knowledge may concern either a specific route one can take to reach a certain location (path route knowledge), or allow a representation of a spatial configuration from a bird’s eye perspective (path survey knowledge). provides LNT screenshots for each of the tasks included. In addition to the findings from patient studies that support the functional distinction between the different domains identified (Claessen & van der Ham, Citation2017), also the outcomes on each of the LNT subscales show clearly dissociable patterns of performance across different age groups (Van der Ham et al., Citation2020). Combined, these findings highlight the need to assess performance on each of the subtasks in order to assess navigation performance in a comprehensive manner.
Especially age has been shown to impact navigation ability (e.g., Gazova et al., Citation2012; Lester et al., Citation2017; Moffat, Citation2009) and consequently performance level in the Leiden Navigation Test (Van der Ham et al., Citation2020). Also gender has frequently been identified as a factor explaining for individual differences in navigation (e.g., Coutrot et al., Citation2018; Gagnon et al., Citation2018; Munion et al., Citation2019), and impacted performance level to a limited extent in the Leiden Navigation Test (Van der Ham et al., Citation2020). Therefore, normative data is provided here, stratified by gender and age. For a patient, their relative performance within the appropriate norm group can be determined for each of the five navigation domains. Typically, in case of an impairment, very low scores are found for a subset of the domains. The norm data have been constructed to accommodate the standard neuropsychological test score interpretation. This information can be used to identify which rehabilitation strategy is most appropriate for an individual (see e.g., M.H.G. Claessen et al., Citation2017; M. N. Van der Kuil et al., Citation2020).
Process description
provides a visual depiction of the different elements of the proposed diagnostic procedure. Importantly, the procedure is started when a problem concerning spatial navigation is detected, either by the patient themselves, the clinician, or by a close relative or friend. Upon this detection, the WQ is administered to assess whether or not the subjective navigation performance is at an impaired level. Next, if impaired subjective navigation performance is detected, the LNT can be administered to gain more insight into the characteristics of the impairment. The LNT outcomes can indicate the severity of the impairment as well as the functional domains of spatial navigation that are impaired.
Figure 2. Flowchart of the proposed diagnostic procedure including the Wayfinding Questionnaire (WQ) and the Leiden Navigation Test (LNT).
Both the WQ and the LNT materials including scoring method and instructions are available online, free of charge, in Dutch as well as English, at www.vanderhamlab.com.
Norm data collection
As described in Van der Ham et al. (Citation2020) and Van der Ham et al. (Citation2021), an online public experiment on navigation abilities was conducted. This large scale experiment was performed in collaboration with the Dutch Ministry of Education, Culture and Science. As part of the national annual event “Het weekend van de wetenschap” (The weekend of science), an open invitation was distributed through national media channels to participate in the experiment. This lead to a large and heterogeneous sample of participants who agreed to participate in a brief formal scientific experiment. The experiment consisted of a few demographic questions and the LNT. Additionally, if participants were willing to participate a few minutes longer, they could opt to also fill out the WQ. No compensation or other incentive other than intrinsic motivation was offered. The study was conducted according to the declaration of Helsinki and approved by the ethical committee of the institute of psychology at Leiden University (#CEP17-0713/250).
Participants
The total number of participants included in the current dataset was 7150 and is described in . All participants to the public experiment were included if they had fully completed the demographic questions, LNT, and had also completely filled out the WQ. In order to create normative scores for males and females separately, non-binary participants were excluded. Participant ages were restricted to 18–89 years old, to include only adult participants. Participants were grouped in 10 year bins, with the exception of the youngest age group, as this group included participants with ages from 18 to 29 years old. An experiment with online participants bears certain risks about e.g., seriousness of participation and limited information concerning participants’ health. However, both the size of the current sample and a number of precautions were taken to reduce such risks. The context of data collection (forming a normative dataset) was communicated very clearly in all public communication about the experiment. The experiment was featured in national media (e.g., TV, radio, newspapers) in which it was clearly mentioned that a reliable normative dataset could aid in neuropsychological diagnostic procedures for e.g., stroke and dementia. The website on which the experiment was posted clearly mentioned a version of the experiment for healthy participants and a version for those with acquired brain injury. A verification of neurological health was included in the informed consent text for healthy participants. Furthermore, the experiment was explicitly supported by the Dutch ministry of education, culture, and science and some of the participants were recruited through an official portal for neuroscientific research (www.hersenonderzoek.nl). In this portal, health data is collected from all subscribers, and researchers actively select their population of interest (here: no neurological or psychiatric history). For the sample used in the current study, an additional filter was that all participants included filled out the WQ in its entirety, which was optional. Only if they volunteered to prolong their participation to the experiment for another 10 minutes they are included in the data discussed here.
Table 1. Sample description for the normative data of the Wayfinding Questionnaire and Leiden Navigation Test, indicating number of females and males included for every age group (in years).
Materials
The normative data were calculated based on performance on the WQ using the final version of the questionnaire, as described by Claessen et al. (Citation2016a) and De Rooij et al. (Citation2019). The WQ consists of 22 questions, distributed across three subscales (Navigation and Orientation, Distance Estimation, Spatial anxiety) which were all included.
The LNT data concerns a subset of the data reported by Van der Ham et al. (Citation2020); only those participants who also completed the WQ and within the age range 18–89 were included here. The LNT consists of 5 subscores: landmark knowledge, egocentric location, allocentric location, path route, and path survey. The landmark knowledge score is based on 8 items, while the other subscores reflect the mean performance of 4 items. See, Van der Ham et al. (Citation2020) for further details concerning task design.
Procedure
The experiment was conducted online, as part of a nationally promoted public experiment. Participants could join the experiment by smartphone or pc. Data collection was open for a year, participants were able to start the experiment at their own convenience. The experiment started with a few demographic questions, then the LNT was presented, which took around 10 minutes in total. Upon completion of the LNT the participant was asked if they would like to continue by filling out an optional questionnaire or if they would prefer to finish their participation. If they chose to fill out the questionnaire, the WQ was presented in full, taking another 10 minutes.
Analyses
The data was grouped based on gender and age group, into 14 participant groups. For each of the groups, the distribution of scores of each of the subscores was calculated. In order to provide insight into this distribution, the following percentile scores were calculated: 1%, 2%, 5%, 10%, 25%, 50%, 75%, 90%, 95%, 98% and 99%.
Results
Wayfinding questionnaire
First, the scores on the WQ were analyzed. depict the percentile scores for each of the participant groups, for females and males, respectively. Descriptive statistics of the raw data are available in the supplementary materials.
Table 2. Normative data for females, per age group for each subscale of the Wayfinding Questionnaire. For the Navigation and Orientation and Distance Estimation subscales the range is 1 (low performance) to 7 (high performance). For the Spatial Anxiety subscale the range is 1 (low anxiety) to 7 (high anxiety).
Table 3. Normative data for males, per age group for each subscale of the Wayfinding Questionnaire.
Leiden navigation test
Next, the scores on the LNT were analyzed in the same way. In the percentile scores for each of the participant groups can be found, for females and males, respectively. Descriptive statistics of the raw data are available in the supplementary materials.
Table 4. Normative data for females, per age group, for each of the subtasks of the Leiden Navigation Test.
Table 5. Normative data for males, per age group, for each of the subtasks of the Leiden Navigation Test.
WQ and LNT scores
As the WQ and LNT are both tests of navigation performance, at a subjective and objective level, respectively, a substantial correlation between both measures is to be expected. To this end, Pearson correlation coefficients were calculated for all subscales. shows the outcomes of this analysis, with the correlation coefficient for each combination of subscales, and level of significance marked. Notably, the WQ navigation and orientation subscale correlates significantly with all LNT subscores. WQ distance estimation does not correlate significantly with LNT landmark and LNT path route; the two subscores that do not entail metric details of the environment.
Table 6. Pearson correlation coefficients for each combination of the WQ and LNT subscales. * p < .05, **p < .01.
Discussion
The goal of the current study was to provide a clinical guideline to respond to complaints of navigation impairment in individuals with acquired brain injury, based on normative data from a large population-based control sample. Navigation impairment is frequently reported by neurological patients, but dedicated standardized testing materials are not yet available. By providing a clinical guideline with two standardized diagnostic tools, with the current work we aimed to facilitate informative diagnostic procedures concerning navigation performance. The WQ and experimental test battery LNT provide crucial elements for the proposed diagnostic procedure, by providing measures of subjective and objective navigation performance, respectively. Additionally, the outcomes can be used to guide the content of subsequent navigation rehabilitation exercises.
In the current study we provide normative data for the WQ as well as the LNT, for the first time. Normative data is presented by age, given the plethora of research showing strong impact of age on navigation performance (e.g., Moffat, Citation2009; Van der Ham et al., Citation2020). Because of the substantial and representative sample size, fourteen separate groups could be created, and percentile scores were calculated for each participant group ranging in size from 50 (oldest female participant group, 80–89 year old) to 1265 for the 60–69 year old females. Normative data was also split up by gender. In existing navigation literature, gender effects are frequently found (e.g., Jordan et al., Citation2004; Munion et al., Citation2019). The strength of such effects appears to depend on the specific task design of the task and possible spatial strategies used by participants (see e.g., Jordan et al., Citation2004). For the specific task design of the Leiden Navigation Test, gender differences are limited. As reported before, this is likely caused by the visual richness of the task design and the resulting spatial strategies (Van der Ham et al., Citation2020). Yet, for the wayfinding questionnaire, a pattern of male overestimation and female underestimation, and a higher level of spatial anxiety in females compared to males have been clearly found. Therefore, a distinction between males and females in the normative dataset is appropriate.
The suggested clinical guideline first entails the assessment of a subjective report of a patient. In case an individual with acquired brain injury reports difficulties finding their way around, which cannot be attributed to physical or other neurological causes (e.g., limited mobility, neglect), the clinician can administer the WQ. If the WQ shows impaired performance on one or more of the subscales, this indicates an impaired level of subjective navigation performance and can be considered an indication that administering the LNT could be helpful. The LNT provides a clarification of objective navigation performance, with subscores reflecting performance on each of the functional domains of navigation performance; landmark, egocentric location, allocentric location, path route, and path survey. The WQ and LNT show significant correlation, in which the navigation and orientation subscale is the most representative, as it correlates significantly with all subscores of the LNT. As the WQ distance estimation subscale correlates significantly only with the subscores of the LNT that reflect metric information (location egocentric, location allocentric, and path survey), this further substantiates the cognitive constructs measures with these subscores. The additional detail in performance provided by the subscores is therefore an essential addition to the self-report scores. As previously found, the subjective scores also appear to follow structural patterns of over- and underestimation, related to age and gender (Van der Ham et al., Citation2021). The objective performance on the LNT therefore provides important clarification. The outcome of the LNT can be used to diagnose navigation impairment in detail, by verifying whether impairment can be detected objectively, and by indicating which navigation domain is affected.
The use of a navigation impairment diagnosis can be highly valuable in interpretation of the complaints of a patient and may provide input to cognitive rehabilitation. Although in an experimental stage, there are multiple navigation training protocols available (Bouwmeester et al., Citation2015; Brooks, Citation1999; Incoccia et al., Citation2009; Kober et al., Citation2013; Lloyd et al., Citation2009; M. N. Van der Kuil et al., Citation2020), which in the future may be developed into formal clinical rehabilitation programs. If the impairment can be clarified in detail, this allows for well-informed decision during rehabilitation. For instance, a patient who specifically has trouble with landmark recognition, may benefit more from training the use of allocentric location information, when a compensatory approach is chosen. Or a patient who has difficulty reading maps could be trained to improve their route learning skills to compensate for this deficit (Van der Kuil et al., Citationsubmitted). Apart from cognitive exercises, the acquired information about the impairment can also support detailed psycho-education. Psycho-education has been shown to be successful tool to help a patient understand the impairment, its cause, and potentially also accept the impairment (e.g., Commissaris et al., Citation1996). Especially anxiety levels may reduce as a result of this. Lastly, a certain level of self-awareness is a key element for both psycho-education and cognitive training protocols, highlighting the need for self-reported complaints as a main starting point of the diagnostic procedure.
It should be noted that all data was collected online, which is a potential limitation. However, Van der Ham et al. (Citation2020) have established that the performance online on the LNT was highly similar to performance in a formal lab setting. Furthermore, a number of precautions were taken to ensure the quality of the data. The precautions included formal communication during recruitment to ensure healthy participants would join and the context in which the experiment was offered: there was a separate version for people with a neurological condition through a separate link on the same webpage. Moreover, the current online approach offers the opportunity to also perform this diagnostic procedure online in a clinical setting, reducing the need for lengthy appointments and travel time for patients. Furthermore, the data is based on sample of exclusively Dutch participants who responded to an open invitation to participate, this may have resulted in a sampling bias to some extent. Education level may have been skewed (relatively high level of education in the sample) and distribution across gender and age was uneven. Nevertheless, the sample size of 7150 participants can be considered very substantial and given its wide distribution across ages 18 to 89, the sample is expected to be sufficiently robust.
In short, with this study, we provide a clinical guideline to address navigation complaints in individuals with acquired brain injury. To this end, the diagnostic tools WQ and LNT can be used, along with the normative data presented here. In future developments, the detailed diagnosis of navigation impairment could be used to optimize cognitive rehabilitation programs to improve navigation skills in patients.
Data availability
Upon acceptance of the manuscript, the authors will make available the full dataset and standardized norms as reported in this paper online at www.vanderham.com
Acknowledgments
The authors wish to thank Milan van der Kuil for his contribution in designing the online experiment and data processing.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Allison, S. L., Fagan, A. M., Morris, J. C., & Head, D. (2016). Spatial navigation in preclinical Alzheimer’s disease. Journal of Alzheimer’s Disease, 52(1), 77–90. https://doi.org/10.3233/JAD-150855
- Bell, B. D. (2012). Route learning impairment in temporal lobe epilepsy. Epilepsy & Behavior, 25(2), 256–262. https://doi.org/10.1016/j.yebeh.2012.07.023
- Boccia, M., Di Vita, A., Diana, S., Margiotta, R., Imbriano, L., Rendace, L., … Guariglia, C. (2019). Is losing one’s way a sign of cognitive decay? Topographical memory deficit as an early marker of pathological aging. Journal of Alzheimer’s Disease, 68(2), 679–693. https://doi.org/10.3233/JAD-180890
- Bouwmeester, L., van de Wege, A., Haaxma, R., & Snoek, J. W. (2015). Rehabilitation in a complex case of topographical disorientation. Neuropsychological Rehabilitation, 25(1), 1–14. https://doi.org/10.1080/09602011.2014.923318
- Brooks, B. M. (1999). Route learning in a case of amnesia: A preliminary investigation into the efficacy of training in a virtual environment. Neuropsychological Rehabilitation, 9(1), 63–76. https://doi.org/10.1080/713755589
- Busigny, T., Pagès, B., Barbeau, E. J., Bled, C., Montaut, E., Raposo, N., … Pariente, J. (2014). A systematic study of topographical memory and posterior cerebral artery infarctions. Neurology, 83(11), 996–1003. https://doi.org/10.1212/WNL.0000000000000780
- Cerman, J., Ross, A., Laczo, J., Martin, V., Zuzana, N., Ivana, M., … Jakub, H. (2018). Subjective spatial navigation complaints-a frequent symptom reported by patients with subjective cognitive decline, mild cognitive impairment and Alzheimer’s disease. Current Alzheimer Research, 15(3), 219–228. https://doi.org/10.2174/1567205014666171120145349
- Claessen, M. H. G., & van der Ham, I. J. M. (2017). Classification of navigation impairment: A systematic review of neuropsychological case studies. Neuroscience & Biobehavioral Reviews, 73, 81–97. https://doi.org/10.1016/j.neubiorev.2016.12.015
- Claessen, M. H., Visser-Meily, J. M., de Rooij, N. K., Postma, A., & van der Ham, I. J. (2016a). A direct comparison of real-world and virtual navigation performance in chronic stroke patients. Journal of the International Neuropsychological Society, 22(4), 467–477. https://doi.org/10.1017/S1355617715001228
- Claessen, M. H. G., Visser-Meily, J. M., de Rooij, N. K., Postma, A., & van der Ham, I. J. (2016b). The wayfinding questionnaire as a self-report screening instrument for navigation-related complaints after stroke: Internal validity in healthy respondents and chronic mild stroke patients. Archives of Clinical Neuropsychology, 31(8), 839–854. https://doi.org/10.1093/arclin/acw044
- Claessen, M. H. G., Visser-Meily, J. M. A., Meilinger, T., Postma, A., de Rooij, N. K., & van der Ham, I. J. M. (2017). A systematic investigation of navigation impairment in chronic stroke patients: Evidence for three distinct types. Neuropsychologia, 103, 154–161. https://doi.org/10.1016/j.neuropsychologia.2017.07.001
- Cogné, M., Taillade, M., N’Kaoua, B., Tarruella, A., Klinger, E., Larrue, F., … Sorita, E. (2017). The contribution of virtual reality to the diagnosis of spatial navigation disorders and to the study of the role of navigational aids: A systematic literature review. Annals of Physical and Rehabilitation Medicine, 60(3), 164–176. https://doi.org/10.1016/j.rehab.2015.12.004
- Commissaris, K., Verhey, F. R., & Jolles, J. (1996). A controlled study into the effects of psychoeducation for patients with cognitive disturbances. The Journal of Neuropsychiatry and Clinical Neurosciences, 8(4), 429–435. https://doi.org/10.1176/jnp.8.4.429
- Coughlan, G., Laczó, J., Hort, J., Minihane, A. M., & Hornberger, M. (2018). Spatial navigation deficits—overlooked cognitive marker for preclinical Alzheimer disease? Nature Reviews Neurology, 14(8), 496–506. https://doi.org/10.1038/s41582-018-0031-x
- Coutrot, A., Silva, R., Manley, E., de Cothi, W., Sami, S., Bohbot, V. D., … Spiers, H. J. (2018). Global determinants of navigation ability. Current Biology, 28(17), 2861–2866. https://doi.org/10.1016/j.cub.2018.06.009
- Cushman, L. A., Stein, K., & Duffy, C. J. (2008). Detecting navigational deficits in cognitive aging and Alzheimer disease using virtual reality. Neurology, 71(12), 888–895. https://doi.org/10.1212/01.wnl.0000326262.67613.fe
- De Rooij, N. K., Claessen, M. H. G., van der Ham, I. J., Post, M. W. M., & Visser-Meily, J. M. A. (2019). The Wayfinding Questionnaire: A clinically useful self-report instrument to identify navigation complaints in stroke patients. Neuropsychological Rehabilitation, 29(7), 1042–1061. https://doi.org/10.1080/09602011.2017.1347098
- Gagnon, K. T., Thomas, B. J., Munion, A., Creem-Regehr, S. H., Cashdan, E. A., & Stefanucci, J. K. (2018). Not all those who wander are lost: Spatial exploration patterns and their relationship to gender and spatial memory. Cognition, 180, 108–117. https://doi.org/10.1016/j.cognition.2018.06.020
- Gazova, I., Vlcek, K., Laczó, J., Nedelska, Z., Hyncicova, E., Mokrisova, I., … Hort, J. (2012). Spatial navigation—a unique window into physiological and pathological aging. Frontiers in Aging Neuroscience, 4, 16. https://doi.org/10.3389/fnagi.2012.00016
- Grewe, P., Lahr, D., Kohsik, A., Dyck, E., Markowitsch, H. J., Bien, C. G., Botsch, M., & Piefke, M. (2014). Real-life memory and spatial navigation in patients with focal epilepsy: Ecological validity of a virtual reality supermarket task. Epilepsy & Behavior, 31, 57–66. https://doi.org/10.1016/j.yebeh.2013.11.014
- He, C., & Hegarty, M. (2020). How anxiety and growth mindset are linked to navigation ability: Impacts of exploration and GPS use. Journal of Environmental Psychology, 71, 101475. https://doi.org/10.1016/j.jenvp.2020.101475
- Incoccia, C., Magnotti, L., Laria, G., Piccardi, L., Guariglia, C. (2009). Topographical disorientation in a patient who never developed navigational skills: The (re) habilitation treatment. Neuropsychological Rehabilitation, 19(2), 291–314. https://doi.org/10.1080/09602010802188344
- Janzen, G., Jansen, C., & van Turennout, M. (2008). Memory consolidation of landmarks in good navigators. Hippocampus, 18(1), 40–47. https://doi.org/10.1002/hipo.20364
- Jordan, K., Schadow, J., Wuestenberg, T., Heinze, H. J., & Jäncke, L. (2004). Different cortical activations for subjects using allocentric or egocentric strategies in a virtual navigation task. Neuroreport, 15(1), 135–140. https://doi.org/10.1097/00001756-200401190-00026
- Klatzky, R. L. (1998). Allocentric and egocentric spatial representations: Definitions, distinctions and interconnections. In C. Freksa & C. Habel (Eds.), Spatial Cognition. p. 1–17.
- Kober, S. E., Wood, G., Hofer, D., Kreuzig, W., Kiefer, M., & Neuper, C. (2013). Virtual reality in neurologic rehabilitation of spatial disorientation. Journal of Neuroengineering and Rehabilitation, 10(1), 17. https://doi.org/10.1186/1743-0003-10-17
- Kremmyda, O., Hüfner, K., Flanagin, V. L., Hamilton, D. A., Linn, J., Strupp, M., … Brandt, T. (2016). Beyond dizziness: Virtual navigation, spatial anxiety and hippocampal volume in bilateral vestibulopathy. Frontiers in Human Neuroscience, 10, 139. https://doi.org/10.3389/fnhum.2016.00139
- Laczó, J., Andel, R., Vyhnalek, M., Vlcek, K., Nedelska, Z., Matoska, V., Gazova, I., Mokrisova, I., Sheardova, K., & Hort, J. (2014). APOE and spatial navigation in amnestic MCI: Results from a computer-based test. Neuropsychology, 28(5), 676–684. https://doi.org/10.1037/neu0000072
- Lawton, C. A. (1994). Gender differences in way-finding strategies: Relationship to spatial ability and spatial anxiety. Sex Roles, 30(11), 765–779. https://doi.org/10.1007/BF01544230
- Lemieux, C. L., Collin, C. A., & Watier, N. N. (2019). Gender differences in metacognitive judgments and performance on a goal-directed wayfinding task. Journal of Cognitive Psychology, 31(4), 453–466. https://doi.org/10.1080/20445911.2019.1625905
- Lemoncello, R., Sohlberg, M. M., & Fickas, S. (2010). When directions fail: Investigation of getting lost behaviour in adults with acquired brain injury. Brain Injury, 24(3), 550–559. https://doi.org/10.3109/02699050903446807
- Lester, A. W., Moffat, S. D., Wiener, J. M., Barnes, C. A., & Wolbers, T. (2017). The aging navigational system. Neuron, 95(5), 1019–1035. https://doi.org/10.1016/j.neuron.2017.06.037
- Livingstone, S. A., & Skelton, R. W. (2007). Virtual environment navigation tasks and the assessment of cognitive deficits in individuals with brain injury. Behavioural Brain Research, 185(1), 21–31. https://doi.org/10.1016/j.bbr.2007.07.015
- Lloyd, J., Riley, G. A., & Powell, T. E. (2009). Errorless learning of novel routes through a virtual town in people with acquired brain injury. Neuropsychological Rehabilitation, 19(1), 98–109. https://doi.org/10.1080/09602010802117392
- Lyons, I. A., Ramirez, G., Maloney, E. A., Rendina, D. N., Levine, S. C., & Beilock, S. L. (2018). Spatial Anxiety: A novel questionnaire with subscales for measuring three aspects of spatial anxiety. Journal of Numerical Cognition, 4(3), 2363–8761. https://doi.org/10.5964/jnc.v4i3.154
- Moffat, S. D. (2009). Aging and spatial navigation: What do we know and where do we go? Neuropsychology Review, 19(4), 478–489. https://doi.org/10.1007/s11065-009-9120-3
- Montello, D. R. (1998). A new framework for understanding the acquisition of spatial knowledge in largescale environments. In M. J. Egenhofer & R. G. Golledge (Eds.), Spatial and temporal reasoning in geographic information systems (pp. 143–154). Oxford University Press.
- Munion, A. K., Stefanucci, J. K., Rovira, E., Squire, P., & Hendricks, M. (2019). Gender differences in spatial navigation: Characterizing wayfinding behaviors. Psychonomic Bulletin & Review, 26(6), 1933–1940. https://doi.org/10.3758/s13423-019-01659-w
- Nadolne, M. J., & Stringer, A. Y. (2001). Ecologic validity in neuropsychological assessment: Prediction of wayfinding. Journal of the International Neuropsychological Society, 7(6), 675–682. https://doi.org/10.1017/S1355617701766039
- Post, M. W., Boosman, H., Van Zandvoort, M. M., Passier, P. E., Rinkel, G. J., & Visser-Meily, J. M. (2011). Development and validation of a short version of the stroke specific quality of life scale. Journal of Neurology, Neurosurgery & Psychiatry, 82(3), 283–286. https://doi.org/10.1136/jnnp.2009.196394
- Siegel, A. W., & White, S. H. (1975). The development of spatial representations of large-scale environments. Advances in Child Development and Behavior, 10, 9–55. https://doi.org/10.1016/S0065-2407(08)60007-5
- Sieverding, M., & Koch, S. C. (2009). (Self-) Evaluation of computer competence: How gender matters. Computers & Education, 52(3), 696–701. https://doi.org/10.1016/j.compedu.2008.11.016
- Tuena, C., Mancuso, V., Stramba-Badiale, C., Pedroli, E., Stramba-Badiale, M., Riva, G., & Repetto, C. (2021). Egocentric and allocentric spatial memory in mild cognitive impairment with real-world and virtual navigation tasks: A systematic review. Journal of Alzheimer’s Disease, 79(1), 95–116. https://doi.org/10.3233/JAD-201017
- Van der Ham, I. J. M., Claessen, M. H. G., Evers, A. W. M., & van der Kuil, M. N. A. (2020). Large-scale assessment of human navigation ability across the lifespan. Scientific Reports, 10(1), 1–12. https://doi.org/10.1038/s41598-020-60302-0
- Van der Ham, I. J. M., Kant, N., Postma, A., & Visser-Meily, J. M. A. (2013). Is navigation ability a problem in mild stroke patients? Insights from self-reported navigation measures. Journal of Rehabilitation Medicine, 45(5), 429–433. https://doi.org/10.2340/16501977-1139
- Van der Ham, I. J. M., van der Kuil, M. N. A., & Claessen, M. H. G. (2021). Quality of self-reported cognition: Effects of age and gender on spatial navigation. Aging & Mental Health, 25(5), 873–878. https://doi.org/10.1080/13607863.2020.1742658
- Van der Ham, I. J. M., van Zandvoort, M. J. E., Meilinger, T., Bosch, S., Kant, N., & Postma, A. (2010). Spatial and temporal aspects of navigation in two neurological patients. NeuroReport, 21(10), 685–689. https://doi.org/10.1097/WNR.0b013e32833aea78
- Van der Kuil, M. N., Evers, A. W., Visser-Meily, J., & van der Ham, I. J. (2020). The effectiveness of home-based training software designed to influence strategic navigation preferences in healthy subjects. Frontiers in Human Neuroscience, 14, 76. https://doi.org/10.3389/fnhum.2020.00076
- Van der Kuil, M. N. A., Visser-Meily, J. M. A., Evers, A. W. M., & van der Ham, I. J. M. (2021). Navigation ability in patients with acquired brain injury: A population-wide online study. Neuropsychological Rehabilitation, 1–24. https://doi.org/10.1080/09602011.2021.1893192
- Van der Kuil, M. N. A., Visser-Meily, J. M. A., Evers, A. W. M., & van der Ham, I. J. M. (submitted). Navigation training for ABI patients: Compensatory strategy training through blended care.